ABSTRACT
Lung volume reduction surgery (LVRS) is an option for select patients with advanced chronic obstructive pulmonary disease (COPD). Current guidelines recommend LVRS for patients with appropriate physiology and heterogeneous distribution of emphysema predominately involving upper lobes. We present an unusual case of a 72-year-old male with an advanced COPD who suffered with recurrent exacerbations despite optimal medical management. He underwent a two-stage bilateral lower lobe LVRS for heterogeneous lower lobe emphysema via video-assisted thoracoscopic (VATS) approach. This resulted in a significant subjective as well as objective improvement in his pulmonary functions, 6-min walk distance and subsequent discontinuation of supplemental oxygen.
INTRODUCTION
Lung volume reduction surgery (LVRS) is an option for patients with advanced chronic obstructive pulmonary disease (COPD). The National Emphysema Treatment Trial (NETT) showed benefit from LVRS among patients with heterogeneous emphysema [1]. Almost all the patients who undergo LVRS have upper lobe predominant disease [2].
Using proper selection criteria, lower lobe LVRS can be as beneficial as the upper lobe procedure.
We report a case of emphysema who successfully underwent staged lower lobe LVRS and provide a review of the literature.
CASE REPORT
A 72-year-old male, an ex-smoker (108 pack-years) with severe COPD presented for an LVRS evaluation. He was on an optimal medical treatment including inhaled corticosteroid, long acting beta-agonist and anti-muscarinic agent and Roflumilast. Despite supplemental oxygen and pulmonary rehabilitation he remained symptomatic and experienced frequent exacerbations requiring repeated steroids bursts.
His chest computed tomography (CT) revealed advanced centrilobular emphysema predominately involving the lower lobes (Fig. 1). His post-bronchodilator forced expiratory volume in 1 s (FEV1) was 0.54 l (17%), total lung capacity (TLC) 133%, residual volume (RV) 289% and a diffusion capacity 33% of predicted. Six-minute walk distance was 170 m. An ambulatory oxygen titration study showed the need for 4 l/min with exertion. The BODE score was 4. Alpha-1 antitrypsin level was normal. Arterial blood gas on room air showed a pO2 of 56 mmHg, pCO2 of 52 and a pH of 7.40. Cardiopulmonary exercise test (CPET) revealed V.O2 max = 10.5 ml/kg/min (43.9%) and a reduced Work Rate (WR) of 33 W (27.5%). The multidisciplinary team’s decision was to proceed with a staged lower lobe LVRS.
Figure 1.

Coronal section of the chest CT showing predominantly emphysematous lower lobes.
He underwent a right lower lobe lung LVRS via video-assisted thoracoscopic (VATS) approach. Roughly half of the lower lobe was endo-resected using a linear stapler cutter with buttressed stapling cartridges. The staple line proceeded from the anterior medial aspect of the lobe to all the way up towards the superior segment in a curvilinear fashion. Two thoracotomy tubes were placed. One was removed the next day and the other was switched to a Heimlich valve on discharge on Day 7. The latter was removed 3 days later.
Three months later, a left lower lobe LVRS via VATS was performed in a similar fashion. The resulting complex staple lines were fortified with a chemical sealant (Fig. 2). Two chest tubes were placed at the end of the procedure. He was discharged on post-op Day 4 with a single chest tube connected to a Heimlich valve which was removed on post-op Day 14.
Figure 2.
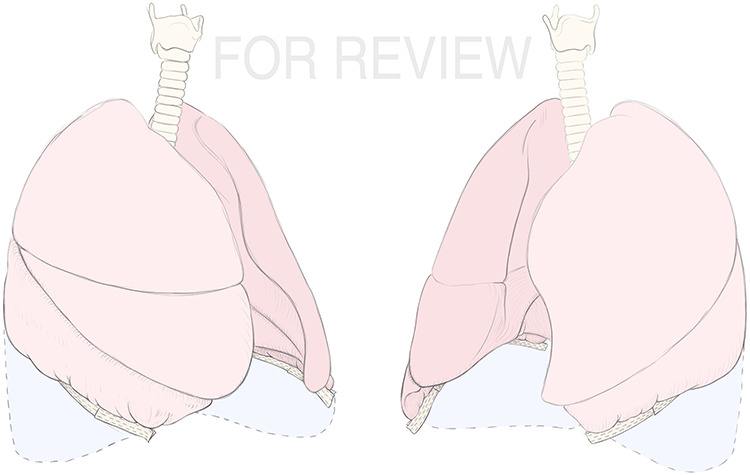
Artist rendition of bilateral lower lobe LVRS.
Preoperative and postoperative pulmonary functions performed at 3 and 6 months are depicted in Table 1. Repeat CPET recorded V.O2 max of 12.9 ml/kg/min (54.7%) and WR of 50 W (37.9%). The Saint George Respiratory Questionnaire (SGRQ) values at baseline and at 1 year are shown in Table 2.
Table 1.
Preoperative and postoperative testing [postoperative cardiopulmonary exercise testing was done 8 months after LVRS]
| Preoperative | 3 months after first LVRS | 2 months after second LVRS | 5 months after second LVRS | |
|---|---|---|---|---|
| FEV1/FVC | 26.36 | 31.4 | 30 | 27 |
| Pre BD FEV1 (l, % predicted) | 0.54 l (17%) | 0.91 l (29%) | 1 l (40%) | 0.95 l (31%) |
| Pre BD FVC (l, % predicted) | 2.1 l (46%) | 2.9 l (67%) | 3.3 l (80%) | 3.5 l (85%) |
| TLC (% predicted) | 133% | 84% | 116% | 96% |
| RV (% predicted) | 289% | 113% | 190% | 132% |
| DLCO (% predicted) | 33% | 40% | 40% | 43% |
| 6-min walk distance (m) | 119 m | 325 m | 341 m | 345 m |
| Work rate | 33 W | 50 W* |
Table 2.
Saint George respiratory questionnaire component
| Saint George respiratory questionnaire | Baseline | 1 year later |
|---|---|---|
| Symptoms | 66.54 | 36.51 |
| Activity | 91.72 | 37.30 |
| Impact | 31.25 | 11.11 |
| Overall | 56.52 | 23.39 |
Over the next 12 months follow-up, the patient reported continued improvement in his dyspnea. His 6-min walk distance improved from 158 to 374 m and he no longer required supplemental oxygen at rest. Since surgery, he suffered a single bout of moderate exacerbation, which was managed as an outpatient with a short course of oral steroids. Figure 3 compares a postoperative to a preoperative chest X-ray.
Figure 3.
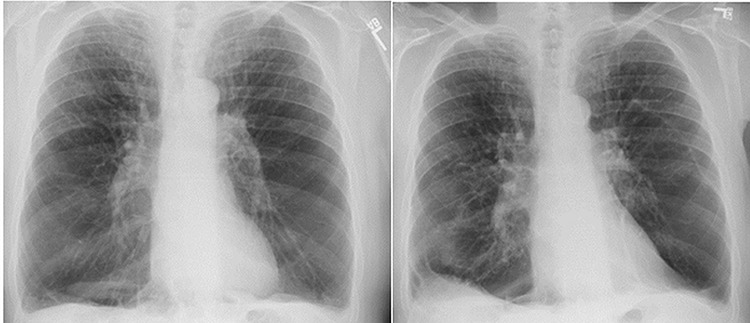
A posterioanterior (PA) chest X-ray comparing preoperative (left) to postoperative (right).
DISCUSSION
LVRS is an accepted therapeutic modality for patients with severe heterogeneous emphysema who are symptomatic despite optimal medical therapy [3]. Incidentally, the majority of patients have upper lobe predominant disease [1]. Interestingly, the lower lobe LVRS is not included in the recommendations.
Recently, reports of LVRS for lower lobe predominant emphysema are emerging in the literature. Perikleous [4] reported outcomes on 36 patients who underwent lower lobe LVRS via VATS for severe heterogeneous emphysema. Of these, 61% had normal alpha-1 Antitrypsin level. The surgery was performed in two stages in four patients. They reported improvement in FEV1 and RV/TLC ratio especially during first few months. These parameters returned to preoperative values at 24 months. The physical components of the quality of life (QOL) measurements also showed improvement. There were two reported deaths in the first 90 days.
Lower lobe predominant emphysema can present with normal alpha-1 antitrypsin level or alpha-1 antitrypsin deficiency (AAD) [5]. Gelb et al. [6] reported their experience with lower lobe LVRS in six patients with AATD. LVRS was staged and performed via VATS. Improvement in FEV1 and DLCO along with reduction in RV was observed. Cassina et al. [7] evaluated 18 COPD patients, with normal alpha-1 antitrypsin level. There were similar physiologic benefits up to 6 months, however in AATD group lung functions (except 6MWD) returned to baseline at 1 year and declined at 24 months. Tutic et al. [8] reported similar observations in 10 COPD patients with AATD who underwent lower lobe LVRS.
Interestingly, the largest trial to date on LVRS, the NETT trial, included 16 patients with AATD who showed worse outcomes for the 10 patients who underwent LVRS, however all these were upper lobe LVRS [9].
Endobronchial valve (EBV) placement is a novel approach to refractory COPD with heterogeneous emphysema [3]. Eberhardt et al. [10] reported outcomes in 60 patients who underwent EBV placement for heterogeneous emphysema, 15 had lower lobe EBV placement. The improvement in FEV1, 6MWD and SGRQ values was similar in both groups who underwent either upper or lower lobe valve placement; the only exception being the change in TLC, which was significantly better with the lower lobe group. None of the patients undergoing lower lobe EBV placement developed any complication. Fifteen complications were observed among 45 patients who underwent upper lobe EBV placement, including one death.
In summary, we believe that LVRS could be considered in select patients with lower lobe heterogeneous emphysema. It may provide effective palliation and a bridge to lung transplantation. At 6 months, our patient continued to enjoy improvements in airflow obstruction and hyperinflation. His QOL was dramatically improved compared to baseline at 1 year. Endobronchial valve therapy is also emerging as a viable lung volume reduction option for patients with lower lobe predominant emphysema.
ACKNOWLEDGEMENTS
None.
CONFLICT OF INTEREST
No conflicts of interest.
FUNDING
None.
ETHICAL APPROVAL
No ethical approval is required.
CONSENT
Informed consent was obtained from the patient.
GUARANTOR STATEMENT
Dr. Mohammed Al-Jaghbeer.
References
- 1. Fishman A, Martinez F, Naunheim K, Piantadosi S, Wise R, Ries A, et al. . A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med 2003;348:2059–73. doi: 10.1056/NEJMoa030287. [DOI] [PubMed] [Google Scholar]
- 2. Ginsburg ME, Thomashow BM, Bulman WA, Jellen PA, Whippo BA, Chiuzan C, et al. . The safety, efficacy, and durability of lung-volume reduction surgery: a 10-year experience. J Thorac Cardiovasc Surg 2016;151:717–24. doi: 10.1016/j.jtcvs.2015.10.095. [DOI] [PubMed] [Google Scholar]
- 3. Global Initiative for Chronic Obstructive Lung Disease (GOLD) Global Strategy for the Diagnosis, Management and Prevention of Chronic Obstructive Pulmonary Disease: 2019 Report. www.goldcopd.org (7 March 2019, date last accessed).
- 4. Perikleous P, Sharkey A, Oey I, Bilancia R, Tenconi S, Rathinam S, et al. . Long-term survival and symptomatic relief in lower lobe lung volume reduction surgery. Eur J Cardiothorac Surg 2017;52:982–8. doi: 10.1093/ejcts/ezx242. [DOI] [PubMed] [Google Scholar]
- 5. Parr DG, Stoel BC, Stolk J, Stockley R. Pattern of emphysema distribution in alpha-1 anti-trypsin deficiency influences lung function impairment. Am J Respir Crit Care Med 2004;170:1172–8. doi: 10.1164/rccm.200406-761OC. [DOI] [PubMed] [Google Scholar]
- 6. Gelb AF, McKenna RJ, Brenner M, Fischel R, Zamel N. Lung function after bilateral lower lobe lung volume reduction surgery for a1-antitrypsin emphysema. Eur Respir J 1999;14:928–33. doi: 10.1034/j.1399-3003.1999.14d33.x. [DOI] [PubMed] [Google Scholar]
- 7. Cassina PC, Teschler H, Konietzko N, Theegarten D, Stamatis G. Two-year results after lung volume reduction surgery in alpha-1 antitrypsin deficiency versus smoker’s emphysema. Eur Respir J 1998;12:1028–32. doi: 10.1183/09031936.98.12051028. [DOI] [PubMed] [Google Scholar]
- 8. Tutic M, Bloch KE, Lardinois D, Brack T, Russi EW, Weder W. Long-term results after lung volume reduction surgery in patients with alpha-1 antitrypsin deficiency. J Thorac Cardiovasc Surg 2004;128:408–13. doi: 10.1016/j.jtcvs.2004.03.040. [DOI] [PubMed] [Google Scholar]
- 9. Stoller JK, Gildea TR, Ries AL, Meli YM, Karafa MT. Lung volume reduction surgery in patients with emphysema and α-1 antitrypsin deficiency. Ann Thorac Surg 2007;83:241–51. doi: 10.1016/j.athoracsur.2006.07.080. [DOI] [PubMed] [Google Scholar]
- 10. Eberhardt R, Herth FJH, Radhakrishnan S, Gompelmann D. Comparing clinical outcomes in upper versus lower lobe endobronchial valve treatment in severe emphysema. Respiration 2015;90:314–20. doi: 10.1159/000437358. [DOI] [PubMed] [Google Scholar]


