ABSTRACT
Primary vaginal leiomyosarcoma (VLMS) is an extremely rare variant of primary vaginal cancers with very poor prognosis irrespective of the stage at presentation and the type of treatment received. It is easily recurrent and has a high propensity for haematogenous spread especially to the lungs. We present the case of a 34-year-old Para 1 + 1 (1 alive) woman with recurrent vaginal mass of 8 years duration after two surgical excisions without histological evaluation. She had examination under anaesthesia and a wide local excision of the vaginal mass. Histological examination of the mass revealed poorly differentiated VLMS with positive surgical margins and she was commenced on adjuvant chemo-radiation. Histological evaluation remains the hallmark for diagnosing rare malignancies like VLMS, which unfortunately is not a standard practice in some resource-constraint settings.
INTRODUCTION
Primary vagina cancer (PVC) is a rare occurrence in gynaecological practice. It accounts for ~1–2% of all malignancies in gynaecology and approximately one-tenth of all vaginal malignancies [1]. It is usually a diagnosis of exclusion, as most vaginal malignancies are metastasis from other primary sites [1]. The cervix and vulva are the most common gynaecological sites, whereas the bladder, urethra and rectum are common non-gynaecological sites [2]. Majority of PVC are squamous in origin, followed by adenocarcinomas, while sarcomas are very rare, accounting for ~1% of vaginal cancers [1,3]. Vaginal leiomyosarcoma (VLMS) is the most common form of vaginal sarcoma seen in adult women while rhabdomyosarcoma is commonly seen in children and adolescents [4,5]. We present a rare case of recurrent primary VLMS, an overview of its management and challenge with diagnosis in resource-constraint setting.
CASE REPORT
A 34-year-old Para 1 + 1 (1 alive) woman presented at the Gynaecological Outpatient Clinic of a public tertiary hospital in Lagos, Nigeria with 8 years history of recurrent vaginal mass and 5 years history of vaginal pain. The mass was initially small like a bean seed but gradually increased in size until it became palpable at the introitus. Vaginal pain was persistent, aching in nature, with a severity of 6 on the numerical pain scale and no aggravating or relieving factors. No history of vaginal instrumentation, abnormal vaginal bleeding or discharge, weight loss, respiratory, urinary and bowel symptoms. She had no history of pelvic irradiation, insertion of vaginal implant, personal or family history of uterine fibroids or malignancies. She had two surgical resections of the tumour in the past, but histology was not carried out due to financial constraint.
Her general, breast and abdominal examination findings were essentially normal but vaginal examination revealed a polypoid mass in the lower vagina. A diagnosis of recurrent vaginal polyp with suspected malignancy was made and she was counselled for examination under anaesthesia (EUA), wide local excision (WLE) and histological evaluation of the tumour.
Investigations revealed normal haematological, renal and liver function profiles. Hepatitis B, C and human immunodeficiency virus screenings were negative; Pap smear was negative for intraepithelial lesion or malignancy. Serum cancer-antigen 125, carcino-embryonic-antigen, chest X-ray and abdomino-pelvic computerized tomography scan were normal.
EUA revealed normal vulva and polypoid mass ~6 cm × 4 cm × 2 cm arising from the lower third of the right lateral vaginal wall. The mass was irregular, firm, encapsulated and attached to the muscular wall. The cervix, uterus, adnexae and rectum were normal. There were no enlarged inguinal lymph nodes. A WLE with a surgical margin of 10 mm was done and histology revealed nodular multi-lobulated solid firm masses with greyish white cut surfaces on macroscopy. Microscopic analysis showed a highly cellular encapsulated lesion, composed of interlacing fascicles of pleomorphic spindle shaped cells with marked nuclear pleomorphism, hyperchromasia, bizarre multinucleated giant cells with abnormal mitosis >10 mitoses/10 HPF. The tumour cells show moderately strong positivity for ki-67, alpha-smooth muscle actin, and desmin but was negative for s-100 (Figs 1–4) and the surgical margins were positive for malignant cells. A diagnosis of poorly differentiated VLMS was made with International Federation of Gynecology and Obstetrics clinical stage 1B disease. She had sequential chemo-radiation therapy with four courses of docetaxel and gemcitabine chemotherapy followed by external beam (45 Gy) and intra-cavitary (25 Gy) radiation. She responded well to the therapy and she is currently being followed up in the clinic.
Figure 1.
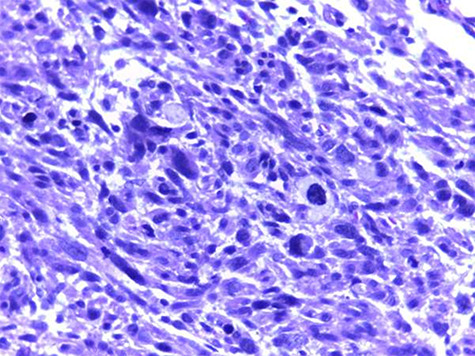
Photomicrograph of haematoxylin and eosin histologic section (×100) shows interlacing fascicles of atypical spindle cells with patchy necrosis, abnormal mitoses and smudge cells.
Figure 4.
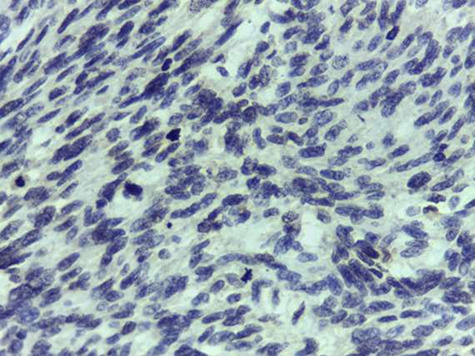
Photomicrograph of S100 immunostain (×100) shows spindle cell negativity.
Figure 2.
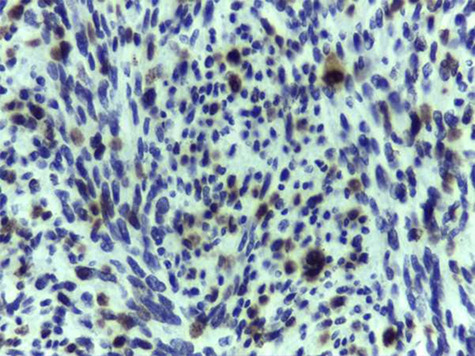
Photomicrograph of ki-67 immunostain (×100) shows moderately strong nuclear staining in >30% of the cell population.
Figure 3.
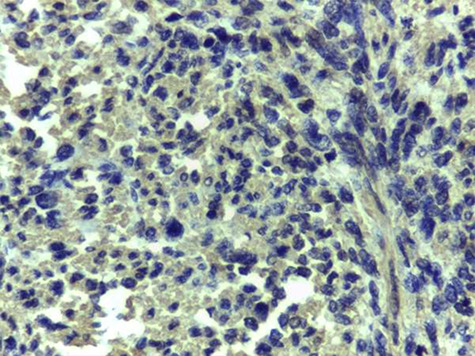
Photomicrograph of α-smooth muscle actin immunostain (×100) shows cytoplasmic staining of the smooth muscle cells.
DISCUSSION
Primary VLMS accounts for 2–3% of vaginal malignancy [6]. This rarity has contributed to the poor understanding of its unique clinical characteristics that could aid early diagnosis. As a result, postoperative histology remains the hallmark of diagnosis, [7] which was delayed in the case presented. The exact aetiology of VLMS is unknown. Exposure to pelvic radiotherapy and insertion of vaginal implants has been implicated in its aetiology [8]; but this was not the case in the patient presented. VLMS is believed to commonly arise from the smooth muscles of the vagina or its adjacent structures [7]. Majority (45%) arises from the posterior vaginal wall, followed by 34% from the lateral vaginal wall and 21% from the anterior vaginal wall [7]. In the patient presented, VLMS originated from the right lateral vaginal wall.
There are strict criteria for the diagnosis of PVC. This is because majority of vaginal malignancies are metastasis from other sites, with 80–90% from the cervix and vulva [1,2]. As a rule, the cancer must be exclusive to the vagina [2], with absence of clinical or histological evidence of cervical or vulvar malignancy or history suggestive of these cancers within the last 5–10 years [1]. This rule was fulfilled in the case presented.
There are no established guidelines for the management of VLMS. However, surgical treatment with or without adjuvant radiotherapy and/or chemotherapy is recommended by most authors [4,7,10]. The preferred surgical treatment is WLE with clear margins. Because of the high rate of recurrence of VLMS and the high potential of haematogenous spread even with early stage disease and complete tumour resection; postoperative radiotherapy and/or chemotherapy are frequently indicated especially in patients with metastasis, positive margins and risk factors for early recurrence. These factors include tumour size ≥ 3 cm, irregular tumour contour, presence of cellular atypia, ≥5 mitoses/10 HPF and poorly differentiated lesions [4,7–10]. The patient presented was commenced on adjuvant therapy because she had all the risk factors, positive surgical margins and a recurrent disease.
This case highlights the challenges encountered in resource-constraint settings where histological evaluation of surgical specimen is usually not considered important by patients and mandatory by physicians. Consequently, this test is usually delayed or not performed at all due to reasons such as financial constraint as seen in the case presented. This highlights the need for advocacy on the importance of performing histology on all surgical specimens, irrespective of the perceived pathology. Vaginal tumours are rare pathological entities that should be subjected to biopsy or excision for histological evaluation, irrespective of its size, clinical appearance and presence or absence of symptoms. This will ensure early diagnosis and management of any malignant lesion especially extremely rare and aggressive malignancy like VLMS.
ACKNOWLEDGEMENTS
The authors appreciate and thank everyone who contributed to the successful writing of the manuscript.
CONFLICT OF INTEREST
None declared.
FUNDING
There was no source of funding.
ETHICAL APPROVAL
Ethics approval for this report was obtained from the human research and ethics committee of the public tertiary hospital where the patient was being managed (ADM/DCST/HREC/APP/3453).
CONSENT
The authors certify that they have obtained all appropriate patient consent. In the consent form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understood that all her identifiable information will not be published.
GUARANTOR
The corresponding author (Adeyemi A. Okunowo) will be the guarantor for this paper.
REFERENCES
- 1. Adhikari P, Vietje P, Mount S. Premalignant and malignant lesions of the vagina. Diagn Histopathol 2017;23:28–34. [Google Scholar]
- 2. Lima M, Rio G, Horta M, Cunha TM. Primary vaginal malignancies: a single oncology Centre experience. J Obstet Gynaecol 2019;39:827–32. [DOI] [PubMed] [Google Scholar]
- 3. Walker DK, Salibian RA, Salibian AD, Belen KM, Palmer SL. Overlooked diseases of the vagina: a directed anatomic-pathologic approach for imaging assessment. Radiographics 2011;31:1583–98. [DOI] [PubMed] [Google Scholar]
- 4. Bassaw B, Fletcher H, Chinnia J. Leiomyosarcoma of the vagina in pregnancy. Eur J Gynaecol Oncol 2015;36:339–40. [PubMed] [Google Scholar]
- 5. Adams TS, Cuello MA. Cancer of the vagina. Int J Gynecol Obstet 2018;143:14–21. [DOI] [PubMed] [Google Scholar]
- 6. Keller NA, Godoy H. Case report. Leiomyosarcoma of the vagina: an exceedingly rare diagnosis. Case Rep Obstet Gynecol 2015;363895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ahram J, Lemus R, Schiavello HJ. Leiomyosarcoma of the vagina: case report and literature review. Int J Gynecol Cancer 2006;6:884–943. [DOI] [PubMed] [Google Scholar]
- 8. Moller K, Mathes GL Jr, Fowler W Jr. Primary leiomyosarcoma of the vagina: case report involving a TVT allograft. Gynecol Oncol 2004;94:840e2. [DOI] [PubMed] [Google Scholar]
- 9. Suh MJ, Park DC. Leiomyosarcoma of the vagina: a case report and review from the literature. J Gynecol Oncol 2008;19:261–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Toeldo G, Oliva E. Smooth muscle tumours of the uterus: a practical approach. Arch Pathol Lab Med 2008;132:595–605. [DOI] [PubMed] [Google Scholar]


