Sir,
Malaria is a major global public health problem with 219 million new cases of malaria in 87 countries as reported in 2017.[1] Despite the improvements in preventive measures and treatment, malaria imposes a great burden, causing 435,000 deaths in 2017.[1] While Plasmodium falciparum malaria is definitely considered more lethal, it is now evident that Plasmodium vivax infection also causes severe morbidity.[2] The spectrum ranges from cough and acute breathlessness to pulmonary edema, acute respiratory distress syndrome, and death even after malaria treatment initiation.[3] We hereby report a case of a 40-year-old male patient who presented with high-grade fever associated with chills and rigors for 1 week. The patient denied any history of cough, dyspnea, headache, and joint pain.
On examination at admission, the patient was conscious, oriented, blood pressure was 90/66 mm Hg, pulse rate was 110/min with normal respiratory rate, and had 98% O2 saturation on room air. Hepatosplenomegaly was present on abdominal examination. The rest of the examination was unremarkable. Investigations revealed that hemoglobin was 11.6 g/dl, white blood count was 2100 (neutrophils – 56% and lymphocytes – 40%), platelets were 22000/mm3, urea was 68 mg/dl, serum creatinine was 1.4 mg/dL, aspartate transaminase was 122 IU/L, (alanine transaminase) ALT was 57 IU/L, total bilirubin was 1.5 mg/dl, and chest roentgenogram was normal. Peripheral smear revealed trophozoites and sporozoites of Plasmodium vivax malaria. The patient was started on injection artesunate 120 mg, intravenous (IV) fluids, and other supportive medications. Fever responded partially, and the patient continued to have mild spikes of fever.
On the 5th day of hospital stay, the patient started having hemoptysis. There was no bleeding from any other site. The patient was tachypneic with respiratory rate of 36/min and saturation dipped to 80% on room air. Respiratory system examination revealed diffuse coarse crepitations bilaterally. Arterial blood gas analysis showed pH of 7.54, HCO3 was 14 mEq/l, PaO2 was 40.5 mmHg, and PaCO2 was 17 mmHg (PaO2/FiO2< 100). Chest roentgenogram showed bilateral diffuse opacities [Figure 1]. The patient was shifted to the intensive care unit, and oxygen inhalation was started.
Figure 1.
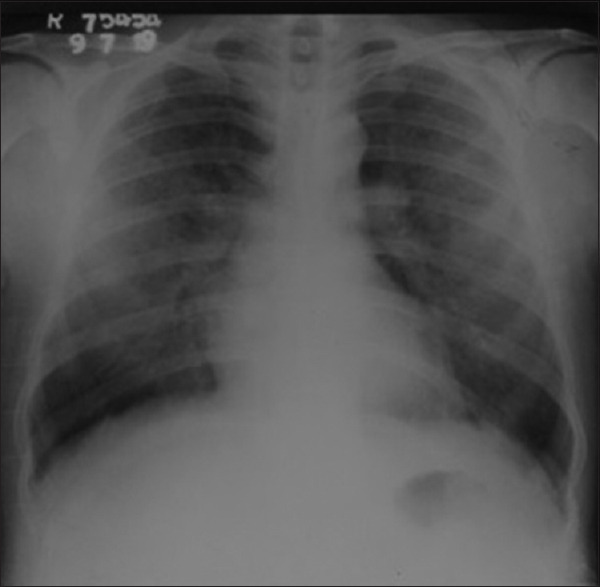
Chest X-ray on day 5, showing bilateral diffuse opacities
Fall in hemoglobin was noted from 11.6 to 7.8 g/dl and platelets reduced to 13,000/mm3. The patient was given platelet and packed cell transfusion and was started on broad-spectrum antibiotics in suspicion of superimposed bacterial infection. Prothrombin time was 12.5 s, INR was 1.1, activated partial thromboplastin time (APTT) was 26.9 s, and D-dimer levels were 330 ng/ml. Serology for leptospirosis and dengue was negative.
Contrast-enhanced CT scan of the chest was done on an urgent basis which showed crazy-paving pattern in bilateral lung fields suggestive of diffuse alveolar hemorrhage [Figure 2]. Anti-nuclear antibody, C-antineutrophil cytoplasmic antibody (ANCA), P-ANCA, and anti-glomerular basement membrane (GBM) antibody were negative. Urine routine microscopy was normal, and sputum for acid-fast bacilli was negative.
Figure 2.

Contrast-enhanced computed tomography chest showing crazy paving suggestive of alveolar haemorrhage
The patient was given methyl prednisolone 1 g IV for 5 days. The patient improved symptomatically, fever subsided, tachypnea resolved, arterial blood gas analysis also improved, and normal vesicular breath sounds were heard over the next 3–4 days. The patient was followed up on outpatient basis. There were no complaints of breathlessness, normal vesicular breath sounds were heard, and chest radiograph was normal.
The causes of diffuse alveolar hemorrhage (DAH) can be divided into infectious and noninfectious although intraalveolar hemorrhage in patients with malaria was found to be a rare finding even after intensive literature search. Most cases of DAH are caused by capillaritis associated with systemic autoimmune diseases such as C-ANCA, P-ANCA-associated vasculitis, anti-GBM disease, and systemic lupus erythematosus, but DAH may also result from inhaled toxins, coagulation disorders, and infection.[3]
The potential mechanisms include endothelial injury with alterations in endothelial permeability, leading to interstitial and alveolar edema and intravascular sequestration of leukocytes. Probably, this leads to inflammation of capillaries and thus leading to intraalveolar hemorrhage. An inflammatory cause is seen in autopsy studies in patients with vivax malaria showing increased alveolar-capillary monocytes and increased pulmonary phagocytic cell activity 1–2 days after the commencement of treatment for vivax malaria.[3,4]
DAH in vivax malaria reflects a posttreatment intravascular inflammatory response to the death of parasites or reperfusion. This is consistent with the fact that our patient too had diffuse alveolar hemorrhage posttreatment. In this case, disseminated intravascular coagulation was ruled out as patient had normal partial thromboplastin, APTT, and normal D-dimer levels. After giving methyl prednisolone, the patient showed improvement in respiratory functions and chest roentgenogram also became normal. Steroids and agents such as cyclophosphamide are being used in patients with DAH secondary to vasculitis.[5] Although our patient improved with steroids, still there is no proven evidence regarding the role of steroids in the management of pulmonary complications of malaria, and this could be an area of research whether steroids can be used for postinflammatory state or not.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.World Health Organization. World Malaria Report 2018. Geneva: WHO; 2018. https://wwwwhoint/malaria/media/world-malaria-report-2018/en/ [Google Scholar]
- 2.Rahimi BA, Thakkinstian A, White NJ, Sirivichayakul C, Dondorp AM, Chokejindachai W. Severe vivaxmalaria: A systematic review and meta-analysis of clinical studies since 1900. Malar J. 2014;13:481. doi: 10.1186/1475-2875-13-481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park MS. Diffuse alveolar hemorrhage. Tuberc Respir Dis (Seoul) 2013;74:151–62. doi: 10.4046/trd.2013.74.4.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anstey NM, Handojo T, Pain MC, Kenangalem E, Tjitra E, Price RN, et al. Lung injury in vivax malaria: Pathophysiological evidence for pulmonary vascular sequestration and posttreatment alveolar-capillary inflammation. J Infect Dis. 2007;195:589–96. doi: 10.1086/510756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ittyachen A, Lakshmanakumar VK, Eapen CK, Joseph MR. Methylprednisolone as adjuvant in treatment of acute respiratory distress syndrome owing to leptospirosis: A pilot study. Indian J Crit Care Med. 2005;9:133–6. [Google Scholar]


