Sir,
Pleural effusion is a common disease that leads to poor quality of life and morbidity and mortality. Rare causes of pleural effusion such as pleural lipomas can pose diagnostic dilemmas to the clinicians. Pleural lipomas are slow-growing tumors, with no malignant potential.[1] The awareness among clinicians about this entity as a rare cause of pleural effusion will help define diagnostic and therapeutic approaches for improved patient outcomes.
A 55-year-old male, farmer by occupation, and never smoker presented with complaints of dry cough off and on for 6 months, dyspnea for 4 months, and dull aching chest pain for 3 months.
Past history revealed that the patient had consulted a local practitioner for his symptoms, 3 month back and was prescribed antituberculosis therapy on the basis of chest X-ray posteroanterior (PA) view. The patient had undergone therapeutic pleurocentesis on three occasions, and approximately 500 ml fluid was evacuated on each occasion. Chest X-ray PA view at admission revealed bilateral pleural effusion (right >left). Ultrasonogram (USG) of the thorax was done and was reported as approximately 1 L of pleural fluid on the right side and 700 ml on the left side. Diagnostic pleurocentesis was done by both sides. Pleural fluid was deep yellow in appearance. Biochemical analysis revealed it to be exudative in nature, lymphocytic predominant on differential cell count with adenosine deaminase (ADA) value of 20 IU/ml on the right side and 18 IU/ml on the left side. Pleural fluid smear was negative for acid-fast bacilli or any microorganism on smear. In view of low ADA values, two consecutive pleural fluid samples were sent for cytology but were negative for malignant cells. USG of the whole abdomen was normal. Contrast-enhanced computed tomography (CT) of the thorax revealed massive pleural effusion with reactive collapse on the right side and moderate pleural effusion on the left side and no other abnormality.
A semirigid thoracoscopy on the right side revealed smooth, lobulated, multiple smooth yellowish nodules studded on the parietal pleura at multiple sites [Figure 1]. The patient had drainage of approximately 200 ml/day through his intercostal chest drain. Histopathology of biopsy sample [Figure 2] was reported as adipose tissue comprising adipocytes with acute and chronic inflammatory infiltrate and no evidence of atypia or malignancy, a finding which is characteristic of pleural lipomas. We made the diagnosis as a case of massive pleural effusion cause pleural lipomatosis and referred the patient to a thoracic surgeon for video-assisted thoracoscopic surgery.
Figure 1.
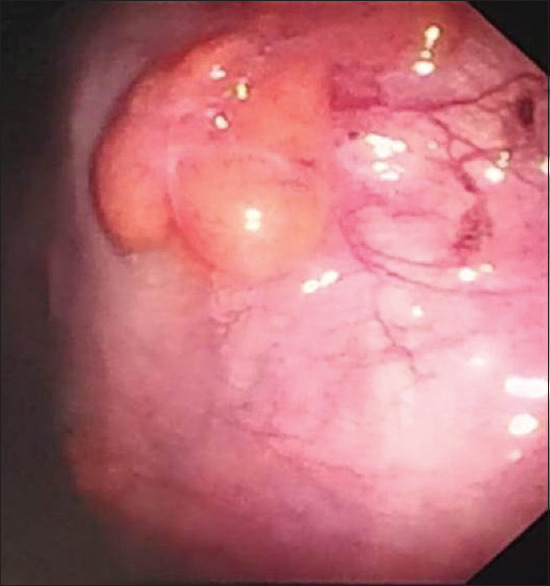
Smooth, lobulated and smooth yellowish nodules studded on the parietal pleura at multiple sites
Figure 2.
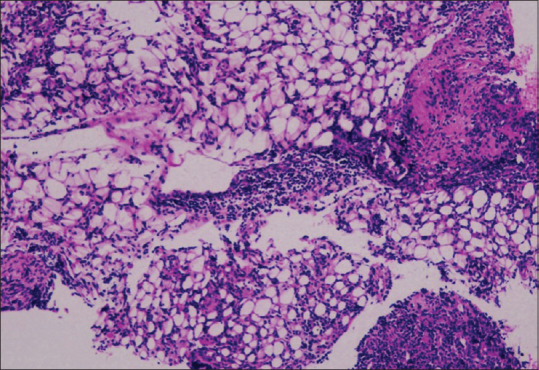
Histopathology of biopsy sample reported as adipose tissue comprising adipocytes
Pleural lipomas are benign soft-tissue neoplasms that originate from the submesothelial layers of parietal pleura and extend into the subpleural, pleural, or extrapleural space. They are soft, encapsulated fatty tumors with slow growth. Pleural lipomas are exceedingly rare, with only three cases reported before 1970, and only 10 additional cases reported after that worldwide.[2]
In most cases, pleural lipomas remain asymptomatic until incidental detection of the lesions at radiography. Symptoms may include nonproductive cough, back pain, exertional dyspnea, or a sensation of heaviness in the chest.[3] Pleural lipomas appear as soft-tissue lesions on chest radiographs and may become extremely large. At CT, they are homogeneous and demonstrate fat attenuation (approximately − 50 HU).[4]
CT scan is the modality of choice for imaging of pleural disease, after an initial assessment by chest X-ray. Semirigid thoracoscopy visualizes the parietal pleura, diaphragm, lung, and anterior and partial posterior mediastinum.[5] In patients with only pleural fluid visible on CT scan, thoracoscopy should be the next investigation for the final diagnosis.[6] In our case after assessment with CT, we used semirigid thoracoscopy to visualize the parietal pleura which revealed masses studding the parietal pleural. Histopathology of the masses revealed lipomas which clinched the diagnosis.
Previously, Abumossalam had reported a case of pleural lipomatosis, leading to massive pleural effusion and was diagnosed by thoracoscopy.[7] Medical thoracoscopy is the procedure of choice for evaluating undiagnosed pleural effusions.[8] The sensitivity of thoracoscopy-guided biopsy in malignant pleural effusions is 95%, compared to 62% for pleural fluid cytology and 44% for closed pleural biopsy.[9] Our case report also highlights the crucial role of thoracoscopy in the diagnosis of pleural effusion due to benign pleural tumors such as lipoma.
To the best of our knowledge, this is the only case of pleural lipomatosis resulting in the massive pleural effusion, reported in Indian literature and the second such case reported from the world literature. The rarity of presentation and the need to sensitize clinicians about this as a possible cause of undiagnosed pleural effusion led us to report this case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Erb CT, Johnson KM, Kim AW. Rare pleural tumors. Clin Chest Med. 2013;34:113–36. doi: 10.1016/j.ccm.2012.12.001. [DOI] [PubMed] [Google Scholar]
- 2.Jayle C, Hajj-Chahine J, Allain G, Milin S, Soubiron L, Corbi P. Pleural lipoma: A non-surgical lesion? Interact Cardiovasc Thorac Surg. 2012;14:735–8. doi: 10.1093/icvts/ivs052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Politis J, Funahashi A, Gehlsen JA, DeCock D, Stengel BF, Choi H. Intrathoracic lipomas. Report of three cases and review of the literature with emphasis on endobronchial lipoma. J Thorac Cardiovasc Surg. 1979;77:550–56. [PubMed] [Google Scholar]
- 4.Kato M, Saji S, Kunieda K, Yasue T, Nishio K, Adachi M. Mediastinal lipoma: Report of a case. Surg Today. 1997;27:766–8. doi: 10.1007/BF02384994. [DOI] [PubMed] [Google Scholar]
- 5.Loddenkemper, Lee P, Noppen M, Mathur PN. Medical thoracoscopy/pleuroscopy: Step by step. Breathe. 2011;8:156–67. [Google Scholar]
- 6.Metintas M, Ak G, Dundar E, Yildirim H, Ozkan R, Kurt E, et al. Medical thoracoscopy vs. CT scan-guided Abrams pleural needle biopsy for diagnosis of patients with pleural effusions: A randomized, controlled trial. Chest. 2010;137:1362–8. doi: 10.1378/chest.09-0884. [DOI] [PubMed] [Google Scholar]
- 7.Abumossalam AM. Pleural lipomatosis: A new pose of occult pleura effusion. Egypt J Bronchol. 2016;10:76–8. [Google Scholar]
- 8.Panjwani A, Salman MR. An uncommon cause of pleural effusion. Breathe (Sheff) 2019;15:e84–9. doi: 10.1183/20734735.0365-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loddenkemper R, Grosser H, Gabler A. Prospective evaluation of biopsy methods in the diagnosis of malignant pleural effusions. Intrapatient comparison between pleural fluid cytology, blind needle biopsy and thoracoscopy. Am Rev Respir Dis. 1983;127:114. [Google Scholar]


