Highlights
-
•
Pre-pandemic disgust proneness predicts coronavirus anxiety and safety behaviors.
-
•
Effect moderated by current perceived stress.
-
•
Highest anxiety response in those with high disgust proneness and current stress.
-
•
Disgust proneness may contribute to maladaptive anxiety responses to the pandemic.
Keywords: Coronavirus, Disgust, Stress, Anxiety, Pandemic
Abstract
Although health anxiety and corresponding safety behaviors can facilitate disease transmission avoidance, they can be maladaptive in excess, including during the coronavirus pandemic. Disgust proneness (i.e., tendency to experience and be sensitive to disgust) is one factor that may predict elevated coronavirus anxiety and safety behaviors during the pandemic, given the role of disgust in avoiding disease transmission. The present study examined the relations between pre-pandemic disgust proneness and coronavirus anxiety and safety behaviors in community adults who completed a 2016 study and were re-contacted on 4/1/2020 (N = 360). Interactions between pre-pandemic disgust proneness and current perceived stress were tested to examine a diathesis-stress model of the role of disgust proneness in anxiety response to the pandemic. Increased pre-pandemic disgust proneness predicted increased coronavirus anxiety and safety behaviors, controlling for number of COVID-19 cases by state. Consistent with a diathesis-stress model, current perceived stress moderated this effect, such that highest coronavirus anxiety and safety behaviors were reported by those with high disgust proneness and high stress. Trait disgust proneness may be a vulnerability factor for anxiety responses to the coronavirus pandemic, particularly among individuals experiencing high stress. Assessing disgust proneness and current stress may facilitate targeted anxiety intervention during the pandemic.
1. Introduction
The coronavirus pandemic and its resulting condition, COVID-19 have devastated society in a multitude of ways, such as the loss of human life, negative economic consequences, enforced social distancing, and the unemployment of countless workers. Among these outcomes, there is concern about the impact of the pandemic on mental health, and who may be most vulnerable to psychological distress. It may be the case that individuals with certain personality traits (e.g., a heightened propensity to experience disgust) are at a greater risk of experiencing heightened coronavirus anxiety, or what a recently proposed model of fear during the coronavirus pandemic describes as fear for the body (Schimmenti, Billieux, & Starcevic, 2020). Indeed, research conducted during the H1N1 “swine-flu” pandemic from 2009 to 2010 and the Ebola outbreak in 2014–2015 found that anxiety responses were positively associated with disgust proneness, health anxiety, and contamination fears (Blakey, Reuman, Jacoby, & Abramowitz, 2015; Brand, McKay, Wheaton, & Abramowitz, 2013; Wheaton, Abramowitz, Berman, Fabricant, & Olatunji, 2012). These studies indicate the existence of identifiable predictors of anxiety during viral outbreaks and suggest the need for similar research during the coronavirus pandemic. Compared to previous viral outbreaks, COVID-19 appears to have a higher rate of transmissibility and a longer incubation period, the latter of which is associated with higher risk of asymptomatic individuals unknowingly infecting others prior to symptom onset (Xie & Chen, 2020). High rates of asymptomatic transmission are thought to contribute to rapid spread of the coronavirus (Li et al., 2020) and may result in increased coronavirus anxiety due to decreased certainty about the health status of others and decreased predictability of one’s own health status and role as potential disease vector.
Coronavirus anxiety may be conceptualized as a specific form of health anxiety, or obsessive and irrational worry about contracting a serious medical condition. Indeed, recent studies indicate coronavirus anxiety responses are largely characterized by fear of contracting the virus (e.g., Ahorsu et al., 2020; Lee, 2020). An appropriate level of health anxiety facilitates adaptive reactions to physical symptoms to prevent and alleviate illness. However, health anxiety that is chronic and/or greater than the severity of the health-related threat may become maladaptive (Taylor, McKay, & Abramowitz, 2012). Health anxiety may also be accompanied by excessive safety behaviors (e.g., Salkovskis, 1991). Although safety behaviors are intended to minimize the risk of illness (e.g., avoidance of contaminants, excessive washing, or overuse of medical supplies), they can also exacerbate distress and functional impairment by preventing the correction of mistaken anxious beliefs (see Helbig-Lang & Petermann, 2010 for a review). Indeed, one recent study found that health anxiety and excessive internet research on the coronavirus is associated with increased coronavirus anxiety (Jungmann & Witthöft, 2020). Thus, identifying additional theoretically informed risk factors that predict coronavirus anxiety and safety behaviors may inform treatment and preventive strategies amidst the pandemic.
It has been theorized that a complex “behavioral immune system” functions to help humans avoid the harmful effects of pathogens (Curtis, de Barra, & Aunger, 2011; Schaller & Duncan, 2007). This system includes facilitated detection of potential infectious pathogens in the environment and pathogens-avoidance behaviors. Evolutionary approaches contend that disgust is mobilized by this system to protect humans from disease (Tybur, Lieberman, & Griskevicius, 2009). There may be individual differences in the extent to which the experience of disgust is deployed as a psychological first line of defense against pathogen threats in the environment. This individual difference process has been operationalized as disgust proneness, a personality trait that consists of two core components, disgust propensity or an individual’s tendency to experience disgust, and disgust sensitivity, an individual’s negative appraisal of a disgust experience (van Overveld, de Jong, Peters, Cavanagh, & Davey, 2006). Disgust proneness may serve an adaptive function by facilitating avoidance of stimuli that present risk for uncleanliness, contamination, and disease. However, this trait has also been implicated as a risk factor for anxiety-related disorders characterized by contamination symptoms (Olatunji, Williams, Lohr, & Sawchuk, 2005) and has been shown to predict excessive health anxiety symptoms (e.g., Thorpe, Patel, & Simonds, 2003; Davey & Bond, 2006; Fan & Olatunji, 2013), further supporting a functional link between disgust and disease avoidance. Disgust proneness may also confer risk for excessive coronavirus anxiety. Consistent with this view, disgust proneness was correlated with swine flu anxiety during the swine flu pandemic (Wheaton et al., 2012).
Although those high in disgust proneness may be more likely to experience elevated anxiety related to the coronavirus pandemic, it is unknown whether this effect may be impacted by features of an individual’s current context. One such contextual feature is perceived stress. Data from China suggest that nearly 30% of the general population reported experiencing moderate to severe levels of distress in the early stages of the pandemic (Qiu et al., 2020; Wang et al., 2020). The coronavirus pandemic has also been a significant source of stress for reasons extending beyond fears of infection. Indeed, economic instability due to loss of work, difficulties balancing childcare and work responsibilities while working from home, and diminished social support due to social distancing may contribute to psychosocial stress. Importantly, there may also be differences in the amount of stress experienced given variability in the extent to which the individual perceives the stress as uncontrollable, unpredictable, and severe, and deems coping resources as insufficient. Consistent with a diathesis-stress model (Monroe & Simons, 1991), perceived stress may amplify the effects of an underlying diathesis, such as disgust proneness. Though research on predictors of mental health during the coronavirus is nascent, one study found that increased stress during the pandemic was associated with maladaptive coping strategies, including behavioral disengagement and substance use, among adults with disabilities and chronic conditions (Umucu, Lee, & Lee, 2020), and another study found higher resilience, or the ability to effectively cope with stress, is associated with lower anxiety during the pandemic (Liu et al., 2020). Together these findings suggest that perceived stress may be an important process that modulates the effect of disgust proneness on coronavirus anxiety and safety behaviors.
The identification of predictors of coronavirus-related anxiety responses is crucial to effectively address mental health issues during the pandemic. Disgust proneness may be conceptualized as a diathesis, or predisposition, that interacts with the individual's subsequent stress response to produce maladaptive responses during the pandemic. Thus, the diathesis–stress model can be a useful framework for exploring how pre-existing traits (diatheses) interact with environmental influences (stressors) to produce excessive coronavirus-related anxiety responses. Accordingly, the present study examines the relations between disgust proneness, perceived stress, and coronavirus-related anxiety and safety behaviors in a sample of adults who were assessed in 2016 and were re-contacted in the early stages of the coronavirus pandemic in the United States. It was hypothesized that pre-pandemic disgust proneness would predict increases in coronavirus anxiety and safety behaviors during the pandemic, and those with high current perceived stress and high disgust proneness 4 years prior to the pandemic would report the highest coronavirus anxiety and safety behaviors.
2. Methods
2.1. Participants
The sample consisted of adults who completed a 2016 survey study on anxiety-related symptoms who were re-contacted to participate in the present study (N = 360). The 2016 sample included adults aged 18–65 who were recruited for a survey study related to sleep and anxiety symptoms (N = 1262). Of the 2016 sample, 28.5% participated when re-contacted. The sample was 88.3 % female with a mean age of 47.53 (SD = 13.42) at follow-up, ranging from 23 to 69. The ethnicity composition was as follows: White (n = 324; 90.5%), African American (n = 9; 2.5%), Asian (n = 6; 1.7 %), Hispanic/Latino (n = 13; 3.6%), Other (n = 6; 1.7%). Information on state of residence and corresponding number of COVID-19 cases can be found in Table 1 .
Table 1.
State of residence of the study sample and number of COVID-19 cases in each state on 4/1/20 (N = 360).
| State of residence | n (%) | Number of cases on 4/1/20 |
|---|---|---|
| New York | 35 (9.7) | 83948 |
| Ohio | 33 (9.2) | 2547 |
| California | 24 (6.7) | 9399 |
| Tennessee | 20 (5.6) | 2933 |
| Florida | 19 (5.3) | 6956 |
| Maryland | 17 (4.7) | 1986 |
| North Carolina | 15 (4.2) | 1675 |
| Oregon | 13 (3.6) | 736 |
| Kentucky | 11 (3.1) | 632 |
| Massachusetts | 11 (3.1) | 7738 |
| Minnesota | 11 (3.1) | 689 |
| Georgia | 10 (2.8) | 4638 |
| Virginia | 10 (2.8) | 1483 |
| Washington | 10 (2.8) | 1608 |
| Colorado | 9 (2.5) | 2982 |
| Michigan | 9 (2.5) | 9315 |
| South Carolina | 9 (2.5) | 1293 |
| Utah | 9 (2.5) | 888 |
| Illinois | 8 (2.2) | 6980 |
| Iowa | 8 (2.2) | 547 |
| Pennsylvania | 8 (2.2) | 6009 |
| Texas | 8 (2.2) | 4355 |
| Missouri | 7 (1.9) | 1607 |
| Indiana | 6 (1.7) | 2564 |
| Alabama | 5 (1.4) | 1060 |
| Arkansas | 5 (1.4) | 590 |
| Wisconsin | 5 (1.4) | 1556 |
| Arizona | 4 (1.1) | 1530 |
| New Jersey | 4 (1.1) | 22255 |
| Connecticut | 3 (0.8) | 3557 |
| Oklahoma | 3 (0.8) | 721 |
| Kansas | 2 (0.6) | 485 |
| Maine | 2 (0.6) | 303 |
| Mississippi | 1 (0.3) | 1073 |
| Nevada | 1 (0.3) | 1279 |
| New Hampshire | 1 (0.3) | 367 |
| New Mexico | 1 (0.3) | 340 |
| West Virginia | 1 (0.3) | 191 |
| Wyoming | 1 (0.3) | 130 |
2.2. Measures
2.2.1. Coronavirus Anxiety Inventory (CAI)
The CAI is a 9-item self-report measure of fear related to the coronavirus pandemic (items are listed in Table 2 ). The CAI was adapted for this study from a similar measure of Ebola-related fear, the Ebola Fear Inventory (EFI; Blakey et al., 2015). In previous research, the EFI demonstrated small to medium, significant correlations with measures of disgust and contamination concerns (Blakey et al., 2015). Items on the CAI are rated on a Likert scale from 1 (not at all) to 5 (very much), and higher scores indicate higher coronavirus fear. The CAI demonstrated adequate internal consistency (α = 0.74) at time 2.
Table 2.
Items on the Coronavirus Anxiety Inventory (CAI) and Coronavirus Safety Behaviors Checklist (CVSBC).
| Scale | Instructions | Item |
|---|---|---|
| Coronavirus Anxiety Inventory (CAI) | For the next set of questions, please answer based on your thoughts and feelings about the 2020 coronavirus (COVID-19). | 1. To what extent are you concerned about the coronavirus? |
| 2. How likely is it that you could become infected with the coronavirus? | ||
| 3. How likely is it that someone you know could become infected with the coronavirus? | ||
| 4. How quickly do you believe contamination from the coronavirus is spreading in the U.S.? | ||
| 5. How much exposure have you had to information about the coronavirus? | ||
| 6. If you did become infected with the coronavirus, to what extent are you concerned that you will be severely ill? | ||
| 7. To what extent has the threat of the coronavirus influenced your decisions to be around people? | ||
| 8. To what extent has the threat of the coronavirus influenced your travel plans? | ||
| 9. To what extent has the threat of the coronavirus influenced your use of safety behaviors (e.g., hand sanitizer)? | ||
| Coronavirus Safety Behavior Checklist (CSBC) | Please rate how much you have done each activity below related to concerns about the coronavirus (COVID-19). | 1. Washing your hands |
| 2. Using hand sanitizer | ||
| 3. Checking the internet for information on the coronavirus | ||
| 4. Seeking reassurance from friends/family | ||
| 5. Seeking reassurance from a medical professional | ||
| 6. Avoiding certain places | ||
| 7. Avoiding touching things | ||
| 8. Avoiding people | ||
| 9. Wearing a mask | ||
2.2.2. Coronavirus Safety Behavior Checklist (CSBC)
The CSBC is a 9-item self-report measure of engagement in behaviors to prevent contracting coronavirus (items are listed in Table 2). The CSBC was adapted for this study from a similar measure of Ebola-related safety behaviors, the Ebola Safety Behaviors Checklist (Blakey et al., 2015). In previous research, the EFI demonstrated small to medium, significant correlations with measures of disgust and contamination concerns (Blakey et al., 2015). Items on the CSBC are rated on a Likert scale from 0 (none) to 10 (extreme amount), and higher scores indicate higher engagement in coronavirus-related safety behaviors. The CSBC demonstrated adequate internal consistency (α = 0.78) at time 2.
2.2.3. Disgust Propensity and Sensitivity Scale-Revised (DPSS-R; van Overveld et al., 2006)
The DPSS-R is a 16-item self-report measure of the tendency to experience disgust in various contexts (i.e., disgust proneness). Items on the DPSS-R are rated on a Likert scale from 1 (never) to 5 (always), and higher scores indicate increased disgust propensity. The DPSS-R demonstrated good internal consistency (α = 0.90) at time 1.
2.2.4. Perceived Stress Scale (PSS; Cohen, Kamarck, & Memelstein, 1983)
The PSS is a 10-item self-report measure of the degree to which an individual perceives their life to be unpredictable, uncontrollable, and overburdened in the past month. Items on the PSS are rated on a Likert scale from 0 (never) to 4 (very often), and higher scores indicate increased stress. The PSS demonstrated adequate internal consistency (α = .89) at time 2.
2.3. Procedure
Participants for the 2016 study were recruited through ResearchMatch, a national health volunteer registry that was created by several academic institutions and supported by the U.S. National Institutes of Health as part of the Clinical Translational Science Award (CTSA) program. ResearchMatch has a large population of volunteers who have consented to be contacted by researchers about health studies for which they may be eligible. Participants were re-contacted with the option to enroll in the present study on April 1, 2020, and the survey remained open for 7 days. Participants were compensated with a $25 gift card drawing for both time points. Study data were collected and managed using REDCap (Research Electronic Data Capture) hosted at Vanderbilt University (Harris et al., 2009). REDCap is a secure, web-based application designed to support data capture for research studies and is supported by UL1 TR000445 from NCATS/NIH. Data on cumulative COVID-19 cases on April 1, 2020 in each state was collected from https://outbreak.info). Review and approval for the 2016 study and the follow-up and all procedures was obtained from the Vanderbilt University Institutional Review Board.
2.4. Data analytic strategy
Data analysis was conducted in SPSS 26. Prior to data analysis, for scale totals with one item missing, mean imputation was used to replace the missing item. Measures with more than one missing item were considered missing and not included in analysis. Two hierarchical linear regression models were tested to examine the predictive effect of pre-pandemic disgust proneness on coronavirus fear and safety behaviors, respectively. Number of COVID-19 cases by state (i.e., the number of COVID-19 cases in a given participant’s state on 4/1/20) was included as a covariate to control for relative risk of exposure to coronavirus. Two moderation models were tested using the PROCESS macro (Hayes, 2017) to examine whether current stress level moderated the relation between pre-pandemic disgust proneness and coronavirus fear and safety behaviors, respectively, controlling for number of COVID-19 cases by state. Predictor variables were mean-centered prior to analysis. Significant interactions were probed with both a simple slopes analysis (Aiken & West, 1991) and regions of significance analysis using the Johnson-Neyman technique (Johnson & Neyman, 1936).
3. Results
3.1. Descriptive statistics and associations between study variables
Descriptive statistics and associations between study variables are shown in Table 3 . Pre-pandemic disgust proneness demonstrated small, significant, and positive associations with current stress and coronavirus fear and safety behaviors.
Table 3.
Descriptive statistics and correlations for study measures (N = 360).
| Measure | 1. | 2. | 3. | 4. | 5. |
|---|---|---|---|---|---|
| 1. Pre DPSSR | -- | ||||
| 2. PSS | .25* | -- | |||
| 3. CAI | .12* | .15* | -- | ||
| 4. CSBC | .19* | .17* | .65* | -- | |
| 5. Cases 4/1 | .01 | .07 | .03 | .03 | -- |
| M | 33.45 | 17.93 | 26.95 | 50.70 | 11,456.96 |
| SD | 10.07 | 7.14 | 4.97 | 14.37 | 24,094.26 |
| Range | 23−69 | 3−40 | 11−36 | 0−90 | 130−83,948 |
Note. Pre DPSSR = pre-pandemic Disgust Propensity and Sensitivity Scale-Revised; PSS = Perceived Stress Scale; CAI = Coronavirus Anxiety Inventory; CSBC = Coronavirus Safety Behavior Checklist; Cases 4/1 = number of COVID-19 cases in a participant’s state on 4/1/20.
p < .01.
3.2. Effects of pre-pandemic disgust proneness on responses to the coronavirus pandemic
3.2.1. Coronavirus anxiety
Number of COVID-19 cases by state did not significantly contribute to the model, F(1,355) = .263, p = .61. Introducing pre-pandemic disgust proneness to the model explained an additional 1.2 % of the variance in coronavirus anxiety, and the R 2 change was significant (p < .05). When number of COVID-19 cases by state and pre-pandemic disgust proneness were included in the model, pre-pandemic disgust predicted a small increase in coronavirus anxiety, B = .15, β = .11, p < .05. See Table 4 for the results of the regression model. Two exploratory follow-up models testing disgust propensity and sensitivity as predictors revealed that pre-pandemic disgust propensity but not sensitivity individually predicted coronavirus anxiety (p < .05).
Table 4.
Model coefficients for the hypothesized models predicting coronavirus anxiety and safety behaviors from pre-pandemic disgust, controlling for number of COVID-19 cases by state (N = 360).
| Outcome |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| CAI |
CSBC |
|||||||||
| Predictor | B | SE | β | t | p | B | SE | β | t | p |
| Step 1 | ||||||||||
| Cases 4/1 | <.001 | <.001 | .03 | .51 | .61 | <.001 | <.001 | .03 | .47 | .64 |
| Step 2 | ||||||||||
| Cases 4/1 | <.001 | <.001 | .03 | .48 | .63 | <.001 | <.001 | .02 | .44 | .66 |
| Pre DPSSR | .06 | .03 | .11 | 2.09 | <.05 | .27 | .07 | .19 | 3.57 | <.001 |
Note. Pre DPSSR = pre-pandemic Disgust Propensity and Sensitivity Scale-Revised; CAI = Coronavirus Anxiety Inventory; CSBC = Coronavirus Safety Behavior Checklist; Cases 4/1 = number of COVID-19 cases in a participant’s state on 4/1/20.
3.2.2. Coronavirus safety behaviors
Number of COVID-19 cases by state did not significantly contribute to the model, F(1,357) = .22, p = .64. Introducing pre-pandemic disgust proneness to the model explained an additional 3.5 % of the variance in coronavirus safety behaviors, and the R 2 change was significant (p < .001). When number of COVID-19 cases by state and pre-pandemic disgust proneness were included in the model, pre-pandemic disgust proneness predicted a small increase in coronavirus safety behaviors, B = .27, β = .19, p < .001. See Table 4 for the results of the regression model. Two exploratory follow-up models testing disgust propensity and sensitivity as predictors revealed that pre-pandemic disgust propensity and sensitivity predicted coronavirus safety behaviors (p’s < .05).
3.3. Moderation by current stress level
3.3.1. Coronavirus anxiety
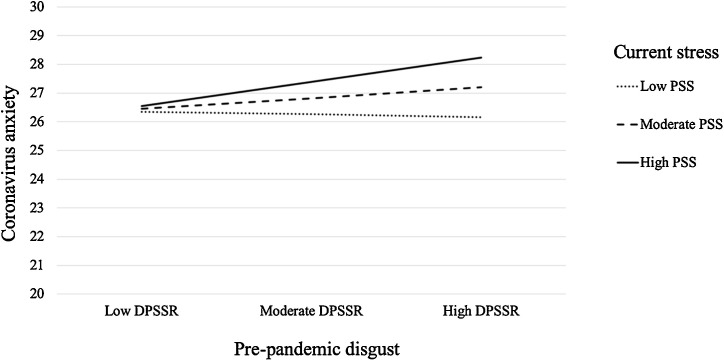
There was a trend-level interaction between pre-pandemic disgust proneness and current stress level to predict coronavirus anxiety, ΔR 2 = .01, F = 3.08, p = .08 (see Table 5 ). Conditional effects analysis revealed that there was no significant relation between pre-pandemic disgust proneness and coronavirus fear at low and medium levels of current stress (p’s > .05). However, at high levels of current stress, there was a significant, positive relation between pre-pandemic disgust proneness and coronavirus anxiety, B = .08, t = 2.36, p < .05 (see Fig. 1 ). A regions of significance analysis identified 21.53 as the score on the PSS at which the relation between pre-pandemic disgust proneness and coronavirus anxiety becomes significant. That is, those with current PSS scores below 21.53 exhibited no link between pre-pandemic disgust proneness and coronavirus anxiety; in contrast, for those with current PSS scores of 21.53 or higher, coronavirus anxiety increase with increasing pre-pandemic disgust proneness.
Table 5.
Model coefficients for the hypothesized moderations between pre-pandemic disgust and current stress to predict coronavirus anxiety and safety behaviors (N = 360).
| Y1 (CAI) |
Y2 (CSBC) |
|||||
|---|---|---|---|---|---|---|
| Predictor | Coeff | SE | p | Coeff | SE | p |
| X (Pre DPSSR) | .04 | .03 | .17 | .20 | .08 | <.05 |
| M (PSS) | .08 | .04 | <.05 | .25 | .11 | <.05 |
| Pre DPSSR X PSS | .01 | .004 | .08 | .03 | .01 | <.05 |
| Cov (Cases 4/1) | <.001 | <.001 | .67 | <.001 | <.001 | .68 |
| ΔR2 | .01 | .08 | .02 | <.05 | ||
| Constant | 26.77 | .30 | <.001 | 50.09 | .85 | <.001 |
| R2 = .04 | R2 = .07 | |||||
| F(4,348) = 3.35, p < .05 | F(4,352) = 6.29, p < .001 | |||||
Note. X = predictor variable; M = moderator variable; Cov = covariate; Pre DPSSR = pre-pandemic Disgust Propensity and Sensitivity Scale-Revised; PSS = Perceived Stress Scale; CAI = Coronavirus Anxiety Inventory; CSBC = Coronavirus Safety Behavior Checklist; Cases 4/1 = number of COVID-19 cases in a participant’s state on 4/1/20.
Fig. 1.
Simple regression slopes of pre-pandemic disgust predicting coronavirus anxiety at values of current stress, controlling for number of COVID-19 cases by state. Pre-pandemic disgust and current stress were mean-centered prior to analysis, such that low, medium, and high represent the sample mean +/- one standard deviation.
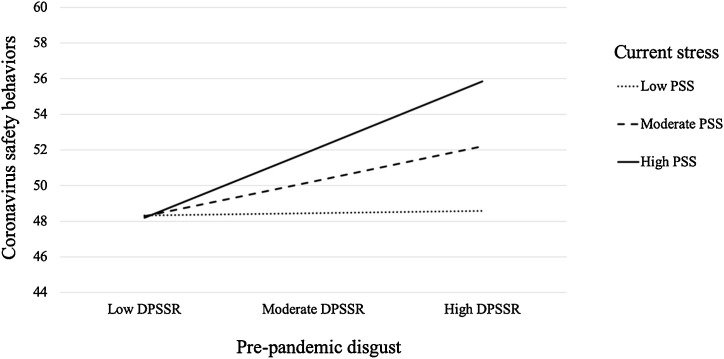
3.3.2. Coronavirus safety behaviors
There was a significant interaction between pre-pandemic disgust proneness and current stress level to predict coronavirus safety behaviors, ΔR 2 = .02, F = 6.06, p < .05 (see Table 5). Conditional effects analysis revealed that there was no significant relation between pre-pandemic disgust proneness and coronavirus safety behaviors at low levels of current stress (p > .05). However, there were significant, positive relations between pre-pandemic disgust proneness and coronavirus safety behaviors at medium, B = .20, t = 2.54, p < .05, and high levels of current stress B = .38, t = 3.78, p < .001 (see Fig. 2 ). A regions of significance analysis identified 17.79 as the score on the PSS at which the relation between pre-pandemic disgust proneness and coronavirus safety behaviors becomes significant. That is, those with current PSS scores below 17.79 exhibited no link between pre-pandemic disgust proneness and coronavirus safety behaviors; in contrast, for those with current PSS scores of 17.79 or higher, coronavirus safety behaviors increase with increasing pre-pandemic disgust proneness.
Fig. 2.
Simple regression slopes of pre-pandemic disgust predicting coronavirus safety behaviors at values of current stress, controlling for number of COVID-19 cases by state. Pre-pandemic disgust and current stress were mean-centered prior to analysis, such that low, medium, and high represent the sample mean +/- one standard deviation. Importantly, this effect is at trend-level.
4. Discussion
The present study examined the predictive effect of pre-pandemic disgust proneness on coronavirus anxiety and safety behaviors during the pandemic, as well as the moderating effect of current levels of perceived stress. Results of the regression models found that pre-pandemic disgust proneness significantly predicted increases in both coronavirus anxiety and safety behaviors, controlling for number of COVID-19 cases by state. These findings replicate previous studies implicating disgust proneness as one factor associated with responses to previous viral outbreaks, including the swine flu pandemic (Wheaton et al., 2012) and the Ebola (Blakey et al., 2015) and zika outbreaks (Blakey & Abramowitz, 2017). Evidence for an effect of prior disgust proneness on coronavirus fear and safety behaviors is also consistent with a recent study showing a concurrent association between increased disgust proneness and fear of contracting the coronavirus (Mckay, Yang, Elhai, & Asmundson, 2020), and extends these findings by showing a predictive effect over 4 years. A limitation of the extant research in this area is the utilization of cross-sectional samples, thereby making it unclear if the observed relations between disgust and responses to viral outbreaks were due to acutely elevated disgust in response to said outbreaks (i.e., state disgust). The present study suggests that disgust proneness in the absence of a disgust-relevant threat (i.e., pre-pandemic trait disgust) contributes to an elevated anxiety response during the coronavirus pandemic. In other words, disgust proneness may be one individual difference factor that confers vulnerability for experiencing increased anxiety and engaging in excessive safety behaviors during the coronavirus pandemic.
The present findings show that heightened disgust proneness before the pandemic results in an increased use of protective behaviors in the midst of the pandemic. This likely reflects the adaptive functions of the complex “behavioral immune system” that functions to help humans avoid contacts with pathogens (Curtis et al., 2011). Indeed, it has been posited that experiencing disgust is a primary mechanism that is employed by the “behavioral immune system” to facilitate disease avoidance (Olatunji, Haidt, McKay, & David, 2008). It is important to note that disgust levels will also increase, as part of the “behavioral immune system”, during pandemics given the threat of infection. This heightened disgust may then facilitate adaptive avoidance of situations and stimuli where contamination is likely to occur. One mechanism may be that those high in pre-existing disgust proneness (trait) may experience even higher levels of (state) disgust during the pandemic which then motivates the use of more safety behaviors. Although this process is largely adaptive, disgust proneness has been found to contribute to excessive safety behavior usage in conditions like contamination-based OCD (e.g., Phillips, Fahy, David, & Senior, 1998; Woody & Teachman, 2000), as well as illness anxiety disorder (Davey & Bond, 2006).
Heightened pre-pandemic disgust proneness may contribute to a response to the pandemic that exceeds that which is evolutionarily adaptive. This may occur when those with elevated pre-pandemic disgust proneness negatively appraise disgust-relevant stimuli and/or situations (e.g., “I will get sick and die if a stranger sneezes in close proximity to me,” “I would not be able to tolerate the disgust associated with touching something a stranger has touched”) in a way that exacerbates a fear response to the coronavirus pandemic. Indeed, research has previously shown that disgust is significantly associated with both danger and germ spread appraisals (Dorfan & Woody, 2011). Safety behaviors are actions performed to prevent, escape, or minimize feared catastrophes and/or associated distress. Safety behaviors become maladaptive when individuals misattribute their safety to the behavior itself, rather than the low probability of the feared outcome (e.g., “I am only safe because I washed my hands,” rather than “it is unlikely I will get sick;” Salkovskis, 1991). Heightened pre-pandemic disgust proneness may also contribute to usage of safety behaviors that exceeds that which is adaptive. Of note, safety behaviors are functionally related to anxious beliefs and are logical, if unnecessary (Blakey & Abramowitz, 2016). For those high in disgust proneness, there may be a tendency to engage in safety behaviors (e.g., excessive handwashing) when such protective acts are not required. This may subsequently facilitate safety misattributions that maintain anxiety during the pandemic. This view is consistent with previous research indicating disgust proneness significantly mediates the relationship between contamination-related obsessive-compulsive symptoms and beliefs (e.g., overestimations of threat) and Swine Flu behaviors and fear (Brand et al., 2013). In addition to disease avoidance, individuals may engage in safety behaviors to mitigate feelings of disgust and distress during a pandemic.
Moderation analyses also revealed that current perceived stress significantly interacted with pre-pandemic disgust proneness to predict coronavirus safety behaviors, while the interactive effect for coronavirus anxiety was at trend level. Specifically, increased pre-pandemic disgust proneness predicted increased coronavirus safety behaviors for those reporting high and medium current perceived stress. In contrast, those reporting low current perceived stress did not demonstrate a significant relation between pre-pandemic disgust proneness and coronavirus safety behaviors. Similarly, though at trend level, increased pre-pandemic disgust proneness predicted increased coronavirus anxiety for those reporting high, but not medium or low, current perceived stress. These findings are consistent with a diathesis-stress framework, such that the vulnerability for an anxiety response to the coronavirus pandemic conferred by elevated pre-pandemic disgust proneness is “activated” by stress. Likewise, when perceived stress is low, pre-pandemic disgust proneness has no impact on response to the pandemic. Indeed, a recent study found heightened COVID-19 distress is associated with difficulties coping during the pandemic (Taylor et al., 2020). One of the unanswered questions in the literature is why people vary in the degree to which they experience disgust (Tybur, Cinar, Karinen, & Perone, 2018). These findings suggest that perceived stress may contribute to variability in disgust proneness and this variability may effect subsequent coronavirus fear and safety behaviors. This diathesis-stress approach offers preliminary insight into who may be most vulnerable to a disproportionate response to the coronavirus pandemic.
The present findings may also have implications for clinical intervention during the pandemic. Clinicians may consider assessing for disgust proneness and stress to facilitate identifying those who may be experiencing particularly high distress. Further, stress reduction interventions may be beneficial for off-setting the detrimental effects of pre-pandemic vulnerability factors, such as disgust proneness. However, the findings of the present study must be considered in light of the study limitations. First, the sample was largely white and female, which limits generalizability to various demographic groups. Second, this study used self-report instruments that may be incomplete measures of disgust proneness, stress, and coronavirus fear and safety behaviors, such that these subjective responses may diverge from responses to clinical interviews or behavioral tasks. Third, although the longitudinal design establishes the temporal precedence of disgust proneness, the lack of manipulation of disgust limits causal interpretations. Finally, given the unprecedented nature of the pandemic, the level of coronavirus fear and safety behaviors that can be considered maladaptive or disproportionate is presently unknown. Thus, future research is needed to identify thresholds at which the distress response to the coronavirus is clinically significant and whether disgust proneness contributes to exceeding such a threshold.
Funding
This work was supported by the National Institute of Mental Health of the National Institutes of Health [F31MH113271]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Compliance with ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/ or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This article does not contain any studies with animals performed by any of the authors. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Contributions
Ms. Cox collected the data, performed the statistical analysis, and contributed to drafts of the manuscript. Ms. Jessup contributed to drafts of the manuscript. Mr. Luber contributed to drafts of the manuscript and data entry. Dr. Olatunji contributed to study design, oversaw data collection, and assisted with statistical analysis and manuscript preparation. All authors contributed to and have approved of the final manuscript.
Declaration of Competing Interest
The authors report no declarations of interest.
References
- Ahorsu, D. K., Lin, C.-Y., Imani, V., Saffari, M., Griffiths, M. D., & Pakpour, A. H. (in press). The Fear of COVID-19 Scale: Development and initial validation. Int J Mental Health Addict. [DOI] [PMC free article] [PubMed]
- Aiken L.S., West S.G. Sage Publications, Inc.; 1991. Multiple regression: Testing and interpreting interactions. [Google Scholar]
- Blakey S.M., Abramowitz J.S. The effects of safety behaviors during exposure therapy for anxiety: Critical analysis from an inhibitory learning perspective. Clinical Psychology Review. 2016;49:1–15. doi: 10.1016/j.cpr.2016.07.002. [DOI] [PubMed] [Google Scholar]
- Blakey S.M., Abramowitz J.S. Psychological predictors of health anxiety in response to the zika virus. Journal of Clinical Psychology in Medical Settings. 2017;24:270–278. doi: 10.1007/s10880-017-9514-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blakey S.M., Reuman L., Jacoby R.J., Abramowitz J.S. Tracing “fearbola”: Psychological predictors of anxious responding to the threat of Ebola. Cognitive Therapy and Research. 2015;39:816–825. doi: 10.1007/s10608-015-9701-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand J., McKay D., Wheaton M.G., Abramowitz J.S. The relationship between obsessive compulsive beliefs and symptoms, anxiety and disgust sensitivity, and Swine Flu fears. Journal of Obsessive-Compulsive and Related Disorders. 2013;2:200–206. doi: 10.1016/j.jocrd.2013.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Memelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Curtis V., de Barra M., Aunger R. Disgust as an adaptive system for disease avoidance behaviour. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 2011;366(1563):389–401. doi: 10.1098/rstb.2010.0117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey G.C.L., Bond N. Using controlled comparisons in disgust psychopathology research: The case of disgust, hypochondriasis and health anxiety. Journal of Behavior Therapy and Experimental Psychiatry. 2006;37:4–15. doi: 10.1016/j.jbtep.2005.09.001. [DOI] [PubMed] [Google Scholar]
- Dorfan N.M., Woody S.R. Danger appraisals as prospective predictors of disgust and avoidance of contaminants. Journal of Social and Clinical Psychology. 2011;30:105–132. [Google Scholar]
- Fan Q., Olatunji B.O. Individual differences in disgust sensitivity and health-related avoidance: Examination of specific associations. Personality and Individual Differences. 2013;55:454–458. doi: 10.1016/j.paid.2013.04.007. [DOI] [Google Scholar]
- Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap): A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010.Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A.F. 2nd ed. Guilford Press; 2017. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. [Google Scholar]
- Helbig-Lang S., Petermann F. Tolerate or eliminate? A systematic review on the effects of safety behavior across anxiety disorders. Clinical Psychology: Science and Practice. 2010;17:218–233. doi: 10.1111/j.1468-2850-2010.01213.x. [DOI] [Google Scholar]
- Johnson P.O., Neyman J. Tests of certain linear hypotheses and their application to some educational problems. Statistical Research Memoirs. 1936;1:57–93. [Google Scholar]
- Jungmann S.M., Witthöft M. Health anxiety, cyberchondria, and coping in the current COVID-19 pandemic: Which factors are related to coronavirus anxiety? Journal of Anxiety Disorders. 2020;73 doi: 10.1016/j.janxdis.2020.102239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A. Coronavirus Anxiety Scale: A brief mental health screener for COVID-19 related anxiety. Death Studies. 2020;44:393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- Li R., Pei S., Chen B., Song Y., Zhang T., Yang W.…Shaman J. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2) Science (80-.) 2020;368:489–493. doi: 10.1126/science.abb3221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Tin G., Wong F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research. 2020:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mckay D., Yang H., Elhai J., Asmundson G. Anxiety regarding contracting COVID-19 related to interoceptive anxiety sensations: The moderating role of disgust propensity and sensitivity. Journal of Anxiety Disorders. 2020:102233. doi: 10.1016/j.janxdis.2020.102233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monroe S.M., Simons A.D. Diathesis-stress theories in the context of life stress research: Implications for the depressive disorders. Psychological Bulletin. 1991;110:406–425. doi: 10.1037/0033-2909.110.3.406. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Williams N.L., Lohr J.M., Sawchuk C.N. The structure of disgust: Domain specificity in relation to contamination ideation and excessive washing. Behaviour Research and Therapy. 2005;43(8):1069–1086. doi: 10.1016/j.brat.2004.08.002. [DOI] [PubMed] [Google Scholar]
- Olatunji B.O., Haidt J., McKay D., David B. Core, animal reminder, and contamination disgust: Three kinds of disgust with distinct personality, behavioral, physiological, and clinical correlates. Journal of Research in Personality. 2008;42:1243–1259. doi: 10.1016/j.jrp.2008.03.009. [DOI] [Google Scholar]
- Disgust: The forgotten emotion of psychiatry [Editorial] Phillips M.L., Fahy T., David A.S., Senior C., editors. The British Journal of Psychiatry. 1998;172:373–375. doi: 10.1192/bjp.172.5.373. [DOI] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID‐ 19 epidemic: Implications and policy recommendations. General Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salkovskis P.M. The importance of behavior in the maintenance of anxiety and panic: A cognitive account. Behavioural Psychotherapy. 1991;19:6–19. doi: 10.1017/S0141347300011472. [DOI] [Google Scholar]
- Schaller M., Duncan L.A. The behavioral immune system: Its evolution and social psychological implications. In: Forgas J.P., Haselton M.G., von Hippel W., editors. Sydney symposium of social psychology. Evolution and the social mind: Evolutionary psychology and social cognition. Routledge/Taylor & Francis Group; 2007. pp. 293–307. [Google Scholar]
- Schimmenti A., Billieux J., Starcevic V. The four hoursemen of fear: An integrated model of understanding fear experiences during the COVID-19 pandemic. Clinical Neuropsychiatry. 2020;17:41–45. doi: 10.36131/CN20200202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor S., McKay D., Abramowitz J.S. Hypochondriasis and health-related anxiety. In: Sturmey P., Hersen M., editors. Handbook of evidence-based practice in clinical psychology, vol 2: Adult disorders; handbook of evidence-based practice in clinical psychology, vol 2: Adult disorders. John Wiley & Sons Inc; Hoboken, NJ: 2012. (pp. 603-619, Chapter xx, 747 Pages) [Google Scholar]
- Taylor, S., Landry, C. A., Paluszek, M. M., Fergus, T. A., McKay, D., Asmundson, G. J. G., in press. COVID stress syndrome: Concept, structure, and correlates. Depress Anx. [DOI] [PMC free article] [PubMed]
- Thorpe S.J., Patel S.P., Simonds L.M. The relationship between disgust sensitivity, anxiety, and obsessions. Behaviour Research and Therapy. 2003;41:1397–1409. doi: 10.1016/S0005-7967(03)00058-5. [DOI] [PubMed] [Google Scholar]
- Tybur J.M., Lieberman D., Griskevicius V. Microbes, mating, and morality: Individual differences in three functional domains of disgust. Journal of Personality and Social Psychology. 2009;97(1):103–122. doi: 10.1037/a0015474. [DOI] [PubMed] [Google Scholar]
- Tybur J.M., Cinar C., Karinen A.K., Perone P. Why do people vary in disgust? Philosophical Transactions of the Royal Society B: Biological Sciences. 2018;373:20170204. doi: 10.1098/rstb.2017.0204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umucu E., Lee B., Lee B. Examining the impact of COVID-19 on stress and coping strategies in individuals with disabilities and chronic conditions. Rehabilitation Psychology. 2020;65(3):193–198. doi: 10.1037/rep0000328. [DOI] [PubMed] [Google Scholar]
- van Overveld W.J.M., de Jong P.J., Peters M.L., Cavanagh K., Davey G.C.L. Disgust propensity and disgust sensitivity: Separate constructs that are differentially related to specific fears. Personality and Individual Differences. 2006;41:1241–1252. doi: 10.1016/j.paid.2006.04.021. [DOI] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S.…Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID‐19) epidemic among the general population in China. International Journal of Environmental Research and Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Fabricant L.E., Olatunji B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognitive Therapy and Research. 2012;36:210–218. doi: 10.1007/s10608-011-9353-3. [DOI] [Google Scholar]
- Woody S.R., Teachman B.A. Intersection of disgust and fear: Normative and pathological views. Clinical Psychology: Science and Practice. 2000;7(3):291–311. doi: 10.1093/clipsy/7.3.291. [DOI] [Google Scholar]
- Xie M., Chen Q. Insight into 2019 novel coronavirus: An updated interim review and lessons from SARS-CoV and MERS-CoV. International Journal of Infectious Diseases. 2020;94:119–124. doi: 10.1016/j.ijid.2020.03.071. [DOI] [PMC free article] [PubMed] [Google Scholar]