Abstract
Background
COVID-19 has affected social interaction and healthcare worldwide.
Methods
We examined changes in presentations and referrals to the primary provider of mental health and community health services in Cambridgeshire and Peterborough, UK (population ~0·86 million), plus service activity and deaths. We conducted interrupted time series analyses with respect to the time of UK “lockdown”, which was shortly before the peak of COVID-19 infections in this area. We examined changes in standardized mortality ratio for those with and without severe mental illness (SMI).
Results
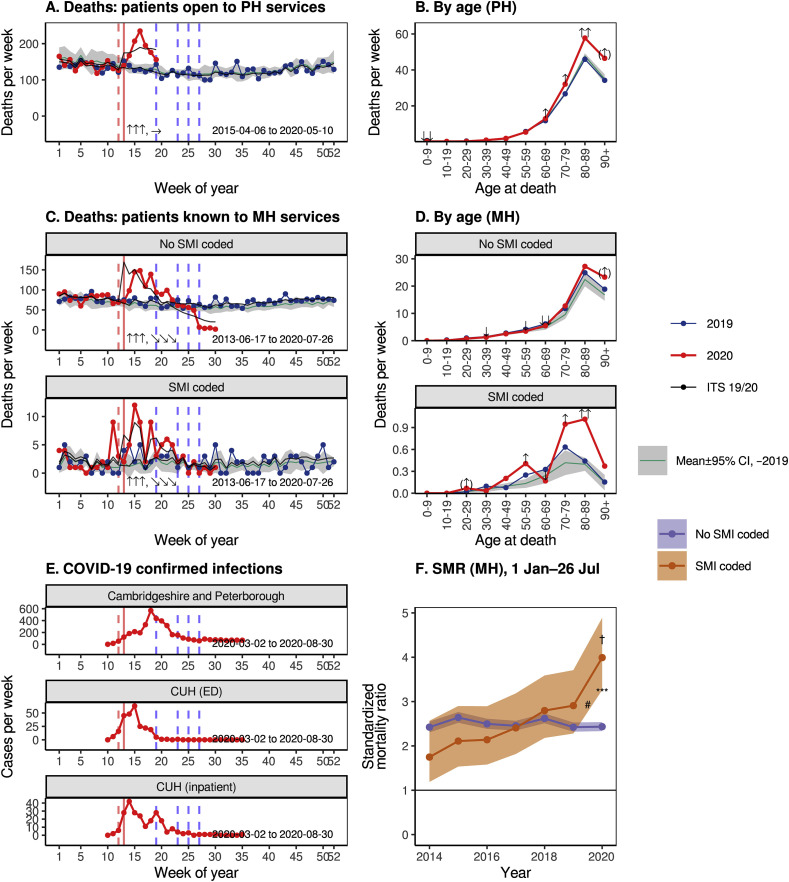
Referrals and presentations to nearly all mental and physical health services dropped at lockdown, with evidence for changes in both supply (service provision) and demand (help-seeking). This was followed by an increase in demand for some services. This pattern was seen for all major forms of presentation to liaison psychiatry services, except for eating disorders, for which there was no evidence of change. Inpatient numbers fell, but new detentions under the Mental Health Act were unchanged. Many services shifted from face-to-face to remote contacts. Excess mortality was primarily in the over-70s. There was a much greater increase in mortality for patients with SMI, which was not explained by ethnicity.
Conclusions
COVID-19 has been associated with a system-wide drop in the use of mental health services, with some subsequent return in activity. “Supply” changes may have reduced access to mental health services for some. “Demand” changes may reflect a genuine reduction of need or a lack of help-seeking with pent-up demand. There has been a disproportionate increase in death among those with SMI during the pandemic.
Keywords: COVID-19/SARS-CoV-2 coronavirus pandemic, Depression, Anxiety, Self-harm, Alcohol and substance misuse, Suicidality, Mortality, Severe mental illness (SMI)
1. Introduction
The COVID-19 pandemic has had profound effects on health services. The UK implemented interpersonal distancing on 2020-03-16 (Prime Minister's Office, 2020a). Its National Health Service (NHS) took steps to release inpatient and critical care capacity from 2020-03-17, including a shift towards remote (videoconferencing and telephone) patient consultations (NHS England and NHS Improvement, 2020). The UK moved to full “lockdown” on 2020-03-23 (Prime Minister's Office, 2020b), legally enforceable thereafter (Hancock, 2020). Partial “unlocking” began in England on 2020-05-10 (Prime Minister's Office, 2020c), and has continued.
The impact of the pandemic on population mental health (MH) is of major interest. The SARS-CoV-2 coronavirus may have direct neurotropic effects in humans: in addition to anosmia/ageusia, COVID-19 has been associated with meningoencephalitis (von Weyhern et al., 2020; Varatharaj et al., 2020) and other neuropsychiatric complications, in which endothelial involvement and bradykinin dysregulation may be important (Varatharaj et al., 2020; Zubair et al., 2020; Romoli et al., 2020; Rogers et al., 2020; Garvin et al., 2020; Roche and Roche, 2020). A broader problem is that the societal response to COVID-19 has had effects with potential for major psychological and psychiatric consequences, including distress in COVID-19 sufferers and their loved ones (including those bereaved); confinement and dramatic reductions in the opportunities for social interaction leading to loneliness; worry about illness and death, which may have adverse psychiatric consequences (Vindegaard and Eriksen Benros, 2020); and changes in healthcare services that may have led to a reduction in support for those with pre-existing mental disorders. Some effects might have occurred in the opposite direction, such as beneficial effect on MH from a society uniting against a “common enemy” (Pridmore et al., 2018). However, to our knowledge, no previous observational study has reported the impact of the pandemic on clinical mental health services (PubMed search for “covid* AND ("mental health" OR psychiatr*) AND "observational study"[pt]”, July 7, 2020). Likewise, no previous study has provided direct evidence of the impact of COVID-19 on mortality for those with severe mental illness (SMI; PubMed search for “covid* AND mortality AND ("serious mental illness" OR "severe mental illness" OR schizophrenia OR schizoaffective OR schizotypal OR delusional OR bipolar OR depression)”, July 7, 2020).
Our objectives were to measure changes in MH and community physical health (PH) service activity and mortality associated with the pandemic and lockdown. We examined population-level changes using data from the single public provider of specialist MH and community PH services to Cambridgeshire and Peterborough (C&P), UK. We examined presentations and referrals to services. We looked for evidence of redirection (e.g. was a reduction in face-to-face attendance associated with increased use of telephone crisis services?) and changes in the type of presentation to MH services (e.g. in anxiety, self-harm, or psychosis). We examined service activity, looking for changes in the nature of service provision (e.g. face-to-face versus remote consultation). Finally, we examined mortality, to establish if there was an excess of deaths in these patient groups, and whether those with severe mental illness (SMI) were at higher risk of dying during the pandemic.
2. METHODS
2.1. Service overview
Cambridgeshire & Peterborough NHS Foundation Trust (CPFT) provides community PH services, psychological therapy services, and all secondary care MH services (including some embedded within primary care) to C&P, which has a population of ~0·86 million (Office for National Statistics, 2020a). It provides MH inpatient facilities in the cities of Cambridge and Peterborough, PH inpatient rehabilitation facilities in Cambridge, Peterborough, Ely, and Wisbech, and Minor Injury Units (MIUs) in Ely, Wisbech, and Doddington. See Supplementary Methods for more details of population demographics, geography, and services.
2.2. Data sources
De-identified data was extracted from CPFT clinical records by CPFT's Information & Performance team and via the CPFT Research Database (NHS research ethics 17/EE/0442; see Supplementary Methods). We obtained data from four clinical records systems (RiO, SystmOne, PCMIS, and Epic; see Supplementary Methods), representing all clinical records systems for CPFT plus one for services provided by CPFT within another Trust (Epic). Data from each system were analysed separately.
2.3. Variables
For MH services, we extracted the following variables, per day:
-
•
Referrals to CPFT teams embedded in primary care. We counted referrals to CPFT's embedded primary care mental health service, and to its Improving Access to Psychological Therapies (IAPT) service, including self-referrals.
-
•
Calls to 111 for MH crises. CPFT provides the NHS 111 MH crisis telephone service. We counted calls and triage psychiatric assessments.
-
•
Referrals to secondary care CPFT teams. We classified teams as (a) child and adolescent mental health (CAMH) teams; (b) community MH teams (CMHTs) for adults; (c) crisis resolution/home treatment teams (CRHTs); (d) adult liaison psychiatry (LP) teams; (e) early intervention in psychosis (EIP) teams; (f) eating disorder teams; (g) other specialist services. See Supplementary Methods for detail.
-
•
Liaison Psychiatry referrals and presenting problems. For CPFT’s LP service at Cambridge University Hospitals (CUH), we counted referrals, split as (a) from the Emergency Department (ED) with its associated Clinical Decision Unit (CDU), and (b) from other wards. When responding to a referral, LP clinicians record the primary reason(s) for referral. We counted presenting problems of (a) alcohol and/or drug use; (b) anxiety; (c) confusion, cognitive problems, requests for assistance with mental capacity assessment, and behavioural disturbance; (d) eating disorders; (e) low mood and suicidal ideation; (f) overdose and other forms of self-harm; (g) psychosis and mood elevation (hypomania/mania).
-
•
Admissions. We counted admissions, discharges, inter-ward transfers, and inpatients per day across MH wards (excluding day-care facilities). We classified admission days as “voluntary” or “detained” according to the patient’s UK Mental Health Act (MHA) status for that day. We classified an admission as a readmission if it began <30 calendar days after a previous discharge for that patient.
-
•
MHA detention. We counted new episodes of detention under the MHA, of all kinds (not individual detentions, i.e. consecutive detention under different sections of the MHA counted as one episode). We counted assessments recorded following police use of section 136 (s136) of the MHA, a police power to take someone suspected of suffering from mental disorder to a place of safety in some circumstances. The data did not cover all detentions under s136 but included those where CPFT provided the place of safety (by far the majority in C&P).
-
•
Documentation. We counted progress note entries by CPFT staff, and binary documents (written by staff or inbound from others), as general measures of activity.
-
•
Appointments/contacts. We counted formally recorded contacts, excluding those marked cancelled, not attended, with a carer (rather than the patient), or where contact with the patient was not explicitly recorded. We split by contact type (telephone versus all other types). Videoconferencing was not recorded as a distinct contact type.
-
•
Deaths. We counted deaths per day. We classified MH patients as having severe mental illness (SMI) or not. Based on the definition of SMI as schizophrenia, schizotypal and delusional disorders, bipolar affective disorder, and severe depression (UK National Institute for Health and Care Excellence, 2016), we looked for a lifetime coded diagnosis of ICD-10 codes F20*, F21*, F22*, F25*, F31*, F32.2, F32.3*, F33.2, and F33.3*. Any under-coding of diagnosis was unmeasured.
For PH services, by day:
-
•
MIU attendees.
-
•
Referrals to children’s and adult services.
-
•
Admissions. Historical daily admission data was not available, so we counted bed-days per month.
-
•
Contacts. We counted contacts by age group (children’s and adult community services) and by contact method (face-to-face or other, e.g. telephone, videoconferencing).
-
•
Deaths. We counted deaths of patients with an open referral to CPFT’s PH services at the time of death.
COVID-19 infection:
-
•
We obtained daily lab-confirmed COVID-19 case rates for Cambridgeshire and Peterborough (Public Health England and NHSX, 2020), by specimen date.
-
•
We counted CUH patients testing positive for COVID-19 for the first time, from anonymised data, where tests were from inpatient wards or the ED.
2.4. Dates
The first date of each available time series is shown in their respective Figures. We used 2020-03-23 (lockdown, week 13) as the event date for interrupted time series (ITS) analysis. We obtained data up to and including the following dates. RiO: 2020-08-09. SystmOne: 2020-05-18 (most data), 2020-05-22 (primary care MH). PCMIS: 2020-05-26. Epic: 2020-08-31 (LP), 2020-08-31 (COVID-19). National data: 2020-08-30.
We truncated the last 7 days of RiO contact data, to allow for delays in recording appointment outcomes (lag estimated). We truncated the last 7 days of SystmOne death data, to allow for delays in death reporting to the NHS Spine (lag estimated), and 14 days of RiO death data, to allow for additional delays in Spine-to-RiO updates. Finally, we truncated all data to the last available full week.
2.5. Service reorganization
A number of services reorganized during this period, influencing activity from the “supply” side (Supplementary Methods).
2.6. Analyses: general
We used R v3.6.2 (R Core Team, 2019). We counted events per week according to the ISO-8601 standard, excluding week 53. For time series data, we conducted ITS analyses using a negative binomial generalized linear model (Ripley et al., 2020) (falling back to Poisson regression under nonconvergence suggesting lack of overdispersion) with augmented segmented regression. Predictors were: time (overall linear trend, with time = 0 at UK lockdown); event (0 before lockdown and 1 at/afterwards, measuring instantaneous change); time × event (0 before lockdown and time afterwards, measuring a change in slope after lockdown); week (a discrete predictor, to account for seasonal autocorrelation across years or other shorter-term phenomena) (Wagner et al., 2002); year (discrete predictor, to account for nonstationarity across years beyond a linear trend); and an intercept. We did not include a time lag. We show ITS model predictions and report the instantaneous and slope-change effects, with associated significance tests shown in the Figures (α = 0.05).
2.7. Analyses: mortality
We examined age- and sex-standardized metrics for mortality. First, for each year, we calculated the mean number of deaths per week, by age at death in 10-year bands. In each age band, we performed ITS analysis using Gaussian regression with predictors year (linear time trend) and year_is_2020 (step change). This method does not account fully for the number of patients “exposed” to risk except via the linear trend, but was applicable to PH data (for which exposure data was unavailable) and MH data.
Secondly, for MH data, we calculated standardized mortality ratios (SMRs). Within each year, a subject's observation (exposure) period began on 1 January or at the subject’s registration (whichever was later), and ended on the date corresponding to the last data available for 2020 (to avoid comparing e.g. winter/spring 2020 to the whole of previous years). Only subjects registered and alive at some point during that period were considered. The observed death count was 1 if the subject died during that period and 0 otherwise. The expected number of deaths for that subject was taken from national mortality tables (unweighted mean of Cambridge, East Cambridgeshire, Fenland, Huntingdon, Peterborough, and South Cambridgeshire) (Office for National Statistics, 2020b), by sex and age (using the subject’s age on 1 January of each year, up to 90), weighted by the duration of the observation period. Across subjects, the total number of observed (O) and expected (E) deaths was calculated. The SMR is O/E, the standard deviation (SD) of ln(SMR) was taken as 1/√O, and the 95% confidence limits of the SMR as e ln(SMR)±1·96/√O (Rothman et al., 2008).
We calculated SMRs separately for those with and without SMI. We compared SMR pairs by taking the SD of ln(SMR ratio) as √(1/O 1 + 1/O 2) (Rothman et al., 2008). We tested whether any change between 2020 and previous years was different for SMI and non-SMI groups via an ITS analysis across all years, using: negative binomial regression; deaths per thousand exposure years as the dependent variable; ln(expected deaths per thousand exposure years) as an offset (Dalgaard, 2008); predictors of year (linear), year_is_2020 (binary), SMI (binary), SMI × year_is_2020, and an intercept.
Since Black, Asian, and minority ethnic (BAME) groups are at disproportionate hazard compared to White ethnic groups of contracting COVID-19, hospital admission, critical care admission, and death from COVID-19 (UK Government Office for Science, 2020), we also included ethnicity as a predictor (White versus ethnic minorities or unrecorded ethnicity), and its interaction with all combinations of year_is_2020 and SMI.
3. RESULTS
3.1. Presentations and referrals to MH services
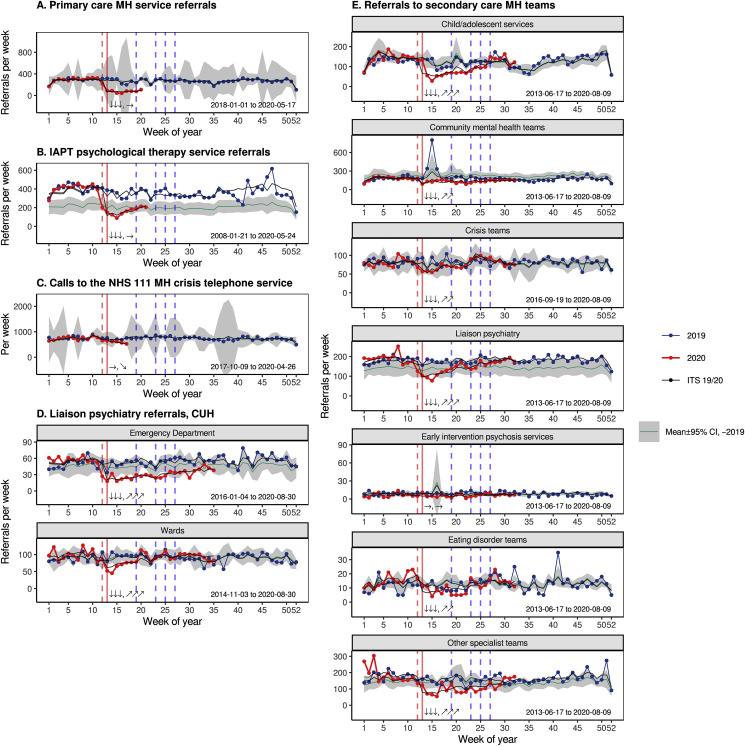
There was a sharp reduction at lockdown in referrals to primary care MH services, psychological therapy, and all secondary care MH teams apart from EIP services (for which there was no significant change), with a subsequent increase towards normal levels for secondary care services (Fig. 1 ). There was a gradual decrease in telephone calls to the NHS 111 MH crisis service (Fig. 1C), and a small immediate drop in triage assessments by that service (p < 0·05) with no significant change thereafter (not shown). LP referrals from wards dropped sharply then gradually increased back to normal (Fig. 1D), likely reflecting the drop in acute hospital inpatient numbers. There was a substantial reduction in LP referrals from the ED followed by a slow increase (Fig. 1D). The changes in referrals to secondary care were proportionally less for patients with SMI than for those without SMI recorded; for example, referrals to crisis teams did not change for those with SMI, and referrals to CMHTs dropped less (Supplementary Results).
Fig. 1.
“Front door” mental health (MH) service activity. (A) Referrals to MH teams embedded in primary care. (B) Referrals (from professionals or patient self-referrals) to CPFT’s IAPT psychological therapy service. (C) Calls from patients to the NHS “111 option 2” mental health crisis telephone service. (D) Referrals to one of CPFT’s Liaison Psychiatry (LP) services, at CUH. (E) Referrals to secondary care MH teams, which may come from outside the Trust (e.g. from general practitioners to community/crisis/specialist teams, or from acute hospital staff to liaison psychiatry) or internally (e.g. from community teams to crisis teams or vice versa). Graphical conventions: The x axis shows week-of-year. The line and ribbon marked “Mean ± 95% CI …” indicate the mean and 95% confidence interval (CI), calculated separately for each week of the year, across all past years available to 2019 inclusive. Weekly data from 2019 to 2020 are shown individually. Vertical lines relate to 2020 and indicate UK social distancing then “lockdown” (red: 16 March, 23 March), followed by phases of “unlocking” in England (blue: 10 May, 1 June, 16 June, 4 July). The “ITS 19/20” lines show predictions from an interrupted time series (see Methods), fitted to data from all years and shown for 2019–2020. ITS effects of interest in relation to UK lockdown (solid vertical red line) are shown textually in the sequence “instantaneous effect, subsequent slope change”, with instantaneous effects shown as up/down arrows (two-tailed; increases ↑↑↑ p < 0·001, ↑↑ p < 0·01, ↑ p < 0·05; → no significant change; decreases ↓↓↓ p < 0·001, ↓↓ p < 0·01, ↓ p < 0·05) and subsequent changes in slope shown as sloping arrows (increases ↗↗↗ p < 0·001, ↗↗ p < 0·01, ↗ p < 0·05; → no significant change; decreases ↘↘↘ p < 0·001, ↘↘ p < 0·01, ↘ p < 0·05). The date range of available data is shown at the bottom of each figure. (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
This drop encompassed services accepting referrals from professionals (primary care MH service, IAPT, specialist MH teams). Service reorganization may therefore have contributed. However, the drop was also observed across services accepting patient self-referral, in part or exclusively (IAPT, 111, LP).
3.2. Presenting MH problems
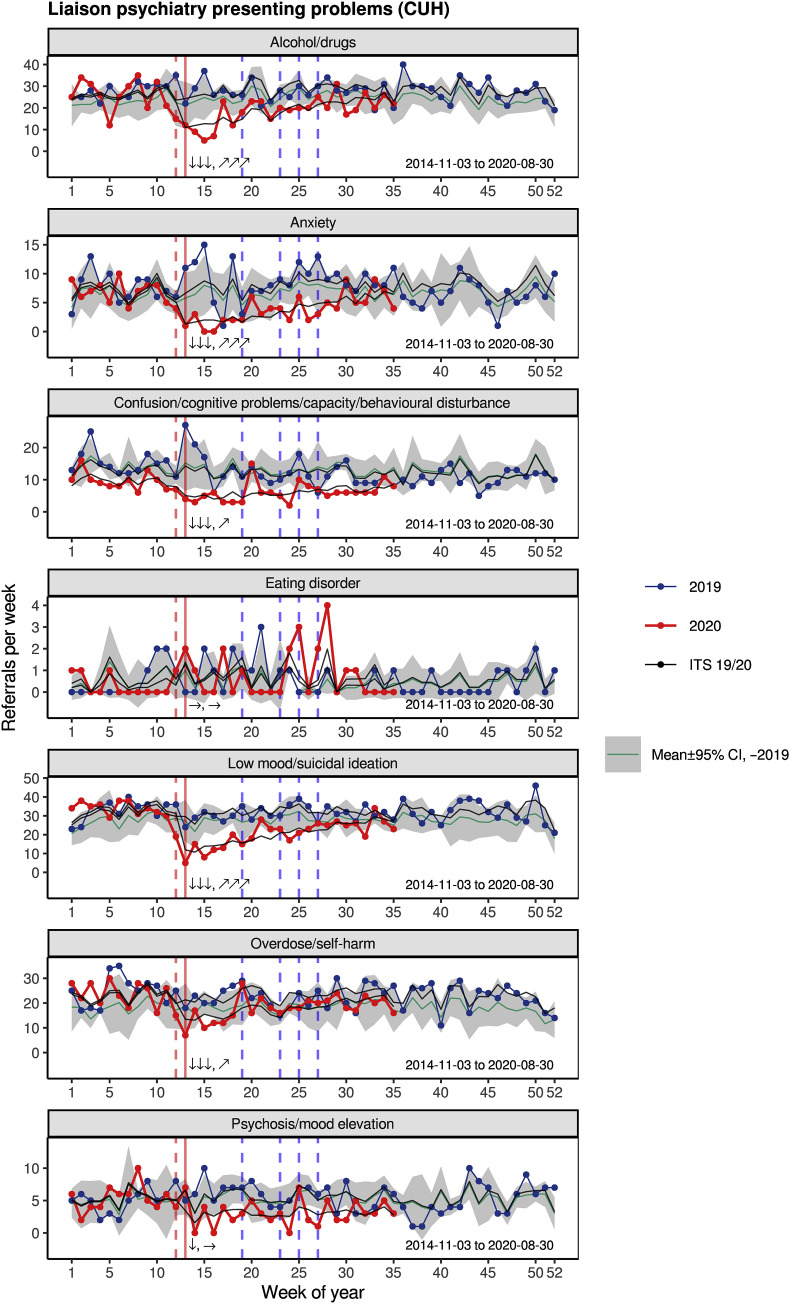
Presenting problems for LP referrals are shown in Fig. 2 . All types of presentation dropped at lockdown and then increased towards normal levels, except presentation with psychosis/mood elevation (small sustained reduction) or eating disorders (no significant change), though these presentations are less common than the other reasons, potentially limiting power.
Fig. 2.
Presenting problems recorded at the time of first LP assessment at CUH. An individual referral may be associated with >1 problem (e.g. suicidal ideation plus overdose). Conventions as for Fig. 1.
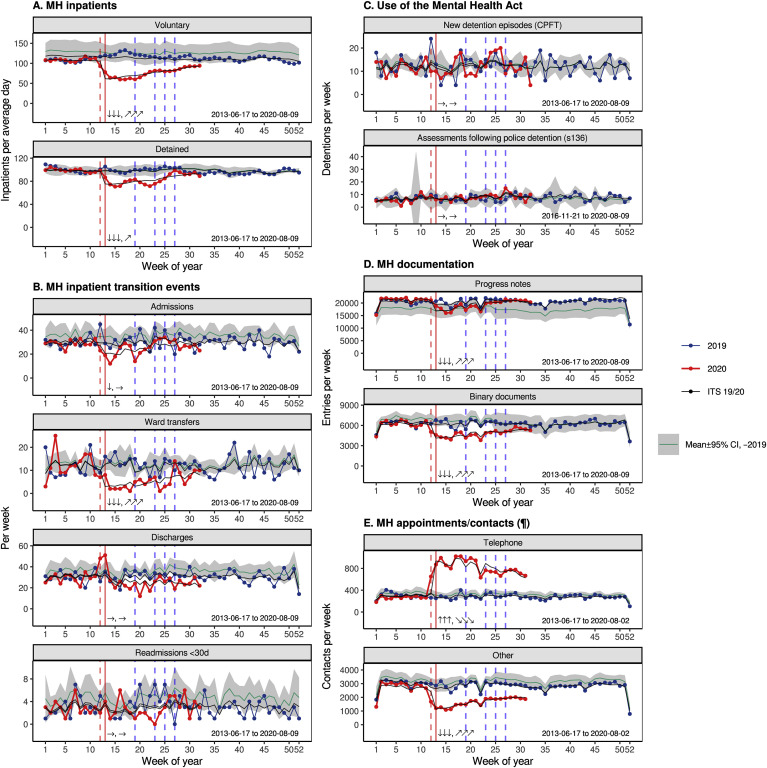
3.3. MH inpatient activity
Prior to the pandemic, the proportion of detained patients (as opposed to voluntary or “informal” inpatients) was high compared to the local historical mean (Fig. 3 A), suggesting higher acuity. Both detained and voluntary inpatient numbers dropped sharply at lockdown (Fig. 3A), reflecting fewer admissions (and a spike in discharges beginning just before lockdown; Fig. 3B). The reduction in inpatient numbers was deliberate (Supplementary Methods). Inter-ward transfers were reduced effectively (Fig. 3B), and readmission rates did not change (Fig. 3B). The same patterns were seen for patients with and without SMI, except that the admission rate did not drop significantly for those with SMI (Supplementary Results).
Fig. 3.
MH inpatient, Mental Health Act, and other service “activity” measures. (A) Number of inpatients on any given day (averaged over each week). (B) Admissions, ward transfers, discharges, and readmissions within 30 days. (C) New detention episodes under the MHA (any section) and assessments following police detention under s136. (D) Volume of documentation. Progress Notes are created by CPFT staff; binary documents may originate from CPFT staff or from others. (E) Booked appointments/contacts (not all contacts are thus recorded), split by telephone contact versus all other recorded kinds (e.g. first assessment, home visit). Conventions as for Fig. 1. (¶ Recent values may be underestimated due to recording lag, though data are truncated to allow for this; see Methods.)
3.4. Mental Health Act
There was no evidence for a change in the use of the MHA, either within the MH service or by police (Fig. 3C); neither was there a change for subgroups with/without SMI (Supplementary Results).
3.5. MH contacts and documentation
Activity, as measured by clinical documentation, dropped (Fig. 3D) and contacts shifted towards telephone consultations (Fig. 3E) (see also Supplementary Results). These changes were substantial and sustained.
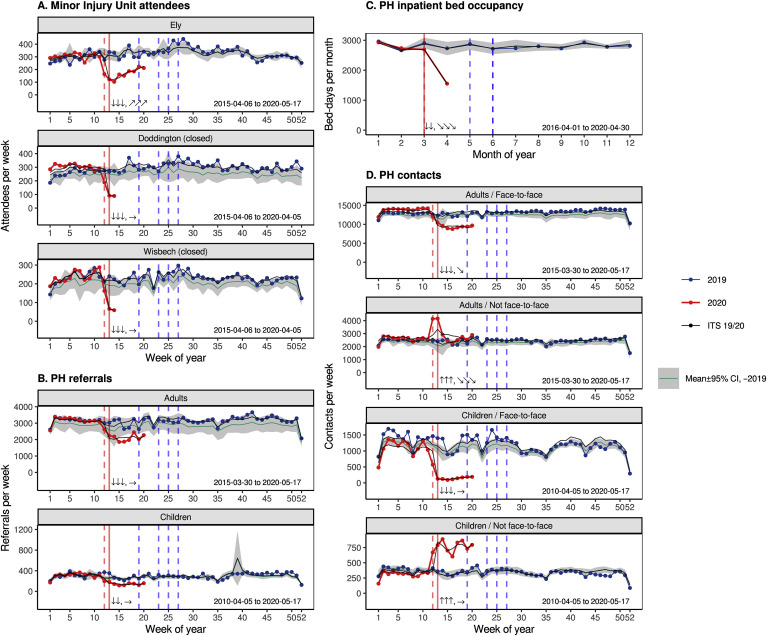
3.6. PH presentations, referrals, and contacts
Attendance at the MIU that remained open dropped dramatically at lockdown and increased slightly thereafter, despite the closure of two other MIUs (Fig. 4 A). Referrals to PH services dropped across age groups (Fig. 4B). PH ward occupancy decreased (Fig. 4C). Face-to-face contacts fell across age groups, with an increase in non-face-to-face contacts (Fig. 4D).
Fig. 4.
Physical health (PH) service activity. (A) Presentations to MIUs. Two units were closed while the other was expanded. (B) Referrals to PH services. (C) PH ward occupancy (as bed-days per month). The ITS was performed by month rather than week but was otherwise as for other analyses. (D) Recorded contacts, split by age group and whether the contacts were face-to-face or not. Conventions as for Fig. 1.
3.7. Deaths
There was a clear and sustained increase in death amongst patients with open referrals to PH services at the time of lockdown (Fig. 5 A), with the excess deaths occurring shortly after the rapid increase in COVID-19 infections in the region (Fig. 5E). The excess of deaths in 2020 was predominantly in the over-70s (Fig. 5B). Deaths in patients known to MH services increased at this time for those with and without SMI (Fig. 5C and D); again, this was primarily in the over-70s, but with additional increases in other age bands, notably for those with SMI (Fig. 5D). More recent data were available for MH services, and in patients without SMI (who were in the majority) a biphasic effect was seen, with a drop in mortality below the historical norm after the initial increase in deaths (Fig. 5C).
Fig. 5.
Confirmed COVID-19 cases for Cambridgeshire and Peterborough, and deaths of CPFT patients. Note that reporting of deaths is delayed, so recent data may be incomplete, but the data are truncated to allow for this (see Methods). (A) Deaths of patients with an open referral to PH services at the time of their death. (B) Deaths from A, by year and age band at death. Annotations show tests of the step change in 2020 from an ITS analysis within that age band (see Methods) [↑↑, ↓↓ indicate increases and decreases respectively with p < 0·01; ↑, ↓ p < 0·05; (↑), (↓) p < 0·1]. (C) Deaths of patients known to MH services, by previous presence of a coded diagnosis of an SMI. (D) Deaths from C, plotted as for B. (E) Confirmed COVID-19 cases for C&P as a whole and for CUH (ED and inpatients only). The C&P spike around week 17–18 is related to the expansion of population testing (see Supplementary Methods) (Mahase, 2020). (F) Age- and sex-standardized mortality ratios (SMRs, ±95% confidence interval) for patients known to MH services, split by the presence of a coded SMI diagnosis or not. SMRs increased from 2019 to 2020 for the SMI group (†p < 0·05). In 2020, the SMR was greater in the SMI group than the non-SMI group (differences for each year: ***p < 0·001). The increase in SMR from 2019 to 2020 was significantly greater in the SMI group than the non-SMI group (#p < 0·05 from ITS analysis; see Results). Note that SMRs are calculated for each year across dates available in 2020. This allows fair comparison with other years (given that deaths normally vary seasonally: compare A,C), though it may overestimate absolute SMRs slightly by comparing Jan–May CPFT figures with Jan–Dec population estimates. Conventions for A, C: as for Fig. 1.
Mortality, measured by SMR, increased significantly from 2019 to 2020 for patients with SMI, and increased significantly more for those with SMI than without (Fig. 5F; ITS analysis, SMI × 2020, p < 0·05). Across all data available from 2020 to date, the change in SMR for those without SMI was not significant (reflecting the biphasic pattern seen in Fig. 5C: an increase followed by a decrease). Across all years, SMI conferred a greater additional risk of mortality in the ethnic minority/unrecorded ethnicity group (SMI × ethnicity, p < 0·05). There was no ethnicity-specific effect in 2020 (terms involving ethnicity × 2020, not significant) and the increased mortality amongst those with SMI in 2020 (as above) was not explicable by ethnicity.
4. Discussion
4.1. Summary
Referrals and self-presentations to health services dropped substantially at lockdown across the MH and community PH system in our area. In some cases, these reflected service-led changes (e.g. closing some teams to non-urgent referrals; discharging patients to create inpatient capacity). For some services, though, activity is driven by patient self-presentation (e.g. 111 crisis calls, attendance at EDs/MIUs) yet activity dropped nonetheless. There was no evidence that suppression of demand in some services led to “redistribution” to any other service, with no increase in demand for MH emergency services (111, crisis teams, ED), even for services permitting self-referral and remote consultation (111). There was no evidence of a compensatory “rebound” in demand beyond initial levels, though this may change in the future, and the trend for some services is now upwards. Service activity dropped less for those with SMI. There was clear evidence of the shift to remote consultation. Mortality increased substantially, with a much greater increase for patients with SMI than without (Fig. 5F).
4.2. Mental health presentations
Our concerns a priori included an increase in MH presentations with affective disorders (anxiety, depression, self-harm, suicide attempts), other stress-exacerbated disorders (psychosis, eating disorders), and referrals for delirium associated with severe COVID-19. None of these effects were observed.
Several authors have highlighted a risk that suicide increases as a result of the pandemic (Gunnell et al., 2020; Holmes et al., 2020), noting such effects after the 2003 severe acute respiratory syndrome (SARS) epidemic. In contrast, suicide rates fall during wars that increase social cohesion by uniting a population against a common foe (Pridmore et al., 2018). COVID-19 may have had some such “cohesion” effect, though a later increase in suicidality remains possible. Reduced presentations with self-harm/suicide attempts may also reflect reduced access to the means of suicide and/or reduced help-seeking; additionally, we do not have data on people who may have ended their life but were not known to our services. Population surveys of UK general mental health suggest a substantial deterioration following lockdown (Banks and Xu, 2020), but this has not translated (thus far) to an increase in presentation with mental disorder in our area. The increase in threshold for referral may be an important factor here.
Lockdown may have had negative psychological effects for many but positive effects for some. For example, psychosocial stressors relating to school (e.g. bullying, examinations) commonly exacerbate MH problems in children (e.g. school avoidance, associated anxiety and depression); schools were closed and examinations cancelled. For some, there may have been beneficial effects of not having to leave the home environment. In contrast, there have been dramatic negative effects for others. The pandemic has brought uncertainty and anxiety both about the disease itself and associated consequences (Rettie and Daniels, 2020; McElroy et al., 2020). Our clinical experience of patients presenting in MH crisis has included people reporting COVID-19-related psychosocial stressors such as loss of employment and support networks (both formal and informal) and confinement (including in emotionally abusive situations), and people with severe mental disorders coming to the attention of the police and MH services having been unable to follow social distancing rules.
4.3. Physical health presentations
The reduction in presentations to the open MIU was abrupt and dramatic, and occurred despite the closure of two others in the area. Whilst a reduction in help-seeking cannot be excluded (injuries still occurring but people not seeking medical attention or presenting to an ED instead), the degree suggests that lockdown has reduced minor injury.
4.4. Inpatient stays
An effort to expedite discharge wherever safe had obvious results. The drop in the number of detained inpatients is particularly striking. Given the lack of change in new MHA detentions, we suggest that Responsible Clinicians perceived an increase in the risk of being admitted (relating to COVID-19 transmission) that shifted the risk/benefit balance, near the end of a detained admission, towards earlier discharge. The sustained reduction in admissions, at least for those without SMI, suggests also a changed threshold for admission—though not for detention and by inference probably therefore for voluntary admission.
4.5. Mortality
There was stark excess mortality in the over-70s in 2020 to date, likely due to COVID-19, but these data also provide strong (albeit observational) evidence that SMI is a major risk factor for death during the pandemic. The baseline SMR in patients known to MH services was high, likely reflecting CPFT's provision of MH care to those with life-limiting illnesses including dementia. The biphasic mortality effect observed in patients without recorded SMI—an increase in deaths when COVID-19 spread in Cambridgeshire and Peterborough, followed by a drop below historical norms—suggests a degree of temporal shift in mortality, i.e. that some patients died earlier within 2020 than they would otherwise have done. However, beyond this, there was a substantial and disproportionate increase in mortality amongst those with SMI during 2020. This was not explained by ethnicity. Our data do not identify the mechanisms conferring additional risk on those with SMI. These might include differences in interpersonal contact and viral transmission risk in those with SMI (Moore et al., 2020); higher rates of comorbidities such as obesity, diabetes, and cardiovascular disease (McGinty et al., 2016) that are associated in turn with greater severity of COVID-19 infection (Liu et al., 2020); and increased mortality via diseases other than COVID-19, potentially via differences in help-seeking or healthcare provision.
4.6. Strengths and weaknesses
These data represent a relatively comprehensive view of NHS-provided MH services in one geographical area (because CPFT provides psychological therapy and all secondary MH care to the entire population of C&P), making it less likely that decreases were compensated for by help-seeking via another NHS service. For some services there were “unmeasured” alternatives (e.g. MH support from charities; support for children from the Local Authority). The data are less comprehensive for PH services, but sufficient to allow some comparison of health-seeking and mortality in the two domains. Changes in referrals to some services may have reflected changes to “demand” or “supply” or both, though activity in other services was more clearly led by patient help-seeking (demand). Widespread travel out of CPFT's catchment area is not a plausible explanation for the changes, given the magnitude of change and national travel bans (Hancock, 2020). Mortality data was available via national reporting mechanisms for all MH patients, but only for PH patients with open referrals to CPFT, and mortality data may be incomplete if delays in national reporting exceeded 7 days. This was a retrospective observational study. Though the associations observed were strong via ITS analysis, a recommended approach for evaluating changes in routine data associated with a well-defined event (Bernal et al., 2017), they do not prove causation. Cambridgeshire and Peterborough have had COVID-19 infection rates spanning the “low middle” of the UK range (Public Health England and NHSX, 2020), which is high internationally (Our World in Data, 2020); our findings may not generalize to areas with different infection rates. The situation is changing rapidly and more recent data may change the overall picture (e.g. if a rebound in demand occurs).
4.7. Conclusions
We show a reduction in demand as well as supply during the early phase of the pandemic for MH and community PH services covering a population of ~0·86 million. The changes in supply may have reduced access to mental health services for some. It remains to be seen whether the changes in demand reflect a reduction in MH morbidity or whether a hidden burden of mental illness will become apparent in months to come. However, activity in a number of services is now increasing; this suggests that there is patient need but that help-seeking has been transiently suppressed. Further research is required into the mechanisms by which SMI is associated with elevated mortality during this pandemic, but we suggest that patients with SMI be considered a high-risk group during COVID-19.
Funding
SC’s, PBJ’s, SB’s, and RNC’s research was supported by the UK Medical Research Council (grant MC_PC_17213 to RNC). PBJ is supported by the UK National Institute for Health Research (NIHR) Applied Research Collaboration East of England. BU is supported by the Gnodde Goldman Sachs Translational Neuroscience Unit at CPFT. ETB is an NIHR Senior Investigator. This research was supported in part by the NIHR Cambridge Biomedical Research Centre; the views expressed are those of the authors and not necessarily those of the NHS, the NIHR, or the Department of Health and Social Care.
The funders had no role in study design, data collection, analysis, interpretation, or writing of the article. RNC had full access to all data in the study and had final responsibility for the decision to submit for publication.
Author contributions
RNC, ETB, BRU, and SC designed the study. SC, RNC, JRL, MPS, and JDA extracted and analysed the data. RNC and SC drafted the manuscript. All authors contributed to data interpretation, and edited and approved the final manuscript.
Data availability
Patient-level data is not publicly available, under NHS Research Ethics terms. Source code and summary data are available on request.
Declaration of competing interest
-
•
Several authors (PBJ, BRU, AM, ETB, ESO, JBD, CFH, FJT, RNC) are CPFT clinicians involved in delivering some of the services discussed here and two (BRU, FJT) are clinical directors and therefore involved in managing them.
-
•
PBJ is a scientific advisory board member for Janssen and Recordati.
-
•
BRU is clinical director of the Windsor Unit at Fulbourn Hospital (CPFT), which delivers clinical trials in dementia/mild cognitive impairment for academic and commercial organisations without personal benefit, and is the clinical lead for dementia for the NIHR Clinical Research Network (CRN) in the East of England. His salary is part-funded by the NIHR CRN. He has been principal investigator on trials for Axovant, Lilly, and EIP Pharma; his institution has benefited from payment for research carried out but he has not personally received any money. His wife is the lead for mental health for Suffolk Clinical Commissioning Group.
-
•
AM’s salary is part-funded by the Anna Freud National Centre for Children and Families, a mental health charity.
-
•
ETB is a scientific advisory board member for Sosei Hepares, and was a half-time employee of GlaxoSmithKline until May 2019.
-
•
RNC consults for Campden Instruments Ltd and receives royalties from Cambridge University Press, Cambridge Enterprise, and Routledge.
-
•
SC, SB, EFO, JBD, CFH, FJT, JDA, MPS, and JRL have nothing else to disclose.
Acknowledgements
We thank Matthew Loftus, Natalie Robinson-Creek, Alykhan Valani, and Mai Wong for assistance with data extraction; Ben Warne for advice on COVID-19 reporting; Ann Cardinal for suggestions; and Melanie Bruneau, Claire Cafferkey, Orna Clark, Myles Doyle, Terry Hill, Damaris Koch, Adele McCormack, Paul Millard, Ben Morris, and Maggie Page for advice on service organization. We thank our anonymous referees for their helpful comments and suggestions.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jpsychires.2020.09.020.
ABBREVIATIONS
- 111
NHS urgent care telephone service (111 is the telephone number)
- BAME
Black, Asian, and minority ethnic
- C&P
Cambridgeshire and Peterborough, UK
- CAMH
child and adolescent mental health
- CDU
Clinical Decision Unit
- COVID-19
Coronavirus disease 2019
- CPFT
Cambridgeshire and Peterborough NHS Foundation Trust
- CRHT
crisis resolution/home treatment team
- CUH
Cambridge University Hospitals NHS Foundation Trust
- ED
Emergency Department
- EIP
early intervention in psychosis
- IAPT
Improving Access to Psychological Therapies
- ICD-10
World Health Organization International Classification of Diseases, 10th Revision
- ISO
International Organization for Standardization
- ITS
interrupted time series
- LP
liaison psychiatry
- MH
mental health
- MHA
UK Mental Health Act
- MIU
Minor Injury Unit
- NHS
UK National Health Service
- PCMIS
Patient Case Management Information System
- PH
physical health
- s136
Section 136 of the MHA
- SARS
severe acute respiratory syndrome
- SARS-CoV-2
severe acute respiratory syndrome coronavirus 2
- SD
standard deviation
- SMI
severe mental illness
- SMR
standardized mortality ratio
- UK
United Kingdom
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Banks J., Xu X. 2020. The mental health effects of the first two months of lockdown and social distancing during the Covid-19 pandemic in the UK. Published online June 10. [DOI] [Google Scholar]
- Bernal J.L., Cummins S., Gasparrini A. Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int. J. Epidemiol. 2017;46:348–355. doi: 10.1093/ije/dyw098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalgaard P. Second ed. Springer; 2008. Introductory Statistics with R. [Google Scholar]
- Garvin M.R., Alvarez C., Miller J.I. A mechanistic model and therapeutic interventions for COVID-19 involving a RAS-mediated bradykinin storm. eLife. 2020;9 doi: 10.7554/eLife.59177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gunnell D., Appleby L., Arensman E. Suicide risk and prevention during the COVID-19 pandemic. Lancet Psychiatr. 2020;7:468–471. doi: 10.1016/S2215-0366(20)30171-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hancock M. 2020. The Health Protection (Coronavirus, Restrictions) (England) Regulations 2020.http://www.legislation.gov.uk/uksi/2020/350/contents/made [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatr. 2020;7:547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Chen S., Liu M., Nie H., Lu H. Comorbid chronic diseases are strongly correlated with disease severity among COVID-19 patients: a systematic review and meta-analysis. Aging Dis. 2020;11:668–678. doi: 10.14336/AD.2020.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahase E. Covid-19: the problems with case counting. BMJ. 2020;370:m3374. doi: 10.1136/bmj.m3374. [DOI] [PubMed] [Google Scholar]
- McElroy E., Patalay P., Moltrecht B. Demographic and health factors associated with pandemic anxiety in the context of COVID-19. Br. J. Health Psychol. 2020 doi: 10.1111/bjhp.12470. Published online Aug 29. [DOI] [PubMed] [Google Scholar]
- McGinty E.E., Baller J., Azrin S.T., Juliano-Bult D., Daumit G.L. Interventions to address medical conditions and health-risk behaviors among persons with serious mental illness: a comprehensive review. Schizophr. Bull. 2016;42:96–124. doi: 10.1093/schbul/sbv101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore R.C., Depp C.A., Harvey P.D., Pinkham A.E. Assessing the real-time mental health challenges of COVID-19 in individuals with serious mental illnesses: protocol for a quantitative study. JMIR Res. Protoc. 2020;9 doi: 10.2196/19203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NHS England. NHS Improvement . 2020. Next steps on NHS response to COVID-19.https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/20200317-NHS-COVID-letter-FINAL.pdf published online March 17. accessed March 18, 2020. [Google Scholar]
- Office for National Statistics . 2020. Estimates of the population for the UK, England and wales, scotland and northern Ireland [mid-2019 estimates]https://www.ons.gov.uk/file?uri=%2fpeoplepopulationandcommunity%2fpopulationandmigration%2fpopulationestimates%2fdatasets%2fpopulationestimatesforukenglandandwalesscotlandandnorthernireland%2fmid2019april2020localauthoritydistrictcodes/ukmidyearestimates20192020ladcodes.xls published online June 24. accessed July 3, 2020. [Google Scholar]
- Office for National Statistics . 2020. Age-standardised mortality rates and age-standardised fertility rates for local authorities in England (2018 based)https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationprojections/datasets/agestandardisedmortalityratesandagestandardisedfertilityratesforlocalauthoritiesinengland accessed June 6, 2020. [Google Scholar]
- Our World in Data . 2020. Total COVID-19 tests, confirmed cases and deaths per million people.https://ourworldindata.org/grapher/covid-tests-cases-deaths-per-million [Google Scholar]
- Pridmore S., Ahmadi J., Pridmore W. Suicide of Australians during the vietnam war. Australas Psychiatr. Bull Roy. Aust. N. Z. Coll. Psychiatr. 2018;26:149–151. doi: 10.1177/1039856217734740. [DOI] [PubMed] [Google Scholar]
- Prime Minister’s Office . 2020. PM statement on coronavirus: 16 March 2020.https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-16-march-2020 published online March 16. accessed March 16, 2020. [Google Scholar]
- Prime Minister’s Office . 2020. PM address to the nation on coronavirus: 23 March 2020.https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-23-march-2020 published online March 23. accessed March 23, 2020. [Google Scholar]
- Prime Minister’s Office . 2020. PM address to the nation on coronavirus: 10 May 2020.https://www.gov.uk/government/speeches/pm-address-to-the-nation-on-coronavirus-10-may-2020 published online May 10. accessed May 27, 2020. [Google Scholar]
- Public Health England, NHSX . 2020. Coronavirus (COVID-19) in the UK.https://coronavirus.data.gov.uk/ [Google Scholar]
- R Core Team . R Foundation for Statistical Computing; Vienna, Austria: 2019. R: A Language and Environment for Statistical Computing.http://www.R-project.org/ [Google Scholar]
- Rettie H., Daniels J. Coping and tolerance of uncertainty: predictors and mediators of mental health during the COVID-19 pandemic. Am. Psychol. 2020 doi: 10.1037/amp0000710. published online Aug 3. [DOI] [PubMed] [Google Scholar]
- Ripley B., Venables B., Bates D.M., Hornik K., Gebhardt A., Firth D. 2020. MASS: support functions and datasets for Venables and Ripley’s MASS.https://cran.r-project.org/web/packages/MASS/ [Google Scholar]
- Roche J.A., Roche R. A hypothesized role for dysregulated bradykinin signaling in COVID‐19 respiratory complications. Faseb. J. 2020 doi: 10.1096/fj.202000967. Published online May 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J.P., Chesney E., Oliver D. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. Lancet Psychiatr. 2020;7:611–627. doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romoli M., Jelcic I., Bernard-Valnet R. A systematic review of neurological manifestations of SARS-CoV-2 infection: the devil is hidden in the details. Eur. J. Neurol. 2020 doi: 10.1111/ene.14382. Published online June 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rothman K.J., Greenland S., Lash T.L. Third ed. Lippincott Williams & Wilkins; Philadelphia, PA, USA: 2008. Modern Epidemiology. [Google Scholar]
- UK Government Office for Science . 2020. Ethnicity and COVID-19: preliminary meeting for SAGE. 2 June 2020. [Google Scholar]
- UK National Institute for Health and Care Excellence . 2016. NG58: coexisting severe mental illness and substance misuse: community health and social care services.https://www.nice.org.uk/guidance/ng58 accessed Oct 17, 2019. [PubMed] [Google Scholar]
- Varatharaj A., Thomas N., Ellul M.A. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiatr. 2020 doi: 10.1016/S2215-0366(20)30287-X. Published online June 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Eriksen Benros M. COVID-19 pandemic and mental health consequences: systematic review of the current evidence. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.048. Published online May 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Weyhern C.H., Kaufmann I., Neff F., Kremer M. Early evidence of pronounced brain involvement in fatal COVID-19 outcomes. Lancet Lond. Engl. 2020;395:e109. doi: 10.1016/S0140-6736(20)31282-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wagner A.K., Soumerai S.B., Zhang F., Ross-Degnan D. Segmented regression analysis of interrupted time series studies in medication use research. J. Clin. Pharm. Therapeut. 2002;27:299–309. doi: 10.1046/j.1365-2710.2002.00430.x. [DOI] [PubMed] [Google Scholar]
- Zubair A.S., McAlpine L.S., Gardin T., Farhadian S., Kuruvilla D.E., Spudich S. Neuropathogenesis and neurologic manifestations of the coronaviruses in the age of coronavirus disease 2019: a review. JAMA Neurol. 2020 doi: 10.1001/jamaneurol.2020.2065. Published online May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Patient-level data is not publicly available, under NHS Research Ethics terms. Source code and summary data are available on request.