Abstract
To report an unusual case of a 71-year-old livestock farmer with systemic brucellosis and ocular involvement. Examination showed vitreous haze with bilateral serous choroidal detachment. He was treated with topical antibiotics and corticosteroids, Tab rifampicin 600 mg and doxycycline 100 mg for 6 weeks with visual recovery and complete resolution of serous choroidal detachment in 2 weeks. This is the first case of bilateral serous choroidal detachment in a case of systemic brucellosis. Immune-mediated complex and direct microbial invasion of uveal tissue leading to serous choroidal detachment is the proposed pathogenesis that responds well to topical corticosteroids.
Keywords: Brucellosis, doxycycline, serous choroidal detachment
Brucellosis is a systemic zoonotic disease caused by Brucella species which presents as undulant fever, sweating, and migratory arthralgia. Ocular manifestations in systemic brucellosis described in the literature are conjunctivitis, episcleritis, posterior uveitis, choroiditis, endogenous endophthalmitis, and neuro-ophthalmic manifestations which are primarily treated with systemic antibiotics and oral corticosteroids. The present case is a unique case, where serous choroidal detachment with vitreous haze is the presenting feature. The serous choroidal detachment coinciding with cutaneous vasculitis, both of which are immunologically mediated, and a complete resolution with topical corticosteroids and systemic rifampicin and doxycycline treatment are first to be described in the literature.
Case Report
A 71 year old male, livestock farmer by profession with known hypertensive and type II diabetes mellitus was admitted in the internal medicine department of our hospital with a complaint of intermittent high-grade fever with chills, malaise, and nausea with no diurnal variation of almost 10 days duration for which he was under evaluation by the internal medicine department. He developed cutaneous vasculitis and ecchymotic patches on upper and lower limbs on day 5 of the admission along with blurring of vision in both eyes.
He underwent detailed immunological and infective workup in view of pyrexia, rash. Vasculitic and immunology workup showed a positive antiphospholipid antibody and the rest were unremarkable. His infectious workup showed a positive Brucella IgM antibody (1.37). His dengue panel was normal. Platelet counts were reduced to 42000/mm3. His echocardiogram showed minimal pericardial effusion.
He complained of blurred vision in both eyes, more in the right eye which coincided with cutaneous ecchymosis. On examination, visual acuity was 20/80 in both eyes. Slit lamp examination showed normal ocular adnexa, mild conjuctival congestion in both eyes with pseudophakia. Rest of the anterior segment examination was unremarkable. Vitreous showed minimal vitreous haze [Fig. 1] with well-defined disc margins and macula normal. Peripheral retinal examination showed 360° serous choroidal detachment in both eyes with the right eye [Fig. 1] more than the left eye. Intraocular pressure was 10 mm Hg with Perkins tonometer.
Figure 1.
(a and b) Fundus photographs of right and left eye posterior pole, disc, and macula, respectively showing vitreous haze. (c) Fundus photograph of a temporal quadrant of the right eye showing shallow serous choroidal detachment (black arrows)
He underwent B-scan ultrasonography, which confirmed a serous choroidal detachment. The optical coherence tomography macula of both eyes was normal with no evidence of cystoid macular edema [Fig. 2]. He was started on topical antibiotics (moxifloxacin 0.5%), topical cycloplegics (homatropine 2%), and topical prednisolone acetate (1%). For systemic brucellosis, he was started on Tab rifampicin 600 mg once a day and Tab doxycycline 100 mg two times a day for 6 weeks. After the systemic medications, fever responded with clearing cutaneous symptoms.
Figure 2.
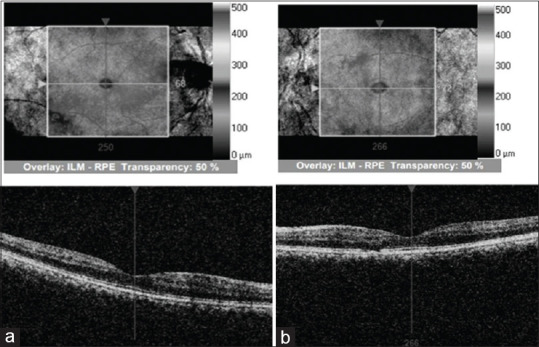
(a) Showing optical coherence tomography of the right eye showing good foveal contour and absence of cystoid edema. (b) Showing left eye good foveal contour, focal loss of inner segment-outer segment line in the nasal parafoveal area and absence of cystoid edema
His visual acuity improved in the next 2 weeks to 20/40 and 20/60 in the right eye and left eye, respectively. The anterior segment showed cleared circumciliary congestion, a quiet anterior chamber, and resolved vitreous haze. The bilateral serous choroidal detachment resolved in 2 weeks [Fig. 3]. His topical antibiotics were discontinued in 2 weeks and topical corticosteroids were tapered on a 2 weekly basis. He was reviewed in 2 months' time with a visual acuity of 20/20 in both eyes and N6 (+3.00 DS) near addition. His anterior segment was unremarkable with complete resolution of vitreous haze, serous choroidal detachment.
Figure 3.
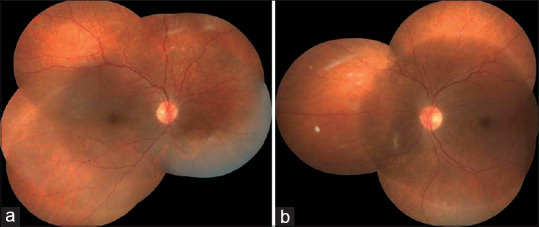
(a and b) Fundus photography pictures of the right and left eye showing clear media, normal disc, and the periphery with resolved vitreous haze and choroidal detachment
Discussion
Brucellosis is a zoonosis caused by the ingestion of unpasteurized milk, contact with livestock and their secretions. The causative organism is a Gram-negative, nonmotile, nonspore-forming, rod-shaped coccobacillus. Four different species were identified among which Brucella abortus and Brucella melitensis are the most common to infect humans.
In the initial stage, sepsis occurs with the classical triad of undulant fever, sweating, and migratory arthralgia. Blood tests reveal low white and red blood cell count, the elevation of liver enzymes. Gastrointestinal symptoms occur in 70% of cases including nausea, vomiting, abdominal pain, hepatosplenomegaly, and liver microabscess. The diagnosis of brucellosis relies on a high index of suspicion with a demonstration of IgM antibodies against Brucella with ELISA.
Fabyan (1912) first described Brucella and its ocular features in experimental guinea pigs which were injected intraperitoneally with B. abortus. He noticed corneal cloudiness and also tubercle-like formations in the sclera, choroid, and lacrimal glands. Lemaire[1] (1924) was the first to report ocular manifestations in brucellosis where he described bilateral optic neuritis and external ophthalmoplegia in a case of brucella meningitis. Conjunctival and fundus petechiae were reported by Wechsler and Gustafson[2] (1942) and Beebe and Meneely[3] (1949) in cases of Brucella endocarditis especially by abortus and melitensis. Rabinowitz[4] et al. published a case report with bilateral peripapillary serous retinal detachments in a case of brucellosis where they postulated low-virulence Brucella organisms in choroidal tissue.
Ocular involvement in brucellosis can be divided into
Pure ophthalmic—conjunctivitis, keratitis, episcleritis, dacryoadenitis, anterior and posterior uveitis, choroiditis, endogenous endophthalmitis.
Neuro-ophthalmologic—para-infectious optic neuritis, retrobulbar neuritis, III, IV, and VI nerve palsies (Brucella meningoencephalitis)
Secondary to Brucella complications—Conjunctival and fundal hemorrhages (thrombocytopenia).
A study by Ronaldo et al.[1] in Peru showed the incidence of ocular brucellosis as 0.7% (7 in 965) and 7.9% (45 in 570) in acute and chronic, respectively with uveitis as the most frequent ocular presentation (82.7%) out of which the most common was posterior uveitis.
Woods[5] et al. and Rolando[6,7] et al. postulated two mechanisms of host-pathogen interaction in brucellosis. First causes direct invasion of the ocular tissue by the microorganism, producing septic emboli to the uveal tissue leading to focal choroiditis. The second involves the formation of immunoglobulin and circulating immune complexes which are implicated in uveitis. In severe infections, these complexes along with the direct invasion of uveal tissue by the microorganism cause increased transmural pressure in choroidal blood vessels leading to serous fluid accumulation and serous choroidal detachment. This explains the mechanism of choroidal detachment in the present case.
In the present case, the systemic antibiotics specific to Brucella helped to reduce the bacterial invasion of the uveal tissue and thus in the reduction of inflammation. Once the inflammation reduces, the choroidal effusion and detachment resolve faster. This explains the improvement with topical corticosteroids alone. Severe inflammation in selected cases may require oral corticosteroids.
Conclusion
This is the first case of bilateral serous choroidal detachment in a case of systemic brucellosis. Immune-mediated complex and direct microbial invasion of uveal tissue leading to serous choroidal detachment is the proposed pathogenesis that responds well to systemic antibiotics and topical corticosteroids.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rolando I, Olarte L, Vilchez G, Lluncor M, Otero L, Paris M, et al. Ocular manifestations associated with brucellosis: A 26-year experience in Peru. Clin Infect Dis. 2008;46:1338–45. doi: 10.1086/529442. [DOI] [PubMed] [Google Scholar]
- 2.Wechsler HF, Gutafson EG. Brucella endocarditis of congenital bicuspid aortic valve. Ann Intern Med. 1942;16:1228–33. [Google Scholar]
- 3.Beebe RT, Meneely JK., Jr Brucella melitensis endocarditis; report of a case. Am Heart J. 8:788–91. doi: 10.1016/0002-8703(49)90536-0. 194. [DOI] [PubMed] [Google Scholar]
- 4.Rabinowitz R, Schneck M, Levy J, Lifshitz T. Bilateral multifocal choroiditis with serous retinal detachment in a patient with Brucella infection: Case report and review of the literature. Arch Ophthalmol. 2005;123:116–8. doi: 10.1001/archopht.123.1.116. [DOI] [PubMed] [Google Scholar]
- 5.Woods A. Experimental Brucellar uveitis. Am J Ophthalmol. 1953;36:1025–42. doi: 10.1016/0002-9394(53)91883-2. [DOI] [PubMed] [Google Scholar]
- 6.Rolando I, Vilchez G, Olarte L, Lluncor M, Carrillo C, Paris M, et al. Brucellar uveitis: Intraocular fluids and biopsy studies. Int J Infect Dis. 2009;13:e206–11. doi: 10.1016/j.ijid.2008.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Rolando I, Tobaru L, Hinostroza S, Guerra L, Carbone A, Carrillo C, et al. Clinical manifestations of brucellar uveitis. Ophthalmic Pract. 1987;5:12–7. [Google Scholar]



