Case
A 54-year-old asymptomatic Caucasian woman with a history of psoriasis and chronic obstructive pulmonary disease (COPD) under treatment with topical and oral corticosteroids was referred for suspicion of choroidal lymphoma in both eyes (OU). The referring physician recommended treatment with rituximab, an anti-CD20 monoclonal antibody. On examination, best-corrected visual acuity was 20/20 in the right eye (OD) and 20/25 in the left eye (OS). The intraocular pressure, extraocular movements, and slit-lamp examination were normal OU. There was no conjunctival lymphoid infiltration OU. On funduscopic examination, there was a uniform mottled appearance of the choroid OU.
What is Your Next Step?
Treat patient with rituximab
Obtain optical coherence tomography (OCT)
Perform fine-needle aspiration biopsy
Advise external beam radiotherapy.
Findings
Funduscopically, the patient had diffuse subtle, yellow, mottled spots deep to the retina OU [Fig. 1a and b], suggesting possible choroidal lymphoma. However, on autofluorescence [Fig. 1c], there was localized hypo- and hyperautofluorescence OD (arrows) in the temporal macula, suggesting focally damaged retinal pigment epithelium (RPE), not typical for choroidal lymphoma which more often shows generalized RPE alterations. By OCT [Fig. 1d], subretinal fluid (SRF) and pachychoroid were documented, measuring 310 μm, suggestive of central serous chorioretinopathy. Furthermore, there was no sign of choroidal infiltration with lymphoma as the choroidal vascular pattern was intact and lacking a “seasick” surface undulation.[1]
Figure 1.
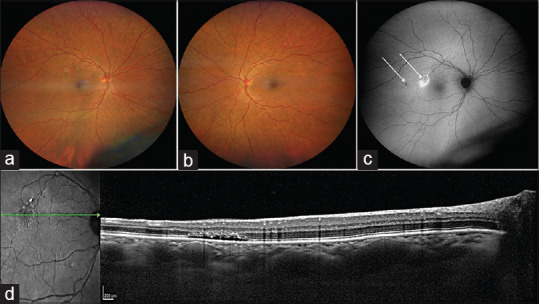
A 54-year-old female was found to have a (a) retinal pigment epithelial (RPE) mottling superotemporal to the foveola in the right eye (OD), and mottled choroid in both eyes (a and b). Autofluorescence OD (c) showed hypo- and hyperautofluorescence near the fovea. Optical coherence tomography (d) documented subretinal fluid, outer retinal loss, and pachychoroid with pachyvessels
Diagnosis
Central serous chorioretinopathy.
Correct Answer
B, Obtain optical coherence tomography (OCT).
Discussion
Central serous chorioretinopathy (CSCR) is a disorder involving choroidal vascular thickening and dilation of choriocapillaris with leakage of fluid under the RPE, producing RPE detachment and fluid accumulation under the retina. In a meta-analysis of 1098 cases of CSCR, 21% occurred in females, often with corticosteroid use.[2] Therefore, our patient was advised to discontinue corticosteroids. For chronic CSCR, oral eplerenone or spironolactone, mineralocorticoid receptor antagonists, or photodynamic therapy can be employed.[2,3] Bousquet et al. reported 3-month visual acuity outcome of 20/37 after eplerenone treatment, significantly improved from 20/66 (P < 0.001) at baseline, inferring the presumed role of corticosteroids in CSCR pathogenesis.[3]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Shields CL, Pellegrini M, Ferenczy SR, Shields JA. Enhanced depth imaging optical coherence tomography (EDI-OCT) of intraocular tumors From placid to seasick to rock and rolling topography. The 2013 Francesco Orzalesi Lecture Retina. 2014;34:1495–512. doi: 10.1097/IAE.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 2.Salehi M, Wenick AS, Law HA, Evans JR, Gehlbach P. Interventions for central serous chorioretinopathy: A network meta-analysis. Cochrane Database Syst Rev. 2015 doi: 10.1002/14651858.CD011841.pub2. 12 Art No: CD011841 doi: 101002/14651858CD011841pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bousquet E, Beydoun T, Zhao M, Hassan L, Offret O, Behar-Cohen F. Mineralocorticoid receptor antagonism in the treatment of chronic central serous chorioretinopathy: A pilot study. Retina (Philadelphia, Pa) 2013;33:2096–102. doi: 10.1097/IAE.0b013e318297a07a. [DOI] [PubMed] [Google Scholar]


