Abstract
Background
Uptake in lung cancer screening for high-risk patients remains low. Eligible patients may not know that this preventive service is available and covered by insurance.
Objectives
The objective of this study was to explore using social media to educate patients about lung cancer screening and assess motivation to discuss lung cancer screening with health-care providers after viewing the educational program.
Methods
Subjects ages 55 to 77 who were current smokers or former smokers who quit in the past 15 years with a more than 30-pack-year smoking history were recruited via a Facebook advertisement. Subjects completed a demographic survey and the Lung Cancer Screening-12 (LCS-12) knowledge measure tool, watched a YouTube video about lung cancer screening, and completed the LCS-12 tool (post-test). Subjects rated their level of motivation to discuss lung cancer screening with their health-care provider.
Results
This study used a pre-experimental, one-group pre-test and post-test design. Scores from the pre- and post-test were analyzed using the paired t-test. Descriptive statistics were used to analyze subject self-reporting of motivation to discuss screening with their provider. The mean knowledge score of participants (n = 31) significantly increased from 5.26 to 8.19 after viewing the video (t = –5.956, p < .001). The mean motivational level (1–5) was 3.52, with a mode of 5.
Conclusions
A lack of knowledge regarding lung cancer screening may negatively impact the health of high-risk patients. This study suggests that social media can be used to increase knowledge of lung cancer screening. These findings demonstrate that the use of social media has a role in improving access to health information.
According to the American Cancer Society (2020), lung cancer is the leading cause of adult cancer-related deaths in the United States, with approximately 228,820 new cases and 135,720 deaths predicted in 2020. The National Lung Screening Trial reported that annual low-dose CT of the chest (LDCT) performed in patients at high risk for lung cancer decreased mortality from lung cancer by 20% (Aberle et al., 2013). The U.S. Preventive Services Task Force gave lung cancer screening with LDCT a Grade B recommendation in 2013 (USPSTF, 2013). Based on this recommendation, the Centers for Medicare & Medicaid Services (CMS) and most commercial insurance providers now cover lung cancer screening with LDCT as a preventive health benefit. However, there has not been a significant increase in the rates of lung cancer screening with LDCT. In fact, between 2010 and 2015, there was only a 0.6% increase in the use of LDCT for lung cancer screening (Jemal & Fedewa, 2017).
Many eligible patients may not know that this preventive service is available and covered by insurance. Harnessing social media as a platform for education may increase awareness of screening. This will result in lung cancer being diagnosed at earlier stages, when it is most treatable, and ultimately may decrease the mortality of lung cancer.
BACKGROUND
Despite insurance coverage, there has been lower-than-expected use of this screening modality. Cardarelli and colleagues (2017) note that eligible patients are not aware of the recommendation for lung cancer screening and do not know what screening entails. According to Retrouvey, Patel, and Shaves (2016), 86.9% of eligible patients surveyed were not aware of the recommendation for lung cancer screening. This lack of knowledge may be due to lack of patient-provider discussions about lung cancer screening (Carter-Harris, Tan, Salloum, & Young-Wolff, 2016a). Carter-Harris and colleagues (2016a) found that less than 20% of screening-eligible patients had discussions with their health-care providers about lung cancer screening in comparison to 50% to 80% having had discussions about breast and colorectal cancer screening. Patients who are informed about cancer screening may be more likely to participate in these screening modalities.
Social media platforms such as YouTube and Facebook are popular outlets for the dissemination of information of all kinds. According to Prochaska, Coughlin, and Lyons (2017), an estimated 89% of adults in the US are online, and 72% own smartphones. Social media outlets have the potential to reach a wide audience with a variety of socioeconomic and cultural backgrounds, while providing low-cost, highly scalable functionality with the use of video for health literacy (Prochaska et al., 2017). Koskan and colleagues (2014) suggested that popular social media sites such as Facebook should be appraised to determine their roles in promoting cancer screening.
Using social media to recruit study patients has been described more frequently over the past few years (Carter-Harris, Bartlett Ellis, Warrick, Rawl, 2016b; Thompson, 2014). Carter-Harris and colleagues (2016b) found that using Facebook is considerably more cost effective than traditional recruiting methods such as newspaper advertisements. The authors posit that due to the stigma associated with smoking, current and former smokers may prefer the privacy and flexibility of social media (Carter-Harris et al., 2016b). Xu and colleagues (2016) discuss that knowledge and awareness of cancer vary widely among the US population and promoting knowledge about cancer should be focused among those with the highest cancer burden. Xu and colleagues (2016) explored the use of social media outlets to disseminate information about cancers and found that social media can be a powerful tool to circulate information to the community and may be able to reduce ethnic and racial disparities.
Health knowledge is a key component of health and allows patients to make informed choices (Kesanen, Leino-Kilpi, Arifulla, Siekkinen, & Valkeapaa, 2014). A systematic review of knowledge tools used in patient education found that most tests were health-problem related, with a mean of 20 true/false/multiple-choice questions specifically designed for the studies in the review (Kesanen et al., 2014).
There are several studies describing the use of educational sessions to improve patient knowledge of lung cancer screening. Rosenkrantz, Mason, Kunzler, and Lee (2016) describe educational sessions about image-based cancer screening and found that roughly 90% of respondents noted an increase in knowledge regarding screening. Mazzone and colleagues (2017) assessed changes in patient knowledge before and after viewing a 6-minute video about lung cancer screening and found that there was an increase in patient knowledge both immediately after viewing the video and 1 month following.
Another factor that may have an impact on the low uptake of lung cancer screening is motivation. Schapira and colleagues (2016) found that uncertainty felt by patients can impact their willingness to undergo lung cancer screening and that by decreasing uncertainty in patients, they may be motivated to undergo screening. One way to alleviate this uncertainty may be to increase patient knowledge.
Ali and colleagues (2015) sought to identify barriers to participation among patients at high risk for lung cancer. The authors found that women, current smokers, older patients, and those from lower socioeconomic groups were less willing to participate in lung cancer screening. Based on this information, strategies to customize educational programs for these subgroups may result in higher levels of motivation for screening.
Jonnalagadda and colleagues (2012) evaluated cognitive and affective beliefs about lung cancer among patients at high risk for lung cancer in relation to their intention to have screening and found that fatalistic beliefs, fear of radiation exposure, and anxiety related to CT scans were associated with decreased intention to screen. Therefore, education addressing these factors may increase patient motivation to pursue screening.
Motivation to have lung cancer screening has also been investigated by examining changes in intention to undergo lung cancer screening in Korean men after receiving information on the benefits and harms of LDCT (Nhung et al., 2015). Ninety-five percent of the participants indicated that they would pursue lung cancer screening after being educated on the benefits of screening and that screening intentions were stronger among current smokers.
SAMPLE
Inclusion criteria for this study were English-speaking adults living in the Commonwealth of Virginia who were between the ages of 55 and 77 and currently smoke or are former smokers who quit in the past 15 years. Exclusion criteria included people who were never smokers, underwent lung cancer screening with LDCT, or had been diagnosed and/or treated for lung cancer. Enrollment in the study was generated through a Facebook advertisement. Eligibility to participate was determined based on a brief online demographic survey. Enrollment remained open until at least 30 subjects completed the study.
DESIGN
This study was conducted using a pre-experimental, one-group pre-test and post-test design. This study was conducted via the internet, as the basis of the study is to determine the effectiveness of using social media for patient education. The two social media platforms that were utilized were Facebook and YouTube. Institutional review board approval was obtained from Old Dominion University.
INSTRUMENTS
Demographic variables collected included age, smoking status, gender, marital status, race, education, and health insurance coverage. The clinical variables included any history of lung cancer that precluded the subject from the study. Motivation to discuss screening with a health-care provider was also assessed. These variables were assessed using a combination of a researcher-designed form and the Lung Cancer Screening-12 (LCS-12).
The LCS-12 is a validated patient knowledge assessment tool that was developed specifically to assess change in knowledge after viewing a video-based decision aid about lung cancer screening (Lowenstein et al., 2016). The LCS-12 contains 12 questions. Each correct question is worth 1 point, and the maximum score is 12, which would indicate excellent knowledge of lung cancer screening. A score of 0 would indicate low knowledge of lung cancer screening. This tool is used with the permission of Dr. Robert Volk, the corresponding author.
PROCEDURES
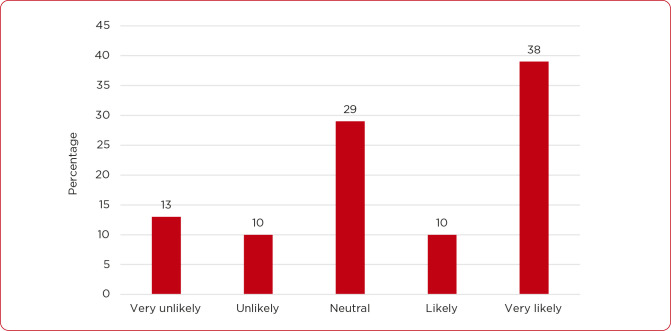
A Facebook advertisement (see Figure 1) was created to recruit potential subjects. Interested subjects clicked on a link within the advertisement that redirected them to a Facebook page containing details about the study, including general eligibility criteria. Potential subjects completed a brief questionnaire to determine eligibility and provide demographic information. Those who were eligible then completed the LCS-12 pre-test regarding their knowledge about lung cancer screening. Participants were directed to a brief educational video about lung cancer screening that was hosted on YouTube. After viewing the video, participants again completed the LCS-12 as a post-test to again assess their knowledge about screening. The final step asked participants to rate their motivation to discuss lung cancer screening with their health-care provider.
Figure 1.
The Facebook advertisement that was created to recruit potential subjects.
RESULTS
Thirty-one subjects who ranged in age from 55 to 74 with a median age of 59 (standard deviation [SD]: 5.44) completed the study. Table 1 lists participants’ sociodemographic characteristics.
Table 1. Demographic Characteristics of Sample.
| Demographic characteristics (n = 31) | n (%) |
|---|---|
| Between ages of 55–77 | |
| Yes | 31 (100) |
| Smoking status | |
| Current | 11 (35.5) |
| Former | 20 (64.5) |
| Quit after 2003 | 31 (100) |
| Have/had lung cancer | |
| Yes | 0 |
| Current age in years | |
| Mean | 60.9 |
| Median | 59 |
| Mode | 56 |
| Gender | |
| Female | 19 (61.3) |
| Male | 12 (38.7) |
| Marital status | |
| Married | 18 (58.1) |
| Divorced | 9 (29) |
| Widowed | 2 (6.5) |
| Unmarried | 2 (6.5) |
| Education | |
| High school | 5 (16.1) |
| Some college | 14 (45.2) |
| Bachelor’s | 7 (22.6) |
| Master’s | 4 (12.9) |
| Doctorate | 1 (3.2) |
| Health insurance | |
| Yes | 24 (77.4) |
| No | 7 (22.6) |
| Type of health insurance | |
| Medicare | 11 (35.5) |
| Other | 13 (41.9) |
| Not applicable | 7 (22.6) |
| Race | |
| Black | 1 (3.2) |
| White | 29 (93.5) |
| Other | 1 (3.2) |
DATA ANALYSIS
IBM SPSS Statistics Version 25 was used for data analysis. Scores for each subject from the pre- and post-test were compared to assess for a change in knowledge after watching the educational video. The paired t-test was used to determine whether a difference exists in the pre- and post-test scores for each subject. This statistical test was two-sided, with a significance level of α set to 0.05 a priori. The mean knowledge score before watching the educational presentation about lung cancer screening was 5.26 (SD: 2.93), and the mean knowledge score after receiving the education was 8.19 (SD: 2.01; see Table 2). The difference in knowledge was statistically significant as tested by the paired t-test (Table 3).
Table 2. Change in Mean Knowledge Score Before and After Education.
| Mean | N | Standard deviation | Standard error mean | |
|---|---|---|---|---|
| Pre-test score | 5.26 | 31 | 2.932 | .527 |
| Post-test score | 8.19 | 31 | 2.007 | .360 |
Table 3. Difference in Knowledge Score (Paired Differences).
| Mean | Standard deviation | Standard error mean | 96% confidence interval of the difference | t | df | Sig. (2-tailed) | ||
|---|---|---|---|---|---|---|---|---|
| Lower |
Upper |
|||||||
| Pre-test and post-test scores | –2.935 | 2.744 | .493 | –3.942 | –1.929 | –5.956 | 30 | .000 |
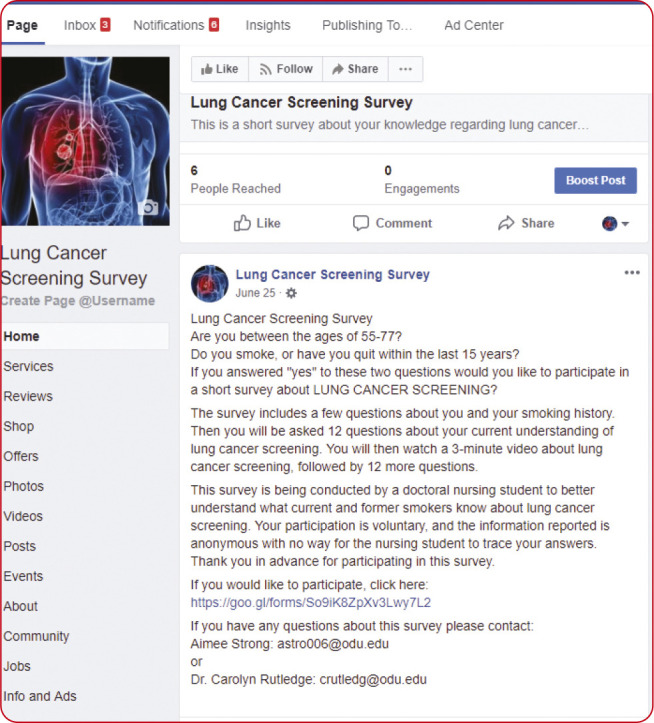
Level of motivation to discuss lung cancer screening with their health-care provider after viewing a lung cancer screening program on social media was also assessed using a Likert scale. Responses to this question were analyzed using descriptive statistics, including mean, mode, and SD. Subjects ranked their motivation to discuss lung cancer screening with their health-care provider on a scale of 1 to 5, with 1 being “very unlikely” and 5 being “very likely.” The mean motivation level was 3.52 with a mode of 5 and SD of 1.43 (Figure 2).
Figure 2.
Level of motivation to discuss screening with provider (n = 31).
DISCUSSION
The data show that social media can be used as a platform for educating patients about lung cancer screening. By raising awareness of not only lung cancer screening but other health screenings, providers can ultimately decrease morbidity and mortality through early detection and early treatment. Patients who receive education on cancer screenings are in a better position to make an informed decision about their health care.
LIMITATIONS
Limitations of this study include a small sample size, participants were primarily Caucasian, and had an above-average level of education. The study was conducted over a 10-week period, limiting the ability to collect a more robust and diverse sample. The data were collected in one geographical location, although social media would allow for national representation.
IMPLICATIONS AND DISCUSSION
This study supports using social media to educate patients. By using the advertising metrics in Facebook, providers can target specific patient populations based on age, gender, interests, and location. Patients are able to view this information in the privacy of their own home and at their leisure.
Increasing awareness of lung cancer screening through social media may be a way to generate conversations between patients and their health-care providers. As the use of social media has become an integral part of people’s lives, patients may feel more comfortable having a conversation about lung cancer screening after seeing it on their Facebook feed, especially if they saw it on their health-care provider’s Facebook page. If a provider’s office is using social media to talk about lung cancer screening, then the provider can use this as an opportunity to address the topic with high-risk patients in the office. This may be another way to harness social media to improve uptake in lung cancer screening.
This study presents several opportunities for further research. Many respondents to the Facebook advertisement were female (61%). Future studies could explore whether gender is a factor in viewing health education on social media. Education level is also an area for future study, as 84% of the subjects in this current study had more than a high school education. Race and ethnicity is also an area for future research. Subjects in this study were predominantly white (94%). Future research could investigate using social media to target minority populations to improve access to health information and thereby improve access to care.
This study also evaluated subjects’ motivation to discuss lung cancer screening with their health-care providers after viewing an educational video on social media. The results show that despite having an increase in knowledge about lung cancer screening, subjects were not very motivated to discuss screening with their providers. One factor that may have influenced subjects’ motivation is that 64.5% of respondents were former smokers. This population may be less motivated to pursue lung cancer screening since they no longer smoke and may have a false sense of security that they are no longer at risk for lung cancer. While the relative risk of lung cancer decreases within 5 years since quitting, it remains more than 3-fold higher than in never smokers after 25 years since quitting (Tindle et al., 2018). Therefore, it is important to educate former smokers on their continued risk for lung cancer and the role of lung cancer screening.
An additional factor related to the level of motivation to discuss lung cancer screening with a health-care provider could be the stigma associated with lung cancer. According to Cataldo and Brodsky (2013), lung cancer patients reported the highest levels of stigma and related psychological distress compared to patients with other cancers. Carter-Harris (2015) found an association between lung cancer stigma and delayed medical help-seeking behaviors. This potential barrier can result in patients not getting screened for lung cancer and presenting with late-stage disease and worse survival. As advanced practitioners, we are often the point of contact for high-risk patients and can educate our patients about their cancer risk. Advanced practitioners can be integral in decreasing the stigma associated with lung cancer by identifying our own implicit biases around smoking, educating our patients and the public about lung cancer, and engaging our legislatures to support lung cancer research.
CONCLUSION
This study shows that, at the very least, social media can be used to improve the knowledge of lung cancer screening. The potential for social media to engage high-risk patients in all aspects of lung cancer screening is limitless and represents an exciting opportunity to impact the health of a vulnerable population.
Footnotes
The authors have no conflicts of interest to disclose.
References
- Aberle D. R., DeMello S., Berg C. D., Black W. C., Brewer B., Church T. R.,...Sicks J. (2013). Results of the two incidence screenings in the National Lung Screening Trial. New England Journal of Medicine, 369(10), 920–931. 10.1056/NEJMoa1208962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali N., Lifford K. J., Carter B., McRonald F., Yadegarfar G., Baldwin D. R.,…Brain K. (2015). Barriers to uptake among high-risk individuals declining participation in lung cancer screening: A mixed methods analysis of the UK Lung Cancer Screening (UKLS) trial. BMJ Open, 5(7), e008254 10.1136/bmjopen-2015-008254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society (2020). Facts & Figures 2020. Retrieved from https://www.cancer.org/cancer/non-small-cell-lung-cancer/about/key-statistics.html
- Cardarelli R., Reese D., Roper K. L., Cardarelli K., Feltner F. J., Studts J. L.,...Shaffer D. (2017). Terminate lung cancer (TLC) study—A mixed-methods population approach to increase lung cancer screening awareness and low-dose computed tomography in eastern Kentucky. Cancer Epidemiology, 46, 1–8. 10.1016/j.canep.2016.11.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter-Harris L. (2015). Lung cancer stigma as a barrier to medical help-seeking behavior: Practice implications. Journal of the American Association of Nurse Practitioners, 27(5), 240–5. 10.1002/2327-6924.12227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter-Harris L., Bartlett Ellis R., Warrick A., & Rawl S. (2016b). Beyond traditional newspaper advertisement: Leveraging Facebook-targeted advertisement to recruit long-term smokers for research. Journal of Medical Internet Research, 18(6), e117 10.2196/jmir.5502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter-Harris L., Tan A. S., Salloum R. G., & Young-Wolff K. C. (2016a). Patient-provider discussions about lung cancer screening pre- and post-guidelines: Health information national trends survey (HINTS). Patient Education and Counseling, 99(11), 1772–1777. 10.1016/j.pec.2016.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cataldo J. K., & Brodsky J. L. (2013). Lung cancer stigma, anxiety, depression and symptom severity. Oncology, 85(1), 33–40. 10.1159/000350834 [DOI] [PubMed] [Google Scholar]
- Jemal A., & Fedewa S. A. (2017). Lung cancer screening with low-dose computed tomography in the United States—2010 to 2015. JAMA Oncology, 3(9), 1278–1281. 10.1001/jamaoncol.2016.6416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonnalagadda S., Bergamo C., Lin J. J., Lurslurchachai L., Diefenbach M., Smith C.,...Wisnivesky J. P. (2012). Beliefs and attitudes about lung cancer screening among smokers. Lung Cancer, 77(3), 526–531. 10.1016/j.lungcan.2012.05.095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kesanen J., Leino-Kilpi H., Arifulla D., Siekkinen M., & Valkeapaa K. (2014). Knowledge tests in patient education: A systematic review. Nursing & Health Sciences, 16(2), 262–273. 10.1111/nhs.12097 [DOI] [PubMed] [Google Scholar]
- Koskan A., Klasko L., Davis S. N., Gwede C. K., Wells K. J., Kumar A.,...Meade C. D. (2014). Use and taxonomy of social media in cancer-related research: A systematic review. American Journal of Public Health, 104(7), e20–e37. 10.2105/ajph.2014.301980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowenstein L. M., Richards V. F., Leal V. B., Housten A. J., Bevers T. B., Cantor S. B.,...Volk R. J. (2016). A brief measure of Smokers’ knowledge of lung cancer screening with low-dose computed tomography. Preventive Medicine Reports, 4, 351–356. 10.1016/j.pmedr.2016.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazzone P. J., Tenenbaum A., Seeley M., Petersen H., Lyon C., Han X., & Wang X. F. (2017). Impact of a lung cancer screening counseling and shared decision-making visit. Chest, 151(3), 572–578. 10.1016/j.chest.2016.10.027 [DOI] [PubMed] [Google Scholar]
- Nhung B. C., Lee Y. Y., Yoon H., Suh M., Park B., Jun J. K.,...Choi K. S. (2015). Intentions to undergo lung cancer screening among Korean men. Asian Pacific Journal of Cancer Prevention, 16(15), 6293–6298. [DOI] [PubMed] [Google Scholar]
- Prochaska J. J., Coughlin S. S., & Lyons E. J. (2017). Social media and mobile technology for cancer prevention and treatment. American Society of Clinical Oncology Educational Book, 37, 128–137. 10.14694/edbk_173841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Retrouvey M., Patel Z., & Shaves S. (2016). US Preventive Services Task Force CT lung cancer screening recommendations: Community awareness and perceptions. Journal of the American College of Radiology, 13(2 suppl), R35–R37. 10.1016/j.jacr.2015.12.011 [DOI] [PubMed] [Google Scholar]
- Rosenkrantz A. B., Mason D., Kunzler N. M., & Lee J. (2016). The radiologist as direct public educator: Impact of sessions demystifying select cancer screening imaging examinations. Journal of the American College of Radiology, 13(2 suppl), R38–R42. 10.1016/j.jacr.2015.12.012 [DOI] [PubMed] [Google Scholar]
- Schapira M. M., Aggarwal C., Akers S., Aysola J., Imbert D., Langer C., & Fraenkel L. (2016). How patients view lung cancer screening. The role of uncertainty in medical decision making. Annals of the American Thoracic Society, 13(11), 1969–1976. 10.1513/AnnalsATS.201604-290OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson M. A. (2014). Social media in clinical trials. American Society of Clinical Oncology Educational Book, 24, e101–e105. 10.14694/EdBook_AM.2014.34.e101 [DOI] [PubMed] [Google Scholar]
- Tindle H. A., Stevenson Duncan M., Greevy R. A., Vasan R. S., Kundu S., Massion P. P., & Freiberg M. S. (2018). Lifetime smoking history and risk of lung cancer: Results From the Framingham Heart Study. Journal of the National Cancer Institute, 110(11), 1201–1207. 10.1093/jnci/djy041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Preventive Services Task Force (2013). U.S. Preventive Services Task Force (USPSTF). Rockville, MD: U.S. Department of Health & Human Services, Agency for Healthcare Research and Quality
- Xu S., Markson C., Costello K. L., Xing C. Y., Demissie K., & Llanos A. A. (2016). Leveraging social media to promote public health knowledge: example of cancer awareness via Twitter. JMIR Public Health Surveillance, 2(1), e17 10.2196/publichealth.5205 [DOI] [PMC free article] [PubMed] [Google Scholar]