Abstract
Background:
Cyclooxygenase-2 (COX-2) has been found to be important for fracture-healing in animal models, raising concerns about use of nonsteroidal anti-inflammatory drugs (NSAIDs) and selective COX-2 inhibitors after fractures. We evaluated associations of NSAIDs, COX-2 inhibitors, and opioids with nonunion after long-bone fracture.
Methods:
Using private health insurance claims data from Optum’s de-identified Clinformatics Data Mart database from January 1, 2000, to September 30, 2015, we identified adults with a single long-bone fracture or commonly paired long-bone fractures who had 1 year of available follow-up data. Using multivariable logistic regression models, we examined associations between NSAID, COX-2-inhibitor, or opioid prescription fills after the fracture and the risk of nonunion within 1 year, defined as a nonunion diagnosis with a procedure to treat the nonunion.
Results:
A nonunion diagnosis with a procedure to treat the nonunion was identified after 2,996 (0.9%) of the 339,864 fracture episodes, with rates varying by fracture site. The risk of that outcome was greater in patients who had filled COX-2-inhibitor prescriptions (adjusted odds ratio = 1.84 [95% confidence interval = 1.38 to 2.46]) or opioid prescriptions (1.69 [1.53 to 1.86]), but not in patients who had filled nonselective-NSAID prescriptions (1.07 [0.93 to 1.23]) after the fracture. Results were similar when the outcome definition was changed to just a nonunion diagnosis.
Conclusions:
COX-2 inhibitors, but not nonselective NSAIDs, were associated with a greater risk of nonunion after fracture. Opioids were also associated with nonunion risk, although patients filling prescriptions for opioids may have had more severe fractures.
Level of Evidence:
Therapeutic Level III. See Instructions for Authors for a complete description of levels of evidence.
Nonunion, a failure of the fracture-healing process, is a major complication that occurs after approximately 2% to 10% of fractures1-5. Fracture location, energy of injury, soft-tissue involvement, and comorbidities influence the risk of nonunion1-3. The contribution of medications to nonunion risk has been of particular interest.
Numerous animal studies have demonstrated that cyclooxygenase-2 (COX-2) is important for fracture-healing6-13, raising concerns about the use of nonsteroidal anti-inflammatory drugs (NSAIDs), which inhibit both COX-1 and COX-2, and the use of selective COX-2 inhibitors. Some, but not all, animal studies have suggested that selective COX-2 inhibitors might impair bone-healing more than nonselective NSAIDs6,9,11. Human studies have yielded conflicting results, and few have evaluated nonselective NSAIDs and COX-2 inhibitors separately1,4,14-20. With heightened awareness of opioid risks, a clearer understanding of the safety of alternative, non-opioid analgesics after fracture is critical.
The purpose of this study was to assess whether use of nonselective NSAIDs or selective COX-2 inhibitors is associated with the risk of nonunion. We also evaluated the risk associated with opioids, hypothesizing a high likelihood of confounding.
Materials and Methods
We conducted a cohort study using Optum’s de-identified Clinformatics Data Mart database to examine claims data from January 1, 2000, to September 30, 2015. Optum’s database is a de-identified administrative private health insurance claims database with sociodemographic, inpatient, outpatient, and prescription claims for >60 million members across the United States.
Cohort Identification
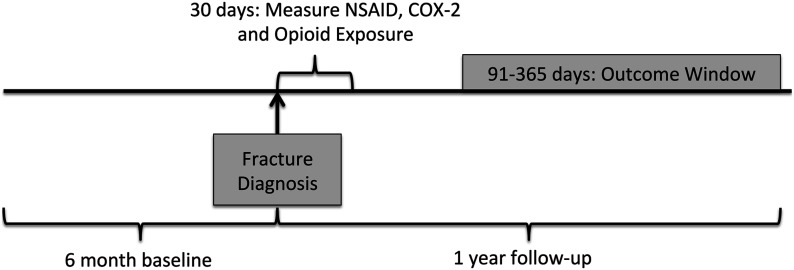
We identified adults ≥18 years old with an inpatient or outpatient International Classification of Diseases, Ninth Revision (ICD-9) diagnosis of fracture of the neck of the femur, another femoral location, the tibia, the fibula, the tibia and fibula, the radius, the ulna, the radius and ulna, the humerus, or the clavicle (see Appendix Table E-1). We focused on these long-bone fractures because nonunion in these regions would be the most symptomatic and likely to receive additional intervention. To ensure that outcomes would be attributable to the fracture of interest, we excluded patients with multiple fractures of these types within 7 days before or after the index date. We also excluded patients with 1 of these fracture diagnoses in the prior year to avoid overlapping outcome windows; patients could contribute multiple fracture episodes if they were >1 year apart. We required ≥6 months of continuous baseline enrollment prior to the fracture and 1 year of continuous enrollment after the fracture to capture outcomes (Fig. 1). We excluded patients with other fracture diagnoses in the year prior to or within 7 days after the index date, patients with bone or metastatic cancer during the baseline period or on the fracture date, and those with a diagnosis of nonunion or malunion in the year prior to the fracture date or in the 90 days after the fracture date, as nonunion would not be expected this soon after a fracture.
Fig. 1.
Study design. Exposure was measured on the basis of prescription fills in a period beginning on the fracture date and ending 30 days after it. Patients with a diagnosis of nonunion or malunion within 90 days after surgery were excluded as nonunion would not be expected this early after fracture. The outcome of nonunion was measured from 91 to 365 days after fracture.
Exposures
We ascertained whether patients filled prescriptions for nonselective NSAIDs, selective COX-2 inhibitors, and/or opioids on the fracture date or in the 30 subsequent days. We also ascertained whether patients filled prescriptions for these medications within 90 days before the fracture date to identify new versus continuing users.
Outcomes
We used 2 nonunion definitions for our evaluations. The primary definition was an inpatient or outpatient ICD-9 diagnosis code for nonunion (733.82) in the 91 to 365 days after the initial fracture diagnosis with a procedure to treat nonunion (surgery, bone-grafting, or electrical bone stimulation) within the 30 days after the diagnosis of nonunion (see Appendix Table E-1) to minimize misclassification and to capture the most clinically relevant nonunions. We also evaluated end points identified using a secondary definition consisting of just an inpatient or outpatient diagnosis of nonunion, which has been shown to have a positive predictive value of 89%21.
Covariates
We ascertained the following covariates, defined in Appendix Table E-1: age, sex, geographical region, year, filled prescriptions for glucocorticoids or anticoagulants in the 90 days prior to the fracture, energy of the injury based on energy codes (high, low, other, or no energy code) in the 3 days before or 7 days after the fracture22, fracture location, open versus closed fracture, initial treatment (none, closed reduction, external fixation, open reduction, open reduction and internal fixation, or percutaneous), location (outpatient, emergency department, or inpatient), and patient comorbidities based on diagnoses in the 6-month baseline period (see Appendix).
Statistical Analysis
We first identified patients who had not filled a prescription for a nonselective NSAID or a COX-2 inhibitor within 90 days prior to the fracture. We then analyzed that group to compare baseline characteristics between patients filling and those not filling a prescription for one of these medications in the 30 days after the fracture. We did this using standardized mean differences, considering an absolute value of ≥0.1 as evidence of meaningful covariate imbalance23. We calculated the crude frequency of nonunion according to both definitions in unexposed patients, those filling a nonselective NSAIDs prescription, and those filling a COX-2 inhibitor prescription as mutually exclusive groups (excluding patients filling both NSAIDs and COX-2 inhibitors). We then performed univariate and multivariable logistic regression adjusting for all measured covariates (including a squared term for age to account for nonlinearity) as well as opioid prescription fills in the 30 days after the fracture and in the 90 days before the fracture, with cluster robust standard errors to account for patients (<5%) contributing multiple fractures24.
We performed analogous analyses to assess associations between baseline characteristics and opioid exposure, limiting analyses to patients who had not filled an opioid prescription within 90 days prior to their fracture. Again, we adjusted for all measured covariates as well as NSAID or COX-2 prescription fills in the 30 days after and 90 days before the fracture.
We conducted several sensitivity analyses. We evaluated interactions between exposure and year categories (2001 to 2005, 2006 to 2010, and 2011 to 2015) and then performed analyses stratified by these time frames. We also assessed interactions between exposure and fracture location and performed subgroup analyses among patients with a tibial or tibial and fibular fracture, those with a distal femoral fracture, and those with a femoral neck fracture. We also explored the impact of filling multiple prescriptions in analyses that categorized exposure as no prescriptions, 1 prescription, or ≥2 prescriptions in the 60 days after the fracture.
Analyses were performed using Stata, version 15.0 (StataCorp). The study was considered exempt by the University of Pennsylvania’s institutional review board.
Results
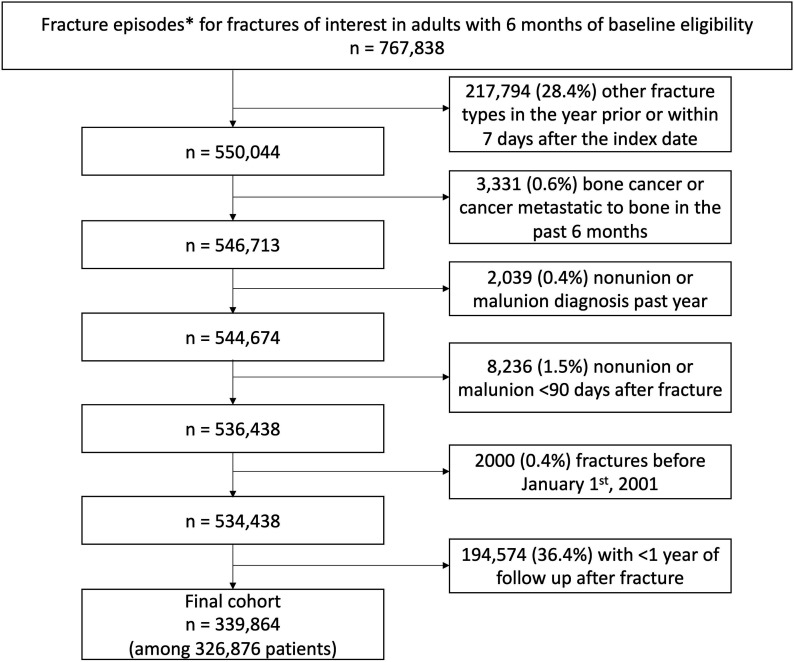
We identified 767,838 fracture episodes among adults with at least 6 months of preceding baseline eligibility (Fig. 2). After applying exclusions there were 339,864 fracture episodes among 326,876 patients.
Fig. 2.
Cohort creation. *Fracture episodes were defined by the presence of a diagnosis for 1 of the fractures of interest, excluding patients with multiple different fracture types within 7 days or with a prior diagnosis for 1 of these fractures within the past year.
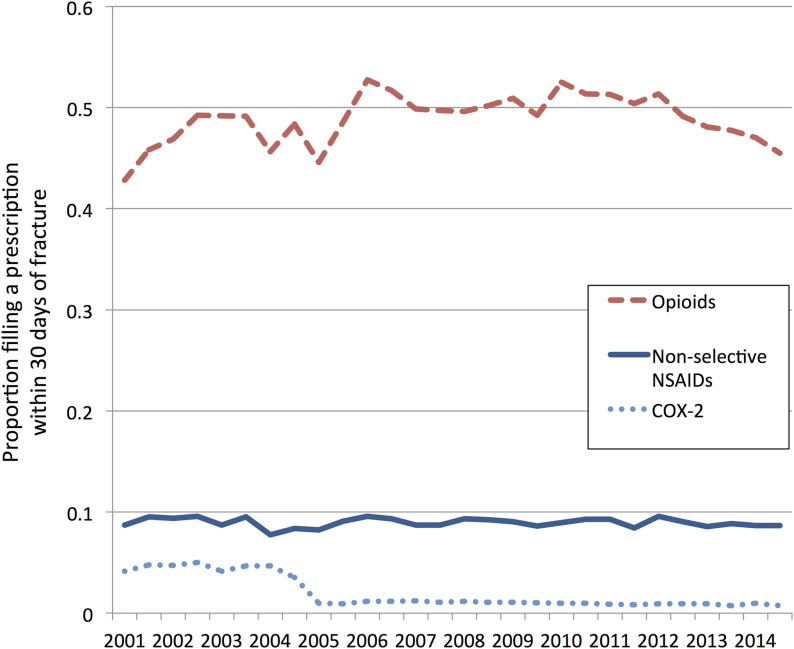
Of 304,721 episodes in patients with no prior NSAID or COX-2 prescriptions, 22,590 (7.4%) were followed by the filling of an NSAID prescription and 2,411 (0.8%) were followed by the filling of a COX-2-inhibitor prescription within 30 days after the fracture. As shown in Figure 3, nonselective-NSAID fills were stable over the study period, while COX-2-inhibitor fills were most common from 2001 to 2004. Patients who filled prescriptions for NSAIDs or a COX-2 inhibitor were younger; more likely to be male; less likely to have a femoral neck fracture; more likely to have a high-energy injury; more likely to be treated as an outpatient and have no surgical treatment for their fracture; less likely to have comorbidities such as cardiac disease, hypertension, kidney disease, and diabetes; and less likely to have received an anticoagulant (Table I).
Fig. 3.
Trends in fills of prescriptions for nonselective NSAIDs, COX-2 inhibitors, and opioids over time after the fractures. The graph shows the proportion of patients with no opioid prescription in the 90 days prior to the fracture who filled an opioid prescription within 30 days after the fracture and the proportions with no NSAID or COX-2-inhibitor prescription in the 90 days prior to the fracture who filled an NSAID or COX-2-inhibitor prescription within 30 days after the fracture.
TABLE I.
Cohort Characteristics
| No NSAID/COX-2 Prescription in the 90 Days Prior to Fracture | No Opioid Prescription in the 90 Days Prior to Fracture | |||||
| No NSAID or COX-2 Within 30 Days After Fracture* (N = 279,720) | NSAID or COX-2 Within 30 Days After Fracture* (N = 25,001) | SMD† | No Opioid Within 30 Days After Fracture* (N = 146,034) | Opioid Within 30 Days After Fracture* (N = 123,807) | SMD† | |
| Demographics | ||||||
| Age (yr) | 59.7 ± 19.2 | 49.1 ± 16.9 | −0.59 | 61.8 ± 19.4 | 54.5 ± 18.6 | −0.39 |
| Female | 176,717 (63.2%) | 13,772 (55.1%) | −0.17 | 92,247 (63.2%) | 74,548 (60.2%) | −0.06 |
| U.S. geographic division | ||||||
| East North Central | 39,262 (14.0%) | 3,557 (14.2%) | 0.01 | 19,923 (13.6%) | 18,414 (14.9%) | 0.04 |
| East South Central | 10,640 (3.8%) | 981 (3.9%) | 0.01 | 4,749 (3.3%) | 5,061 (4.1%) | 0.04 |
| Middle Atlantic | 15,863 (5.7%) | 1,464 (5.9%) | 0.01 | 10,389 (7.1%) | 5,996 (4.8%) | −0.10 |
| Mountain | 31,664 (11.3%) | 2,266 (9.1%) | −0.08 | 14,853 (10.2%) | 14,124 (11.4%) | 0.04 |
| New England | 12,010 (4.3%) | 1,039 (4.2%) | −0.01 | 7,347 (5.0%) | 4,579 (3.7%) | −0.07 |
| Pacific | 33,737 (12.1%) | 2,572 (10.3%) | −0.06 | 17,662 (12.1%) | 13,714 (11.1%) | −0.03 |
| South Atlantic | 61,880 (22.1%) | 6,866 (27.5%) | 0.12 | 31,201 (21.4%) | 29,593 (23.9%) | 0.06 |
| West North Central | 40,284 (14.4%) | 2,311 (9.2%) | −0.16 | 24,423 (16.7%) | 14,824 (12.0%) | −0.14 |
| West South Central | 32,710 (11.7%) | 3,861 (15.4%) | 0.11 | 14,639 (10.0%) | 16,906 (13.7%) | 0.11 |
| Unknown | 1,670 (0.6%) | 84 (0.3%) | −0.04 | 848 (0.6%) | 596 (0.5%) | −0.01 |
| Fracture characteristics | ||||||
| Fracture location | ||||||
| Radius | 77,695 (27.8%) | 8,236 (32.9%) | 0.11 | 39,642 (27.1%) | 38,442 (31.0%) | 0.09 |
| Neck of femur | 57,711 (20.6%) | 1,396 (5.6%) | −0.46 | 37,463 (25.7%) | 13,166 (10.6%) | −0.40 |
| Humerus | 51,178 (18.3%) | 4,930 (19.7%) | 0.04 | 21,629 (14.8%) | 27,587 (22.3%) | 0.19 |
| Clavicle | 21,841 (7.8%) | 3,488 (14.0%) | 0.20 | 9,201 (6.3%) | 13,730 (11.1%) | 0.17 |
| Tibia | 20,441 (7.3%) | 2,020 (8.1%) | 0.03 | 11,139 (7.6%) | 8,396 (6.8%) | −0.03 |
| Fibula | 13,977 (5.0%) | 1,498 (6.0%) | 0.04 | 8,272 (5.7%) | 5,304 (4.3%) | −0.06 |
| Ulna | 13,021 (4.7%) | 1,598 (6.4%) | 0.08 | 7,082 (4.8%) | 6,100 (4.9%) | 0.00 |
| Radius and ulna | 9,569 (3.4%) | 963 (3.9%) | 0.02 | 3,959 (2.7%) | 5,730 (4.6%) | 0.10 |
| Femur | 8,396 (3.0%) | 433 (1.7%) | −0.08 | 4,952 (3.4%) | 2,362 (1.9%) | −0.09 |
| Tibia and fibula | 5,891 (2.1%) | 439 (1.8%) | −0.03 | 2,695 (1.8%) | 2,990 (2.4%) | 0.04 |
| Open fracture | 15,945 (5.7%) | 1,056 (4.2%) | −0.07 | 7,534 (5.2%) | 7,809 (6.3%) | 0.05 |
| Energy of injury | ||||||
| Low | 46,110 (16.5%) | 3,691 (14.8%) | −0.05 | 20,901 (14.3%) | 23,747 (19.2%) | 0.13 |
| High | 24,455 (8.7%) | 3,662 (14.6%) | 0.19 | 7,752 (5.3%) | 18,576 (15.0%) | 0.33 |
| Other | 35,073 (12.5%) | 2,569 (10.3%) | −0.07 | 17,177 (11.8%) | 15,916 (12.9%) | 0.03 |
| No energy code | 174,082 (62.2%) | 15,079 (60.3%) | −0.04 | 100,204 (68.6%) | 65,568 (53.0%) | −0.33 |
| Location | ||||||
| Outpatient | 151,267 (54.1%) | 17,483 (69.9%) | 0.33 | 83,095 (56.9%) | 67,094 (54.2%) | −0.06 |
| Emergency department | 47,667 (17.0%) | 4,677 (18.7%) | 0.04 | 20,446 (14.0%) | 26,388 (21.3%) | 0.19 |
| Inpatient | 80,786 (28.9%) | 2,841 (11.4%) | −0.45 | 42,493 (29.1%) | 30,325 (24.5%) | −0.10 |
| Treatment | ||||||
| None | 247,725 (88.6%) | 24,000 (96.0%) | 0.28 | 128,159 (87.8%) | 113,842 (92.0%) | 0.14 |
| Closed reduction | 3,309 (1.2%) | 157 (0.6%) | −0.06 | 1,910 (1.3%) | 1,008 (0.8%) | −0.05 |
| External fixation | 23,197 (8.3%) | 638 (2.6%) | −0.26 | 12,715 (8.7%) | 7,339 (5.9%) | −0.11 |
| Open reduction and internal fixation | 4,005 (1.4%) | 146 (0.6%) | −0.09 | 2,366 (1.6%) | 1,227 (1.0%) | −0.06 |
| Open reduction | 421 (0.2%) | 15 (0.1%) | −0.03 | 252 (0.2%) | 103 (0.1%) | −0.03 |
| Percutaneous | 1,063 (0.4%) | 45 (0.2%) | −0.04 | 632 (0.4%) | 288 (0.2%) | −0.04 |
| Comorbidities | ||||||
| Anxiety | 22,910 (8.2%) | 2,098 (8.4%) | 0.01 | 10,024 (6.9%) | 8,952 (7.2%) | 0.01 |
| Depression | 32,494 (11.6%) | 2,586 (10.3%) | −0.04 | 14,541 (10.0%) | 12,099 (9.8%) | −0.01 |
| Chronic pain | 16,021 (5.7%) | 1,329 (5.3%) | −0.02 | 6,146 (4.2%) | 4,765 (3.8%) | −0.02 |
| Coronary artery disease | 34,672 (12.4%) | 1,449 (5.8%) | −0.23 | 18,308 (12.5%) | 10,024 (8.1%) | −0.15 |
| Congestive heart failure | 18,057 (6.5%) | 451 (1.8%) | −0.24 | 9,699 (6.6%) | 4,011 (3.2%) | −0.16 |
| Obesity | 11,397 (4.1%) | 1,042 (4.2%) | 0.01 | 4,786 (3.3%) | 4,630 (3.7%) | 0.03 |
| Peptic ulcer disease | 3,102 (1.1%) | 145 (0.6%) | −0.06 | 1,389 (1.0%) | 902 (0.7%) | −0.02 |
| End-stage renal disease | 1,571 (0.6%) | 22 (0.1%) | −0.08 | 667 (0.5%) | 345 (0.3%) | −0.03 |
| Alcoholism | 1,960 (0.7%) | 201 (0.8%) | 0.01 | 780 (0.5%) | 877 (0.7%) | 0.02 |
| Diabetes | 38,609 (13.8%) | 2,164 (8.7%) | −0.16 | 19,297 (13.2%) | 13,424 (10.8%) | −0.07 |
| Osteoporosis | 13,161 (4.7%) | 522 (2.1%) | −0.15 | 7,279 (5.0%) | 4,040 (3.3%) | −0.09 |
| Hypertension | 94,042 (33.6%) | 5,266 (21.1%) | −0.29 | 49,534 (33.9%) | 32,162 (26.0%) | −0.17 |
| Chronic kidney disease | 17,566 (6.3%) | 499 (2.0%) | −0.22 | 8,782 (6.0%) | 4,284 (3.5%) | −0.12 |
| Chronic obstructive pulmonary disease | 17,406 (6.2%) | 674 (2.7%) | −0.17 | 8,205 (5.6%) | 4,701 (3.8%) | −0.09 |
| Asthma | 9,567 (3.4%) | 761 (3.0%) | −0.02 | 4,331 (3.0%) | 3,515 (2.8%) | −0.01 |
| Cerebrovascular disease | 8,897 (3.2%) | 280 (1.1%) | −0.14 | 5,083 (3.5%) | 2,199 (1.8%) | −0.11 |
| Osteoarthritis | 29,841 (10.7%) | 1,684 (6.7%) | −0.14 | 14,847 (10.2%) | 8,132 (6.6%) | −0.13 |
| Rheumatoid arthritis | 3,961 (1.4%) | 189 (0.8%) | −0.06 | 1,844 (1.3%) | 1,271 (1.0%) | −0.02 |
| Medications within 90 days before fracture | ||||||
| NSAIDs | 0 (0%) | 0 (0%) | 0.00 | 7,245 (5.0%) | 6,982 (5.6%) | 0.03 |
| Selective COX-2 inhibitor | 0 (0%) | 0 (0%) | 0.00 | 1,880 (1.3%) | 1,915 (1.5%) | 0.02 |
| Opioid | 49,012 (17.5%) | 3,795 (15.2%) | −0.06 | 0 (0%) | 0 (0%) | 0.00 |
| Anticoagulant | 11,101 (4.0%) | 233 (0.9%) | −0.20 | 4,484 (3.1%) | 3,155 (2.5%) | −0.03 |
| Glucocorticoids | 12,832 (4.6%) | 1,067 (4.3%) | −0.02 | 4,493 (3.1%) | 5,107 (4.1%) | 0.06 |
Except for age, which is given as the mean and standard deviation, the values are given as the number of fractures with the percentage in parentheses.
SMD = standardized mean difference or standardized difference in proportions, with an SMD of ≥0.1 indicating imbalance in the covariate (indicated in bold).
Of 269,841 episodes in patients with no prior opioid use, 123,807 (45.9%) were followed by the filling of an opioid prescription within 30 days after the fracture. Opioid fills increased from 2001 to 2010 and declined from 2010 to 2015 (Fig. 3). Patients who filled prescriptions for opioids were younger, less likely to have a femoral neck fracture, more likely to have a high-energy or low-energy injury (compared with no energy code), and more likely to be treated in the emergency department than those who did not fill an opioid prescription (Table I). Differences in comorbidities were less pronounced than those between patients filling and patients not filling NSAID prescriptions.
A nonunion diagnosis and a procedure to treat the nonunion had occurred within 1 year after 2,996 (0.9%) of the fracture episodes, with rates ranging from 0.3% for radius fractures to 4.1% for fractures of both the tibia and the fibula (Table II). Nonunion diagnoses were made within 1 year after 5,471 (1.6%) of the episodes, with rates ranging from 0.5% for radial fractures to 5.9% for fractures of the tibia and fibula.
TABLE II.
Frequency of Nonunion by Fracture Location
| Fracture Location | No. | Nonunion Diagnosis and Procedure to Treat* | Nonunion Diagnosis* |
| Radius | 94,939 | 256 (0.3%) | 499 (0.5%) |
| Neck of femur | 65,434 | 346 (0.5%) | 1,054 (1.6%) |
| Humerus | 62,811 | 713 (1.1%) | 1,243 (2.0%) |
| Clavicle | 27,361 | 464 (1.7%) | 771 (2.8%) |
| Tibia | 26,683 | 259 (1.0%) | 400 (1.5%) |
| Fibula | 17,618 | 119 (0.7%) | 206 (1.2%) |
| Ulna | 16,243 | 140 (0.9%) | 254 (1.6%) |
| Radius and ulna | 11,422 | 125 (1.1%) | 186 (1.6%) |
| Femur | 10,296 | 282 (2.7%) | 445 (4.3%) |
| Tibia and fibula | 7,057 | 292 (4.1%) | 413 (5.9%) |
| Total | 339,864 | 2,996 (0.9%) | 5,471 (1.6%) |
The values are given as the number of fractures with the percentage in parentheses.
NSAID, COX-2, and Opioid Prescriptions After Fracture and the Risk of Nonunion
As shown in Table III, the filling of nonselective-NSAID prescriptions after fracture was not associated with nonunion in adjusted analyses using either nonunion-outcome definition, with an adjusted odds ratio (aOR) of 1.07 (95% confidence interval [CI] = 0.93 to 1.23] for a nonunion diagnosis plus procedure and an aOR of 1.08 (95% CI = 0.96 to 1.20) for a nonunion diagnosis alone. COX-2-inhibitor prescription fills, however, were associated with a greater risk of a nonunion diagnosis plus procedure (aOR = 1.84 [95% CI = 1.38 to 2.46]) and of a nonunion diagnosis alone (aOR = 1.48 [95% CI = 1.16 to 1.89]). Opioid prescription fills were also associated with a greater risk of nonunion, which was partially but not fully attenuated in adjusted models (unadjusted OR = 2.71 [95% CI = 2.48 to 2.96] and aOR = 1.69 [95% CI = 1.53 to 1.86] for nonunion diagnosis plus procedure; unadjusted OR = 2.05 [95% CI = 1.92 to 2.18] and aOR = 1.53 [95% CI = 1.43 to 1.64] for nonunion diagnosis alone). Unadjusted analyses and full models are shown in Appendix Tables E-2, E-3, and E-4.
TABLE III.
Association Between Nonselective NSAIDs, COX-2 Inhibitors, and Opioids with Nonunion
| No. | Nonunion Diagnosis and Procedure to Treat | Nonunion Diagnosis | |||
| Nonunion (no. [%]) | aOR* (95% CI) | Nonunion (no. [%]) | aOR* (95% CI) | ||
| NSAID/COX-2 analysis† | |||||
| Neither | 279,720 | 2,250 (0.8%) | Reference | 4,188 (1.5%) | Reference |
| Nonselective NSAID | 22,590 | 236 (1.0%) | 1.07 (0.93-1.23) | 387 (1.7%) | 1.08 (0.96-1.20) |
| COX-2 | 2,411 | 51 (2.1%) | 1.84 (1.38-2.46) | 69 (2.9%) | 1.48 (1.16-1.89) |
| Opioid analysis‡ | |||||
| No opioid | 146,034 | 702 (0.5%) | Reference | 1,513 (1.0%) | Reference |
| Opioid | 123,807 | 1,599 (1.3%) | 1.69 (1.53-1.86) | 2,600 (2.1%) | 1.53 (1.43-1.64) |
Adjusted odds ratios (aORs) are from multivariable logistic regression models with all covariates of interest.
NSAID/COX-2 analyses excluded patients with NSAID or COX-2 prescription fills within 90 days prior to the fracture and were adjusted for current and previous opioid use.
Opioid analyses excluded patients with opioid prescription fills in the 90 days prior to the fracture and were adjusted for previous and current NSAID and COX-2 use.
Sensitivity and Subgroup Analyses
Rates of nonunion declined somewhat over time, with a 1.0% frequency of a nonunion diagnosis plus procedure in 2001 to 2005, 0.9% in 2006 to 2010, and 0.7% in 2011 to 2015. These year categories had no significant impact on the association between NSAID/COX-2 or opioid prescription fills and nonunion (p for interaction = 0.18 and 0.20, respectively; stratified analyses in Appendix Table E-5). Associations between NSAID/COX-2 prescription fills and nonunion did not differ by the anatomical location of the fracture (p for interaction = 0.89), whereas the association between opioid prescription fills and nonunion differed by fracture location (p for interaction = 0.01), with weaker associations between opioids and nonunion for distal femoral, humeral, and radial fractures. The results for tibial fractures, distal femoral fractures, and femoral neck fractures are shown in Appendix Table E-6. Patients filling multiple prescriptions for NSAIDs, COX-2 inhibitors, or opioids in the 60 days after fracture all had higher rates of nonunion (see Appendix Table E-7).
NSAID, COX-2, and Opioid Prescriptions Prior to Fracture and the Risk of Nonunion
In adjusted models, filling a prescription for a nonselective NSAID or COX-2 inhibitor in the 90 days before the fracture was associated with an increased risk of a nonunion diagnosis plus procedure (aOR = 1.44 [95% CI = 1.27 to 1.62] for NSAIDs and aOR = 1.60 [95% CI = 1.29 to 1.98] for COX-2 inhibitors) or a nonunion diagnosis (aOR = 1.36 [95% CI = 1.24 to 1.49] for NSAIDs and aOR = 1.76 [95% CI = 1.51 to 2.19] for COX-2 inhibitors). Filling an opioid prescription in the 90 days before the fracture was not associated with an increased risk of a nonunion diagnosis plus procedure (aOR = 1.04 [95% CI = 0.95 to 1.15]) and was only modestly associated with a nonunion diagnosis (aOR = 1.09 [95% CI = 1.02 to 1.17]).
Discussion
In this large health-care claims database, we found that filling a prescription for a nonselective NSAID after fracture was not associated with an increased risk of nonunion in the subsequent year. Both COX-2-inhibitor and opioid prescription fills after fracture were associated with a greater risk of nonunion.
Animal studies, including those using COX-2 knockout mice and those using COX-2 inhibitors in mice, rats, and rabbits, have shown that COX-2 production of prostaglandins is a key pathway in fracture-healing, particularly immediately after the occurrence of a fracture6-12. In humans, reduced COX-2 expression has also been noted in the callus of fractures with nonunion compared with those with normal healing25. The effect of COX-2 inhibition in animal studies, however, appears to depend on the dose, timing, and duration of COX-2 inhibition9,10. Nonselective NSAIDs, which block both COX-1 and COX-2, could hypothetically also impair fracture-healing. Animal study data on nonselective NSAIDs are mixed, with some studies demonstrating impaired fracture-healing and others showing some delay in fracture-healing without differences in rates of nonunion6,9-11,13,26.
Whether nonselective NSAIDs or COX-2 inhibitors are associated with nonunion at the doses used clinically has been uncertain. Small cohort studies have shown conflicting results15,16,18-20,27. Zura et al. examined a large administrative database and found that use of an NSAID with an opioid was associated with an increased risk of nonunion compared with an opioid alone, but NSAID use was not associated with nonunion when compared with no analgesic use; however, nonselective NSAIDs were not examined separately from COX-2 inhibitors1. An ecological study by Wang and Bhattacharyya showed that rates of nonunion increased from 2000 to 2004, when COX-2-inhibitor use was more frequent, and declined with the abrupt drop in use of COX-2 inhibitors from 2004 to 2005, possibly implicating COX-2 inhibitors as particularly important for nonunion risk; however, the study could not directly evaluate associations between COX-2 inhibitors and nonunion4. A prospective study of patients with tibial fracture demonstrated no association between NSAID use and a composite outcome that included nonunion28.
In this context, our results provide credible evidence supporting the safety of nonselective NSAID use at commonly utilized doses after fracture. It should be noted that nonselective NSAIDs may have temporary effects on bone-healing that are quickly reversible and that effects may be dose and duration-dependent9. While the NSAID doses that patients received in this study were not associated with fracture, we cannot rule out the possibility that prolonged use of high-dose NSAIDs could impact fracture-healing. We did find that patients filling multiple prescriptions for nonselective NSAIDs, COX-2 inhibitors, or opioids in the 60 days after fracture had significantly higher rates of nonunion. These analyses may be explained by reverse causation—patients with more severe injuries, poor healing, and persistent pain after fracture would be more likely to continue analgesic medications after the first month—but we cannot rule out the possibility that higher doses or durations of NSAIDs could confer nonunion risk. Interestingly, we found that patients who filled a prescription for a nonselective NSAID or COX-2 inhibitor prior to their fracture were at greater risk for nonunion, findings similar to those noted by others14,17. One possible explanation is that patients already receiving chronic NSAIDs or COX-2 inhibitors before a fracture are exposed to longer durations or higher doses after the fracture and that this greater exposure has an impact on fracture-healing. At the doses and durations of nonselective NSAIDs most commonly used in clinical practice, however, we did not find a significant association between a nonselective-NSAID prescription fill after fracture and nonunion.
Filling a prescription for a selective COX-2 inhibitor after fracture was associated with a greater risk of nonunion. While residual confounding might explain this relationship, the fact that this association is different from that seen with nonselective NSAIDs and that this result is in accordance with both animal studies and previous clinical reports4 reinforces concerns about COX-2-inhibitor use after fracture. While certain potent COX-2 inhibitors are no longer available, we found similar associations between COX-2 prescription fills and nonunion even from 2011 to 2015. These data also highlight the importance of distinguishing COX-2 inhibitors from nonselective NSAIDs in studies of nonunion.
Opioids were associated with an increased risk of nonunion, as has been described in other clinical studies1,14. There is less evidence to support a mechanism between opioids and nonunion29, and the potential for confounding is substantial. Indeed, patients who filled an opioid prescription had higher-energy injuries and were more likely to be treated in the inpatient setting or emergency department than patients who did not fill an opioid prescription. Adjustment for measurable factors, which did substantially attenuate the association between opioids and nonunion, is unlikely to have completely accounted for the confounding by indication. Prior opioid use, which would not be expected to be confounded to the same degree by injury severity, was not associated the primary nonunion outcome.
Several limitations are important to note. Outcomes were based on administrative claims, although our primary outcome required not only a diagnosis code for nonunion (which has been shown to have a high positive predictive value for nonunion21) but also a procedure to treat the nonunion, to capture the most clinically relevant events. Exposure to NSAIDs, COX-2 inhibitors, or opioids was ascertained on the basis of dispensed prescriptions, but it is not possible to determine whether patients actually took these medications and for how long. This limitation and the possible use of over-the-counter NSAIDs or illicit opioids by ostensibly unexposed patients could bias results toward the null. Our study also lacked adequate statistical power to allow us to individually examine specific medications or assess interactions between opioids and NSAIDs, and we were limited in our ability to separately evaluate different fracture sites. We excluded patients with multiple fractures unless they were commonly paired, and the majority of the included patients were treated as outpatients without a surgical procedure to treat their fracture; thus, our results may not apply to patients at higher risk for nonunion. Also, we studied an insured population. Musculoskeletal trauma and risk factors associated with nonunion may be more common in uninsured or underinsured patients. Residual confounding is likely—fracture severity cannot fully be captured by the measures that we used (e.g., fracture treatment, treatment location, and energy of injury), and some nonunion risk factors such as tobacco use could not be accurately measured. Thus, finding no association between nonspecific NSAIDs and nonunion is reassuring, but the associations seen with COX-2 inhibitors and especially opioids could be due to confounding. Finally, because this study ended in 2015, we could not assess recent changes in prescribing patterns in response to the opioid epidemic.
In conclusion, filling a single nonselective NSAID prescription after fracture was not associated with a greater risk of nonunion. In contrast, filling prescriptions for COX-2 inhibitors was associated with a greater nonunion risk, a finding that is compatible with data from animal studies and other epidemiologic studies. Opioids were also associated with greater risk of nonunion, although patients filling prescriptions for opioids may have more severe, high-risk fractures, which could have contributed to this observed association.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F904).
Footnotes
Investigation performed at the University of Pennsylvania, Philadelphia, Pennsylvania
A commentary by Willem-Jan Metsemakers, MD, PhD, is linked to the online version of this article at jbjs.org.
Disclosure: This work was supported by grants from the National Institutes of Health (NIH) (K23 AR073931-01 and R01 AG064589). On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/F903).
References
- 1.Zura R, Xiong Z, Einhorn T, Watson JT, Ostrum RF, Prayson MJ, Della Rocca GJ, Mehta S, McKinley T, Wang Z, Steen RG. Epidemiology of fracture nonunion in 18 human bones. JAMA Surg. 2016. November 16;151(11):e162775 Epub 2016 Nov 16. [DOI] [PubMed] [Google Scholar]
- 2.Zura R, Braid-Forbes MJ, Jeray K, Mehta S, Einhorn TA, Watson JT, Della Rocca GJ, Forbes K, Steen RG. Bone fracture nonunion rate decreases with increasing age: a prospective inception cohort study. Bone. 2017. February;95:26-32. Epub 2016 Nov 9. [DOI] [PubMed] [Google Scholar]
- 3.Richards CJ, Graf KW, Jr, Mashru RP. The effect of opioids, alcohol, and nonsteroidal anti-inflammatory drugs on fracture union. Orthop Clin North Am. 2017. October;48(4):433-43. Epub 2017 Jul 29. [DOI] [PubMed] [Google Scholar]
- 4.Wang Z, Bhattacharyya T. Trends of non-union and prescriptions for non-steroidal anti-inflammatory drugs in the United States, 1993-2012. Acta Orthop. 2015;86(5):632-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tzioupis C, Giannoudis PV. Prevalence of long-bone non-unions. Injury. 2007. May;38(Suppl 2):S3-9. [DOI] [PubMed] [Google Scholar]
- 6.Simon AM, Manigrasso MB, O’Connor JP. Cyclo-oxygenase 2 function is essential for bone fracture healing. J Bone Miner Res. 2002. June;17(6):963-76. [DOI] [PubMed] [Google Scholar]
- 7.Zhang X, Schwarz EM, Young DA, Puzas JE, Rosier RN, O’Keefe RJ. Cyclooxygenase-2 regulates mesenchymal cell differentiation into the osteoblast lineage and is critically involved in bone repair. J Clin Invest. 2002. June;109(11):1405-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lu LY, Loi F, Nathan K, Lin TH, Pajarinen J, Gibon E, Nabeshima A, Cordova L, Jämsen E, Yao Z, Goodman SB. Pro-inflammatory M1 macrophages promote osteogenesis by mesenchymal stem cells via the COX-2-prostaglandin E2 pathway. J Orthop Res. 2017. November;35(11):2378-85. Epub 2017 Mar 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gerstenfeld LC, Al-Ghawas M, Alkhiary YM, Cullinane DM, Krall EA, Fitch JL, Webb EG, Thiede MA, Einhorn TA. Selective and nonselective cyclooxygenase-2 inhibitors and experimental fracture-healing. Reversibility of effects after short-term treatment. J Bone Joint Surg Am. 2007. January;89(1):114-25. [DOI] [PubMed] [Google Scholar]
- 10.Simon AM, O’Connor JP. Dose and time-dependent effects of cyclooxygenase-2 inhibition on fracture-healing. J Bone Joint Surg Am. 2007. March;89(3):500-11. [DOI] [PubMed] [Google Scholar]
- 11.O’Connor JP, Capo JT, Tan V, Cottrell JA, Manigrasso MB, Bontempo N, Parsons JR. A comparison of the effects of ibuprofen and rofecoxib on rabbit fibula osteotomy healing. Acta Orthop. 2009. October;80(5):597-605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bergenstock M, Min W, Simon AM, Sabatino C, O’Connor JP. A comparison between the effects of acetaminophen and celecoxib on bone fracture healing in rats. J Orthop Trauma. 2005. Nov-Dec;19(10):717-23. [DOI] [PubMed] [Google Scholar]
- 13.Gerstenfeld LC, Thiede M, Seibert K, Mielke C, Phippard D, Svagr B, Cullinane D, Einhorn TA. Differential inhibition of fracture healing by non-selective and cyclooxygenase-2 selective non-steroidal anti-inflammatory drugs. J Orthop Res. 2003. July;21(4):670-5. [DOI] [PubMed] [Google Scholar]
- 14.Buchheit T, Zura R, Wang Z, Mehta S, Della Rocca GJ, Steen RG. Opioid exposure is associated with nonunion risk in a traumatically injured population: an inception cohort study. Injury. 2018. July;49(7):1266-71. Epub 2018 May 21. [DOI] [PubMed] [Google Scholar]
- 15.Burd TA, Hughes MS, Anglen JO. Heterotopic ossification prophylaxis with indomethacin increases the risk of long-bone nonunion. J Bone Joint Surg Br. 2003. July;85(5):700-5. [PubMed] [Google Scholar]
- 16.Sagi HC, Jordan CJ, Barei DP, Serrano-Riera R, Steverson B. Indomethacin prophylaxis for heterotopic ossification after acetabular fracture surgery increases the risk for nonunion of the posterior wall. J Orthop Trauma. 2014. July;28(7):377-83. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez RK, Do TP, Critchlow CW, Dent RE, Jick SS. Patient-related risk factors for fracture-healing complications in the United Kingdom General Practice Research Database. Acta Orthop. 2012. December;83(6):653-60. Epub 2012 Nov 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McDonald E, Winters B, Nicholson K, Shakked R, Raikin S, Pedowitz DI, Daniel JN. Effect of postoperative ketorolac administration on bone healing in ankle fracture surgery. Foot Ankle Int. 2018. October;39(10):1135-40. Epub 2018 Jul 4. [DOI] [PubMed] [Google Scholar]
- 19.DePeter KC, Blumberg SM, Dienstag Becker S, Meltzer JA. Does the use of ibuprofen in children with extremity fractures increase their risk for bone healing complications? J Emerg Med. 2017. April;52(4):426-32. Epub 2016 Oct 14. [DOI] [PubMed] [Google Scholar]
- 20.Giannoudis PV, MacDonald DA, Matthews SJ, Smith RM, Furlong AJ, De Boer P. Nonunion of the femoral diaphysis. The influence of reaming and non-steroidal anti-inflammatory drugs. J Bone Joint Surg Br. 2000. July;82(5):655-8. [DOI] [PubMed] [Google Scholar]
- 21.Boudreau DM, Yu O, Spangler L, Do TP, Fujii M, Ott SM, Critchlow CW, Scholes D. Accuracy of ICD-9 codes to identify nonunion and malunion and developing algorithms to improve case-finding of nonunion and malunion. Bone. 2013. February;52(2):596-601. Epub 2012 Nov 19. [DOI] [PubMed] [Google Scholar]
- 22.Ziadé N, Jougla E, Coste J. Using vital statistics to estimate the population-level impact of osteoporotic fractures on mortality based on death certificates, with an application to France (2000-2004). BMC Public Health. 2009. September 17;9:344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009. November 10;28(25):3083-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cameron AC, Miller DL. A practitioner’s guide to cluster-robust inference. J Hum Resour. 2015;50(2):317-72. [Google Scholar]
- 25.Daluiski A, Ramsey KE, Shi Y, Bostrom MP, Nestor BJ, Martin G, Hotchkiss R, Stephan DA. Cyclooxygenase-2 inhibitors in human skeletal fracture healing. Orthopedics. 2006. March;29(3):259-61. [DOI] [PubMed] [Google Scholar]
- 26.Beck A, Krischak G, Sorg T, Augat P, Farker K, Merkel U, Kinzl L, Claes L. Influence of diclofenac (group of nonsteroidal anti-inflammatory drugs) on fracture healing. Arch Orthop Trauma Surg. 2003. September;123(7):327-32. Epub 2003 Jun 13. [DOI] [PubMed] [Google Scholar]
- 27.Borgeat A, Ofner C, Saporito A, Farshad M, Aguirre J. The effect of nonsteroidal anti-inflammatory drugs on bone healing in humans: a qualitative, systematic review. J Clin Anesth. 2018. September;49:92-100. Epub 2018 Jun 15. [DOI] [PubMed] [Google Scholar]
- 28.Schemitsch EH, Bhandari M, Guyatt G, Sanders DW, Swiontkowski M, Tornetta P, Walter SD, Zdero R, Goslings JC, Teague D, Jeray K, McKee MD; Study to Prospectively Evaluate Reamed Intramedullary Nails in Patients with Tibial Fractures (SPRINT) Investigators. Prognostic factors for predicting outcomes after intramedullary nailing of the tibia. J Bone Joint Surg Am. 2012. October 3;94(19):1786-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chrastil J, Sampson C, Jones KB, Higgins TF. Postoperative opioid administration inhibits bone healing in an animal model. Clin Orthop Relat Res. 2013. December;471(12):4076-81. Epub 2013 Aug 17. [DOI] [PMC free article] [PubMed] [Google Scholar]