Abstract
Background:
Open tibial fractures are common injuries in low and middle-income countries, but there is no consensus regarding treatment with intramedullary nailing versus external fixation. The purpose of the present study was to compare the outcomes of initial treatment with intramedullary nailing or external fixation in adults with open tibial fractures.
Methods:
We conducted a randomized clinical trial (RCT) at a tertiary orthopaedic center in Tanzania. Adults with acute diaphyseal open tibial fractures were randomly assigned to statically locked, hand-reamed intramedullary nailing or uniplanar external fixation. The primary outcome was death or reoperation for the treatment of deep infection, nonunion, or malalignment. Secondary outcomes included quality of life as measured with the EuroQol-5 Dimensions (EQ-5D) questionnaire, radiographic alignment, and healing as measured with the modified Radiographic Union Scale for Tibial fractures (mRUST).
Results:
Of the 240 patients who were enrolled, 221 (92.1%) (including 111 managed with intramedullary nailing and 110 managed with external fixation) completed 1-year follow-up. There were 44 primary outcome events (with rates of 18.0% and 21.9% in the intramedullary nailing and external fixation groups, respectively) (relative risk [RR] = 0.83 [95% confidence interval (CI), 0.49 to 1.41]; p = 0.505). There was no significant difference between the groups in terms of the rate of deep infection. Intramedullary nailing was associated with a lower risk of coronal malalignment (RR = 0.11 [95% CI, 0.01 to 0.85]; p = 0.01) and sagittal malalignment (RR = 0.17 [95% CI, 0.02 to 1.35]; p = 0.065) at 1 year. The EQ-5D index favored intramedullary nailing at 6 weeks (mean difference [MD] = 0.07 [95% CI = 0.03 to 0.11]; p < 0.001), but this difference dissipated by 1 year. Radiographic healing (mRUST) favored intramedullary nailing at 6 weeks (MD = 1.2 [95% CI = 0.4 to 2.0]; p = 0.005), 12 weeks (MD = 1.0 [95% CI = 0.3 to 1.7]; p = 0.005), and 1 year (MD = 0.8 [95% CI = 0.2 to 1.5]; p = 0.013).
Conclusions:
To our knowledge, the present study is the first RCT assessing intramedullary nailing versus external fixation for the treatment of open tibial fractures in sub-Saharan Africa. Differences in primary events were not detected, and only coronal alignment significantly favored the use of intramedullary nailing.
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
The tibial shaft is the most common site of long-bone fractures and is also the most common site of open fractures1. Although epidemiological data from low and middle-income countries are lacking, it is reasonable to assume that the incidence of tibial fractures is rising due to a well-documented increase in road-traffic injuries2. Despite advances in treatment, including routine prophylactic antibiotics, prompt debridement, and early soft-tissue coverage, these injuries are associated with high rates of infection and nonunion3. Moreover, the operative treatment of open fractures is recognized as a bellwether procedure for monitoring and planning of essential surgical care in low and middle-income countries4.
Despite the importance of appropriate open tibial fracture treatment, the optimum method of definitive skeletal stabilization remains unclear. External fixation provides fracture stabilization with minimal soft-tissue disturbance. In austere environments, a greater risk of infection5,6 and concerns regarding sterility7 lead many surgeons to minimize the use of internal implants in order to limit the risk of wound infection. Moreover, the implants for external fixation can readily be reused, making them more available and affordable in low and middle-income countries8. On the other hand, internal fixation of the tibial shaft can be achieved with intramedullary nails or plates, and intramedullary nails are considered the standard of care in high-income countries because of their superior mechanical properties and the limited soft-tissue dissection required for their use9. While the existing literature supports intramedullary nailing compared with external fixation for the treatment of open tibial fractures, the association is weak and we do not know whether these findings apply to similarly injured patients in low and middle-income countries using locally available facilities and implants10,11.
We conducted a randomized clinical trial to determine the rate of reoperation for the treatment of deep infection, nonunion, or malalignment following uniplanar external fixation as compared with statically locked intramedullary nailing for the treatment of open tibial shaft fractures not requiring a flap for closure. The secondary objectives were to compare secondary complication rates (malalignment, superficial infection), radiographic healing, and health-related quality of life.
Materials and Methods
We conducted a prospective randomized clinical trial at a tertiary referral hospital in Dar es Salaam, Tanzania from December 17, 2015, to March 25, 2017. The trial objectives, study design, and protocol were described in a previous report12. All patients with open tibial fractures who arrived at the hospital emergency department were screened for enrollment. Inclusion criteria were an age of ≥18 years, an AO/Orthopaedic Trauma Association (OTA) type-42 open tibial shaft fracture13, and presentation within 24 hours after the injury. Patients were included if the traumatic wounds could be closed, could be treated with skin-grafting, or could be expected to heal secondarily (Gustilo-Anderson type I to IIIA)14. Patients were excluded if they had an injury requiring a flap to cover exposed bone following debridement (Gustilo-Anderson IIIB), vascular injury requiring repair (Gustilo-Anderson IIIC), ipsilateral femoral fracture, contralateral femoral or tibial fracture, pathological fracture, preexisting lower-limb deformity, severe traumatic brain injury (TBI, Glasgow Coma Scale <12), spinal cord injury, severe burns (involving >10% of the total body surface area or >5% of the total body surface area with full-thickness or circumferential injury), previous ipsilateral leg injury requiring surgery, or inability to comply with follow-up (Fig. 1). We excluded type-IIIB fractures because of the relative lack of soft-tissue transfer and microvascular capability at our institution. All patients who were eligible after preoperative clinical screening completed written informed consent in either English or Swahili. The study was approved by ethical review boards at the participating institutions and registered with ClinicalTrials.gov (NCT03861624).
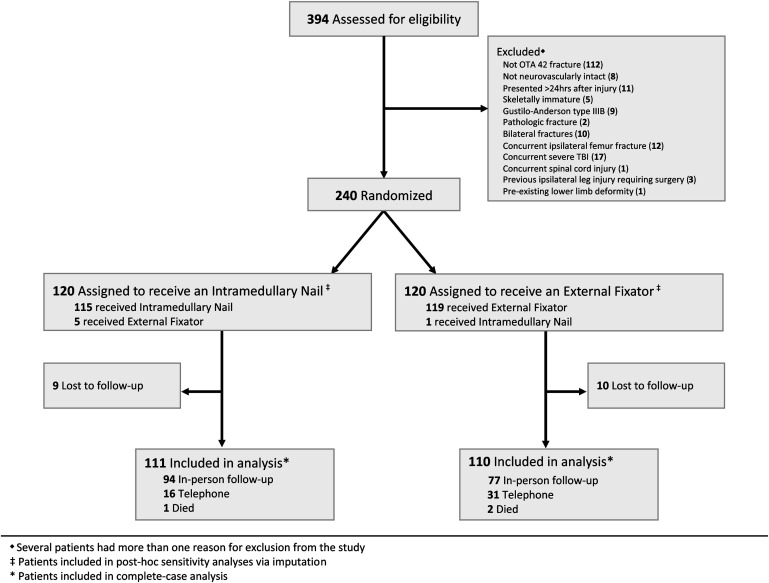
Fig. 1.
CONSORT (Consolidated Standards of Reporting Trials) diagram demonstrating participant flow through the trial. Some patients had >1 reason for exclusion.
An attempt was made to treat all participants with initial irrigation and debridement within 24 hours after admission, although in a few instances operating room unavailability resulted in slight additional delays. If the surgeon found the injury eligible for inclusion, the patient was randomized to intramedullary nailing or external fixation. We used a centralized web-based electronic randomization tool, REDCap (Research Electronic Data Capture)15, with blocks randomly permuted in sizes of 4, 6, or 8.
All subjects were managed with intravenous ceftriaxone at the time of presentation to the emergency department (1 g/day for 2 days). Open reduction was performed in all cases with use of the traumatic wound or a counterincision as required; this allowed visual confirmation of the medullary placement of intramedullary nails. Restoration of functional alignment in both treatment groups was assessed clinically; intraoperative fluoroscopy was not used in any case. Patients who were randomized to intramedullary nailing were managed with a hand-reamed SIGN nail with a targeting arm for proximal and distal interlocking (SIGN Fracture Care International). Those patients were allowed toe-touch status for 6 weeks after surgery followed by weight-bearing as tolerated. Patients who were randomized to external fixation received the AO uniplanar Dispofix external fixator (Dispofix Indústria e Comércio), with 2 Schanz pins (5 or 6 mm) (DePuy Synthes) in the proximal segment and 2 Schanz pins in the distal segment connected to a single stainless-steel bar with AO pin-to-bar clamps. Patients randomized to external fixation initially were kept non-weight-bearing and were converted to a weight-bearing patellar tendon-bearing cast by a consultant or resident surgeon after a minimum of 6 weeks and maximum of 3 months on the basis of the radiographic appearance of fracture callus. Thirty faculty specialists and 25 supervised resident surgeons participated in the study after having confirmed prior training and experience both in the use of the SIGN nail and in the application of an AO uniplanar external fixator. Treatment with intramedullary nailing or external fixation was rendered with any of these qualified individuals serving as primary surgeon.
All data collection was performed by research coordinators with use of REDCap software15. Prior to randomization, we collected baseline demographic and socioeconomic data and baseline health-related quality of life with use of the EuroQol-5 Dimension, 3-Level questionnaire (EQ-5D-3L)16. After discharge, patients were followed at 2 weeks, 6 weeks, 3 months, 6 months, and 1 year. Orthogonal radiographs were made postoperatively, at 6 weeks, and at each subsequent visit.
The primary events of death or reoperation for the treatment of deep infection, nonunion, or malalignment were adjudicated by 2 fellowship-trained orthopaedic trauma surgeons (D.W.S., S.M.) who were not involved in the clinical care of study subjects; decisions were reached by consensus. All radiographs were evaluated in duplicate for coronal and sagittal alignment with use of goniometry and for healing with use of the modified Radiographic Union Scale for Tibial fractures (mRUST). Deep infection was defined as (1) exposed bone at any time point, (2) any wound drainage occurring after the 3-month appointment, or (3) an infection requiring surgical debridement. A nonunion was defined as (1) a reoperation to promote bone-healing or (2) an mRUST score of ≤10 at or after the 6-month follow-up visit when surgery was recommended for the treatment of nonunion17. Malalignment was not considered a primary event unless a reoperation was performed for deformity correction.
Superficial infections, delayed wound-healing, and malalignment were considered secondary events. Pin-site infections were not considered surgical site infections. A deformity threshold of >10° in the coronal or sagittal plane at 1 year, regardless of whether the patient underwent reoperation, was considered malalignment18,19. The EQ-5D-3L index and the EQ-VAS (visual analog scale) were secondary outcome measures collected at each follow-up visit. Adverse events were monitored by investigators every 6 months.
Statistical Analysis
Data from a pilot study informed sample-size calculations20. In that study, the rate of unplanned reoperation was 20% following external fixation and 3.8% following intramedullary nailing, leading us to power our study to detect a 15% risk difference in the primary event (20% with external fixation versus 5% with intramedullary nailing). We are not aware of any comparable studies in the literature to guide these estimates given the implants used and austere study environment; nevertheless, this effect size was supported by low complication rates reported in association with SIGN nail use21, higher complication rates in association with external fixation for the treatment of open tibial fractures, and risk differences of 12% to 17% favoring intramedullary nailing in 2 large meta-analyses available at the time of study inception10,22. Using a power of 80% and 2-sided alpha of 0.05, we estimated that the study would require 88 patients in each treatment group (176 total) to evaluate the primary outcome at 1 year. Accounting for a 20% potential loss to follow-up, we estimated a sample size requirement of 240 patients (120 per group).
For each analysis of composite primary or secondary outcomes, events were counted only once per subject. Treatment effects on binary outcomes at 1 year were reported as relative risks (RRs) with 95% confidence intervals (CIs) with use of the Fisher exact test for significance. Continuous secondary outcomes, namely the EQ-5D-3L index, EQ-VAS, and mRUST, were assessed for between-group differences with use of the Student t test at 1 year and longitudinal linear mixed-effects regression models. A priori subgroups were identified to evaluate potential effect modification by sex, surgeon experience, delay to surgery, OTA fracture classification, and Gustilo-Anderson open fracture type with use of the Cochran-Mantel-Haenszel chi-square test. All tests were 2-tailed with a 0.05 significance level. Analyses of primary and secondary outcomes were performed with complete-case data with use of intention-to-treat principles whereby each subject was analyzed with the treatment group to which they had been were randomized. Post-hoc sensitivity analyses of the primary and secondary outcomes were conducted to assess sensitivity to missingness of data with use of multiple imputation with chained equations (MICE), and models were fit to give a pooled estimate of the treatment effect23. All analyses were conducted with use of STATA SE version 15 (StataCorp).
Results
We assessed 394 patients for eligibility and randomly assigned 240 patients to receive intramedullary nailing (n = 120) or external fixation (n = 120) (Fig. 1). Of those enrolled, 221 patients (92.1%) (including 111 managed with intramedullary nailing and 110 managed with external fixation) died or completed 1 year of follow-up. The typical patient was male, 33 years of age, and injured in a road traffic collision causing a low to moderate-severity diaphyseal open tibial fracture (Table I). The level of experience of the primary surgeon was similar between treatment groups. Crossover was minimal between groups (Fig. 1), and there were no conversions of temporizing external fixation to intramedullary nailing. Single-stage debridement and primary closure was performed in all cases. An as-treated sensitivity analysis yielded similar results for primary and secondary outcomes.
TABLE I.
Characteristics of Study Participants*
| Characteristic | Total (N = 221) | Intramedullary Nailing (N = 111) | External Fixation (N = 110) |
| Age (yr) | 32.9 ± 10.6 | 33.3 ± 11.8 | 31.8 ± 9.5 |
| Male sex (no. of patients) | 189 (85.5%) | 98 (88.3%) | 91 (82.7%) |
| No formal employment (no. of patients) | 173 (78.3%) | 91 (82.0%) | 82 (74.5%) |
| Mechanism of injury (no. of patients) | |||
| Road traffic injury | 208 (94.1%) | 104 (93.7%) | 104 (94.5%) |
| Car | 32 (14.5%) | 13 (11.7%) | 19 (17.3%) |
| Motorbike | 87 (39.4%) | 48 (43.2%) | 39 (35.5%) |
| Pedestrian | 89 (40.3%) | 43 (38.7%) | 46 (41.8%) |
| Other | 12 (5.4%) | 7 (6.3%) | 5 (4.5%) |
| Current smoker (no. of patients) | 42 (19.0%) | 16 (14.4%) | 26 (23.6%) |
| Alcohol use (no. of patients) | 81 (36.7%) | 45 (40.5%) | 36 (32.7%) |
| Body mass index (kg/m2) | 25.0 ± 4.9 | 25.2 ± 5.2 | 24.7 ± 4.5 |
| Diabetes mellitus (no. of patients) | 9 (4.1%) | 8 (7.2%) | 1 (0.9%) |
| No medical insurance (no. of patients) | 179 (81.0%) | 88 (79.3%) | 91 (82.7%) |
| Interval from injury to hospital (hr) | 7.9 ± 5.0 | 7.6 ± 4.7 | 8.3 ± 5.3 |
| Delayed presentation to hospital (no. of patients) | |||
| <6 hr delay | 79 (35.7%) | 46 (41.4%) | 33 (30.0%) |
| 6 to 24 hr delay | 139 (62.9%) | 64 (57.7%) | 75 (68.2%) |
| >24 hr delay† | 1 (0.05%) | 0 (0%) | 1 (0.9%) |
| Interval from injury to first antibiotic delivery (hr) | 11.5 ± 6.6 | 11.1 ± 6.6 | 11.8 ± 6.5 |
| Antibiotic delivered (no. of patients) | |||
| Ceftriaxone only | 217 (98.2%) | 109 (98.2%) | 108 (98.2%) |
| Ceftriaxone, gentamycin, and metronidazole | 3 (1.4%) | 2 (1.8%) | 1 (0.9%) |
| Interval from hospital arrival to surgery (hr) | 6.0 ± 5.5 | 6.0 ± 5.5 | 6.0 ± 5.5 |
| Delay from hospital arrival to surgery (no. of patients) | |||
| <6 hr | 127 (57.5%) | 62 (55.9%) | 65 (59.1%) |
| 6 to 24 hr | 83 (37.6%) | 44 (39.6%) | 39 (35.5%) |
| >24 hr | 11 (5.0%) | 5 (4.5%) | 6 (5.5%) |
| OTA classification (no. of patients) | |||
| Type A | 73 (48.0%) of 152 | 36 (45.6%) of 79 | 37 (50.7%) of 73 |
| Type B | 62 (40.8%) of 152 | 34 (43.0%) of 79 | 28 (38.4%) of 73 |
| Type C | 17 (11.2%) of 152 | 9 (11.4%) of 79 | 8 (11.0%) of 73 |
| OTA wound classification (no. of patients) | |||
| Skin: edges do not approximate | 51 (23.1%) | 22 (19.8%) | 29 (26.4%) |
| Muscle: loss of muscle with retained function | 4 (1.8%) | 1 (0.9%) | 3 (2.7%) |
| Bone loss: segmental | 4 (1.8%) | 1 (0.9%) | 3 (2.7%) |
| Vascular: injury without ischemia | 4 (1.8%) | 3 (2.7%) | 1 (0.9%) |
| Contamination: surface contamination | 16 (7.2%) | 4 (3.6%) | 12 (10.9%) |
| Gustilo-Anderson classification (no. of patients) | |||
| Type I | 14 (6.3%) | 6 (5.4%) | 8 (7.3%) |
| Type II | 181 (81.9%) | 89 (80.2%) | 92 (83.6%) |
| Type III | 26 (11.8%) | 16 (14.4%) | 10 (9.1%) |
| Primary surgeon (no. of patients) | |||
| Resident/trainee | 185 (93%) of 200 | 94 (93%) of 101 | 91 (92%) of 99 |
| Faculty/specialist | 15 (8%) of 200 | 7 (7%) of 101 | 8 (8%) of 99 |
| Wound length (cm) | 3.7 ± 2.5 | 3.6 ± 2.7 | 3.7 ± 2.4 |
The values are given as the mean and the standard deviation or as the number of patients, with the percentage in parentheses. Various demographic data were not reported for all patients.
One patient presented at 24.3 hours and was included in the study.
The rate of primary outcome events did not significantly differ by treatment (18.0% for intramedullary nailing compared with 21.9% for external fixation; RR = 0.83 [95% CI, 0.49 to 1.41]). There were no significant differences in terms of the rate of death or the rates of reoperation for the treatment of deep infection, nonunion, or malalignment when analyzed separately (Table II). The secondary events of superficial surgical site infections and delayed wound-healing were reported throughout the study, and there were no differences in the rates of these events by treatment. Immediate postoperative malalignment was noted in 3 patients in the external fixation group, compared with 1 patient in the intramedullary nailing group (p = 0.34). However, the risk of malalignment was lower in association with intramedullary nailing than external fixation at 1 year (coronal, RR = 0.11 [95% CI, 0.01 to 0.85]; sagittal, RR = 0.17 [95% CI, 0.02 to 1.35]) (Table II).
TABLE II.
Study Outcomes by Treatment Type
| Outcome | Total* (N = 221) | Intramedullary Nailing* (N = 111) | External Fixator* (N = 110) | Relative Risk (95% CI) | P Value |
| Primary outcome | 44 (19.9%) | 20 (18.0%) | 24 (21.8%) | 0.83 (0.49 to 1.41) | 0.505 |
| Reoperation for deep infection | 28 (12.7%) | 15 (13.5%) | 13 (11.8%) | 1.14 (0.57 to 2.29) | 0.840 |
| Reoperation for nonunion | 11 (5.0%) | 3 (2.7%) | 8 (7.3%) | 0.37 (0.10 to 1.36) | 0.135 |
| Reoperation for malalignment | 2 (0.9%) | 1 (0.9%) | 1 (0.9%) | 0.99 (0.06 to 15.65) | 1.000 |
| Death | 3 (1.4%) | 1 (0.9%) | 2 (1.8%) | 0.50 (0.05 to 5.39) | 0.622 |
| Secondary events | 28 (12.7%) | 13 (11.7%) | 15 (13.6%) | 0.86 (0.43 to 1.72) | 0.691 |
| Superficial SSI† | 18 (8.1%) | 8 (7.2%) | 10 (9.1%) | 0.79 (0.33 to 1.93) | 0.632 |
| Delayed wound-healing | 10 (4.5%) | 5 (4.5%) | 5 (4.5%) | 0.99 (0.30 to 3.33) | 1.000 |
| Coronal malalignment >10° | 10 (4.5%)‡ | 1 (0.9%) | 9 (8.2%) | 0.11 (0.01 to 0.85) | 0.010 |
| Sagittal malalignment >10° | 7 (3.2%)‡ | 1 (0.9%) | 6 (5.5%) | 0.17 (0.02 to 1.35) | 0.065 |
| Secondary outcomes§ | |||||
| EQ-5D-3L index# | 0.91 ± 0.1 | 0.90 ± 0.1 | 0.91 ± 0.1 | — | 0.634 |
| EQ-VAS** | 90.9 ± 9.4 | 91.2 ± 9.6 | 90.7 ± 9.3 | — | 0.711 |
| mRUST†† | 12.5 ± 3.3 | 13.0 ± 3.0 | 12.1 ± 3.5 | — | 0.058 |
The data are given as the mean and the standard deviation or as the number of patients, with the percentage in parentheses.
Pin-site infections were not included as superficial surgical site infections (SSIs).
Thirteen individuals had malalignment at 1 year, of whom 4 had biplanar deformity.
Secondary outcomes were compared between treatment groups at 1 year with use of the Student t test.
The EQ-5D-3L index measures health-related quality of life.
VAS = visual analog scale.
mRUST = modified Radiographic Union Scale for Tibial fractures.
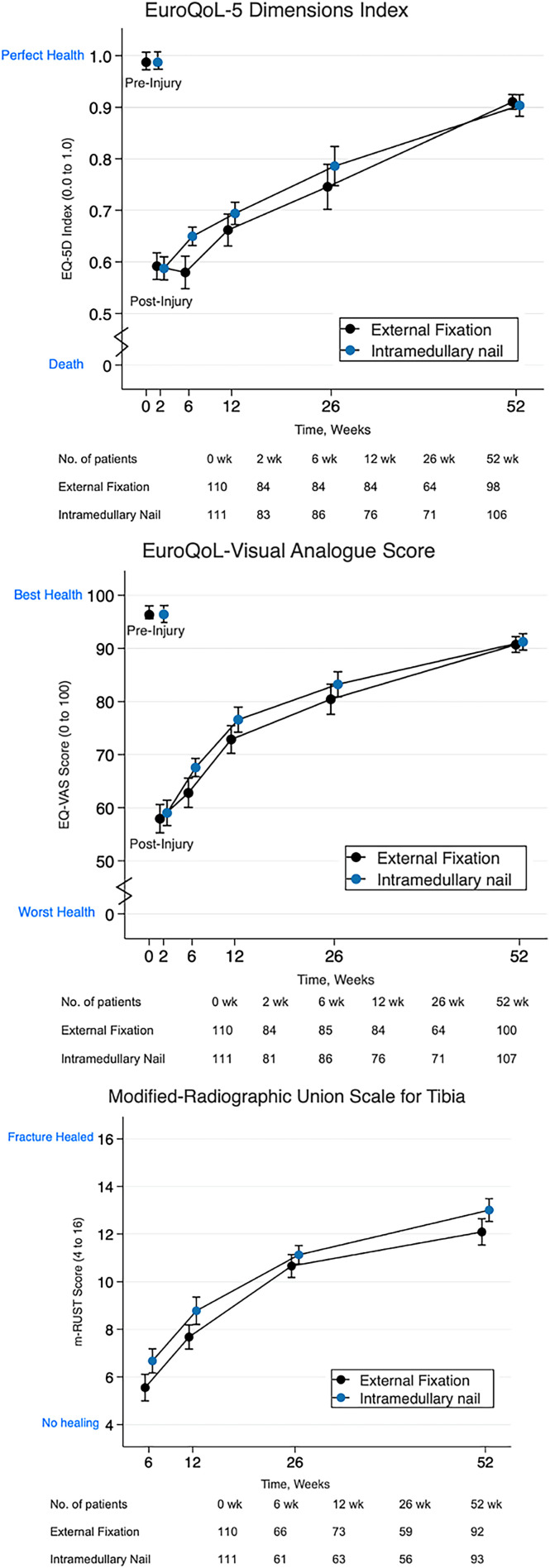
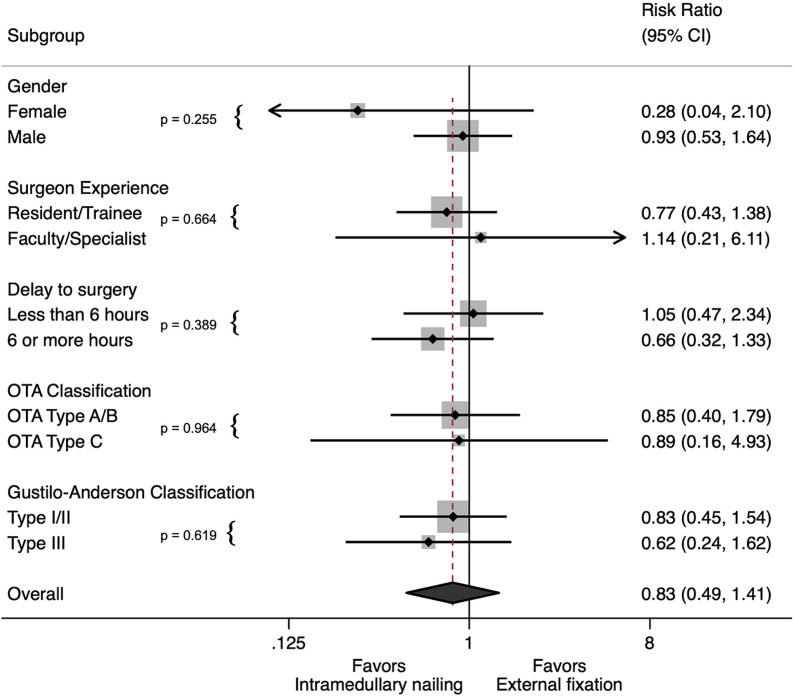
There was a significant difference in terms of the EQ-5D-3L index at 6 weeks in favor of intramedullary nailing (Fig. 2, Table III). Differences in the EQ-5D-3L index trended toward significance in favor of intramedullary nailing at 12 and 26 weeks, but this difference diminished by 1 year. EQ-VAS scores were significantly lower at 6 weeks in association with intramedullary nailing while nearing significance at 12 and 26 weeks. Again, the difference in EQ-VAS diminished by 1 year. Modified RUST scores differed significantly in favor of intramedullary nailing at all but 26 weeks (Fig. 2, Table III). Sensitivity analyses using multiple imputation demonstrated similar results. Subgroup analyses did not suggest effect modification by sex, surgeon experience, surgical delay, OTA fracture type, or Gustilo-Anderson type (Fig. 3).
Fig. 2.
Figs. 2-A, 2-B, and 2-C Line graphs showing temporal trends in secondary outcomes by treatment arm. The values are shown as the mean and 95% CI at baseline and each follow-up visit. Fig. 2-A EuroQol-5 Dimensions index. Fig. 2-B EuroQoL visual analog scale score. Fig. 2-C Modified Radiographic Union Scale for Tibial fractures (mRUST).
Fig. 3.
Forest plot showing subgroup analyses of the effects of the treatment arm on the primary outcome (reoperation). Surgeon experience was categorized as high (faculty member or specialist) or low (trainee or resident). Delay in surgery was categorized as <6 or ≥6 hours from time of hospital arrival to surgery. Fracture severity was classified as more severe (OTA type 42C) or less severe (OTA type 42A or 42B). Gustilo-Anderson classification was classified as more severe (type III) or less severe (type I or II).
TABLE III.
Secondary Outcomes by Treatment Type
| Secondary Outcomes | Intramedullary Nailing | External Fixation | Difference (95% CI) | P Value for Adjusted Analysis | |||
| Mean and Standard Deviation | No. of Patients | Mean and Standard Deviation | No. of Patients | Unadjusted* | Adjusted† | ||
| EQ-5D-3L index‡ | |||||||
| At 2 wk | 0.59 ± 0.11 | 83 | 0.59 ± 0.09 | 84 | −0.01 (−0.01 to 0.00) | 0.00 (−0.04 to 0.03) | 0.829 |
| At 6 wk | 0.65 ± 0.11 | 86 | 0.58 ± 0.17 | 84 | 0.07 (0.05 to 0.08) | 0.07 (0.03 to 0.11) | <0.001 |
| At 12 wk | 0.69 ± 0.15 | 76 | 0.66 ± 0.16 | 84 | 0.03 (0.03 to 0.03) | 0.03 (−0.01 to 0.07) | 0.118 |
| At 26 wk | 0.78 ± 0.18 | 71 | 0.74 ± 0.22 | 64 | 0.04 (0.03 to 0.05) | 0.04 (−0.02 to 0.10) | 0.195 |
| At 52 wk | 0.90 ± 0.12 | 106 | 0.91 ± 0.12 | 98 | −0.01 (−0.01 to −0.01) | −0.01 (−0.02 to 0.02) | 0.542 |
| EQ-VAS§ | |||||||
| At 2 wk | 58.8 ± 13.0 | 81 | 57.9 ± 11.5 | 84 | 0.9 (0.5 to 1.3) | 1.0 (−2.3 to 4.3) | 0.561 |
| At 6 wk | 67.7 ± 13.9 | 86 | 62.7 ± 13.3 | 85 | 5.0 (4.9 to 5.1) | 4.7 (1.7 to 7.8) | 0.002 |
| At 12 wk | 76.7 ± 14.9 | 76 | 72.6 ± 13.5 | 84 | 4.1 (3.4 to 4.5) | 3.4 (−0.4 to 7.2) | 0.076 |
| At 26 wk | 83.1 ± 13.0 | 71 | 80.2 ± 12.4 | 64 | 2.9 (2.8 to 2.9) | 2.5 (−0.4 to 5.5) | 0.096 |
| At 52 wk | 91.2 ± 9.6 | 107 | 90.7 ± 9.3 | 100 | 0.5 (0.5 to 0.5) | 0.5 (−1.9 to 2.8) | 0.695 |
| mRUST# | |||||||
| At 6 wk | 6.8 ± 2.0 | 61 | 5.6 ± 1.8 | 66 | 1.3 (1.2 to 1.3) | 1.2 (0.4 to 2.0) | 0.005 |
| At 12 wk | 8.9 ± 2.6 | 63 | 7.7 ± 2.2 | 73 | 1.2 (1.0 to 1.3) | 1.0 (0.3 to 1.7) | 0.005 |
| At 26 wk | 11.3 ± 2.3 | 56 | 10.8 ± 2.1 | 59 | 0.4 (0.4 to 0.5) | 0.4 (−0.2 to 1.1) | 0.207 |
| At 52 wk | 13.0 ± 3.0 | 93 | 12.1 ± 3.5 | 92 | 0.9 (0.8 to 1.0) | 0.8 (0.2 to 1.5) | 0.013 |
The values are calculated as the mean value for the intramedullary nailing group minus the mean value for the external fixation group. A positive score indicates that treatment favors intramedullary nailing.
Linear mixed-effects regression model of complete-case data with a time-by-treatment interaction as a fixed effect and patient as the random intercept.
The EQ-5D-3L index measures health-related quality of life on the basis of a descriptive system, with 0 indicating death and 1 indicating perfect health. The minimum clinically important difference is 0.08 point.
The EQ-VAS measures health-related quality of life on a visual analog scale ranging from 0 (worst imaginable health state) to 100 (best imaginable health state).
The mRUST quantifies radiographic fracture-healing, with a possible range of 4 to 16.
Discussion
In this randomized clinical trial in which uniplanar external fixation was compared with intramedullary nailing as definitive stabilization for open tibial fractures in Tanzania, we found no difference in the composite primary event of death or reoperation for deep infection, nonunion, or malalignment at 1 year. There were significant early differences in quality of life in favor of intramedullary nailing, but these differences did not persist at 1 year. We found higher malalignment rates among subjects randomized to external fixation and improved radiographic union scores among subjects randomized to intramedullary nailing.
These results are consistent with those of similar trials demonstrating a higher incidence of malunion and a trend toward a greater risk of unplanned reoperation among patients managed with external fixation (Table IV)9,24-26. Four prior studies evaluated unreamed intramedullary nailing and uniplanar external fixation, although 17% of the pooled sample of patients in those studies had Gustilo-Anderson type-IIIB injuries, which were excluded from the present study. The largest study, by Henley et al., was a prospective trial of 174 patients with type-II, IIIA, and IIIB injuries9. More severely injured patients were managed with external fixation in that study. The authors found an increased number of total operations (including planned reoperations), a higher malunion rate, and a higher rate of superficial infection due to pin-site infections in the external fixation group. However, when only reoperations for nonunion or deep infection were considered, the differences were not significant despite the imbalance between groups due to injury severity. The next largest study, by Shayesteh Azar et al., enrolled 113 patients with type-I/II open fractures and showed no significant difference in any outcome measured25. Whereas those prior studies were underpowered and limited by methodological shortcomings, the pooled magnitude and direction of effects are consistent with our findings favoring intramedullary nailing across the primary and secondary outcomes measured.
TABLE IV.
Randomized Studies Comparing External Fixation to Unreamed Nailing for Open Tibial Fractures*
| Study Site | Study Type | Concealed Randomization | Total No. of Patients | Treatment (no. of patients) | Gustilo-Anderson (no. of patients) | Reoperation for Nonunion, Infection, or Malunion | Nonunion | Infection | Malalignment | |||||||
| EF | IMN | Types I-IIIA | Type IIIB | EF | IMN | EF | IMN | EF | IMN | EF | IMN | |||||
| Previous studies | ||||||||||||||||
| Tu et al.26 (1995) | Taiwan | PCT | No | 36 | 18 | 18 | 20 | 16 | 39% (7 of 18) | 39% (7 of 18) | 28% (5 of 18) | 17% (3 of 18) | 11% (2 of 18) | 22% (4 of 18) | 17% (3 of 18) | 0% (0 of 18) |
| Henley et al.9 (1998) | United States | PCT | No | 174 | 70 | 104 | 148 | 26 | 39% (27 of 70) | 25% (26 of 104) | 17% (12 of 70) | 13% (13 of 104) | 21% (15 of 70) | 13% (13 of 104) | 31% (22 of 70)† | 8% (8 of 104) |
| Mohseni et al.24 (2011) | Iran | RCT | NR | 50 | 25 | 25 | 28 | 22 | 40% (10 of 25) | 16% (4 of 25) | 8% (2 of 25) | 0% (0 of 25) | 32% (8 of 25) | 16% (4 of 25) | 24% (6 of 25)† | 0% (0 of 25) |
| Shayesteh Azar et al.25 (2011) | Iran | RCT | NR | 113 | 59 | 54 | 113 | 0 | 7% (4 of 59) | 6% (3 of 54) | 5% (3 of 59) | 2% (1 of 54) | 2% (1 of 59) | 4% (2 of 54) | NR | NR |
| Total | 373 | 172 | 201 | 309 | 64 | 24% (41 of 172) | 20% (40 of 201) | 13% (22 of 172) | 8% (17 of 201) | 15% (26 of 172) | 11% (23 of 201) | 27% (31 of 113) | 5% (8 of 147) | |||
| Current study | Tanzania | RCT | Yes | 240 | 120 | 120 | 240 | 0 | 22% (24 of 110) | 18% (20 of 111) | 7% (8 of 110) | 3% (3 of 111) | 12% (13 of 110) | 14% (15 of 111) | 8% (9 of 110)† | 1% (1 of 111) |
EF = external fixation, IMN = intramedullary nailing, PCT = prospective controlled trial, NR = not reported, and RCT = randomized clinical trial.
P < 0.05.
We found that intramedullary nailing was not associated with an increased infection rate compared with external fixation when used for the treatment of open fractures. The possibility of infection due to internal fixation is a common consideration among surgeons in the study setting when selecting treatment for open tibial fractures27. The preference for external fixation, particularly for Gustilo-Anderson type-III injuries, was evident in an international survey in which more than half of surgeons from Asia, Africa, and South America chose external fixation28. We demonstrated that intramedullary nailing is a feasible treatment method that promotes better early postoperative quality of life and improved 1-year alignment without increasing infectious complication rates.
The present study demonstrated that treatment with intramedullary nailing resulted in less malalignment than external fixation at 1 year. This finding is consistent with literature showing that external fixation results in difficulties with anatomical fracture restoration because of the lack of direct fracture reduction, weaker mechanical fracture stabilization, and the need for removal prior to osseous union11. Bhandari et al. reported a pooled RR of malunion in favor of unreamed nailing versus external fixation (RR = 0.42 [95% CI, 0.25 to 0.71])10. Coronal plane malunion of as little as 5° has been associated with knee and ankle arthritis at long-term follow-up29 and therefore may be considered a surrogate for long-term outcomes of importance. In the present study, patients with malalignment had an average 1-year mRUST (and standard deviation) of only 11 ± 3.2. This finding suggests not only that is healing impaired in the setting of deformity but that its prevention with intramedullary nailing could affect radiographic end points of fracture repair that are directly targeted by surgeons.
The higher early quality of life after intramedullary nailing is not surprising given the inconveniences of an external fixator. In the present study, quality of life in the treatment groups equilibrated between 6 and 12 weeks, the period during which external fixators were removed, despite differences in radiographic healing and final alignment. It is possible that the lifestyle impact of an external fixator is a more important driver of quality-of-life differences than the degree of healing or limb alignment in this population30.
The present study had several limitations. The study was underpowered to detect absolute differences in the primary event rate of <15% (a fourfold reduction), and, while the 17% RR reduction that we found may be clinically important, our study was underpowered to demonstrate this finding with statistical certainty. Also, after recognizing that many patients for whom surgery had been recommended could not undergo surgery for financial reasons, we adjusted the definition of our primary outcome in order to detect clinical failures whether or not they underwent reoperation. Finally, no economic measurements were completed to evaluate the cost-effectiveness of treatment. In the future, larger trials with longer follow-up and economic analyses will be necessary to understand patient, payer, and societal financial implications of treatment choice.
In the present study, performed in Tanzania, there was no difference in the rate of unplanned reoperation for infection, nonunion, or malalignment between intramedullary nailing and external fixation when used for the treatment of open tibial fractures not requiring tissue transfer. Intramedullary nailing significantly reduced the risk of malalignment and was associated with sustained improvements in radiographic healing. These modest differences in secondary outcomes are of unknown clinical importance; therefore, these findings do not necessarily indicate that intramedullary nailing of open tibial fractures is superior to external fixation in the low and middle-income country setting.
Footnotes
Investigation performed at the Muhimbili Orthopaedic Institute, Muhimbili National Hospital, Dar es Salaam, Tanzania, and the University of California San Francisco, San Francisco, California
Disclosure: This study was funded by the Wyss Medical Foundation, the Doris Duke Charitable Foundation, and the National Center for Advancing Translational Science (NCATS) of the National Institutes of Health (grant number UL1TR001872), none of which had a role in design, analysis, interpretation, or dissemination of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (including a relationship with SIGN Fracture Care International, the nonprofit company that designed and manufactured the implant used in this clinical trial) (http://links.lww.com/JBJS/F712).
Data Sharing
A data-sharing statement is provided with the online version of the article (http://links.lww.com/JBJS/F713).
References
- 1.Larsen P, Elsoe R, Hansen SH, Graven-Nielsen T, Laessoe U, Rasmussen S. Incidence and epidemiology of tibial shaft fractures. Injury. 2015. April;46(4):746-50. Epub 2015 Jan 16. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Global status report on road safety 2018. 2018. Accessed 2019 Dec 30 https://www.who.int/violence_injury_prevention/road_safety_status/2018/en/ [Google Scholar]
- 3.Bhandari M, Guyatt G, Tornetta P, 3rd, Schemitsch EH, Swiontkowski M, Sanders D, Walter SD; Study to prospectively evaluate reamed intramedullary nails in patients with tibial fractures investigators. Randomized trial of reamed and unreamed intramedullary nailing of tibial shaft fractures. J Bone Joint Surg Am. 2008. December;90(12):2567-78.19047701 [Google Scholar]
- 4.O’Neill KM, Greenberg SL, Cherian M, Gillies RD, Daniels KM, Roy N, Raykar NP, Riesel JN, Spiegel D, Watters DA, Gruen RL. Bellwether procedures for monitoring and planning essential surgical care in low- and middle-income countries: caesarean delivery, laparotomy, and treatment of open fractures. World J Surg. 2016. November;40(11):2611-9. [DOI] [PubMed] [Google Scholar]
- 5.Bhangu A Ademuyiwa AO Aguilera ML, et al. ; GlobalSurg Collaborative. Surgical site infection after gastrointestinal surgery in high-income, middle-income, and low-income countries: a prospective, international, multicentre cohort study. Lancet Infect Dis. 2018. May;18(5):516-25. Epub 2018 Feb 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jamison DT, Summers LH, Alleyne G, Arrow KJ, Berkley S, Binagwaho A, Bustreo F, Evans D, Feachem RG, Frenk J, Ghosh G, Goldie SJ, Guo Y, Gupta S, Horton R, Kruk ME, Mahmoud A, Mohohlo LK, Ncube M, Pablos-Mendez A, Reddy KS, Saxenian H, Soucat A, Ulltveit-Moe KH, Yamey G. [Global health 2035: a world converging within a generation]. Salud Publica Mex. 2015. Sep-Oct;57(5):444-67. Spanish. [PubMed] [Google Scholar]
- 7.Fast O, Fast C, Fast D, Veltjens S, Salami Z, White MC. Limited sterile processing capabilities for safe surgery in low-income and middle-income countries: experience in the Republic of Congo, Madagascar and Benin. BMJ Glob Heal. 2017;2:e000428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bach O, Hope MJ, Chaheka CV, Dzimbiri KM. Disability can be avoided after open fractures in Africa-results from Malawi. Injury. 2004. September;35(9):846-51. [DOI] [PubMed] [Google Scholar]
- 9.Henley MB, Chapman JR, Agel J, Harvey EJ, Whorton AM, Swiontkowski MF. Treatment of type II, IIIA, and IIIB open fractures of the tibial shaft: a prospective comparison of unreamed interlocking intramedullary nails and half-pin external fixators. J Orthop Trauma. 1998. January;12(1):1-7. [DOI] [PubMed] [Google Scholar]
- 10.Bhandari M, Guyatt GH, Swiontkowski MF, Schemitsch EH. Treatment of open fractures of the shaft of the tibia. J Bone Joint Surg Br. 2001. January;83(1):62-8. [DOI] [PubMed] [Google Scholar]
- 11.Fu Q, Zhu L, Lu J, Ma J, Chen A. External fixation versus unreamed tibial intramedullary nailing for open tibial fractures: a meta-analysis of randomized controlled trials. Sci Rep. 2018. August 24;8(1):12753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ibrahim J, Liu M, Yusi K, Haonga B, Eliezer E, Shearer DW, Morshed S. Conducting a randomized controlled trial in Tanzania: Institute for Global Orthopaedics and Traumatology and the Muhimbili Orthopaedic Institute. J Orthop Trauma. 2018. October;32(Suppl 7):S47-51. [DOI] [PubMed] [Google Scholar]
- 13.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018. January;32(Suppl 1):S1-170. [DOI] [PubMed] [Google Scholar]
- 14.Gustilo RB, Mendoza RM, Williams DN. Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984. August;24(8):742-6. [DOI] [PubMed] [Google Scholar]
- 15.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009. April;42(2):377-81. Epub 2008 Sep 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dolan P. Modeling valuations for EuroQol health states. Med Care. 1997. November;35(11):1095-108. [DOI] [PubMed] [Google Scholar]
- 17.Litrenta J, Tornetta P, 3rd, Mehta S, Jones C, OʼToole RV, Bhandari M, Kottmeier S, Ostrum R, Egol K, Ricci W, Schemitsch E, Horwitz D. Determination of radiographic healing: an assessment of consistency using RUST and modified RUST in metadiaphyseal fractures. J Orthop Trauma. 2015. November;29(11):516-20. [DOI] [PubMed] [Google Scholar]
- 18.Nicoll EA. Fractures of the tibial shaft. A survey of 705 cases. J Bone Joint Surg Br. 1964. August;46:373-87. [PubMed] [Google Scholar]
- 19.Puno RM, Vaughan JJ, Stetten ML, Johnson JR. Long-term effects of tibial angular malunion on the knee and ankle joints. J Orthop Trauma. 1991;5(3):247-54. [DOI] [PubMed] [Google Scholar]
- 20.Haonga BT, Liu M, Wu HH, Zehraban Z, Eliezer EN. Reoperation rates following intramedullary nailing versus external fixation of Gustilo Type 3A open tibia shaft fractures. East African Orthop J. 2016;10:55-9. [Google Scholar]
- 21.Young S, Lie SA, Hallan G, Zirkle LG, Engesaeter LB, Havelin LI. Low infection rates after 34,361 intramedullary nail operations in 55 low- and middle-income countries: validation of the Surgical Implant Generation Network (SIGN) online surgical database. Acta Orthop. 2011. December;82(6):737-43. Epub 2011 Nov 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foote CJ, Guyatt GH, Vignesh KN, Mundi R, Chaudhry H, Heels-Ansdell D, Thabane L, Tornetta P, 3rd, Bhandari M. Which surgical treatment for open tibial shaft fractures results in the fewest reoperations? A network meta-analysis. Clin Orthop Relat Res. 2015. July;473(7):2179-92. Epub 2015 Feb 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raghunathan T, Lepkowski J, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001. June;27(1):85-95. [Google Scholar]
- 24.Mohseni MA, Soleimanpour J, Mohammadpour H, Shahsavari A. AO tubular external fixation vs. unreamed intramedullary nailing in open grade IIIA-IIIB tibial shaft fractures: a single-center randomized clinical trial. Pak J Biol Sci. 2011. April 15;14(8):490-5. [DOI] [PubMed] [Google Scholar]
- 25.Shayesteh Azar M, Karimi Nasab M, Sajadi Saravi M, Shafiee SE, Daneshpoor SM, Hadian A, Khademloo M. Comparison of intramedullary nailing and external fixation in the treatment of open tibial fractures. J Mazandaran Univ Med Sci. 2011;21(85):139-46. [Google Scholar]
- 26.Tu YK, Lin CH, Su JI, Hsu DT, Chen RJ. Unreamed interlocking nail versus external fixator for open type III tibia fractures. J Trauma. 1995. August;39(2):361-7. [DOI] [PubMed] [Google Scholar]
- 27.Marsh JL, Nepola JV, Wuest TK, Osteen D, Cox K, Oppenheim W. Unilateral external fixation until healing with the dynamic axial fixator for severe open tibial fractures. J Orthop Trauma. 1991;5(3):341-8. [DOI] [PubMed] [Google Scholar]
- 28.Bhandari M, Guyatt GH, Swiontkowski MF, Tornetta P, 3rd, Sprague S, Schemitsch EH. A lack of consensus in the assessment of fracture healing among orthopaedic surgeons. J Orthop Trauma. 2002. September;16(8):562-6. [DOI] [PubMed] [Google Scholar]
- 29.Milner SA, Davis TRC, Muir KR, Greenwood DC, Doherty M. Long-term outcome after tibial shaft fracture: is malunion important? J Bone Joint Surg Am. 2002. June;84(6):971-80. [DOI] [PubMed] [Google Scholar]
- 30.Sprague S, Petrisor BA, Jeray KJ, McKay P, Scott T, Heels-Ansdell D, Schemitsch EH, Liew S, Guyatt GH, Walter SD, Bhandari M. Factors associated with health-related quality of life in patients with open fractures. J Orthop Trauma. 2018. January;32(1):e5-11. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
A data-sharing statement is provided with the online version of the article (http://links.lww.com/JBJS/F713).