Abstract
Background:
Anterior column-posterior hemitransverse fractures are prevalent in the elderly and are often associated with quadrilateral surface (QLS) comminution. Several special QLS buttress plates have been introduced, but evidence of their comparability with traditional fixation devices is lacking. This biomechanical study aimed to compare special QLS buttress plates with traditional fixation devices.
Methods:
Anterior column-posterior hemitransverse fractures with an isolated QLS fragment were created on 24 composite hemipelves and were allocated to 4 fixation groups: (1) infrapectineal QLS buttress plate, (2) suprapectineal QLS buttress plate, (3) suprapectineal reconstruction plate with 3 periarticular long screws, and (4) infrapectineal reconstruction plate with 3 periarticular long screws. Specimens were loaded to simulate partial weight-bearing (35 to 350 N) or full weight-bearing (75 to 750 N). A testing machine was synchronized with a 3-dimensional video tracking system to optically track displacement at the points of interest and to calculate construct stiffness. The fixation systems were compared using the Kruskal-Wallis and Mann-Whitney U tests.
Results:
The experimental results of the partial and full weight-bearing simulations were surprisingly similar. During 40 loading cycles, the maximum displacement on the 6 predetermined points did not exceed 1.1 mm. Multiple-group comparisons of relative displacements of each predetermined measurement point did not differ significantly (p > 0.05). The suprapectineal reconstruction plate with 3 periarticular long screws demonstrated the greatest construct stiffness and significantly greater stiffness than the infrapectineal plate with long screws (p < 0.017). However, no significant difference (p > 0.017) in stiffness was identified between the infrapectineal QLS buttress plate and the suprapectineal reconstruction plate with long screws.
Conclusions:
The suprapectineal pelvic brim plate with 3 periarticular long screws remains the gold standard to treat anterior column-posterior hemitransverse fractures. The special infrapectineal QLS buttress plate provides stiffness and stability comparable with those of standard fixation. However, moving the pelvic brim plate from the suprapectineal border to the infrapectineal border is not recommended for anterior column-posterior hemitransverse fractures because it significantly decreases fixation stiffness.
Clinical Relevance:
Special QLS buttress plates may be an alternative fixation method for anterior column-posterior hemitransverse acetabular fractures in the elderly, especially when a less invasive anterior intrapelvic approach is selected.
As the worldwide population ages and the elderly remain active later in life, the incidence of acetabular fractures among patients >60 years of age has increased by 2 to 3 times over the past 3 decades1-3. The anterior column-posterior hemitransverse fracture pattern, the classic acetabular fracture in the geriatric population, is often associated with protrusion of the femoral head and medial migration of the quadrilateral surface (QLS)4-6.
To reduce and stabilize the medialization of the femoral head and QLS, stable fixation is indispensable, but the relative osteopenia in the elderly creates difficulty achieving adequate fracture fixation7,8. Early on, the most commonly reported fixation method for anterior column-posterior hemitransverse fractures was pelvic brim plates with long periarticular screws or additional infra-acetabular screws through the classic ilioinguinal approach9. Later, to improve direct visualization of the QLS, anterior intrapelvic approaches such as the modified Stoppa10,11, pararectus12,13, and supra-ilioinguinal14 have been popularized for infrapectineal and QLS buttress plating even closer to the ischial spine, all of which were parallel to the pelvic brim and perpendicular to the suprapectineal plate15. Placing the infrapectineal plate in the same plane as the displacement rather than perpendicular to the displacement (suprapectineal plate) may be more helpful for preventing protrusion in older patients16. Based on our team’s years of clinical experience in the surgical treatment of acetabular fractures, 2 special QLS buttress plates, the infrapectineal plate and the suprapectineal plate, were introduced and achieved good clinical results in our patients.
No comparative biomechanical data on these newly developed QLS buttress plates and traditional constructs are available with regard to the fixation of typical acetabular fractures in the elderly. Therefore, this biomechanical study aimed to determine which of 4 selected fixation constructs is the stiffest and best able to prevent secondary displacement of an anterior column-posterior hemitransverse fracture model with a free QLS fragment.
Materials and Methods
Specimens and Fracture Model
Twenty-four fourth-generation composite right large hemipelves (Sawbones; Pacific Research Laboratories) were used in this study. Referring to the study by May et al.5, a model of a typical acetabular fracture in the elderly (i.e., an anterior column-posterior hemitransverse fracture with disruption of the QLS) was created for the biomechanical assessment of 4 different fixation constructs. In pursuit of a consistent fracture model, computed tomographic (CT) data of the Sawbones hemipelvis were obtained to reconstruct a 3-dimensional model. An anterior column-posterior hemitransverse fracture model with QLS disruption and a corresponding osteotomy template similar to a jig were then designed (Mimics Suite 17.0, Materialise; and Geomagic Studio 2012, Raindrop Geomagic). The computer-aided design template was subsequently printed by rapid prototyping technology using nylon material, and a thin wire saw was used to create an identical osteotomy along the template.
Instrumentation
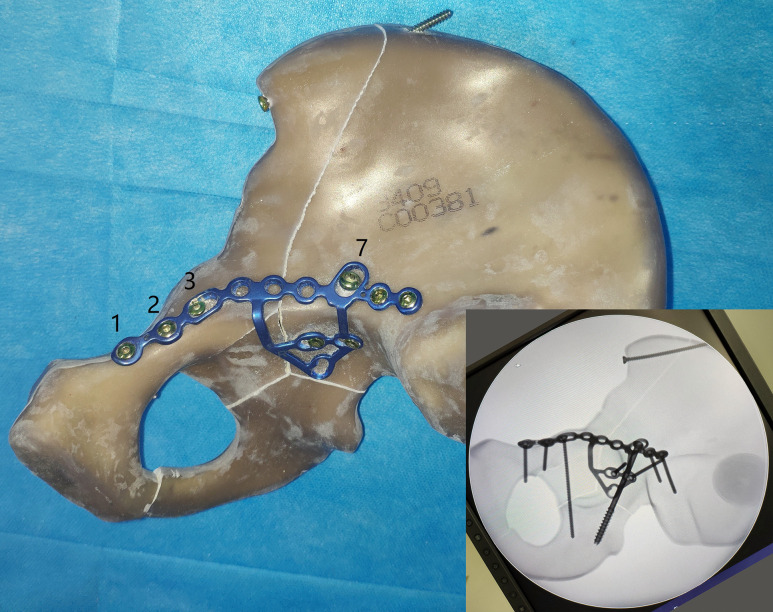
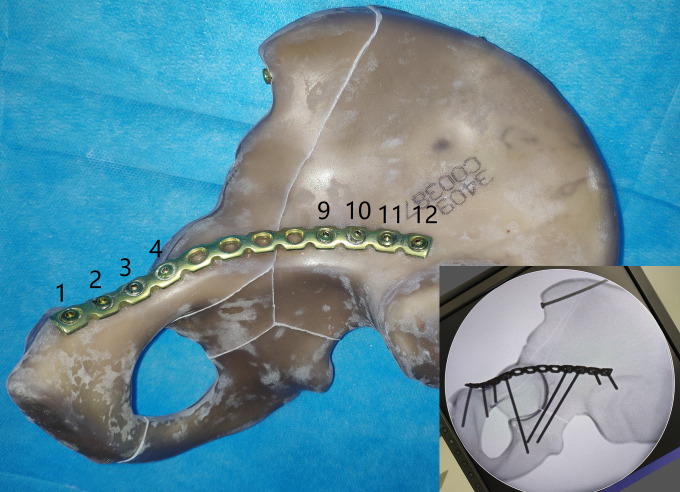
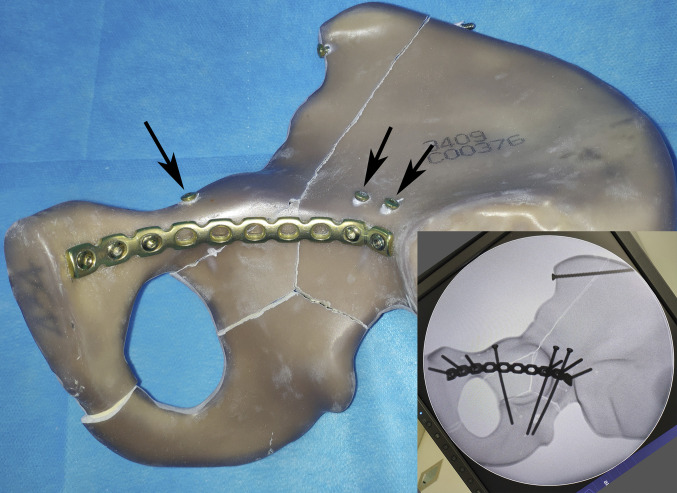
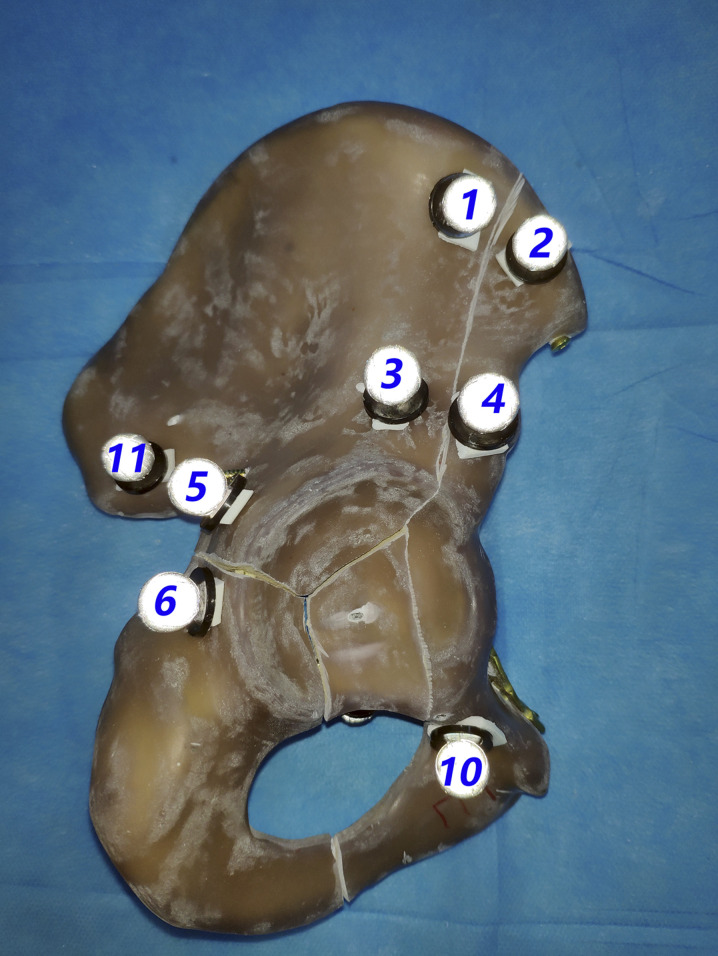
A total of 4 fixation constructs were tested and fluoroscopy was used to verify proper implant placement and fracture fixation (Figs. 1-A through 1-D): (1) special infrapectineal QLS buttress plate (Fig. 1-A); (2) special suprapectineal QLS buttress plate with an infra-acetabular screw (3.5-mm cortical screw, 80 mm) in hole 3 and a posterior column lag screw (7.3-mm cannulated lag screw, 90 mm) in hole 7 (Fig. 1-B); (3) 12-hole suprapectineal pelvic reconstruction plate with an infra-acetabular screw (3.5-mm cortical screw, 80 mm) in hole 4 and 2 posterior column screws (3.5-mm cortical screw, 90 mm) in holes 9 and 10 (Fig. 1-C); and (4) 10-hole infrapectineal pelvic reconstruction plate with 3 long periarticular screws, the same as in the suprapectineal reconstruction plate fixation construct (Fig. 1-D). An additional 3.5-mm cortical screw was inserted at the iliac crest to fix the high anterior column fracture in all groups.
Figs. 1-A through 1-D Photographs and fluoroscopic images showing the 4 different constructs for stabilization of the anterior column-posterior hemitransverse fracture.
Fig. 1-A.

A special infrapectineal QLS buttress plate.
Fig. 1-B.
A special suprapectineal QLS buttress plate with an infra-acetabular screw in hole 3 and a posterior column lag screw in hole 7.
Fig. 1-C.
A 12-hole suprapectineal pelvic reconstruction plate with an infra-acetabular screw in hole 4 and 2 posterior column screws in holes 9 and 10.
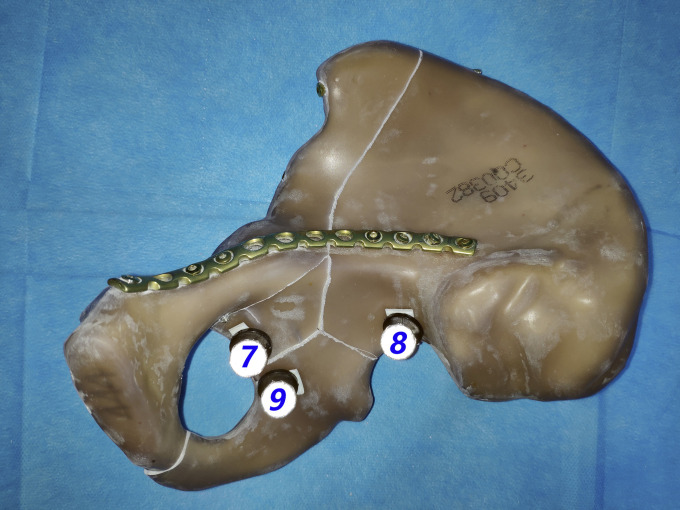
Fig. 1-D.
A 10-hole infrapectineal pelvic reconstruction plate with 3 long periarticular screws (black arrows), the same as in the suprapectineal reconstruction plate fixation construct.
Biomechanical Setup
We adopted a loading methodology similar to those mentioned by Chang et al.17 and Kistler et al.18. Similarly, the composite hemipelvis and femur (Sawbones; Pacific Research Laboratories) were coupled in a 3-dimensional model and the axis of the femoral neck was used as the biomechanical loading vector (SOLIDWORKS 2017; Dassault Systèmes SolidWorks). The axis should be oriented vertically in this coordinate system because of the design of the testing machine; meanwhile, a fixture for constraining the posterior aspect of the iliac bone and a block for supporting the symphysis were designed to maintain the hemipelvis model in a horizontal position. Thus, the symphysis was allowed sliding action in the horizontal plane, and movement was prevented in the direction of the applied force but was unrestricted in all directions perpendicular to the joint reaction force. For the femoral head, a custom-designed metal sphere with a 52-mm diameter was used to freely articulate with the acetabulum, similar to the test by Vigdorchik et al.19.
Biomechanical Testing
A testing machine (MTS Bionix Servohydraulics Test Systems Model 370.02; MTS Systems) was used to perform the mechanical loading. A 3-dimensional video tracking system (VICON VERO; Vicon Motion Systems) was used to track the 3-dimensional motion of the selected points on the hemipelvis and to measure displacement of the spatial coordinates20. A total of 12 markers were used, including 11 on the pelvis model and 1 on the testing machine as the calibration point. Eleven markers were attached to these selected points in pairs (Figs. 2-A and 2-B). Six pairs of markers located on opposite sides of the fracture site (1-2, 3-4, 5-6, 7-8, 7-9, and 7-10) were considered of interest, and their relative displacements were calculated in the 3-dimensional spatial coordinates. The spatial resolution of the system is in the order of 0.1 mm.
Figs. 2-A and 2-B Photographs showing a total of 11 infrared light-reflecting markers attached to the predetermined points along the fracture line of the anterior column-posterior hemitransverse fracture model.
Fig. 2-A.
Markers 1, 2, 3, 4, 5, 6, 10, and 11.
Fig. 2-B.
Markers 7, 8, and 9.
Loading Protocol
The 4 different fixation constructs (6 Sawbones specimens per fixation group) were compared in terms of displacements along the fracture sites, especially of the QLS. Three phases of mechanical loading were applied to each sample based on previously published data using the following protocol: (1) 250 settling cycles of 17.5 to 175 N at a machine velocity of 60 mm/min, (2) 20 cycles of 35 to 350 N at a machine velocity of 10 mm/min with optical tracking simulating the postoperative phase of recommended partial weight-bearing (according to May et al.5), and (3) 20 cycles of 75 to 750 N at a machine velocity of 10 mm/min with optical tracking simulating the single-leg stance (according to Culemann et al.4).
Data Collection
For each loading cycle, force and displacement data were recorded by a personal computer connected with the MTS Bionix. We defined the axial stiffness (in N/mm) of the construct as the slope of the force-displacement curves generated from the test system.
The marker data were synchronized in MATLAB (MathWorks) for characterizing the motion at each pair of markers crossing the fracture lines. The relative displacement (in millimeters) of the fracture line was defined according to the maximum change of the relative distance of each pair of markers in the spatial coordinates.
The first loading phase (17.5 to 175-N loading, 250 cycles) was our preloading test, which aimed to achieve a relatively stable state between the system and the constructs, so no data collection was performed. Data were collected during the subsequent 2 loading phases (35 to 350 N and 75 to 700 N).
Statistical Analysis
The statistical analysis was performed using MATLAB software. Nonparametric tests were used because the sample values were not normally distributed according to the homogeneity test of variance. First, a multiple-group comparison of the 4 groups were performed using the Kruskal-Wallis test with significance set at p = 0.05. Next, if the multiple comparisons showed a significant difference (p < 0.05), the Mann-Whitney U test was used to compare the group with the suprapectineal reconstruction plate and long screws with each of the 3 other groups. The Bonferroni correction was utilized in these post hoc pairwise comparisons, with p < 0.017 being considered significant.
Results
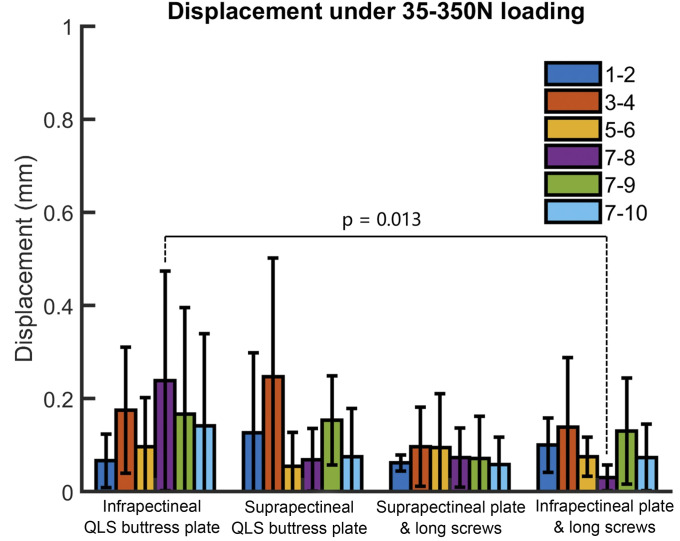
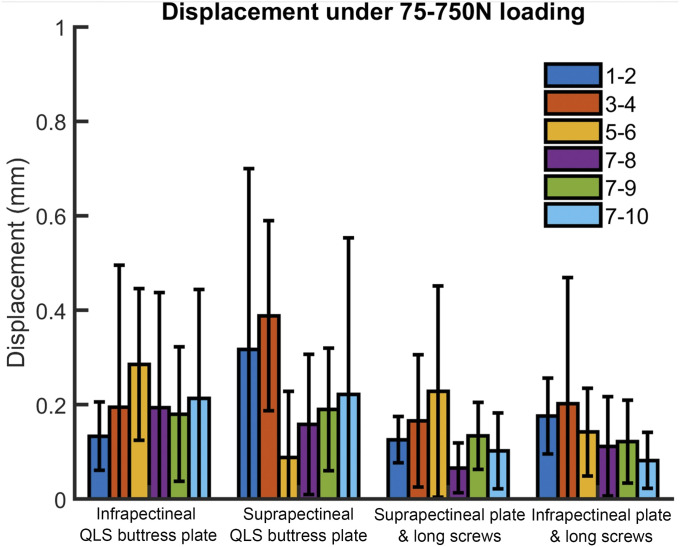
The relative displacements of the 6 predetermined pairs of measurement points for all 4 groups are presented as the median and the range in Table I (35 to 350-N loading cycle) and Table II (75 to 750-N loading cycle). These tables also show the p values for the multiple-group comparisons. The maximum displacement of the measurement point pairs among all specimens did not exceed 1 mm except for points 1 and 2 in the 75 to 750-N loading test (1.08 mm). From the distribution trend of the bar graph (Figs. 3 and 4), the displacement value of each measurement point pair in the other 3 groups was greater than that in the group with the suprapectineal reconstruction plate and long screws; however, multiple-group comparisons showed no significant difference among the 4 groups (p > 0.05).
Fig. 3.
Bar graph showing the values of relative displacement in millimeters for the 4 groups at the 6 predetermined measurement points under the 35 to 350-N loading test. The differences with significance are indicated with a p value. The bars indicate the mean and the error bars indicate the standard deviation.
Fig. 4.
Bar graph showing the values of relative displacement in millimeters for the 4 groups at the 6 predetermined measurement points under the 75 to 750-N loading test. The bars indicate the mean and the error bars indicate the standard deviation.
TABLE I.
Displacements at Predetermined Measurement Points Under 35 to 350-N Loading Tests
| Paired Markers | Group | P Value† | |||
| Infrapectineal QLS Buttress Plate* | Suprapectineal QLS Buttress Plate* | Suprapectineal Reconstruction Plate with Long Screws* | Infrapectineal Reconstruction Plate with Long Screws* | ||
| 1-2 | 0.06 (0.01 to 0.14) | 0.05 (0.01 to 0.46) | 0.07 (0.04 to 0.08) | 0.10 (0.03 to 0.18) | 0.738 |
| 3-4 | 0.16 (0.02 to 0.37) | 0.17 (0.03 to 0.74) | 0.08 (0.02 to 0.23) | 0.09 (0.04 to 0.43) | 0.579 |
| 5-6 | 0.07 (0 to 0.28) | 0.03 (0.01 to 0.20) | 0.07 (0 to 0.32) | 0.07 (0.02 to 0.14) | 0.717 |
| 7-8 | 0.12 (0.04 to 0.55) | 0.05 (0.01 to 0.20) | 0.06 (0.01 to 0.18) | 0.03 (0 to 0.06) | 0.056 |
| 7-9 | 0.08 (0.05 to 0.63) | 0.16 (0.03 to 0.29) | 0.05 (0 to 0.25) | 0.11 (0.01 to 0.22) | 0.394 |
| 7-10 | 0.08 (0.03 to 0.54) | 0.03 (0.02 to 0.28) | 0.04 (0.01 to 0.17) | 0.05 (0.01 to 0.18) | 0.535 |
The values are given as the median in millimeters, with the range in parentheses.
Multiple-group comparisons were performed with use of the Kruskal-Wallis test with a significance level of p = 0.05.
TABLE II.
Displacements at Predetermined Measurement Points Under 75 to 750-N Loading Tests
| Paired Markers | Group | P Value† | |||
| Infrapectineal QLS Buttress Plate* | Suprapectineal QLS Buttress Plate* | Suprapectineal Reconstruction Plate with Long Screws* | Infrapectineal Reconstruction Plate with Long Screws* | ||
| 1-2 | 0.12 (0.05 to 0.26) | 0.21 (0 to 1.08) | 0.11 (0.06 to 0.18) | 0.16 (0.09 to 0.30) | 0.295 |
| 3-4 | 0.10 (0.02 to 0.14) | 0.45 (0.05 to 0.62) | 0.23 (0 to 0.29) | 0.10 (0.01 to 0.65) | 0.297 |
| 5-6 | 0.27 (0.11 to 0.49) | 0.03 (0 to 0.36) | 0.15 (0.01 to 0.55) | 0.17 (0.03 to 0.24) | 0.120 |
| 7-8 | 0.07 (0.03 to 0.66) | 0.15 (0.01 to 0.43) | 0.04 (0.01 to 0.14) | 0.09 (0.01 to 0.25) | 0.657 |
| 7-9 | 0.14 (0.02 to 0.38) | 0.17 (0.07 to 0.44) | 0.17 (0.02 to 0.19) | 0.14 (0.01 to 0.23) | 0.846 |
| 7-10 | 0.15 (0.01 to 0.55) | 0.09 (0.02 to 0.89) | 0.07 (0.04 to 0.24) | 0.06 (0.02 to 0.15) | 0.912 |
The values are given as the median in millimeters, with the range in parentheses.
Multiple-group comparisons were performed with use of the Kruskal-Wallis test with a significance level of p = 0.05.
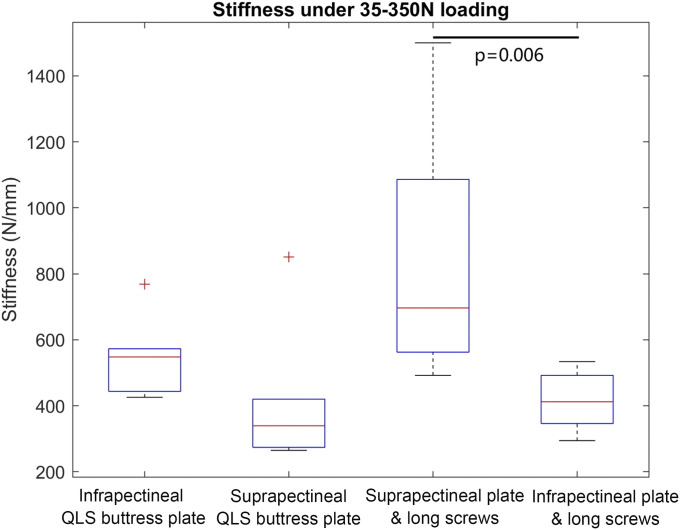
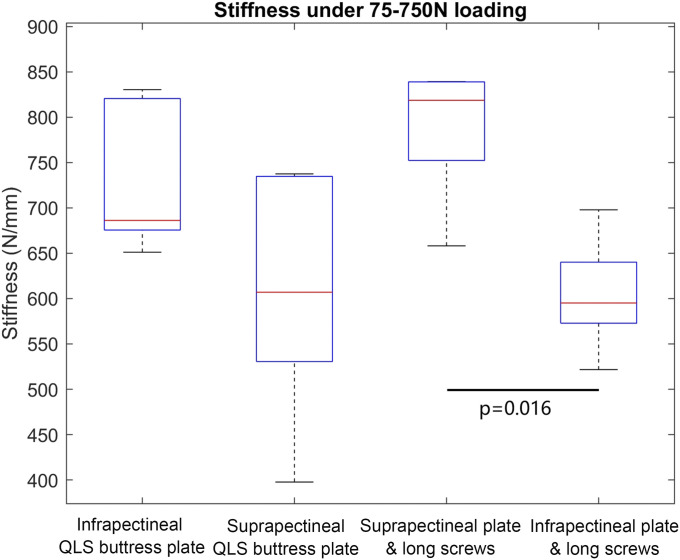
The axial stiffnesses of all 4 fixation constructs under the 35 to 350-N and 75 to 750-N loading cycles are presented as the median and the range and as the mean and the standard deviation in Table III. Box-and-whisker plots are depicted with p values when the differences were significant in Figures 5 and 6. For the 35 to 350-N loading phase, the standard suprapectineal reconstruction plating fixation construct demonstrated the greatest stiffness (838.96 ± 385.01 N/mm), a significant difference (p = 0.006) from the infrapectineal reconstruction plating fixation construct (415.12 ± 96.08 N/mm). However, there was no difference between the standard suprapectineal fixation and the infrapectineal QLS buttress plate (551.02 ± 122.46 N/mm; p = 0.132) or the suprapectineal QLS buttress plate (414.77 ± 221.27 N/mm; p = 0.026).
Fig. 5.
Box-and-whisker plots showing the values of axial stiffness in N/mm for the 4 different fixation constructs under the 35 to 350-N loading test. The horizontal red line in each box indicates the median value, the top and bottom borders of the box show the 75th and 25th percentiles, the whiskers show the 10th and 90th percentiles, and the + symbols show outliers. The differences with significance are indicated with a p value.
Fig. 6.
Box-and-whisker plots showing the values of axial stiffness in N/mm for the 4 different fixation constructs under the 75 to 750-N loading test. The horizontal red line in each box indicates the median value, the top and bottom borders of the box show the 75th and 25th percentiles, and the whiskers show the 10th and 90th percentiles. The differences with significance are indicated with p values.
TABLE III.
Axial Stiffness for All 4 Constructs
| Stiffness Under 35 to 350-N Loading | Stiffness Under 75 to 750-N Loading | |
| Infrapectineal QLS buttress plate | ||
| Median* | 547.87 (425.68 to 768.29) | 686.19 (651.15 to 830.37) |
| Mean† | 551.02 ± 122.46 | 725.01 ± 78.95 |
| Suprapectineal QLS buttress plate | ||
| Median* | 339.34 (264.71 to 851.35) | 607 (397.66 to 737.51) |
| Mean† | 414.77 ± 221.27 | 602.41 ± 128.86 |
| Suprapectineal reconstruction plate with long screws | ||
| Median* | 696.43 (492.19 to 1,500) | 818.61 (658.15 to 839.21) |
| Mean† | 838.96 ± 385.01 | 787.71 ± 151.76 |
| Infrapectineal reconstruction plate with long screws | ||
| Median* | 412.04 (294.39 to 492.19) | 595.12 (521.69 to 697.9) |
| Mean† | 415.12 ± 96.08 | 605.09 ± 127.01 |
| P value for multiple-group comparison‡ | 0.011§ | 0.020§ |
| P value for pairwise comparisons# | ||
| Infrapectineal QLS buttress plate vs. suprapectineal reconstruction plate with long screws | 0.132 | 0.329 |
| Suprapectineal QLS buttress plate vs. suprapectineal reconstruction plate with long screws | 0.026 | 0.017 |
| Infrapectineal reconstruction plate with long screws vs. suprapectineal reconstruction plate with long screws | 0.006§ | 0.016§ |
The values are given as the median in N/mm, with the range in parentheses.
The values are given as the mean in N/mm and the standard deviation.
Multiple-group comparisons were performed with use of the Kruskal-Wallis test with a significance level of p = 0.05.
Significant.
Pairwise comparisons were performed with use of the Mann-Whitney U test with Bonferroni correction with a significance level of p = 0.017.
For the 75 to 750-N loading cycle, similarly, the standard suprapectineal reconstruction plating fixation (787.71 ± 151.76 N/mm) demonstrated a stiffness greater than those of the other tested groups and showed a significant difference (p = 0.016) compared with the infrapectineal reconstruction plating construct (605.09 ± 127.01 N/mm). Again, the stiffnesses of the infrapectineal QLS buttress plate (725.01 ± 78.95 N/mm, p = 0.329) and the suprapectineal QLS buttress plate (602.41 ± 128.86 N/mm, p = 0.017) were comparable with that of the standard suprapectineal fixation.
The results of the post hoc power analysis are shown in Table IV.
TABLE IV.
Post Hoc Power Analysis of the 4 Outcomes
| Parameter and Loading Cycle | Effect Size f* | Power† |
| Displacement | ||
| 35 to 350 N | 0.16 | 8.2% |
| 75 to 750 N | 0.48 | 41.0% |
| Stiffness | ||
| 35 to 350 N | 1.41 | 99.9% |
| 75 to 750 N | 1.00 | 97.4% |
A value of 0.10 indicates small, 0.25 indicates medium, and 0.40 indicates large.
A value of ≥80% is desired.
Discussion
The anterior column-posterior hemitransverse fracture pattern with protrusion of the femoral head and medial migration of the QLS is prevalent in the growing elderly population. Anatomical reduction resulting in a congruent hip joint is the ultimate goal, but adequate internal fixation can maintain fracture reduction and allow painless early mobility until fracture-healing is achieved5,18,21. The choice of internal fixation for such acetabular fractures involving the QLS (suprapectineal or infrapectineal plating fixation and periarticular long screws or QLS buttress plating fixation) is controversial. However, to our knowledge, no direct biomechanical comparison between suprapectineal and infrapectineal fixation has been performed to date.
Although biomechanical studies showed that plate fixation with long periarticular screws was comparable with or superior to QLS buttress plating in biomechanical stability, the insertion of these screws always bears the risk of joint penetration and offers inadequate stability with a high risk of failure and poor outcomes; thus, a secondary hip arthroplasty is required afterward16,22. Therefore, we have developed 2 special QLS buttress plates, suprapectineal and infrapectineal, that have demonstrated good clinical results in our patients. Similarly, no comparative biomechanical data on these newly developed QLS buttress plates and classic fixation constructs are available.
Based on the above 2 points, a typical acetabular fracture model in the elderly (anterior column-posterior hemitransverse) with QLS disruption was created for the biomechanical assessment of 4 different fixation constructs. Because suprapectineal plating fixation with long periarticular screws represents the gold standard for stabilizing anterior column-posterior hemitransverse fractures, it was designated as the control group in this experiment4-6. Therefore, a total of 3 pairwise comparisons were used to explore the biomechanical stiffness and stability of each fixation construct between standard suprapectineal reconstruction plating fixation and the other 3 fixations (infrapectineal QLS buttress plate, suprapectineal QLS buttress plate, and infrapectineal reconstruction plate with 3 periarticular long screws).
To simulate the postoperative phase of recommended partial weight-bearing, 20 cycles of 35 to 350-N loading were performed after 250 settling preload cycles of 17.5 to 175 N. Because the maximum displacement of the predetermined point pairs among all specimens did not exceed 1.1 mm, the medial displacement of the quadrilateral plate was sufficiently prevented by the 4 fixation constructs under the modeled biomechanical conditions5. The multiple-group comparison of relative displacements on each predetermined measurement point pair among the 4 groups showed no significant difference (p > 0.05). However, the comparison of construct stiffness showed that the standard fixation method performed better than the other methods. Importantly, the infrapectineal QLS buttress plate that spans both columns through the QLS was statistically comparable with the standard fixation construct, with only a trend toward a difference (p = 0.132). This finding is similar to those of previous studies demonstrating that the final stiffness of the infrapectineal QLS buttress plate was comparable with traditional fixation constructs in a transtectal transverse model18. In addition, the pairwise comparison showed that suprapectineal reconstruction plating fixation was significantly stiffer than infrapectineal fixation (p = 0.006). This might be explained by the mechanics of the normal hip joint during stance (i.e., the weight-bearing area of the hip joint is concentrated in the superior region). Therefore, the standard fixation construct comprised a suprapectineal plate supporting superiorly along the pelvic brim, which biomechanically constitutes a bridge between the weight-bearing acetabular roof and the pelvis, obtaining the best stability.
For various reasons, partial weight-bearing is often not practical in the elderly. Therefore, another 20 cycles of 75 to 750-N loading were performed after the 35 to 350-N loading cycle to simulate the full weight-bearing phase. Interestingly, the experimental results were strikingly similar to those shown above.
Overall, for partial or full weight-bearing loading simulations, the suprapectineal pelvic brim plate with 3 periarticular long screws represents the gold standard for stabilizing the anterior column-posterior hemitransverse fracture pattern. The special infrapectineal QLS buttress plate provides stiffness and stability comparable with those of the standard fixation construct.
A successful acetabular fracture surgical procedure consists of more than just an appropriate fixation construct; an improved surgical approach is also necessary, especially for elderly patients. Traditionally, the standard suprapectineal plate combined with periarticular long screws is usually inserted using an ilioinguinal approach, which requires laborious exposure and is associated with a high complication rate. Recent advances in surgical approaches, including the emergence of less invasive intrapelvic approaches such as the modified Stoppa, pararectus, or supra-ilioinguinal approaches10-14, provide improved access to the QLS and the medial aspect of the posterior column with lower patient morbidity. Afterward, buttress plating of the medial wall and spanning fixation from the posterior to anterior columns via a single anterior incision became possible15,18. Thus, in the present study, we compared the strength and construct stiffness of 2 such QLS buttress plates with the standard bicolumnar fixation methods using a column plate and periarticular long screws and revealed that these newer QLS buttress plates are biomechanically viable options when the less invasive anterior intrapelvic approach is desired for anterior column-posterior hemitransverse fracture stabilization.
This study had several limitations. First, artificial bone models could not represent the biological changes that occur in vivo because of the absence of soft-tissue and muscular forces, which may have affected test results. Second, the Sawbones model was produced in accordance with normal bone density, which did not account for the osteopenia in the typical elderly patient with an anterior column-posterior hemitransverse fracture. Third, the artificial bones showed higher stiffness than human bones and the uniform property distribution within the foam core did not account for the natural variations in density and force distribution seen throughout the human bones23. Fourth, a sample size of 6 per study group may be considered relatively small, and, as a result, some biomechanically meaningful differences may have been missed. A future biomechanical study design with a larger number of samples is needed. Other limitations were that 1 marker per fragment was not sufficient to determine the movements between the fragments. Three markers per fragment would be feasible, but it is admittedly challenging.
In conclusion, this biomechanical study assessed 4 fixation constructs for stabilizing anterior column-posterior hemitransverse fractures with QLS disruption. All 4 constructs could maintain stable fixation under simulated partial or full weight-bearing activity. Meanwhile, the suprapectineal pelvic brim plate with 3 periarticular long screws remains the gold standard. Importantly, the special infrapectineal QLS buttress plate provides stiffness and stability comparable with the standard fixation construct. Therefore, in situations in which a less invasive anterior approach is desired, the use of newer QLS buttress plates presents an alternative fixation method that is at least comparable with standard forms of fixation at resisting fracture motion and medial subluxation. However, it is not recommended to move the pelvic brim plate from the suprapectineal border to the infrapectineal border for anterior column-posterior hemitransverse fractures because it will significantly decrease the fixation strength.
Acknowledgments
Note: The authors gratefully acknowledge Zhimin Lai, Chongbing Liu, Zhonghua Lian, and Yanjie Ye from Double Medical Technology for their technical assistance and Zhenping Yin from the School of Electronic Information, Wuhan University, Wuhan, China, for performing the statistical analysis.
Footnotes
Investigation performed at the Department of Orthopaedics, Union Hospital, Tongji Medical College, Huazhong University of Science & Technology, Wuhan, People’s Republic of China
Disclosure: The National Natural Science Foundation of China (grants No. 81672158 and No. 81371939) funded the purchase of composite hemipelves, and the National Key R&D Program of China (2016YFC1100100) funded testing fees. The implants for the osteosynthesis were provided by Double Medical Technology, Inc. (Xiamen, China). Double Medical Technology, Inc. did not play any role in the data analysis or the writing of this article. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJS/F792).
References
- 1.Archdeacon MT, Kazemi N, Collinge C, Budde B, Schnell S. Treatment of protrusio fractures of the acetabulum in patients 70 years and older. J Orthop Trauma. 2013. May;27(5):256-1-9. [DOI] [PubMed] [Google Scholar]
- 2.Butterwick D, Papp S, Gofton W, Liew A, Beaulé PE. Acetabular fractures in the elderly: evaluation and management. J Bone Joint Surg Am. 2015. May 6;97(9):758-1-9. [DOI] [PubMed] [Google Scholar]
- 3.Antell NB, Switzer JA, Schmidt AH. Management of acetabular fractures in the elderly. J Am Acad Orthop Surg. 2017. August;25(8):577-1-9. [DOI] [PubMed] [Google Scholar]
- 4.Culemann U, Holstein JH, Köhler D, Tzioupis CC, Pizanis A, Tosounidis G, Burkhardt M, Pohlemann T. Different stabilisation techniques for typical acetabular fractures in the elderly—a biomechanical assessment. Injury. 2010. April;41(4):405-1-9 Epub 2009 Dec 24. [DOI] [PubMed] [Google Scholar]
- 5.May C, Egloff M, Butscher A, Keel MJB, Aebi T, Siebenrock KA, Bastian JD. Comparison of fixation techniques for acetabular fractures involving the anterior column with disruption of the quadrilateral plate: a biomechanical study. J Bone Joint Surg Am. 2018. June 20;100(12):1047-1-9. [DOI] [PubMed] [Google Scholar]
- 6.Tanoğlu O, Alemdaroğlu KB, İltar S, Özmeriç A, Demir T, Erbay FK. Biomechanical comparison of three different fixation techniques for anterior column posterior hemitransverse acetabular fractures using anterior intrapelvic approach. Injury. 2018. August;49(8):1513-1-9 Epub 2018 Jun 18. [DOI] [PubMed] [Google Scholar]
- 7.Spitler CA, Kiner D, Swafford R, Doty D, Goulet R, Jones LC, Hydrick J, Nowotarski P. Generating stability in elderly acetabular fractures-a biomechanical assessment. Injury. 2017. October;48(10):2054-1-9 Epub 2017 Jul 24. [DOI] [PubMed] [Google Scholar]
- 8.Mears DC. Surgical treatment of acetabular fractures in elderly patients with osteoporotic bone. J Am Acad Orthop Surg. 1999. Mar-Apr;7(2):128-1-9. [DOI] [PubMed] [Google Scholar]
- 9.Letournel E. The treatment of acetabular fractures through the ilioinguinal approach. Clin Orthop Relat Res. 1993. July;292:62-1-9. [PubMed] [Google Scholar]
- 10.Cole JD, Bolhofner BR. Acetabular fracture fixation via a modified Stoppa limited intrapelvic approach. Description of operative technique and preliminary treatment results. Clin Orthop Relat Res. 1994. August;305:112-1-9. [PubMed] [Google Scholar]
- 11.Sagi HC, Afsari A, Dziadosz D. The anterior intra-pelvic (modified Rives-Stoppa) approach for fixation of acetabular fractures. J Orthop Trauma. 2010. May;24(5):263-1-9. [DOI] [PubMed] [Google Scholar]
- 12.Keel MJB, Ecker TM, Cullmann JL, Bergmann M, Bonel HM, Büchler L, Siebenrock KA, Bastian JD. The pararectus approach for anterior intrapelvic management of acetabular fractures: an anatomical study and clinical evaluation. J Bone Joint Surg Br. 2012. March;94(3):405-1-9. [DOI] [PubMed] [Google Scholar]
- 13.Märdian S, Schaser KD, Hinz P, Wittenberg S, Haas NP, Schwabe P. Fixation of acetabular fractures via the ilioinguinal versus pararectus approach: a direct comparison. Bone Joint J. 2015. September;97-B(9):1271-1-9. [DOI] [PubMed] [Google Scholar]
- 14.Chen K, Ji Y, Huang Z, Navinduth R, Yang F, Sun T, Xiong Z, Yao S, Ahn J, Guo X. Single modified ilioinguinal approach for the treatment of acetabular fractures involving both columns. J Orthop Trauma. 2018. November;32(11):e428-1-9. [DOI] [PubMed] [Google Scholar]
- 15.Qureshi AA, Archdeacon MT, Jenkins MA, Infante A, DiPasquale T, Bolhofner BR. Infrapectineal plating for acetabular fractures: a technical adjunct to internal fixation. J Orthop Trauma. 2004. March;18(3):175-1-9. [DOI] [PubMed] [Google Scholar]
- 16.Laflamme GY, Hebert-Davies J, Rouleau D, Benoit B, Leduc S. Internal fixation of osteopenic acetabular fractures involving the quadrilateral plate. Injury. 2011. October;42(10):1130-1-9 Epub 2010 Dec 14. [DOI] [PubMed] [Google Scholar]
- 17.Chang JK, Gill SS, Zura RD, Krause WR, Wang GJ. Comparative strength of three methods of fixation of transverse acetabular fractures. Clin Orthop Relat Res. 2001. November;392:433-1-9. [DOI] [PubMed] [Google Scholar]
- 18.Kistler BJ, Smithson IR, Cooper SA, Cox JL, Nayak AN, Santoni BG, Sagi HC. Are quadrilateral surface buttress plates comparable to traditional forms of transverse acetabular fracture fixation? Clin Orthop Relat Res. 2014. November;472(11):3353-1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vigdorchik JM, Jin X, Sethi A, Herzog DT, Oliphant BW, Yang KH, Vaidya R. A biomechanical study of standard posterior pelvic ring fixation versus a posterior pedicle screw construct. Injury. 2015. August;46(8):1491-1-9 Epub 2015 May 7. [DOI] [PubMed] [Google Scholar]
- 20.van Zwienen CMA, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB. Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma. 2004. October;18(9):589-1-9. [DOI] [PubMed] [Google Scholar]
- 21.Chen K, Yang F, Yao S, Xiong Z, Sun T, Zhu F, Telemacque D, Drepaul D, Ren Z, Guo X. Application of computer-assisted virtual surgical procedures and three-dimensional printing of patient-specific pre-contoured plates in bicolumnar acetabular fracture fixation. Orthop Traumatol Surg Res. 2019. September;105(5):877-1-9 Epub 2019 Jul 9. [DOI] [PubMed] [Google Scholar]
- 22.Mears DC, Velyvis JH. Acute total hip arthroplasty for selected displaced acetabular fractures: two to twelve-year results. J Bone Joint Surg Am. 2002. January;84(1):1-1-9. [DOI] [PubMed] [Google Scholar]
- 23.Girardi BL, Attia T, Backstein D, Safir O, Willett TL, Kuzyk PR. Biomechanical comparison of the human cadaveric pelvis with a fourth generation composite model. J Biomech. 2016. February 29;49(4):537-1-9 Epub 2016 Jan 22. [DOI] [PubMed] [Google Scholar]