Abstract
Background:
Comparative time to recovery after operative and nonoperative treatment for rotator cuff tears is an important consideration for patients. Hence, we compared the time to achieve clinically meaningful reduction in shoulder pain and function after treatment.
Methods:
From February 2011 to June 2015, a multicenter cohort of patients with rotator cuff tears undergoing operative or nonoperative treatment was recruited. After propensity score weighting, the Kaplan-Meier method was used to estimate the time to achieve a minimal clinically important difference (MCID), >30% reduction, and >50% reduction in the Shoulder Pain and Disability Index (SPADI) and the American Shoulder and Elbow Surgeons (ASES) scores. (In our analysis, both ASES and SPADI were coded such that a lower number corresponded to a better outcome; thus, the word “reduction” was used to indicate improvement in both ASES and SPADI scores.) A 2-stage test was conducted to detect a difference between the 2 groups.
Results:
In this cohort, 96 patients underwent nonoperative treatment and 73 patients underwent a surgical procedure. The surgical treatment group and the nonoperative treatment group were significantly different with respect to SPADI and ASES scores (p < 0.05). The maximum difference between groups in achievement of the MCID for the SPADI scores was at 3.25 months, favoring the nonoperative treatment group. The probability to achieve the MCID was 0.06 (95% confidence interval [CI], 0.00 to 0.12) for the surgical treatment group compared with 0.40 (95% CI, 0.29 to 0.50) for the nonoperative treatment group. The surgical treatment group had a greater probability of achieving >50% reduction in SPADI scores at 15.49 months (0.20 [95% CI, 0.12 to 0.29] for the surgical treatment group compared with 0.04 [95% CI, 0.00 to 0.09] for the nonoperative treatment group). The surgical treatment group had a greater probability of achieving >50% reduction in ASES scores at 24.74 months (0.96 [95% CI, 0.84 to 0.99] for the surgical treatment group compared with 0.66 [95% CI, 0.53 to 0.75] for the nonoperative treatment group). The differences for >30% reduction in SPADI and ASES scores and the MCID for ASES scores were not significant.
Conclusions:
Patients undergoing nonoperative treatment had significantly better outcomes in the initial follow-up period compared with patients undergoing a surgical procedure, but this trend reversed in the longer term. These data can be used to inform expectations for nonoperative and operative treatments for rotator cuff tears.
Level of Evidence:
Therapeutic Level II. See Instructions for Authors for a complete description of levels of evidence.
Shoulder pain has a lifetime prevalence of up to 66.7%1, and a common related etiology is a rotator cuff tear2. The prevalence of rotator cuff tears, including symptomatic tears, increases with age3. The numbers of medical visits and surgical procedures for rotator cuff tears have increased considerably in the last decade4,5 and will likely continue to increase with an aging and more active U.S. population. Despite the high prevalence and patient burden6 of rotator cuff tears, there is sparse evidence to guide clinical decision-making when providing nonoperative and operative treatment options for patients7. We have previously published comparative outcomes of nonoperative and surgical treatments at up to 18 months in patients with rotator cuff tears8. Patients are interested to know how quickly and to what magnitude the shoulder will improve after nonoperative and operative treatments, especially in the longer term; these data have not been published from our cohort. Data to guide informed decision-making are lacking in this area from studies that compare both treatments.
In a well-defined prospective cohort of patients diagnosed with rotator cuff tears, we compared the time to achieve clinically meaningful improvement in shoulder pain and function between operative and nonoperative treatment groups. We hypothesized that patients undergoing surgical treatment would achieve a greater magnitude of recovery in shoulder pain and function but at a later follow-up than patients undergoing nonoperative treatment.
Materials and Methods
Patient Population
Patients were recruited as part of a multicenter, longitudinal cohort study termed the Rotator Cuff Outcomes Workgroup (ROW). Additional details about the ROW cohort have been previously published9-13. We included patients who were diagnosed with symptomatic partial or full rotator cuff tears from 3 academic and 1 community outpatient sports or shoulder clinics from February 2011 to June 2015. A sports medicine or shoulder fellowship-trained physician with expertise in shoulder pathologies clinically diagnosed the rotator cuff tear. Additional details on how a diagnosis was established is provided later. Patients were recruited by shoulder experts in specialty clinics and not in primary care clinics to ensure more accurate and consistent diagnoses. All patients were at least 45 years of age and had experienced at least 4 weeks of shoulder symptoms. Patients with a concurrent shoulder fracture, active cervical radiculopathy (defined as neck pain radiating to the shoulder or arm), or prior ipsilateral shoulder surgical procedure were excluded. All inclusion and exclusion criteria were applied to the symptomatic shoulder. The decision for a surgical procedure was established between the patient and the treating physician with shared decision-making. Patients who completed the baseline questionnaire and who were advised to undergo surgical or nonoperative treatment for rotator cuff tear were included in this analysis (n = 169) (see Appendix). All patients provided informed consent, and the study was approved by the appropriate institutional review boards.
Structured History Questionnaire and Outcome Measures
All patients completed a structured questionnaire at enrollment. An abbreviated version of this questionnaire was then mailed to patients at each follow-up time. The questionnaire included questions with regard to basic demographic information, alcohol and tobacco use, shoulder use at work, education level, onset of symptoms, and patient expectation for improvement. Patients also completed a modified Fear-Avoidance Beliefs Questionnaire (FABQ)14 and the 5-question Mental Health Inventory (MHI-5)15.
Shoulder pain and function outcomes were measured using the Shoulder Pain and Disability Index (SPADI)16 and the American Shoulder and Elbow Surgeons (ASES) Standardized Shoulder Form17. The SPADI is a self-administered 13-item questionnaire developed to measure pain and disability associated with shoulder pathology. Scores range from 0 to 100 points, with higher scores indicating worse pain and function. The ASES score is another common outcome measure of shoulder pain and function. Similar to the SPADI score, it is also scored from 0 to 100 points, but with lower scores indicating more severe pain and function.
The minimal clinically important difference (MCID) is defined as the smallest improvement of a given outcome that a patient perceives as beneficial and would mandate a change in patient management18. Based on prior studies, the MCID from baseline is a decrease of 10.0 points19 for the SPADI scores and an increase of 13.9 points20 for the ASES scores. In our analysis, both ASES and SPADI were coded such that a lower number corresponded to a better outcome; thus, the word “reduction” was used to indicate improvement in both ASES and SPADI scores.
Diagnostic Imaging
Shoulder magnetic resonance imaging (MRI) scans were read blinded by 2 authors of the study (N.B.J. and either L.D.H. or J.E.K.). Our methodology with regard to MRI review in this study has been previously described12 and showed good interrater and intrarater reliability compared with readings by a musculoskeletal radiologist.
Diagnosis of Rotator Cuff Tear
The diagnosis of a rotator cuff tear in this study was determined both clinically by attending-level physicians who had received additional fellowship training in sports medicine or shoulder pathologies and by MRI findings indicating rotator cuff pathology. We ensured the inclusion of patients without MRI scans (n = 24), as patients who do not undergo surgical intervention (i.e., nonoperatively treated patients) often do not require MRI. Also, diagnosing rotator cuff tears on imaging findings alone is thought to be incomplete, as imaging can often demonstrate structural abnormalities in asymptomatic persons. We excluded patients thought to have a rotator cuff tear on clinical impression, but without such evidence on MRI (n = 36).
Nonoperative Treatment and Surgical Procedures
The recommended nonoperative treatment was physical therapy for 6 to 12 weeks. Physical therapy programs involved rotator cuff strengthening, scapular stabilization exercises, and capsular stretching. The surgical procedure included a rotator cuff repair that was performed by 1 of the study surgeons. Adjuvant procedures such as debridement, biceps tenodesis or tenotomy, acromioclavicular joint resection, or distal clavicular excision were performed if indicated at the time of the surgical procedure. Patients underwent routine postoperative rehabilitation and were typically in a sling for about 3 to 6 weeks after the surgical procedure. Patients in either group could undergo additional interventions such as injections or other oral or topical medications, if indicated. Patients could also cross over from one treatment arm to the other.
Longitudinal Follow-up
Patients were followed at approximately 3, 6, 12, 18, 24, 36, 48, and 60 months after completion of the baseline visit. Follow-up was performed primarily by mail with telephone or email reminders.
Outcomes Analyzed
We analyzed 6 outcome end points for this study: the times to achieve (1) the MCID for SPADI scores, (2) >30% reduction in SPADI scores from baseline, (3) >50% reduction in SPADI scores from baseline, (4) the MCID for ASES scores, (5) >30% reduction in ASES scores from baseline, and (6) >50% reduction in ASES scores from baseline. These reduction thresholds have been previously used in the musculoskeletal literature21. Patients missing baseline SPADI scores were excluded from the SPADI analyses (n = 5) and patients missing baseline ASES scores were excluded from the ASES analyses (n = 2). Patients who had baseline scores that were lower than the MCID in SPADI score (n = 4) and ASES score (n = 5) were excluded from MCID analyses because these patients could not have the opportunity to achieve MCID during follow-up.
Statistical Analysis
We used reconciled double data entry to ensure the highest-quality data entry. For the time-to-event analysis, the actual date that the patient completed the questionnaires was used. If this information was missing (n = 22), we instead used the closest approximation that could be discerned from the data. The intent-to-treat approach was employed for all analyses, such that patients who crossed from one treatment arm to the other (n = 16) were analyzed in their original treatment group. In the surgical treatment group, 4 patients underwent only nonoperative treatment, and 12 patients in the nonoperative treatment group underwent surgical treatment.
Multiple imputation by predictive mean matching was used to impute data for variables with missing values. Because patients were not randomized to treatment, propensity score weighting was used to adjust for inherent differences between the treatment groups because of the lack of randomization in this prospective cohort study. This is a widely used and accepted methodology22-24. Weighting was performed by calculating the inverse probability of treatment weights for the surgical treatment and nonoperative treatment groups25. A standardized mean difference was calculated between the 2 groups before and after propensity score weighting to determine if the surgical treatment and nonoperative treatment groups had similar characteristics after weighting.
The Kaplan-Meier method was used to estimate the time-to-event distributions for our 6 outcome measures. Because the log-rank test has demonstrated low power in the presence of crossing time-to-event distributions apparent in our data, we employed the 2-stage test described by Qiu and Sheng26 to compare the 2 groups. This test compares overall differences in distributions, but it does not directly compare directional differences. Thus, we also compared the time to event at the time of maximum difference between the 2 treatment groups among all possible time points of follow-up27. To control the type-I error rate for multiple testing (e.g., post priori testing), the Bonferroni correction was used and a p value of <0.004 was considered significant. The Bonferroni p value was calculated by dividing 0.05 by the number of unique event times for each outcome. The median time and 95% confidence interval (CI) for each treatment group to achieve the MCID, >30% reduction, and >50% reduction for SPADI and ASES scores were also calculated. Statistical analysis was performed using the R computing environment (R Foundation for Statistical Computing)28.
Results
In the ROW cohort, 96 patients were recommended to undergo nonoperative treatment and 73 patients were recommended to undergo a surgical procedure (Table I). Patients who underwent a surgical procedure were younger (mean age, 58.8 years for the surgical treatment group compared with 64.6 years for the nonoperative treatment group; p < 0.001), had higher baseline median SPADI scores (54 points in the surgical treatment group compared with 40 points in the nonoperative treatment group; p = 0.004), and higher baseline median ASES scores (54 points in the surgical treatment group compared with 49 points in the nonoperative treatment group; p = 0.015). A higher proportion of patients undergoing a surgical procedure had full-thickness tears (79% in the surgical treatment group compared with 56% in the nonoperative treatment group; p = 0.003) and traumatic tears (72% in the surgical treatment group compared with 39% in the nonoperative treatment group; p < 0.001). After propensity score weighting was applied to mitigate imbalances in patient characteristics between the 2 groups, the standardized mean differences between groups decreased. This is the desired outcome when adjusting for differences in patient characteristics in a nonrandomized cohort study. Patients crossed over from the nonoperative treatment arm to a surgical procedure (n = 12) at a median of 5.4 months (range, 2.2 to 14 months).
TABLE I.
Baseline Patient Characteristics of the ROW Cohort Undergoing Nonoperative or Operative Treatment for Rotator Cuff Tears Before and After Propensity Score Weighting (N = 169)
| Before Weighting | After Weighting | |||||
| Nonoperative Treatment | Operative Treatment | Standardized Mean Difference* | Nonoperative Treatment | Operative Treatment | Standardized Mean Difference* | |
| Demographic characteristics | ||||||
| Age† (yr) | 64.62 ± 8.29 | 58.82 ± 8.36 | 0.698 | 61.01 ± 8.41 | 60.79 ± 8.76 | 0.027 |
| Sex‡ | ||||||
| Male | 47 (49.0%) of 96 | 45 (61.6%) of 73 | 0.257 | 17.7 (51.5%) | 17.9 (51.6%) | 0.002 |
| Female | 49 (51.0%) of 96 | 28 (38.4%) of 73 | 0.257 | 16.75 (48.6%) | 16.86 (48.5%) | 0.002 |
| Level of education‡ | ||||||
| College or above | 62 (66.0%) of 94 | 47 (66.2%) of 71 | 0.005 | 23.5 (68.8%) | 23.8 (69.6%) | 0.018 |
| Less than college | 34 (35.4%) of 94 | 24 (33.8%) of 71 | 0.005 | 10.95 (31.8%) | 10.96 (31.5%) | 0.018 |
| Marital status‡ | ||||||
| Married | 68 (73.1%) of 93 | 56 (76.7%) of 73 | 0.083 | 25.7 (75.3%) | 26.3 (75.7%) | 0.010 |
| Single, married, or divorced | 25 (26.9%) of 93 | 17 (23.3%) of 73 | 0.083 | 8.75 (25.4%) | 8.46 (24.3%) | 0.010 |
| Social history‡ | ||||||
| Alcohol use | ||||||
| >1 to 2 times per week | 44 (46.8%) of 94 | 39 (54.9%) of 71 | 0.163 | 16.5 (48.2%) | 16.3 (47.7%) | 0.011 |
| <3 to 4 times per month | 50 (53.2%) of 94 | 32 (45.1%) of 71 | 0.163 | 17.95 (52.1%) | 18.46 (53.1%) | 0.011 |
| Past or current smoker | 52 (55.3%) of 94 | 34 (47.9%) of 71 | 0.149 | 17.4 (50.8%) | 17.7 (51.8%) | 0.020 |
| Comorbidities | ||||||
| FABQ Physical Activity Score† (points) | 15.66 ± 5.72 | 19.21 ± 4.39 | 0.696 | 17.53 ± 4.63 | 17.83 ± 4.65 | 0.065 |
| MHI-5 score† (points) | 80.00 ± 14.74 | 79.91 ± 15.64 | 0.006 | 80.07 ± 14.02 | 80.07 ± 15.48 | <0.001 |
| Presence of >1 comorbidity‡ | 49 (51.0%) of 96 | 30 (41.1%) of 73 | 0.201 | 17.2 (50.0%) | 17.3 (49.8%) | 0.003 |
| Biceps tendinitis‡ | 27 (28.1%) of 96 | 20 (27.4%) of 73 | 0.016 | 9.1 (26.5%) | 9.2 (26.5%) | <0.001 |
| Shoulder characteristics | ||||||
| Dominant shoulder affected‡ | 64 (69.6%) of 92 | 53 (75.7%) of 70 | 0.138 | 23.2 (70.5%) | 24.2 (72.7%) | 0.049 |
| Duration of symptoms† (mo) | 18.93 ± 37.94 | 22.35 ± 40.66 | 0.087 | 19.62 ± 46.59 | 23.99 ± 40.42 | 0.100 |
| Daily shoulder use at work‡ | 22 (23.2%) of 95 | 18 (25.0%) of 72 | 0.043 | 10.0 (29.9%) | 9.1 (26.5%) | 0.077 |
| Traumatic etiology‡ | 28 (39.4%) of 71 | 34 (72.3%) of 47 | 0.702 | 12.3 (47.1%) | 12.0 (56.5%) | 0.188 |
| Patient expectation for less than “great improvement”‡ | 34 (36.2%) of 94 | 4 (5.6%) of 72 | 0.813 | 4.3 (12.7%) | 4.0 (11.8%) | 0.028 |
| Baseline SPADI† (points) | 44.47 ± 21.32 | 54.22 ± 21.35 | 0.457 | 52.19 ± 20.99 | 51.11 ± 21.54 | 0.051 |
| Baseline ASES† (points) | 47.70 ± 18.15 | 54.41 ± 17.87 | 0.373 | 53.79 ± 17.84 | 51.68 ± 18.15 | 0.118 |
| External rotation ratio† | 0.80 ± 0.34 | 0.67 ± 0.45 | 0.333 | 0.78 ± 0.27 | 0.77 ± 0.51 | 0.027 |
| Tear characteristics on MRI | ||||||
| Fatty infiltration‡ | 19 (26.8%) of 71 | 24 (39.3%) of 61 | 0.270 | 7.6 (29.2%) | 9.9 (34.9%) | 0.122 |
| Presence of >1 tendon tear‡ | 24 (30.4%) of 79 | 23 (34.8%) of 66 | 0.095 | 10.3 (36.3%) | 11.2 (36.9%) | 0.012 |
| Full-thickness tear of any tendon‡ | 44 (55.7%) of 79 | 52 (78.8%) of 66 | 0.508 | 17.9 (63.1%) | 20.3 (66.8%) | 0.077 |
| Cross-sectional area of tear† (cm2) | 7.83 ± 14.88 | 13.94 ± 19.65 | 0.351 | 9.99 ± 16.78 | 12.70 ± 20.14 | 0.146 |
| Presence of infraspinatus tear‡ | 22 (27.8%) of 79 | 23 (34.8%) of 66 | 0.151 | 10.0 (35.2%) | 11.0 (36.2%) | 0.022 |
| Boileau stage of tendon retraction‡ | ||||||
| Stage 1 | 61 (77.2%) of 79 | 43 (65.2%) of 66 | 0.269 | 26.45 (76.8%) | 25.86 (74.4%) | 0.023 |
| Stage 2 or more | 18 (22.8%) of 79 | 23 (34.8%) of 66 | 0.269 | 8.0 (28.3%) | 8.9 (29.3%) | 0.023 |
This is the most commonly used statistic to examine the balance of covariate distribution between treatment groups. The value will approach zero as balance improves.
The values are given as the mean and standard deviation.
The values are given as the number of patients, with the percentage in parentheses.
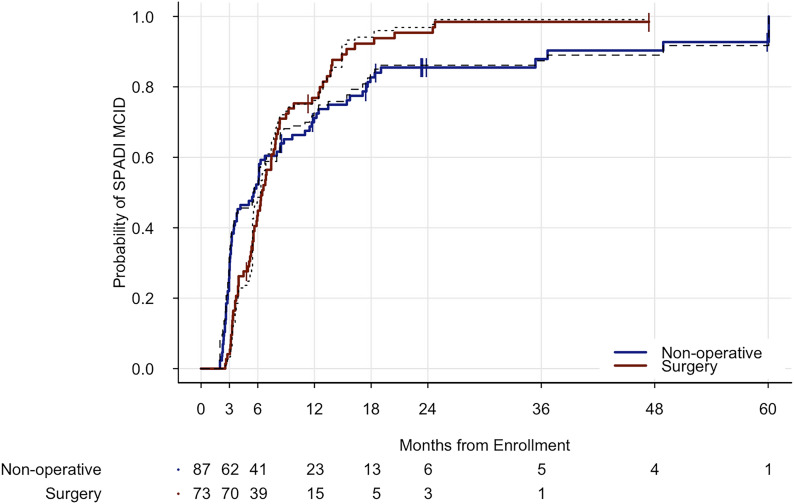
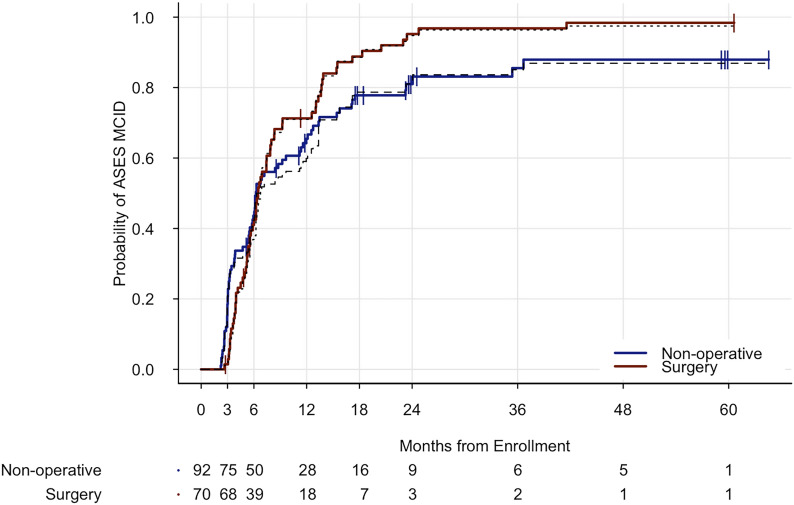
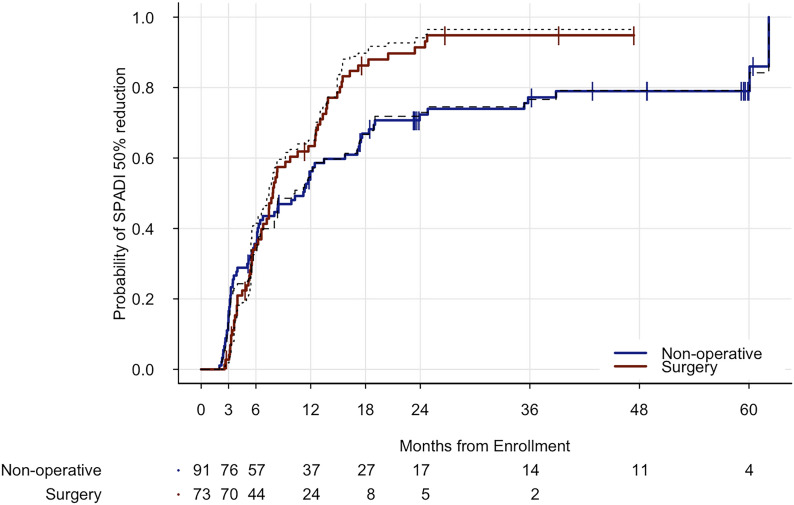
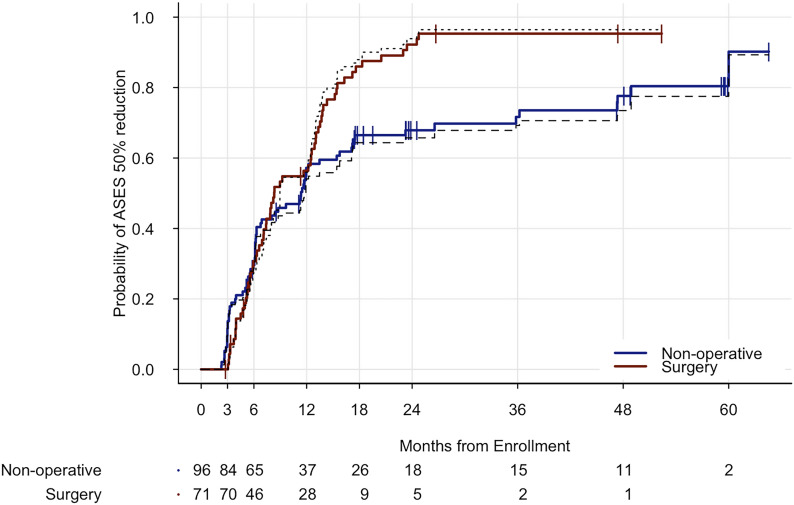
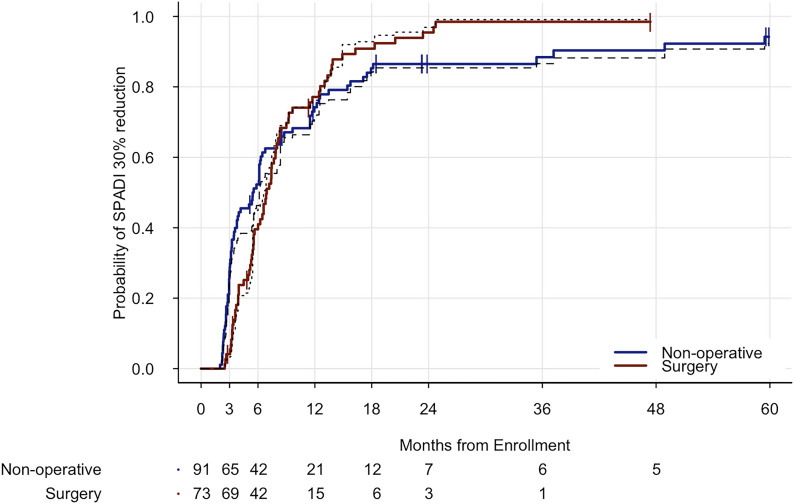
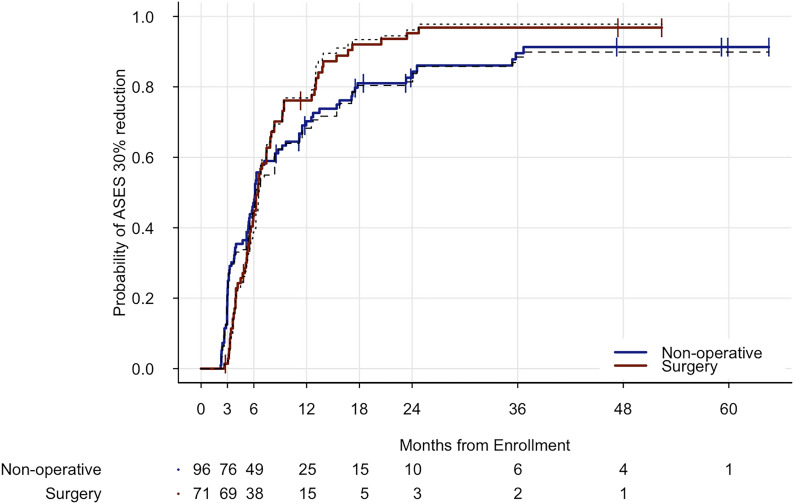
The 2-stage test showed that the difference between the surgical treatment and nonoperative treatment groups reached significance (p < 0.05) for all 6 outcome end points (Table II). When calculating the time points at which the difference between the 2 groups was at a maximum, the nonoperative treatment group had a significantly greater probability than the surgical treatment group to achieve the MCID for the SPADI scores at 3.3 months (0.40 [95% CI, 0.29 to 0.50] compared with 0.06 [95% CI, 0.00 to 0.12]; p = 0.00012) (Fig. 1-A, Table III), but, for the MCID for the ASES scores, the differences between groups were not significant at the Bonferroni-corrected significance level of p < 0.0004 (Fig. 1-B). The surgical treatment group also had a significantly greater probability than the nonoperative treatment group to achieve >50% reduction in SPADI scores at 15.5 months (0.20 [95% CI, 0.12 to 0.29] compared with 0.04 (95% CI, 0.00 to 0.12]; p = 0.00019) (Fig. 2-A) and >50% reduction in ASES scores at 24.7 months (0.96 [95% CI, 0.84 to 0.99] compared with 0.66 [95% CI, 0.53 to 0.75]; p = 0.00003) (Fig. 2-B). The differences between the 2 groups for >30% reduction in SPADI scores (Fig. 3-A) or ASES scores (Fig. 3-B) were also not significant at the Bonferroni-corrected significance level.
Fig. 1-A.
The cumulative incidence curve for achieving the MCID in SPADI scores in the nonoperative treatment group (blue) and the surgical treatment group (red). The dashed lines indicate adjustment after propensity score weighting.
Fig. 1-B.
The cumulative incidence curve for achieving the MCID in ASES scores in the nonoperative treatment group (blue) and the surgical treatment group (red). The dashed lines indicate adjustment after propensity score weighting.
Fig. 2-A.
The cumulative incidence curve for achieving >50% reduction in SPADI scores in the nonoperative treatment group (blue) and the surgical treatment group (red). The dashed lines indicate adjustment after propensity score weighting.
Fig. 2-B.
The cumulative incidence curve for achieving >50% reduction in ASES scores in the nonoperative treatment group (blue) and the surgical treatment group (red). The dashed lines indicate adjustment after propensity score weighting.
Fig. 3-A.
The cumulative incidence curve for achieving >30% reduction in SPADI scores in the nonoperative treatment group (blue) and the surgical treatment group (red). The dashed lines indicate adjustment after propensity score weighting.
Fig. 3-B.
The cumulative incidence curve for achieving >30% reduction in ASES scores in the nonoperative treatment group (blue) and the surgical treatment group (red). The dashed lines indicate adjustment after propensity score weighting.
TABLE II.
Two-Stage Test for Comparison of the Time-to-Event Curves Between the Nonoperative Treatment Group and the Surgical Treatment Group*
| Outcome | First-Stage Test P Value† | Overall P Value |
| SPADI scores | ||
| MCID | 0.53 | 0.025 |
| >30% reduction | 0.91 | 0.025 |
| >50% reduction | 0.024 | 0.024 |
| ASES scores | ||
| MCID | 0.19 | 0.025 |
| >30% reduction | 0.35 | 0.025 |
| >50% reduction | 0.020 | 0.020 |
Results of the 2-stage procedure for each of the 6 outcomes.
This is the p value from the basic log-rank test. When this p value was <0.025 (e.g., >50% reductions for SPADI and ASES scores), it could be concluded that the 2 curves were different and the second stage was not performed. However, for the remainder of the outcomes, the second-stage test was conducted. All 6 outcomes were significant according to the 2-stage procedure.
TABLE III.
Time Points of Maximum Difference in the Time-to-Event Curves Between the Nonoperative Treatment Group and the Surgical Treatment Group*
| Outcome | Significance Level | P Value | Months |
| SPADI scores | |||
| MCID | 0.00043 | 0.00012 | 3.25† |
| >30% reduction | 0.00045 | 0.00074 | 3.25 |
| >50% reduction | 0.00044 | 0.00019 | 15.49† |
| ASES scores | |||
| MCID | 0.00046 | 0.00485 | 3.25 |
| >30% reduction | 0.00047 | 0.00332 | 3.25 |
| >50% reduction | 0.00046 | 0.00003 | 24.74† |
Time-to-event curves were adjusted by propensity scoring. To adjust for multiple comparisons, the significance level was set at 0.05 divided by the number of unique event times. The p values for >30% reductions for SPADI and ASES scores and the MCID for the ASES score did not reach the level of significance.
Significantly different according to this method.
Discussion
We performed a longitudinal cohort study of patients with rotator cuff tears undergoing nonoperative or surgical treatment and followed patients for up to approximately 5 years. Overall, there was a significant difference between the operative and nonoperative treatment groups for all of the outcomes (MCID and >30% and >50% reduction for SPADI and ASES scores). At 3.3 months, the nonoperative treatment group had significantly better outcomes compared with the surgical treatment group for the MCID for the SPADI scores. However, at 15.5 months (for >50% reduction in SPADI scores) and at 24.7 months (for >50% reduction in ASES scores), the surgical treatment group had significantly better outcomes compared with the nonoperative treatment group.
Prior literature has assessed data on operative and nonoperative treatment outcomes, but data on the difference in recovery times after surgical and nonoperative treatments have not been presented10,29-32. Our previously published study compared outcomes of propensity score-weighted surgical and nonoperative treatment groups with rotator cuff tears. However, the previous study did not address comparative time to outcomes (i.e., time to event). Also, the study population was different (n = 127) and patients were not followed past 18 months. In that prior study, a greater percentage of patients in the surgical treatment group showed >30% and >50% reduction compared with the nonoperative treatment group. Also, a recent retrospective study by Ramme et al. found that, in a propensity score-matched cohort of patients with only full-thickness tears, a surgical treatment group had improved outcomes at 2.35 months compared with a nonoperative treatment group at 2.30 months33. In comparison, our cohort included both full-thickness and partial tears.
However, in this study, the nonoperative treatment group performed better initially compared the surgical treatment group. Most patients in the surgical treatment group underwent a surgical procedure in the first few months after recruitment and hence were still recovering from postoperative pain. After the postoperative recovery and rehabilitation phase, patients in the surgical treatment group started to show more improved outcomes in shoulder pain and function compared with the nonoperative treatment group.
It is also interesting that patients in both the nonoperative and surgical treatments had a high likelihood of improvement regardless of their treatment arm. There was >80% probability of achieving the desired outcome (MCID, >30% reduction, or >50% reduction) by the end of the study period at 60 months in both treatment groups and both outcome measures. This finding is consistent with several studies suggesting good outcomes for both nonoperative and surgical treatments for rotator cuff tears34-39.
The maximal differences in the time to event between the surgical treatment group and the nonoperative treatment group occurred at 3.3 months for the MCID for SPADI scores, at 15.5 months for >50% reduction in SPADI scores, and at 24.7 months for >50% reduction in ASES scores. We can infer from this that our patients, on average, required a longer duration to maximize improvement in the surgical treatment arm compared with the nonoperative treatment arm. Also, a significantly higher proportion of patients are likely to achieve a greater magnitude of improvement (as defined by >50% reduction) in the surgical treatment group compared with the nonoperative treatment group during the longer term. Based on these findings, patients with an expectation for a greater magnitude of improvement from baseline and those who are willing to wait longer for the improved outcomes may be counselled toward a surgical procedure. Conversely, a nonoperative treatment plan may be more suitable for patients who desire earlier improvement but are also accepting of smaller magnitude of improvement. Patient expectations from treatment are associated with better outcomes40. Data from our study can be used to educate patients about expectations for operative and nonoperative treatments and thus be directly applicable to patient care and education.
The limitations of our study included a cohort design leading to inherent bias in patients undergoing operative treatment compared with those undergoing nonoperative treatment. We adjusted for this issue using propensity scores. Although we collected information on known factors that may influence treatment selection and outcomes, it is possible that unknown confounders were not included in our analysis. A limitation of our cohort study was patient crossover between treatment arms. Although we had a relatively low rate of crossover, this could bias results. The inclusion of patients who were not clinically indicated for an MRI scan (n = 24) was also a limitation. Another limitation was that outcome scores captured at the date of questionnaire completion may have reflected an earlier time point during the specific follow-up interval. However, this is the standard methodology used in time-to-event analysis.
In conclusion, in this prospective cohort study of patients with rotator cuff tears, there was a significant difference between the operative and nonoperative treatment groups with respect to shoulder pain and function. Patients undergoing nonoperative treatment had improved outcomes in the initial follow-up period compared with patients undergoing a surgical procedure, but this trend reversed in the longer term. These data can be used to inform expectations for nonoperative and operative treatments for rotator cuff tears. Patients with an expectation for a greater magnitude of improvement from baseline and those who are willing to wait longer for the improved outcomes may be counseled toward a surgical procedure. A nonoperative treatment plan may be more suitable for patients who desire earlier improvement but are also accepting of a smaller magnitude of improvement.
Appendix
Supporting material provided by the authors is posted with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJS/F860
Footnotes
Investigation performed at Vanderbilt University Medical Center, Nashville, Tennessee
A commentary by Sarav S. Shah, MD, is linked to the online version of this article at jbjs.org.
Disclosure: This work was supported by grants from the National Institutes of Health (NIH) (K23AR059199 and U34AR069201). On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/F859).
References
- 1.Luime JJ, Koes BW, Hendriksen IJM, Burdorf A, Verhagen AP, Miedema HS, Verhaar JA. Prevalence and incidence of shoulder pain in the general population; a systematic review. Scand J Rheumatol. 2004;33(2):73-81. [DOI] [PubMed] [Google Scholar]
- 2.Meislin RJ, Sperling JW, Stitik TP. Persistent shoulder pain: epidemiology, pathophysiology, and diagnosis. Am J Orthop (Belle Mead NJ). 2005. December;34(12)(Suppl):5-9. [PubMed] [Google Scholar]
- 3.Teunis T, Lubberts B, Reilly BT, Ring D. A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg. 2014. December;23(12):1913-21. [DOI] [PubMed] [Google Scholar]
- 4.Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL. National trends in rotator cuff repair. J Bone Joint Surg Am. 2012. February 1;94(3):227-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jain NB, Higgins LD, Losina E, Collins J, Blazar PE, Katz JN. Epidemiology of musculoskeletal upper extremity ambulatory surgery in the United States. BMC Musculoskelet Disord. 2014. January 8;15:4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Minns Lowe CJ, Moser J, Barker K. Living with a symptomatic rotator cuff tear ‘bad days, bad nights’: a qualitative study. BMC Musculoskelet Disord. 2014. July 9;15:228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Littlewood C, Rangan A, Beard DJ, Wade J, Cookson T, Foster NE. The enigma of rotator cuff tears and the case for uncertainty. Br J Sports Med. 2018. October;52(19):1222 Epub 2018 Apr 12. [DOI] [PubMed] [Google Scholar]
- 8.Jain NB, Ayers GD, Fan R, Kuhn JE, Warner JJP, Baumgarten KM, Matzkin E, Higgins LD. Comparative effectiveness of operative versus nonoperative treatment for rotator cuff tears: a propensity score analysis from the ROW cohort. Am J Sports Med. 2019. November;47(13):3065-72. Epub 2019 Sep 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jain NB, Luz J, Higgins LD, Dong Y, Warner JJ, Matzkin E, Katz JN. The diagnostic accuracy of special tests for rotator cuff tear: the ROW cohort study. Am J Phys Med Rehabil. 2017. March;96(3):176-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jain NB, Ayers GD, Fan R, Kuhn JE, Baumgarten K, Matzkin E, Higgins LD. Predictors of pain and functional outcomes after the nonoperative treatment of rotator cuff tears. Orthop J Sports Med. 2018. August 3;6(8):2325967118788531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dickinson RN, Ayers GD, Archer KR, Fan R, Page C, Higgins LD, Kuhn JE, Baumgarten KM, Matzkin E, Jain NB. Physical therapy versus natural history in outcomes of rotator cuff tears: the Rotator Cuff Outcomes Workgroup (ROW) cohort study. J Shoulder Elbow Surg. 2019. May;28(5):833-8. Epub 2018 Dec 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of magnetic resonance imaging assessment of rotator cuff: the ROW study. PM R. 2015. March;7(3):245-54.e3; quiz 254. Epub 2014 Aug 30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jain NB, Ayers GD, Fan R, Kuhn JE, Baumgarten KM, Matzkin E, Higgins LD. Predictors of pain and functional outcomes after operative treatment for rotator cuff tears. J Shoulder Elbow Surg. 2018. August;27(8):1393-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Waddell G, Newton M, Henderson I, Somerville D, Main CJ. A Fear-Avoidance Beliefs Questionnaire (FABQ) and the role of fear-avoidance beliefs in chronic low back pain and disability. Pain. 1993. February;52(2):157-68. [DOI] [PubMed] [Google Scholar]
- 15.Berwick DM, Murphy JM, Goldman PA, Ware JE, Jr, Barsky AJ, Weinstein MC. Performance of a five-item mental health screening test. Med Care. 1991. February;29(2):169-76. [DOI] [PubMed] [Google Scholar]
- 16.Roach KE, Budiman-Mak E, Songsiridej N, Lertratanakul Y. Development of a shoulder pain and disability index. Arthritis Care Res. 1991. December;4(4):143-9. [PubMed] [Google Scholar]
- 17.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA, Zuckerman JD. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994. November;3(6):347-52. Epub 2009 Feb 13. [DOI] [PubMed] [Google Scholar]
- 18.Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin Trials. 1989. December;10(4):407-15. [DOI] [PubMed] [Google Scholar]
- 19.Williams JW, Jr, Holleman DR, Jr, Simel DL. Measuring shoulder function with the Shoulder Pain and Disability Index. J Rheumatol. 1995. April;22(4):727-32. [PubMed] [Google Scholar]
- 20.Werner BC, Chang B, Nguyen JT, Dines DM, Gulotta LV. What change in American Shoulder and Elbow Surgeons Score represents a clinically important change after shoulder arthroplasty? Clin Orthop Relat Res. 2016. December;474(12):2672-81. Epub 2016 Jul 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Friedly JL, Comstock BA, Turner JA, Heagerty PJ, Deyo RA, Sullivan SD, Bauer Z, Bresnahan BW, Avins AL, Nedeljkovic SS, Nerenz DR, Standaert C, Kessler L, Akuthota V, Annaswamy T, Chen A, Diehn F, Firtch W, Gerges FJ, Gilligan C, Goldberg H, Kennedy DJ, Mandel S, Tyburski M, Sanders W, Sibell D, Smuck M, Wasan A, Won L, Jarvik JG. A randomized trial of epidural glucocorticoid injections for spinal stenosis. N Engl J Med. 2014. July 3;371(1):11-21. [DOI] [PubMed] [Google Scholar]
- 22.Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011. May;46(3):399-424. Epub 2011 Jun 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li L, Greene T. A weighting analogue to pair matching in propensity score analysis. Int J Biostat. 2013. July 31;9(2):215-34. [DOI] [PubMed] [Google Scholar]
- 24.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983. April;70(1):41-55. [Google Scholar]
- 25.Cole SR, Hernán MA. Adjusted survival curves with inverse probability weights. Comput Methods Programs Biomed. 2004. July;75(1):45-9. [DOI] [PubMed] [Google Scholar]
- 26.Qiu P, Sheng J. A two-stage procedure for comparing hazard rate functions. J R Stat Soc Series B Stat Methodol. 2008. February;70(1):191-208. [Google Scholar]
- 27.Klein JP, Logan B, Harhoff M, Andersen PK. Analyzing survival curves at a fixed point in time. Stat Med. 2007. October 30;26(24):4505-19. [DOI] [PubMed] [Google Scholar]
- 28.R Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2013. [Google Scholar]
- 29.Kukkonen J, Joukainen A, Lehtinen J, Mattila KT, Tuominen EK, Kauko T, Äärimaa V. Treatment of nontraumatic rotator cuff tears: a randomized controlled trial with two years of clinical and imaging follow-up. J Bone Joint Surg Am. 2015. November 4;97(21):1729-37. [DOI] [PubMed] [Google Scholar]
- 30.Moosmayer S, Lund G, Seljom U, Svege I, Hennig T, Tariq R, Smith HJ. Comparison between surgery and physiotherapy in the treatment of small and medium-sized tears of the rotator cuff: a randomised controlled study of 103 patients with one-year follow-up. J Bone Joint Surg Br. 2010. January;92(1):83-91. [DOI] [PubMed] [Google Scholar]
- 31.Lambers Heerspink FO, van Raay JJAM, Koorevaar RCT, van Eerden PJ, Westerbeek RE, van ’t Riet E, van den Akker-Scheek I, Diercks RL. Comparing surgical repair with conservative treatment for degenerative rotator cuff tears: a randomized controlled trial. J Shoulder Elbow Surg. 2015. August;24(8):1274-81. [DOI] [PubMed] [Google Scholar]
- 32.Yamada N, Hamada K, Nakajima T, Kobayashi K, Fukuda H. Comparison of conservative and operative treatments of massive rotator cuff tears. Tokai J Exp Clin Med. 2000. December;25(4-6):151-63. [PubMed] [Google Scholar]
- 33.Ramme AJ, Robbins CB, Patel KA, Carpenter JE, Bedi A, Gagnier JJ, Miller BS. Surgical versus nonsurgical management of rotator cuff tears: a matched-pair analysis. J Bone Joint Surg Am. 2019. October 2;101(19):1775-82. [DOI] [PubMed] [Google Scholar]
- 34.Bokor DJ, Hawkins RJ, Huckell GH, Angelo RL, Schickendantz MS. Results of nonoperative management of full-thickness tears of the rotator cuff. Clin Orthop Relat Res. 1993. September;294:103-10. [PubMed] [Google Scholar]
- 35.Fucentese SF, von Roll AL, Pfirrmann CWA, Gerber C, Jost B. Evolution of nonoperatively treated symptomatic isolated full-thickness supraspinatus tears. J Bone Joint Surg Am. 2012. May 2;94(9):801-8. [DOI] [PubMed] [Google Scholar]
- 36.Itoi E, Tabata S. Conservative treatment of rotator cuff tears. Clin Orthop Relat Res. 1992. February;275:165-73. [PubMed] [Google Scholar]
- 37.Tashjian RZ. Epidemiology, natural history, and indications for treatment of rotator cuff tears. Clin Sports Med. 2012. October;31(4):589-604. Epub 2012 Aug 30. [DOI] [PubMed] [Google Scholar]
- 38.Kuhn JE, Dunn WR, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW; MOON Shoulder Group. Effectiveness of physical therapy in treating atraumatic full-thickness rotator cuff tears: a multicenter prospective cohort study. J Shoulder Elbow Surg. 2013. October;22(10):1371-9. Epub 2013 Mar 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zuke WA, Leroux TS, Gregory BP, Black A, Forsythe B, Romeo AA, Verma NN. Establishing maximal medical improvement after arthroscopic rotator cuff repair. Am J Sports Med. 2018. March;46(4):1000-7. Epub 2017 Jun 26. [DOI] [PubMed] [Google Scholar]
- 40.Dunn WR, Kuhn JE, Sanders R, An Q, Baumgarten KM, Bishop JY, Brophy RH, Carey JL, Harrell F, Holloway BG, Jones GL, Ma CB, Marx RG, McCarty EC, Poddar SK, Smith MV, Spencer EE, Vidal AF, Wolf BR, Wright RW; MOON Shoulder Group. 2013 Neer Award: predictors of failure of nonoperative treatment of chronic, symptomatic, full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2016. August;25(8):1303-11. [DOI] [PubMed] [Google Scholar]