Abstract
Background:
Several classification systems exist for sacral fractures; however, these systems are primarily descriptive, are not uniformly used, have not been validated, and have not been associated with a treatment algorithm or prognosis. The goal of the present study was to demonstrate the reliability of the AOSpine Sacral Classification System among a group of international spine and trauma surgeons.
Methods:
A total of 38 sacral fractures were reviewed independently by 18 surgeons selected from an expert panel of AOSpine and AOTrauma members. Each case was graded by each surgeon on 2 separate occasions, 4 weeks apart. Intrarater reproducibility and interrater agreement were analyzed with use of the kappa statistic (κ) for fracture severity (i.e., A, B, and C) and fracture subtype (e.g., A1, A2, and A3).
Results:
Seventeen reviewers were included in the final analysis, and a total of 1,292 assessments were performed (646 assessments performed twice). Overall intrarater reproducibility was excellent (κ = 0.83) for fracture severity and substantial (κ = 0.71) for all fracture subtypes. When comparing fracture severity, overall interrater agreement was substantial (κ = 0.75), with the highest agreement for type-A fractures (κ = 0.95) and the lowest for type-C fractures (κ = 0.70). Overall interrater agreement was moderate (κ = 0.58) when comparing fracture subtype, with the highest agreement seen for A2 subtypes (κ = 0.81) and the lowest for A1 subtypes (κ = 0.20).
Conclusions:
To our knowledge, the present study is the first to describe the reliability of the AOSpine Sacral Classification System among a worldwide group of expert spine and trauma surgeons, with substantial to excellent intrarater reproducibility and moderate to substantial interrater agreement for the majority of fracture subtypes. These results suggest that this classification system can be reliably applied to sacral injuries, providing an important step toward standardization of treatment.
Sacral fractures are commonly seen in the context of high-energy trauma with associated pelvic-ring injuries. The predominant mechanisms of injury are motor vehicle collisions, motor vehicles striking pedestrians, motorcycle accidents, falls from a height, or crush injuries1. Up to 25% of sacral fractures are associated with a neurologic injury because of the close proximity of the lumbosacral plexus1. Because of the complex nature of these injuries, they are often treated by a multidisciplinary team that may consist of spine surgeons, orthopaedic trauma surgeons, and/or general trauma surgeons. A unifying fracture classification system that facilitates communication between physicians and guides treatment is therefore essential to the management of these complex injuries.
Historically, sacral fracture classifications have primarily been incorporated into the orthopaedic trauma classifications for pelvic-ring injuries. Isler and Ganz described a sacral fracture classification system that focused on lumbosacral instability, based primarily on morphological characteristics pertaining to the L5-S1 facet joint and secondarily on resulting pathomechanics2. Several classification systems have described sacral fractures primarily on the basis of fracture morphology3-8. The system described by Denis et al. classifies fractures on the basis of the location relative to the foramen and in terms of progressively higher risk of neurological injury, with zone-I fractures being lateral to the foramen, zone-II fractures going through the foramen but remaining lateral to the spinal canal, and zone-III fractures extending medial to the foramen into the spinal canal3. Roy-Camille et al. described a morphological classification for transverse sacral fractures, postulating that the fracture pattern was dependent on the presence of extension or flexion of the lumbar spine at the time of injury4. In addition, a descriptive system combining vertical and horizontal patterns has been proposed to classify fractures morphologically (H-type, U-type, T-type, and lambda-type)8. Although these systems are individually effective in describing specific features of sacral fractures, they are primarily descriptive, they are not uniformly used, and none are sufficiently comprehensive to account for the full spectrum of sacral fractures; furthermore, none of the aforementioned classifications have been rigorously validated, nor have they been associated with a treatment algorithm or prognosis.
The current AOSpine Trauma classification was developed by the AOSpine Trauma Knowledge Forum to create a comprehensive and easy-to-use fracture classification system for surgeons. Initially developed to classify thoracolumbar spine fractures, it has since expanded to classify subaxial cervical spine fractures9,10. Both of these classification systems have been validated through an international group of spine surgeons noted to be clinical experts in the treatment of these fractures11,12. Similarly to the previous 2 systems, the specific aims of the present study were to (1) demonstrate the reliability of the AOSpine Sacral Classification System among a group of international spine and orthopaedic trauma surgeons and (2) demonstrate which sacral fracture patterns may be difficult to classify reliably, identifying areas for improvement before treatment protocols can be designated.
Materials and Methods
Development of Classification System
The methodology behind the creation of the AOSpine classification has been described in detail in the publication of the AOSpine Thoracolumbar Spine Classification System12. In brief, multiple face-to-face meetings of both AOSpine surgeons and AOTrauma orthopaedic surgeons were held, and a preliminary sacral classification was developed. Once the preliminary system was completed, a survey was sent to all members of AOSpine and AOTrauma seeking input on the classification. The results of the initial survey were published by Schroeder et al. and showed that despite some variability by region, experience, or specialty, the majority of responses were consistent13.
Validation Process
A total of 18 reviewers from high-volume trauma centers were chosen from AOSpine (14 surgeons) and AOTrauma (4 surgeons) to describe the reliability of this classification. All of the selected cases included high-energy sacral fractures with different morphological subtypes. A total of 38 cases were selected, and 3 experienced surgeons developed the gold-standard master key for each case by consensus. All cases were reviewed independently by 18 different individual surgeons with use of computed tomography on 2 separate occasions, 4 weeks apart. To ensure that the reviewers had an understanding of the classification, they were initially instructed to review a video and written tutorial describing the classification and were then asked to classify 10 fractures; the reviewers were required to successfully classify 8 of 10 fractures prior to beginning the validation process.
Statistical Analysis
The kappa statistic (κ), as proposed by Fleiss, was calculated to assess the reliability of the classification system among different observers (interrater agreement) and the reproducibility for the same observer on separate occasions (intrarater reproducibility)14. The Fleiss kappa statistic measures the agreement of multiple raters who rate multiple subjects, with the rating based on multiple categories. The coefficients were interpreted with use of the Landis and Koch grading system, which defines κ ≤ 0.2 as slight reliability (agreement/reproducibility), 0.2 < κ ≤ 0.4 as fair reliability, 0.4 < κ ≤ 0.6 as moderate reliability, 0.6 < κ ≤ 0.8 as substantial reliability, and κ > 0.8 as excellent reliability15. Interrater agreement was calculated for the most severe injury type (i.e., A, B, or C) as well as subtype (e.g., A1, A2, or A3). Intrarater reproducibility was calculated for each case by assessing for the most severe injury type as well as for the subtype.
Overview of Classification System
In short, the sacral classification consists of a hierarchical system divided into 3 main types based on morphological criteria: type-A (lower sacrococcygeal) fractures, type-B (posterior pelvic) fractures, and type-C (spinopelvic) fractures. Each type is further subdivided into 3 or 4 subtypes based on severity grade. Type-A fractures (Figs. 1, 2, and 3) are injuries to the lower sacrococcygeal spine that occur below the level of the sacroiliac joint. Because type-A fractures do not involve the weight-bearing axis or the posterior pelvic ring, they have no effect on posterior-pelvic or spinopelvic stability. Type-B fractures (Figs. 4, 5, and 6) are unilateral vertical sacral fractures in which the ipsilateral superior S1 facet is continuous with the medial portion of the sacrum, therefore maintaining spinopelvic stability while posterior pelvic stability may be compromised. Type-C fractures (Figs. 7 through 10) describe injuries that result in spinopelvic instability and are divided into 4 subtypes. Case-specific modifiers (M1 through M4) include presence of substantial soft-tissue injury, metabolic bone disease, anterior pelvic-ring injury, and sacroiliac joint injury. Neurologic modifiers (N0 through N3) designate intact neurologic status, transient neurologic deficit, nerve-root injury, and cauda equina injury. Neither case-specific modifiers nor neurologic modifiers were included in the present study because no clinical information was provided.
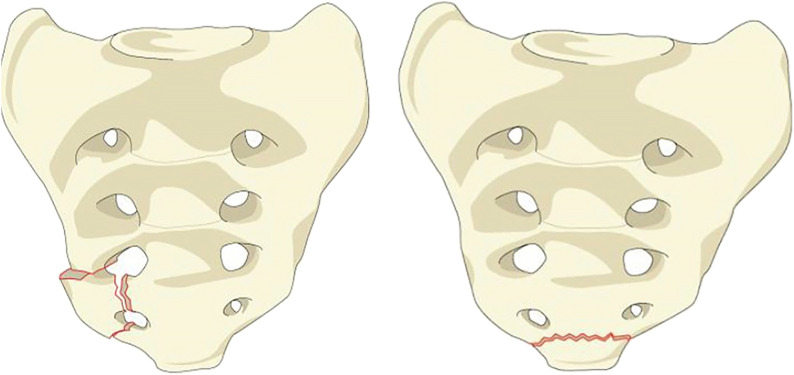
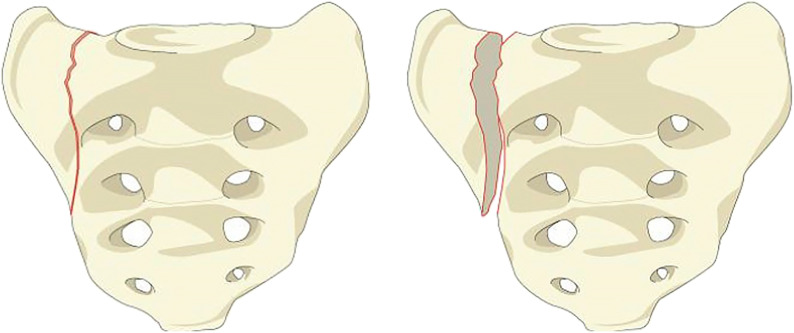
Fig. 1.
Sacral A1 fracture. A1 fractures describe coccygeal or ligamentous avulsion injuries.
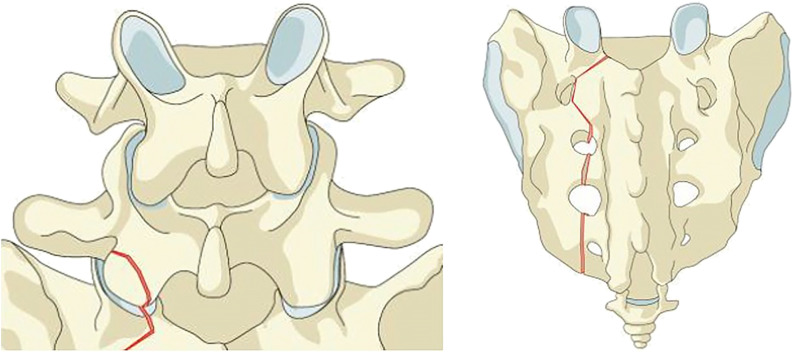
Fig. 2.
Sacral A2 fracture. Sagittal and coronal views of A2 fractures showing variations of a nondisplaced fracture line below the level of the sacroiliac joint.
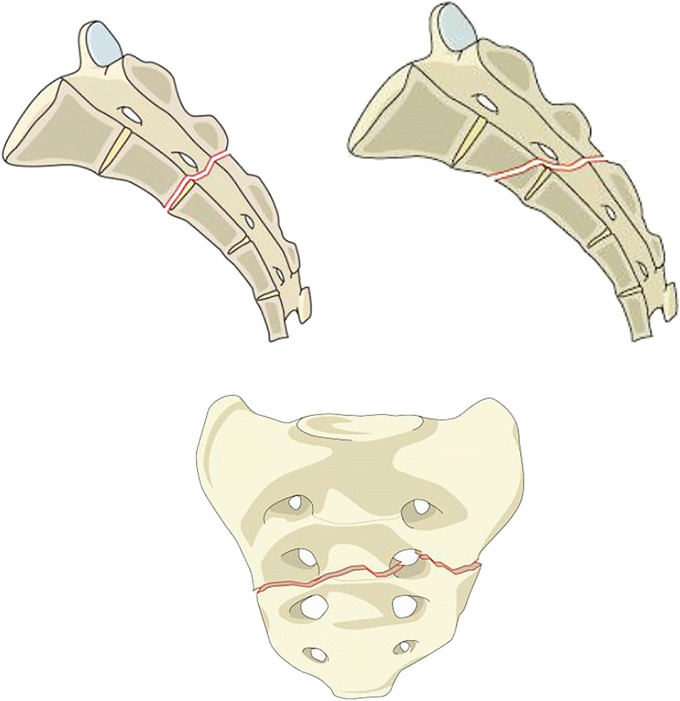
Fig. 3.
Sacral A3 fracture. A3 fractures are displaced transverse fractures below the level of the sacroiliac joint.
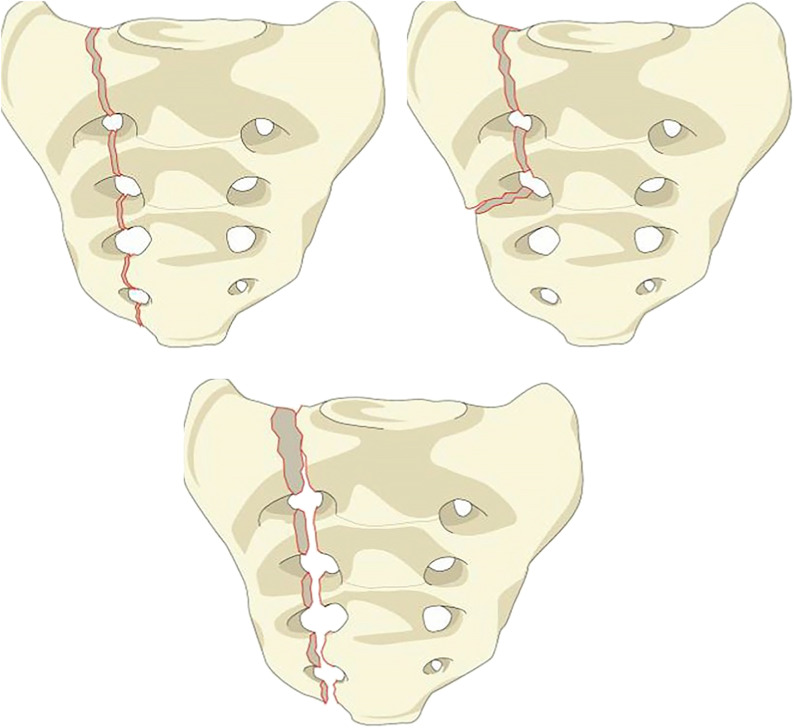
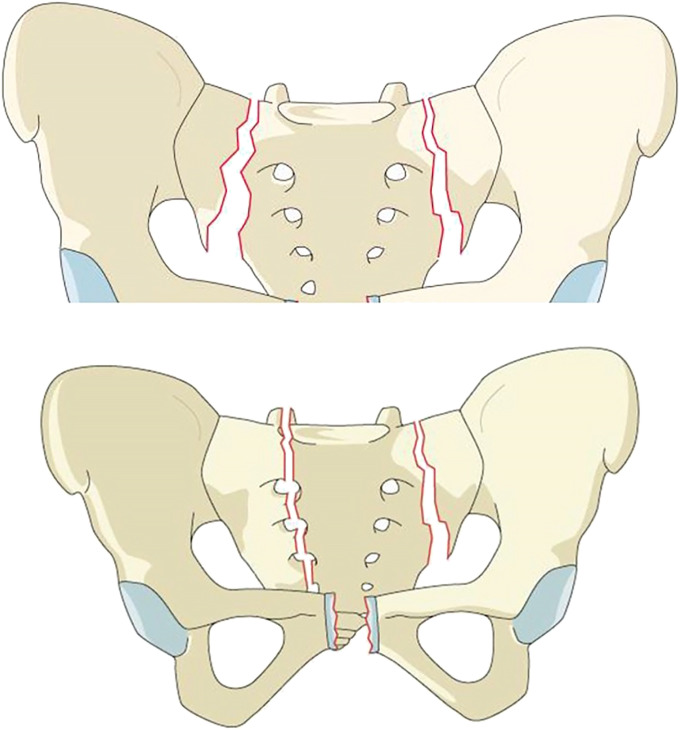
Fig. 4.
Sacral B1 fracture. Coronal representation of a B1 fracture showing a central fracture line that involves the spinal canal.
Fig. 5.
Sacral B2 fracture. B2 fractures are transalar fractures that do not involve the foramina or the spinal canal.
Fig. 6.
Sacral B3 fracture. B3 fractures describe transforaminal fractures that do not involve the spinal canal.
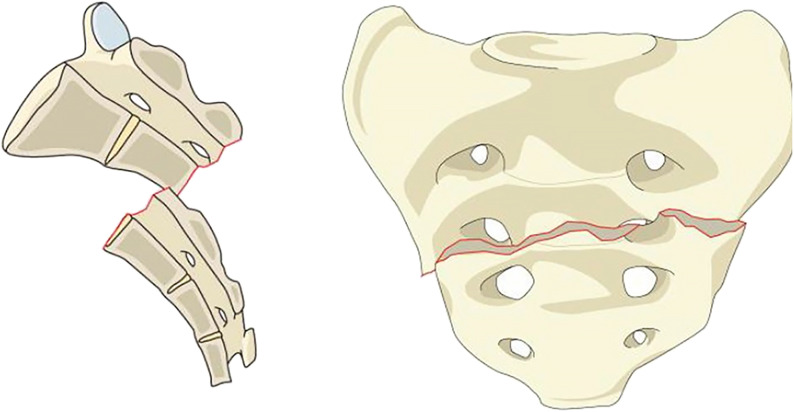
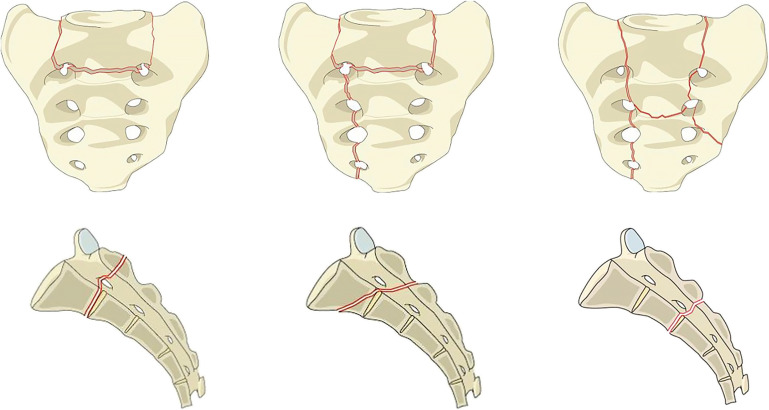
Fig. 7.
Sacral C0 fracture. Coronal and sagittal representations of type C0 fractures, i.e., nondisplaced sacral U-type variant fractures.
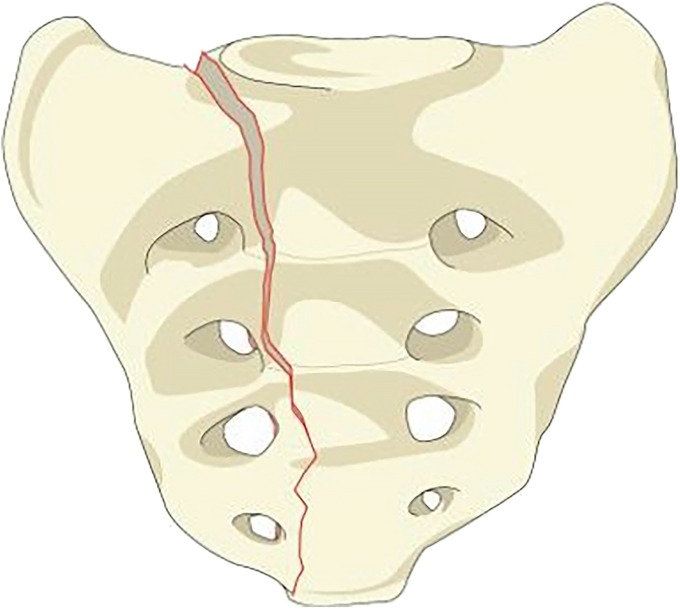
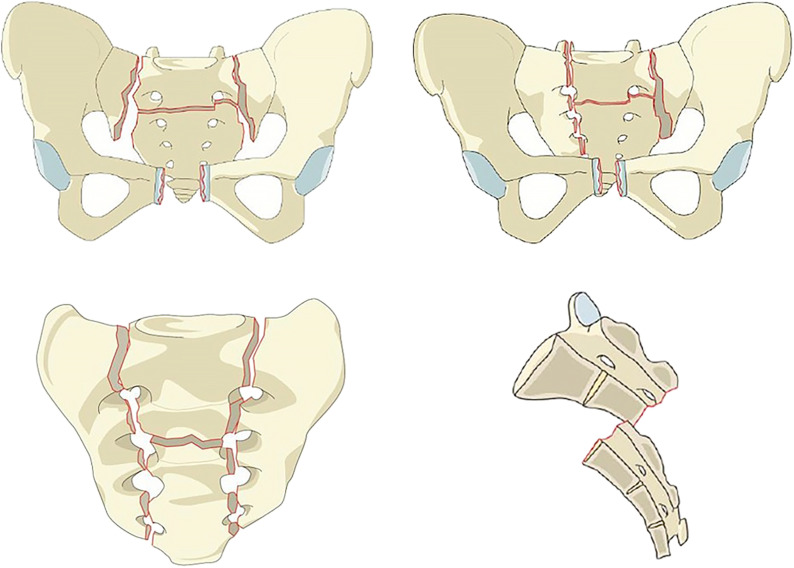
Fig. 10.
Sacral C3 fracture. C3 fractures are displaced sacral U-type fractures.
Fig. 8.
Sacral C1 fracture. A vertical fracture line medial to the ipsilateral S1 facet indicates spinopelvic instability and is designated as a C1 fracture.
Fig. 9.
Sacral C2 fracture. C2 fractures indicate bilateral vertical fractures without a transverse component.
Results
Out of the 18 reviewers, 1 reviewer did not complete the first and second assessments and therefore was excluded from the final analysis. All 10 subtypes of fractures were reported in this classification system (A1 through C3). A total of 1,292 assessments were performed (646 assessments performed twice) (Table I).
TABLE I.
Injury Patterns
| Sacral Classification | N |
| A1 | 27 |
| A2 | 111 |
| A3 | 66 |
| B1 | 50 |
| B2 | 367 |
| B3 | 199 |
| C0 | 81 |
| C1 | 93 |
| C2 | 64 |
| C3 | 218 |
| Missing | 16 |
Interrater Agreement
Overall agreement was moderate, with a combined kappa statistic for the sacral classification of 0.58 (Table II). The lowest level of agreement was observed in fracture subtype A1 (κ = 0.20), whereas the highest agreement was observed in fracture subtype A2 (κ = 0.81). In addition, A2, A3 (κ = 0.78), C3 (κ = 0.73), B1 (κ = 0.68), and B2 (κ = 0.62) fractures all had a level of agreement above the overall agreement (κ = 0.58). There were a total of 8 cases that had unanimous agreement in the first assessment and 5 cases that had unanimous agreement in the second assessment, with only 2 of the cases achieving unanimous agreement in both assessments.
TABLE II.
Interrater Agreement for Sacral Classification Fracture Subtypes
| Fracture Subtype | Kappa |
| A1 | 0.20 |
| A2 | 0.81 |
| A3 | 0.78 |
| B1 | 0.68 |
| B2 | 0.62 |
| B3 | 0.45 |
| C0 | 0.35 |
| C1 | 0.29 |
| C2 | 0.37 |
| C3 | 0.73 |
| Combined | 0.58 |
When comparing interrater agreement between levels of fracture severity (i.e., A, B, or C), the overall agreement was substantial (κ = 0.75) (Table III). The highest interrater agreement was observed in fracture severity type A (κ = 0.95). Severity types B (κ = 0.72) and C (κ = 0.70) showed similar rates of interrater agreement.
TABLE III.
Interrater Agreement of Sacral Classification Severity Category
| Fracture Severity | Kappa |
| A | 0.95 |
| B | 0.72 |
| C | 0.70 |
| Combined | 0.75 |
Intrarater Reproducibility
Overall, intrarater reproducibility was substantial when assessing all fracture subtypes (κ = 0.71) and excellent when assessing fracture severity category (κ = 0.83) (Table IV). Among all reviewers, all but 2 had a substantial or higher reproducibility (κ > 0.6) between the 2 assessment sessions for fracture subtype. Four reviewers had excellent reproducibility results (κ > 0.8). When assessing fracture severity, all but 1 reviewer had substantial or higher reproducibility (κ > 0.6) and 9 reviewers had excellent reproducibility (κ > 0.8).
TABLE IV.
Intrarater Reproducibility for Each Fracture Subtype and Fracture Severity Category
| Reviewer | Fracture Subtype | Fracture Severity |
| 1 | 0.52 | 0.83 |
| 2 | 0.69 | 0.91 |
| 3 | 0.84 | 0.96 |
| 4 | 0.87 | 0.95 |
| 5 | 0.64 | 0.81 |
| 6 | 0.90 | 1.00 |
| 7 | 0.90 | 0.95 |
| 8 | 0.72 | 0.87 |
| 9 | 0.61 | 0.78 |
| 10 | 0.62 | 0.77 |
| 11 | 0.56 | 0.78 |
| 12 | 0.68 | 0.58 |
| 13 | 0.68 | 0.76 |
| 14 | 0.71 | 0.75 |
| 15 | 0.78 | 0.92 |
| 16 | 0.68 | 0.78 |
| 17 | 0.65 | 0.78 |
| Average | 0.71 | 0.83 |
Discussion
Sacral fractures are relatively uncommon, with heterogeneous anatomic characteristics and clinical presentation; therefore, current treatments are varied and nonstandardized. Previous attempts at developing classification systems have yielded largely descriptive systems that focused separately on specific components of sacral fractures (location of fracture, transverse fracture displacement and angulation, L5-S1 facet involvement, etc.). None of these classifications have been validated, and none have integrated the various components of sacral fracture morphology into a comprehensive treatment and prognosis-based fracture classification. The AOSpine Sacral Classification System described in the present article characterizes injury morphology on the basis of increasing levels of posterior pelvic and spinopelvic instability. Type-A fractures are not associated with either posterior pelvic or spinopelvic instability, type-B fractures are associated with posterior pelvic instability but not spinopelvic instability, and type-C fractures are associated with spinopelvic instability. In addition, modifiers indicating concomitant patient-specific characteristics that may affect treatment and prognosis, as well as the neurologic status of the patient, can be added to increase specificity. The development of this classification system was based on a methodology consistent with previously described and validated AOSpine classification systems with use of an expert panel of international spine and orthapaedic trauma surgeons11,12. Furthermore, given the complexities of sacral fractures, as well as the fact that these fractures are often treated by both spine surgeons (orthopaedic and neurosurgical) and orthopaedic trauma surgeons, a survey of possible controversial components of the classification was sent to all members of AOSpine and AOTrauma prior to finalizing the classification.
Because of the pelvic-ring injuries that commonly occur in association with sacral fractures, previous classifications of sacral fractures have been incorporated into more general orthopaedic trauma classifications for pelvic injuries, such as the Letournel, Tile, Isler, or AO/OTA classification systems2,16-19. Tile noted that the stability of the pelvic ring depended on the integrity of the posterior weight-bearing sacroiliac joint complex, along with the integrity of the sacroiliac, sacrotuberous, and sacrospinous ligaments16. Similarly, Isler and Ganz classified sacral fractures on the basis of the morphological characteristics, particularly with respect to the integrity of the L5-S1 facet joint, and the implications of such characteristics on lumbosacral stability2. In 2007, the AO and Orthopaedic Trauma Association (OTA) created a combined classification system (AO/OTA) for pelvic-ring injuries that classifies injuries on the basis of location and, similarly to the Tile system, has implications regarding pelvic stability18. In 1985, Roy-Camille et al. were among the first to retrospectively identify a larger group of patients with fractures of the upper sacrum as a result of a high-energy mechanism, and determined a classification system based on the pattern of displacement of the transverse sacral fracture, which had implications on operative treatment4. Strange-Vognsen and Lebech added to this classification to further describe a comminuted, axial compression-type injury7. Sabiston and Wing retrospectively reviewed 35 sacral fractures and described a simple classification system with 3 types based on morphology: a vertical fracture with associated pelvic-ring injury, a lower-segment sacral fracture, and an upper-segment sacral fracture5. In a 1988 study, Denis et al. retrospectively reviewed 236 cases and developed a concise and easy-to-use classification system3. This system categorizes fractures on the basis of the location relative to the sacral foramina and notes an increasing prevalence of neurologic injury with progressively more medial fracture location, occurring in up to 57% of central sacral fractures3; however, this rate of neurologic injury is highly variable depending on the fracture pattern. For example, central sacral fractures with a vertical orientation are noted to have a very low incidence of neurologic injury, whereas those with a transverse component designating a U-type fracture have a much higher rate of neurologic injury20. More recently, Lehman et al. created a comprehensive classification system for complex lumbosacral injuries that accounts for injury morphology, integrity of the posterior ligamentous complex, and neurologic status21; however, to date, this system has not achieved widespread adoption.
Because of the inherent differences between all of the systems, current classification schemes are inadequate to account for the relationship between all types of injuries and to standardize treatment algorithms. Arising from the apparent need for a concise and comprehensive sacral fracture classification system, the AOSpine Sacral Classification System was developed. In the present study, the validation process showed substantial (κ = 0.75) interrater agreement for determining fracture severity (i.e., A, B, or C) and moderate (κ = 0.58) interrater agreement for determining fracture subtype (e.g., A1, A2). These results are directly comparable with the previously validated AOSpine classifications for the cervical subaxial spine (κ = 0.64 for subtype and κ = 64 for severity) and the thoracolumbar spine (κ = 0.56 for subtype and κ = 0.74 for severity)11,12. Interestingly, in the present study, even though agreement for fracture severity group A (κ = 0.95) was the highest, agreement was lowest when rating fracture subtype A1 (κ = 0.20). Because A1 fractures designate ligamentous avulsion injuries or compression fractures, this discrepancy in agreement for subtype-A1 fractures compared with type-A fractures may be due to the result of a difficulty in diagnosing these subtle injuries. In contrast, agreement was much higher for subtypes A2 (κ = 0.81) and A3 (κ = 0.78), which designate nondisplaced and displaced transverse fractures below the sacroiliac joint, indicating that these injuries are much more readily apparent on imaging. Other subtypes that scored as fair agreement (0.2 < κ ≤ 0.4) were fracture subtypes C0, C1, and C2. Although low agreement for C0 and C1 fractures may be explained in part due to difficulty in identifying subtle nondisplaced fracture lines, the reason for low agreement for C2 fractures is unclear and may be a result of the low number of fractures fitting this description. Nevertheless, overall agreement for all type-C fractures was substantial (κ = 0.70). When analyzing intrarater reproducibility, reviewers fared better when rating fracture severity (κ = 0.83, excellent) than when rating fracture subtype (κ = 0.71, substantial). This difference likely represents the fact that overall fracture severity (i.e., lower sacrococcygeal, posterior pelvic, or spinopelvic injuries) is easier to categorize, whereas identifying the exact fracture subtype requires interpretation of fracture lines, leading to variability among surgeons. All reviewers scored moderate reproducibility or higher, indicating strong internal validity to this scoring mechanism.
Limitations of this study include that it was conducted with a group of AOSpine and AOTrauma surgeons who may have varying degrees of familiarity with previously developed AOSpine trauma classification systems. Although not directly applicable to the sacral fracture classification, familiarity with previous systems may help surgeons classify fractures on the basis of severity. Including surgeons completely unfamiliar with the classification system would have provided a more robust test of reliability. Also, fractures were presented to reviewers with use of key images obtained from data image files that showed the fracture morphology and thus it is possible that by scanning the entire imaging file some reviewers might have changed their responses. Furthermore, this study assessed reliability of the classification system in a limited set of fracture patterns; however, future studies with incorporation of other existing classification systems would provide assessment of validity. These estimates of reliability should be considered preliminary and are likely to represent the upper bounds because they were obtained from experienced raters. Finally, any classification system inherently cannot account for all possible fracture patterns because classification systems are by nature dichotomous and fracture patterns are continuous variables. Therefore, any difficulty with fracture classification should be clearly communicated between physicians to prevent misdiagnosis or change in treatment.
Conclusions
To our knowledge, the present study is the first to describe the reliability of the AOSpine Sacral Classification System. Similar to previously described AOSpine trauma classifications, the results from the present study show that this system provides moderate to substantial interrater reliability among a group of international spine surgeons. This is an important first step toward standardizing treatment algorithms for patients with these uncommon, complex injuries.
Acknowledgments
Note: The authors thank Christian Knolls from AOCID for statistical analysis and support.
Footnotes
Disclosure: This study was organized and funded by AOSpine through the AOSpine Knowledge Forum Trauma, a focused group of international trauma experts in the field of orthopaedic traumatology and spine. AOSpine is a clinical division of the AO Foundation, which is an independent medically guided not-for-profit organization. Study support was provided directly through the AOSpine Research Department. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had a relevant financial relationship in the biomedical arena outside the submitted work (http://links.lww.com/JBJS/F857).
References
- 1.Mehta S, Auerbach JD, Born CT, Chin KR. Sacral fractures. J Am Acad Orthop Surg. 2006. November;14(12):656-65. [DOI] [PubMed] [Google Scholar]
- 2.Isler B, Ganz R. Classification of pelvic ring injuries. Injury. 1996;27(Suppl 1):S-A3-12. [DOI] [PubMed] [Google Scholar]
- 3.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988. February;227:67-81. [PubMed] [Google Scholar]
- 4.Roy-Camille R, Saillant G, Gagna G, Mazel C. Transverse fracture of the upper sacrum. Suicidal jumper’s fracture. Spine. 1985. November;10(9):838-45. [DOI] [PubMed] [Google Scholar]
- 5.Sabiston CP, Wing PC. Sacral fractures: classification and neurologic implications. J Trauma. 1986. December;26(12):1113-5. [DOI] [PubMed] [Google Scholar]
- 6.Schmidek HH, Smith DA, Kristiansen TK. Sacral fractures. Neurosurgery. 1984. November;15(5):735-46. [DOI] [PubMed] [Google Scholar]
- 7.Strange-Vognsen HH, Lebech A. An unusual type of fracture in the upper sacrum. J Orthop Trauma. 1991;5(2):200-3. [DOI] [PubMed] [Google Scholar]
- 8.Vaccaro AR, Kim DH, Brodke DS, Harris M, Chapman JR, Schildhauer T, Routt ML, Sasso RC. Diagnosis and management of sacral spine fractures. Instr Course Lect. 2004;53:375-85. [PubMed] [Google Scholar]
- 9.Schnake KJ, Schroeder GD, Vaccaro AR, Oner C. AOSpine classification systems (subaxial, thoracolumbar). J Orthop Trauma. 2017. September;31(Suppl 4):S14-23. [DOI] [PubMed] [Google Scholar]
- 10.Divi SN, Schroeder GD, Oner FC, Kandziora F, Schnake KJ, Dvorak MF, Benneker LM, Chapman JR, Vaccaro AR. AOSpine- spine trauma classification system: the value of modifiers: a narrative review with commentary on evolving descriptive principles. Global Spine J. 2019. May;9(1)(Suppl):77S-88S. Epub 2019 May 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vaccaro AR, Koerner JD, Radcliff KE, Oner FC, Reinhold M, Schnake KJ, Kandziora F, Fehlings MG, Dvorak MF, Aarabi B, Rajasekaran S, Schroeder GD, Kepler CK, Vialle LR. AOSpine subaxial cervical spine injury classification system. Eur Spine J. 2016. July;25(7):2173-84. Epub 2015 Feb 26. [DOI] [PubMed] [Google Scholar]
- 12.Kepler CK, Vaccaro AR, Koerner JD, Dvorak MF, Kandziora F, Rajasekaran S, Aarabi B, Vialle LR, Fehlings MG, Schroeder GD, Reinhold M, Schnake KJ, Bellabarba C, Cumhur Öner F. Reliability analysis of the AOSpine thoracolumbar spine injury classification system by a worldwide group of naïve spinal surgeons. Eur Spine J. 2016. April;25(4):1082-6. Epub 2015 Jan 20. [DOI] [PubMed] [Google Scholar]
- 13.Schroeder GD, Kurd MF, Kepler CK, Krieg JC, Wilson JR, Kleweno CP, Firoozabadi R, Bellabarba C, Kandizoria F, Schnake KJ, Rajesekaran S, Dvorak MF, Chapman JR, Vialle LR, Oner FC, Vaccaro AR. The development of a universally accepted sacral fracture classification: a survey of AOSpine and AOTrauma members. Global Spine J. 2016. November;6(7):686-94. Epub 2016 Mar 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fleiss JL. Measuring nominal scale agreement among many raters. Psychol Bull. 1971;76(5):378-82. [Google Scholar]
- 15.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977. March;33(1):159-74. [PubMed] [Google Scholar]
- 16.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988. January;70(1):1-12. [DOI] [PubMed] [Google Scholar]
- 17.Letournel E. [Surgical fixation of displaced pelvic fractures and dislocations of the symphysis pubis (excluding acetabular fractures) (author’s transl)]. Rev Chir Orthop Repar Appar Mot. 1981;67(8):771-82. French. [PubMed] [Google Scholar]
- 18.Marsh JL, Slongo TF, Agel J, Broderick JS, Creevey W, DeCoster TA, Prokuski L, Sirkin MS, Ziran B, Henley B, Audigé L. Fracture and dislocation classification compendium - 2007: Orthopaedic Trauma Association Classification, Database and Outcomes Committee. J Orthop Trauma. 2007. Nov-Dec;21(10)(Suppl):S1-133. [DOI] [PubMed] [Google Scholar]
- 19.Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF. Introduction: fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018. January;32(Suppl 1):S1-170. [DOI] [PubMed] [Google Scholar]
- 20.Bellabarba C, Stewart JD, Ricci WM, DiPasquale TG, Bolhofner BR. Midline sagittal sacral fractures in anterior-posterior compression pelvic ring injuries. J Orthop Trauma. 2003. January;17(1):32-7. [DOI] [PubMed] [Google Scholar]
- 21.Lehman RA, Jr, Kang DG, Bellabarba C. A new classification for complex lumbosacral injuries. Spine J. 2012. July;12(7):612-28. [DOI] [PubMed] [Google Scholar]