Abstract
Background:
The American College of Clinical Pharmacy (ACCP) prepared clinical pharmacist competencies that have specific recommendations. Recently, many efforts to advance clinical pharmacy services in Egypt exist. The literature revealed that no country has assessed the extent of applicability of ACCP competencies in its current pharmacy practice setting. Egyptian pharmacists can provide feedback about applicability of such competencies in clinical pharmacy settings in Egypt.
Objective:
The objective of this study was to investigate the extent to which ACCP competencies were implemented by Egyptian clinical pharmacists and therefore evaluate development of clinical pharmacy practice in Egypt. The study also investigated factors affecting the applicability of such competencies in the current clinical pharmacy practice setting in Egypt.
Methods:
Four hundred and ninety-five randomly selected clinical pharmacists from several hospitals were invited to participate in a cross sectional survey using a self-administered validated questionnaire composed of 31 questions classified into six domains. This questionnaire was designed to determine the pharmacists’ perception about applicability of ACCP competencies to clinical pharmacy practice in Egypt.
Results:
The response rate was 64% as 317 out of 495 pharmacists completed the questionnaire. These pharmacists were categorized according to age; gender; qualifications; years of previous work experience, years since BSc. and type of hospitals they are currently working at. Analysis of data revealed the professionalism domain to have the highest percentage of acceptance among pharmacists, while the system-based care & population health domain had the lowest percentage of acceptance. Results also showed that qualifications of participants did not affect their response in three domains; “Direct Patient Care”, “Systems-based Care & Population Health” and “Continuing Professional Development” (p=0.082, 0.081, 0.060), respectively. Nevertheless, qualifications of participants did affect their response in the other three domains; “Pharmacotherapy Knowledge”, “Communication” and “Professionalism” (p<0.05). The age of pharmacists, gender, years of previous work experience, and graduation year did not affect their responses in all six domains. The type of hospital they are currently working at, though, affected their responses where, there was a highly statistically significant increase of the mean score of all domains among participants working at the NGOs/private hospitals compared to governmental hospitals (p<0.001).
Conclusions:
Egyptian pharmacists generally apply high percentage of ACCP competencies but the provided clinical pharmacy services need to be improved through applying the standards of best practice.
Keywords: Clinical Competence; Pharmacists; Professional Practice; Professionalism; Pharmacy Service, Hospital; Education, Pharmacy, Graduate; Cross-Sectional Studies; Egypt
INTRODUCTION
One of the most dramatic changes affecting pharmacy education and the future of pharmacy practice is the emerged concept of clinical pharmacy.1 The field of “clinical pharmacy” was developed in the early sixties, However, one of the first times this term was used was by Heber W. Youngken Jr. who in 1953 wrote an article titled “The Washington Experiment-Clinical Pharmacy” that was published in the American Journal of Pharmaceutical Education.2 Expansion of a new role for the pharmacist came gradually with the many socioeconomic changes related to current medical care. The idea of the new role referred to as “Clinical Pharmacist” developed in several parts of America and in 1969 it appeared to emerge as patient-oriented pharmaceutical services.1 This resulted in more direct contact with other health care team members, especially physicians and nurses.1 The use of the term “clinical pharmacists” has also been recently criticized as it gives the impression that pharmacists are either clinically trained or not, though in reality all pharmacists are trained to provide maximum patient care. Clinical pharmacists are practitioners who provide medication management and health care for patients.3 They are licensed pharmacists with advanced education and training who possess the clinical competencies necessary to practice in team-based, direct patient care environments.4 Clinical pharmacists have many roles such as evaluating of medication therapy; making pharmaceutical care plan; following-up evaluation and medication monitoring; documenting directly in the patient’s medical record the medication-related assessment and planning of care to optimize patient outcomes.5
Competency-based education has been defined in various ways and interpreted differently among academic programs. Spady (1977) defines competency-based education as “a data-based, adaptive, performance-oriented set of integrated processes that facilitate, measure, record and certify within the context of flexible time parameters the demonstration of known, explicitly stated, and agreed upon learning outcomes that reflect successful functioning in life roles.6 Riesman (1979) defines competency-based education as: A form of education that derives curriculum from an analysis of a prospective or actual role in modern society and that attempts to certify student progress on the basis of demonstrated performance in some or all aspects of that role. Theoretically, such explanations of competence are independent of time served in formal educational settings.7 The awareness for competency-based pharmacy education is relatively recent compared to other health care professional programs. The American Association of Colleges of Pharmacy has pioneered the implementation of educational outcome-based guidelines since the early 1990s.8 Descriptions of the entry-into-practice requirements for professional pharmacists are available for Australia, Canada, Europe and the United Kingdom.9,10 The design of a competency-based curriculum ideally follows a specific sequence from competencies to assessments, to learning outcomes, to teaching-learning activities.11 Conscious choices and decisions on all organizational levels are needed to achieve consistency between learning tasks, feedback to students, teacher roles, and organization of the curriculum.12 Development of competences in pharmacy practice is a basic prerequisite for providing pharmacy care and being responsible for patient treatment outcomes.13 In the United States, medical education has increased its interest in competency-based Education over the past several years.14 Acquiring new knowledge and skills is essential for professional competency.15 Competency standards in pharmacy training and education have been formulated by different organizations to focus on various stages in the development of students, residents, and clinical pharmacists.16 The American Society of Health-System Pharmacists (ASHP) published a book containing competency modules that can be utilized by hospitals as a competency program. The book contains many topics, such as infection control, patient counseling, renal dosing, fire safety and medication safety.17 The American Pharmacists’ Association (APhA) edited code of ethics for Pharmacists which includes the basic principles underlying the roles and responsibilities of pharmacists. These principles are established to guide pharmacists in their relations with patients, healthcare team and society.18 The fifth principle is “A pharmacist maintains professional competence” which is a key point in the pharmacy career.18
The American College of Clinical Pharmacy (ACCP) prepared clinical pharmacist competencies that have specific recommendations. According to ACCP, competency programs should include clinical problem solving, judgment, decision making, communication & education, medical information evaluation & management, management of patient populations and therapeutic knowledge.19 ACCP is taking the means to improve the health of humans by covering most borders of clinical pharmacy. According to this function and its center principles, ACCP is confirming that any clinical pharmacist must have the knowledge, expertise’s, attitudes, and behaviors required to transmit medication management which occur in team-based and direct patient care atmospheres.20 According to the ACCP competencies, the expectations that clinical pharmacists should be medication experts are present and classified into six essential domains: communication, systems-based care & population health, pharmacotherapy knowledge, professionalism, direct patient care and continuing professional development. In comparison with the physician’s competencies, they are especially designed to reflect the clinical pharmacy skillfulness required supplying ACCP requirements in team-based settings and patient-centered approach.20 Clinical pharmacists must complete the training and education needed to fulfill these competencies. Also, they must carry out big efforts to maintain these competences through continuous professional development. Cooperation between healthcare team will also be needed to guarantee that these competencies drive clinical pharmacists to maintain professional development and assessment by higher educational institutions, professional societies, postgraduate training programs and employers.20 Although these competencies are similar to the competences of physicians, clinical pharmacist competencies more worthily reflect big focus on pharmacotherapy and guarantee optimal medication-related outcomes and patient needs.19,21 This similarity based on all these competencies are intended to ensure that a practitioner can provide comprehensive medication management (CMM) as outlined in the ACCP Standards of Practice.4
Recently, there are a lot of efforts to advance clinical pharmacy services. In developing countries, the pharmacy practice models significantly vary based on establishing clinical pharmacy and practice.22 For example, in England, pharmacy practice research was implemented firstly in faculties of pharmacy and conjugated with post-graduation studies in the fields of health promotion programs and wellness and contributed to the development and improvement of pharmacy practice.23 In United States, There were two evolutions that shaped clinical pharmacy practice including the formation of residencies in clinical pharmacy and doctor of pharmacy degree (PharmD) programs. The Doctor of Pharmacy (PharmD) is a professional doctorate degree, also known as a clinical doctorate - a term only used in the health professions.24 The list of countries that transitioned from the BPharm to the PharmD degree, as their entry-level qualification are as follows: US, Canada (plan to offer an all-PharmD in 2020), Hungary, Italy, Japan, South Korea, Pakistan, Saudi Arabia, Thailand, Benin, Cameroon, Republic of Congo, Senegal, Tunisia, Nigeria and Ghana.25 Federal funding assisted with greatly expanding clinical pharmacy education programs in colleges of pharmacy.26 In African countries like Ethiopia, there seems to be a severe shortage of number of pharmacists. Only 1088 pharmacists are serving 80 million people which is equal to 0.14/10,000 person.27 The clinical pharmacy plan was implemented in 2007 with an objective of training patient centered pharmacy practitioners by extending the undergraduate pharmacy program from 4 to 5 years of clinical pharmacy approach.28 In Nigeria, a conversion from the traditional pharmacists’ role of compounding and dispensing of drugs began in the 1980s with the introduction of unit dose-dispensing systems and drug information services in some hospitals.29 In Saudi Arabia, the Saudi Council for health specialties developed the clinical pharmacy approach by establishing a residency program, which comprises of a two year accredited training with board certification for clinical pharmacy specialties to the graduates passing the final exam.30 In Qatar, Hamad Medical Corporation (HMC) incorporated clinical pharmacy services (CPS) at most settings (inpatient, outpatient and community) as of January 2014.31 In the United Arab Emirates, more clinical pharmacy training programs have been put in place to meet the high demand for pharmacists in the country. In October 2008, Gulf Medical University launched the Doctor of Pharmacy (PharmD) program to meet the high need of clinical pharmacy activities.32
Egypt is a developing country, with a population of approximately 100 million people.33 The healthcare system in Egypt is very complex, with a large number of private and public entities participating in the provision of medical care. Patients can obtain their medical services from university teaching hospitals, public hospitals, private hospitals, medical centers and pharmacies. The Egyptian healthcare system faces many problems including the complexity of medicines; the high cost of drugs and the lack of a sufficient number of healthcare services. There are approximately 230,000 registered pharmacists in Egypt.34 It is estimated that there is one pharmacist per 2,100 persons (compared to one pharmacist per 5,000 persons internationally) and one pharmacist for every 1.5 physicians (compared with one pharmacist for every three physicians internationally).34 The clinical pharmacy movement in Egypt was slow. Few publications have addressed the changes in pharmacy education and pharmacy practice in Egypt.35,36 El Anowr reported that, in 1980, visiting professors from the United States led the efforts to bring clinical pharmacy to Egypt, where they gave lectures at the faculty of pharmacy at Tanta University and trained some lecturers in clinical pharmacy.36 In 1994, the basic principles of clinical pharmacy were implemented at the faculty of pharmacy at Ain Shams University. After that, many faculties of pharmacy established a clinical pharmacy practice department.
In Egypt, the old model of the dispensing pharmacist is still common. But big efforts
are being made to keep speed with the needs of a developed healthcare system.
Egyptian pharmacists understand the need to play very important roles in the
rational use of medications in safe manner and are willing to accept this important
responsibility to guarantee maximum therapeutic benefit and reach the best clinical
outcomes.37 Although there are a lot of
challenges to optimize and monitor drug use, there has been a rising interest in
extending the role of the pharmacist in Egypt as a clinical pharmacist. The Egyptian
Ministry of Health established a decree number 391 for year 2012 to ensure
implementing clinical pharmacy services at all governmental hospitals.37 In Egypt, before September 1997, the
role pharmacists
pharmacists working in Egyptian hospitals
was
working in Egyptian hospitals
was mostly dispensing.38 All these factors led to the development of
clinical pharmacy practice in Egypt. Clinical pharmacy in Egypt was newly developed
and needs international competencies like ACCP competencies to develop clinical
pharmacy practice. This paper encourages different researchers to study these
competencies in different countries. Reviewing the literature revealed that no
country has assessed the extent of applicability of ACCP competencies in its current
pharmacy practice setting.
mostly dispensing.38 All these factors led to the development of
clinical pharmacy practice in Egypt. Clinical pharmacy in Egypt was newly developed
and needs international competencies like ACCP competencies to develop clinical
pharmacy practice. This paper encourages different researchers to study these
competencies in different countries. Reviewing the literature revealed that no
country has assessed the extent of applicability of ACCP competencies in its current
pharmacy practice setting.
The objective of this study was to investigate the extent to which American College of Clinical Pharmacy (ACCP) competencies were implemented by Egyptian clinical pharmacists and therefore evaluate the development of clinical pharmacy practice in Egypt. We used ACCP competencies as a tool for this purpose. It also investigated factors affecting the applicability of such competencies in the current clinical pharmacy practice setting in Egypt.
METHODS
Four hundred and ninety-five randomly selected clinical pharmacists from different hospitals participated in a survey planned to determine their perception about applicability of ACCP competencies to clinical pharmacy practice in Egypt. A multi-stage random sample was used to select participants. The Hospitals were divided into two categories: thirty two Governmental Hospitals and four NGOs/Private Hospitals. The sample was calculated by CDC epi.info online calculator for survey (www.OpenEpi.com) as follows:
The total target population size was 3000 pharmacists. Hypothesized percent of response: 50% +/- 5; we want 95% confidence limit, alpha error: 5% and Design effect:1. Sample size (n) was at least 341 with proportion of 20% from NGOs/Private hospitals and 80% from Governmental hospitals. From governmental hospitals 12 hospitals were chosen randomly by excel and another three hospitals from NGOs/Private hospitals also was chosen randomly. From each hospital (33 pharmacists) were selected randomly by Excel after setting the sample frame from each hospital by their serial number at their work without knowing their identity. The participants were of different age, gender, qualifications, graduation year and years of previous work experience. A validated questionnaire composed of six competency domains which are divided into 31 questions recognized by ACCP was used.20 The questionnaire was distributed in paper format by random individual interviews to 495 pharmacists for self-completion. All the paper forms were filled on spot. The answers to this questionnaire were evaluated using Likert scoring system which ranged from one to five in ordinal scale: 1 being the lowest and 5 being the highest. Factors investigated to assess their effect on pharmacists’ expectations of the applicability of ACCP competencies were age, gender, qualifications, years of previous work experience, years since BSc, and type of hospitals pharmacists where they are currently working at.
First, the study instrument of validated questionnaire was sent to researchers and professionals from pharmaceutical backgrounds (pharmacists and academia) to give their expert opinion with respect to its simplicity (as our native language is Arabic).20 Second, a pilot study was conducted by asking a small sample of pharmacists (N=20) for their opinions on making the questionnaire simpler and shorter. Participants from different hospitals were selected for the pilot study. Reliability was calculated using SPSS v.25 (IBM Corp., Armonk, NY, USA), and Cronbach’s alpha was 0.77, 0.87, 0.92, 0.90, 0.81 and 0.92 for the six domains, respectively. The data from the pilot study were not used in the final analysis. Cronbach’s alpha as a reliability test was conducted. The study was approved by the Research Ethics Committee of the Faculty of Pharmacy, Beni-Suef University (Rec-H-PhBsu-19002).
Analysis of data was performed using SPSS v.25 for Windows. Likert scale analysis was used to calculate the mean rank of each domain to be used as a numeric scale variable.
Description of quantitative variables was in the form of mean and standard deviation (SD) except for the domains regarding the qualification categories, they were presented as median and IQR (non-normally distribution). Description of qualitative variables was in the form of numbers and percents. Kruskal Wallis test was used to compare between different qualifications regarding the mean of each domain. Independent t-test was used to compare between the mean of the six domains of governmental and non-governmental participants. Pearson correlation was used to correlate between age, years since BSc and years of experience and the six domains (r was considered weak at ≤0.3, moderate at 0.4 to 0.6 and strong at more than 0.6). Significant level was considered when p-value<0.05
RESULTS
A total of 317 out of 495 pharmacists completed the questionnaire with a response rate of 64% with a female dominance (82.3%). The average age of the participants was 29.9 years (SD=6) ranging between 22 and 55 years of age. The participants had a minimum of one year previous work experience and maximum of 32 years of previous work experience with a mean of 6.3, (SD=5) years. The mean years since BSc was 8.3 (SD=6) years. The percentage of participants holding a BSc degree was 199(62.8%), whereas 57 (18%) had a Clinical Pharmacy Diploma, 16 (5%) had a PharmD, 2 (0.6%) had a National Fellowship Certificate, 17 (5.4%) had a Master’s degree, 24 (7.6%) had an American Board Certificate, and 2 (0.6%) had a PhD. Results also showed that 246 (77.6%) of the participating pharmacists worked in governmental hospitals while 71 (22.4%) worked in NGOs/private hospitals.
Table 1 illustrates the values of each domain of ACCP competencies after application of Likert scale analysis to transform the frequency of answers in each domain into scale variables. The values of all domains ranged from 3.2 to 3.6 and the relative weights of their scores ranged from 64.0% to 72.4%. Results also showed that 26.5%, 25.9%, 16.7%, 32.8%, 32.5%, and 30.6% of participants strongly agreed with the applicability of “Direct Patient Care”; “Pharmacotherapy Knowledge”; “Systems-based Care & Population Health”; “Communication”; “Professionalism” and “Continuing Professional Development” domains respectively.
Table 1. Pharmacists’ expectations about applicability of each ACCP competency domain.
| Domains; Mean (SD) | Relative weight of the score % (SD) | Domains’ Grades | ||||
|---|---|---|---|---|---|---|
| Strongly disagree | Disagree | Partially agree | Agree | Strongly agree | ||
| Direct Patient Care: 3.5 (1.0) | 69.1% (20.7) | 18(5.7%) | 54(17.0%) | 79(24.9%) | 82(25.9%) | 84(26.5%) |
| Pharmacotherapy Knowledge: 3.4 (1.0) | 68.1%, (20.0) | 18(5.7%) | 46(14.5%) | 75(23.7%) | 96(30.3%) | 82(25.9%) |
| Systems- based Care & Population Health: 3.2 (1.0) | 64.0%, (20.5) | 30(9.5%) | 68(21.5%) | 74(23.3%) | 92(29.0%) | 53(16.7%) |
| Communication: 3.5±1 | 70.9%, (20.8) | 25(7.9%) | 26(8.2%) | 64(20.2%) | 98(30.9%) | 104(32.8%) |
| Professionalism: 3.6 (1.0) | 72.4%, (19.3) | 17(5.4%) | 36(11.4%) | 62(19.6%) | 99(31.2%) | 103(32.5%) |
| Continuing Professional Development: 3.5 (1.0) | 70.2%, (19.3) | 11(3.5%) | 43(13.6%) | 73(23.0%) | 93(29.3%) | 97(30.6%) |
The values of each domain of ACCP competencies after application of Likert scale analysis to transform the frequency of answers in each domain into scale variables.
Results showed that there was no statistically significant linear correlation between pharmacists’ age, years since BSc and years of previous work experience and the mean score of all domains [p>0.05] (Table 2). Similarly, when results were stratified by gender, there was no statistically significant differences between males and females regarding the score of all 6 domains; (p=0.489, 0.680, 0.559, 0.928, 0.861and 0.308, respectively) (Table 3).
Table 2. Correlation between pharmacists’ age, graduation year, and years of previous work experience and different domains.
| ACCP Competency Domains | Pearson’s r (p-value) | ||
|---|---|---|---|
| Age | Graduation Year | Work experience | |
| Direct Patient Care | -0.030 (0.598) | -0.016 (0.776) | -0.034 (0.549) |
| Pharmacotherapy Knowledge | -0.027 (0.633) | -0.011 (0.847) | -0.037 (0.509) |
| Systems-based Care & Population Health | -0.007 (0.905) | 0.022 (0.702) | 0.009 (0.879) |
| Communication | -0.009 (0.876) | 0.011 (0.841) | -0.005 (0.927) |
| Professionalism | 0.032 (0.573) | 0.057 (0.308) | 0.031 (0.581) |
| Continuing Professional Development | 0.062 (0.270) | 0.075 (0.184) | 0.039 (0.485) |
Table 3. Effect of gender on applicability of ACCP competencies.
| ACCP competency domains | Males (n=56) mean (SD) | Females (n=261) mean (SD) | p-value |
|---|---|---|---|
| Direct patient care | 3.5 (1.0) | 3.4 (1.1) | 0.489 |
| Pharmacotherapy knowledge | 3.5 (0.8) | 3.4 (1.0) | 0.680 |
| Systems-based care and population health | 3.3 (0.9) | 3.2 (1.1) | 0.559 |
| Communication | 3.6 (0.9) | 3.5 (1.1) | 0.928 |
| Professionalism | 3.6 (0.9) | 3.6 (1.0) | 0.861 |
| Continuing professional development | 3.4 (1.0) | 3.5 (0.9) | 0.308 |
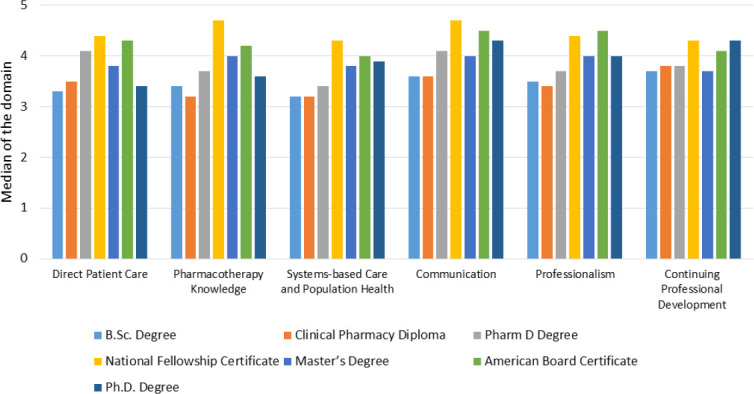
Results also showed that qualifications of participating pharmacists did not affect their perception of applicability of “Direct Patient Care”; “Systems-based Care & Population Health” and “Continuing Professional Development” domains (p=0.08, 0.08, and 0.06, respectively). On the other hand, qualifications of participating pharmacists had an effect on their perception of applicability of “Pharmacotherapy Knowledge”; “Communication” and “Professionalism” domains (p<0.05). Regarding the “Pharmacotherapy Knowledge” domain, the median (IQR) of the domain score among pharmacists with BSc, Clinical Pharmacy Diploma, PharmD, National Fellowship Certificate, Master’s degree, American Board Certificate and PhD. was 3.4 (2.6-4.0), 3.2 (2.4-4.0), 3.7 (3.2-4.6), 4.7 (4.4-5.0), 4.0 (3.2-4.2), 4.2 (3.3-4.5), 3.6 (2.4-4.8), respectively. The median score of pharmacists with National Fellowship Certificate as evident was the highest of all qualifications. There was a statistically significant difference between Clinical Pharmacy Diploma and both the American Board Certificate & National Fellowship Certificate (p<0.05) among participants with respect to “Pharmacotherapy Knowledge” domain. In the same domain, there was a statistically significant difference between BSc degree and both the American Board Certificate & National Fellowship Certificate (p<0.05). Regarding the “Communication” domain, the median (IQR) of the domain score among pharmacists with BSc, Clinical Pharmacy Diploma, PharmD, National Fellowship Certificate, Master’s degree, American Board Certificate and PhD was 3.6 (2.8-4.2), 3.6 (3.0-4.2), 4.1 (3.2-4.6), 4.7 (4.4-5.0), 4.0 (3.4-4.4), 4.5 (3.5-4.8), 4.3 (4.0-4.6) respectively. Again, the median score of pharmacists with National Fellowship Certificate as evident was the highest of all qualifications. There was a statistically significant difference between the response of participants with American Board Certificate and participants with both BSc and Clinical Pharmacy Diploma (p<0.05). Regarding the “Professionalism” domain, the median (IQR) of the domain among pharmacists with BSc, Clinical Pharmacy Diploma, PharmD, National Fellowship Certificate, Master’s degree, American Board Certificate and PhD. was 3.5 (3.0-4.3), 3.4 (3.0-4.3), 3.8 (2.9-4.8), 4.4 (3.8-5.0), 4.0 (3.3-4.5), 4.5 (3.6-5.0), 4.0 (4.0-4.8), respectively. The median score of American Board certified pharmacists as evident was the highest of all qualifications. There was a statistically significant difference between the median score of participants with the American Board Certificate compared to those with BSc degree and Clinical Pharmacy Diploma with respect to the “Professionalism” domain (p<0.05). Figure 1 demonstrates the effect of different qualifications of participating pharmacists on the median score of all ACCP competency domains.
Figure 1. Effect of different qualifications of pharmacists on median scores of ACCP Competency Domains.
Regarding the effect of type of hospitals (governmental versus NGOs/private), that participating pharmacists are working at, on their expectations of the applicability of ACCP competency domains, results showed a highly statistically significant increase of all mean domain scores among pharmacists working in the NGOs/private hospitals compared to governmental hospitals (p<0.001) as demonstrated in Table 4.
Table 4. Effect of type of hospitals (governmental versus NGOs/private) that participating pharmacists are currently working at, on their expectations of the applicability of ACCP competency domains.
| ACCP competency domains | Governmental mean (SD) | NGOs/Private mean (SD) | p-value |
|---|---|---|---|
| Direct patient care | 3.3 (1.03) | 3.9 (0.87) | p<0.001 |
| Pharmacotherapy knowledge | 3.3 (1.02) | 3.7 (0 .83) | p<0.001 |
| Systems-based care and population health | 3.1 (1.03) | 3.6 (0 .88) | p<0.001 |
| Communication | 3.4 (1.06) | 3.9 (0.85) | p<0.001 |
| Professionalism | 3.5 (0.99) | 4.0 (0.74) | p<0.001 |
| Continuing professional development | 3.4 (0.95) | 3.8 (0.92) | p<0.001 |
DISCUSSION
A major problem for clinical pharmacy practice in Egyptian hospitals is that the hospitals do not have enough qualified pharmacists to establish clinical pharmacy services and educate pharmacy students’ clinical skills during their training. Other challenges for pharmacists in clinical pharmacy practice are earning the acceptance of other healthcare team and being recognized as competent to select treatment therapy.39 The relationship between the pharmacist and physician has been characterized as complex, and some physicians have been annoyed with pharmacists providing direct patient care.40 Pharmacist-Physician communication is an important factor in the healthcare process to prevent medication errors and ensure medication safety. Many papers have studied the presence of a communication gap between physicians and pharmacists.41,42 Active communication between pharmacists and physicians in healthcare settings is essential to enhancing patient outcomes. Not only in Egypt but also in other Arabic countries including United Arab Emirates, Kuwait, Jordan, Sudan and Saudi Arabia.43-47 A ministerial decree was also issued in 2014 to increase the duration of pharmaceutical education of BSc from five to six years. The sixth year will include training in communities, hospitals, and industrial premises to ensure that pharmacy graduates have obtained the competencies required for professional practice as a pharmacist. All these factors encouraged them to study ACCP competencies as standard competencies in Egypt.
In Egypt, and according to the results of this study, pharmacists believe that ACCP competencies are generally being applied in clinical pharmacy practice settings. About one-third of the participants strongly agreed that “Communication”, “Professionalism”, and “Continuing Professional Development” domains of ACCP competencies are being applied by clinical pharmacists in Egypt. The pharmacists are expected to have good communication skills needed to deliver the best service to their patients, uphold the highest standards of integrity and honesty, serve as a credible role model and leader for students, trainees and colleagues by exhibiting the values and behaviors of a professional with active engagement in professional societies and in training of future clinical pharmacists. Results of this study also showed that about one-fourth of participants agreed that “Direct Patient Care” and “Pharmacotherapy Knowledge” domains are being applied by clinical pharmacists in Egypt, whereas only 16.7% of participants strongly agreed that “Systems-based Care & Population Health” domain of ACCP competency is being applied at the national level. Indeed, as part of the best clinical pharmacy practice, several elements of this domain are yet to be implemented in the majority of clinical pharmacy settings in Egypt. Examples of such elements are the use of health care delivery systems & health informatics to optimize the care of individual patients and patient populations, participation in identifying system-based errors & implementing solutions, resolving medication-related problems to improve patient and population health and quality metrics, applying knowledge of pharmacoeconomics & risk-benefit analysis to patient-specific and population-based care, participation in developing processes to improve transitions of care & design quality improvement processes to improve medication use.
Results showed that there was no statistically significant linear correlation between pharmacists’ age, years since BSc. and years of previous work experience and the mean score of all ACCP competency domains which reflects that such factors did not have any effect on pharmacists’ response to the survey questions regarding their expectations of the applicability of ACCP competencies. Similarly, gender of participants had no significant effect on their applicability scoring across all six domains.
Qualifications of participating pharmacists exerted a variable effect on different domains where it did not affect the pharmacists’ perception of applicability of “Direct Patient Care”, “Systems-based Care & Population Health” and “Continuing Professional Development” domains but it had an effect on the pharmacists’ perception of applicability of “Pharmacotherapy Knowledge”, “Communication” and “Professionalism” domains.
The highest applicability scoring of National Fellowship certificate in many domains may reflect the good standard of this program curriculum dealing with practical/professional direct patient care elements included in ACCP competencies. Nevertheless, this interpretation may not be warranted given that participating pharmacists with National Fellowship Certificate constituted only 2 (0.6%) of the sample.
The pharmacists working at the NGOs/private hospitals responded with higher scores reflecting their beliefs about the applicability of all ACCP competency domains compared to pharmacists working in governmental hospitals and due to difference in services between the governmental and NGO/private hospitals in Egypt. Indeed, in NGOs/Private hospitals, there is great awareness about the importance of applying the best clinical pharmacy practice standards to meet the needs of patients. Also, the better financial resources of private versus governmental hospitals may explain the participants’ responses regarding applicability of ACCP standards.
Finally, the present study had several strengths and limitations. The wide range of participants’ age, years since BSc, and years of previous work experience (22-55, 1-33, and 1-32 years, respectively) may be considered strengths of this study because it reflects a wide spectrum of opinions. Three limitation of this study are the relatively small sample size of 317 participating pharmacists, the female dominance of the sample (82.3%) and the sample of hospitals seems to be skewed to Cairo and the North of Egypt with limited number of hospitals from the South/Upper Egypt. However, it is the first study investigating the applicability of ACCP competencies in clinical pharmacy practice settings in Egypt. The number of participating female pharmacists was higher than male pharmacists probably because most of the men tend to travel outside of Egypt after earning their BSc. Degree seeking higher income to support their families. National Fellowship Certificate & PhD degree programs necessitate acceptance criteria that are difficult to be met and tend to have lengthy course of studies. Greater effort needs to be directed towards increasing studies about applicability of several international competencies on clinical pharmacy practice in Egypt and also in other countries especially competencies concerning with system based care and what benefits can be reflected from this on patients’ health-related quality of life. We must focus on weak points in clinical pharmacy practice in Egypt according to results of the study and make continuous follow up in cooperation with the Ministry of Health and Population. Results of the study can encourage other researchers in different countries to use ACCP competencies and other international competencies to evaluate clinical pharmacy practice in their institutions.
CONCLUSIONS
Egyptian pharmacists generally apply high percentage of ACCP competencies but the provided clinical pharmacy services need to be improved through applying the standards of best practice, particularly with respect to “Systems-based Care & Population Health” domain of ACCP competencies, for the purpose of delivering the best patient-care services in all hospitals in Egypt.
Footnotes
CONFLICT OF INTEREST
The authors declare not relevant conflicts of interest or financial relationships.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sector.
Contributor Information
Mahmoud A. Elmaaty, PharmD. Clinical Pharmacy Specialist. Children Cancer Hospital Egypt 57357 (CCHE 57357), Cairo (Egypt). mahallawy_90@yahoo.com
Ahmed A. Elberry, PhD. Professor of Clinical Pharmacology. Faculty of Medicine, Beni-Suef University. Beni Suef (Egypt). berry_ahmed@yahoo.com
Raghda R. Hussein, PhD. Lecturer of Clinical Pharmacy. Department of Clinical Pharmacy, Faculty of Pharmacy, Beni-Suef University. Beni Suef (Egypt). raghda.hussien@pharm.bsu.edu.eg
Doaa M. Khalil, MS. Assistant Lecturer of Public Health and Community Medicine, Faculty of Medicine, Beni-Suef University. Beni Suef (Egypt). doaamahmoud@med.bsu.edu.eg
Amani E. Khalifa., PhD. Scientific Consultant for Pharmacy Affairs, Children Cancer Hospital Egypt 57357 (CCHE 57357). Cairo (Egypt). amani.khalifa@57357.org
References
- 1.Francke GN. Evolvement of “clinical pharmacy”. Drug Intell Clin Pharm. 1969;3(12):348–354. [Google Scholar]
- 2.Youngken H. The Washington Experiment—Clinical Pharmacy. Am J Pharm Educ. 1953;17:64–70. [Google Scholar]
- 3.Patient-Centered Primary Care Collaborative. The patient-centered medical home:integrating comprehensive medication management to optimize patient outcomes. [accessed Jul 1 2020]. Available at: https://www.pcpcc.org/sites/default/files/media/medmanagement.pdf .
- 4.American College of Clinical Pharmacy. Standards of practice for clinical pharmacists. Pharmacotherapy. 2014;34(8):794–797. doi: 10.1002/phar.1438. [DOI] [PubMed] [Google Scholar]
- 5.Yee GC, Haas CE. Standards of practice for clinical pharmacists:the time has come. Pharmacotherapy. 2014;34(8):769–770. doi: 10.1002/phar.1450. [DOI] [PubMed] [Google Scholar]
- 6.Spady WG. Competency based education:A bandwagon in search of a definition. Educ Res. 1977;6(1):9–14. doi: 10.3102/0013189X006001009. [DOI] [Google Scholar]
- 7.Gervais J. The operational definition of competency-based education. The Journal of Competency-Based Education. 2016;1(2):98–106. doi: 10.1002/cbe2.1011. [DOI] [Google Scholar]
- 8.Medina MS, Plaza CM, Stowe CD, Robinson ET, DeLander G, Beck DE, Melchert RB, Supernaw RB, Roche VF, Gleason BL, Strong MN, Bain A, Meyer GE, Dong BJ, Rochon J, Johnston P. Center for the Advancement of Pharmacy Education 2013 educational outcomes. Am J Pharm Educ. 2013;77(8):162. doi: 10.5688/ajpe778162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stupans I, McAllister S, Clifford R, Hughes J, Krass I, March G, Owen S, Woulfe J. Nationwide collaborative development of learning outcomes and exemplar standards for Australian pharmacy programmes. Int J Pharm Pract. 2015;23(4):283–291. doi: 10.1111/ijpp12163. [DOI] [PubMed] [Google Scholar]
- 10.Atkinson J, De Paepe K, Pozo AS, Rekkas D, Volmer D, Hirvonen J, Bozic B, Skowron A, Mircioiu C, Marcincal A, Koster A, Wilson K, van Schravendijk C. The Second Round of the PHAR-QA Survey of Competences for Pharmacy Practice. Pharmacy (Basel) 2016;4(3):27. doi: 10.3390/pharmacy4030027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frank JR, Snell LS, Cate OT, Holmboe ES, Carraccio C, Swing SR, Harris P, Glasgow NJ, Campbell C, Dath D, Harden RM, Iobst W, Long DM, Mungroo R, Richardson DL, Sherbino J, Silver I, Taber S, Talbot M, Harris KA. Competency-based medical education:theory to practice. Med Teach. 2010;32(8):638–645. doi: 10.3109/0142159x.2010.501190. [DOI] [PubMed] [Google Scholar]
- 12.Koster A, Schalekamp T, Meijerman I. Implementation of Competency-Based Pharmacy Education (CBPE) Pharmacy (Basel) 2017;5(1):10. doi: 10.3390/pharmacy5010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McRobbie D, Webb D, Bates I, Wright J, Davies J. Assessment of clinical competence:designing a competence grid for junior pharmacists. Pharm Educ. 2018;1(2):10. [Google Scholar]
- 14.Medina MS. Does Competency-Based Education Have a Role in Academic Pharmacy in the United States? Pharmacy (Basel) 2017;5(1):13. doi: 10.3390/pharmacy5010013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tran TT, El-Ibiary S, Tindula R, Rai N, Nguyen A, Le J. Unique pharmacist competency program at community-based, teaching hospitals. J Hosp Adm. 2013;2(3):119. doi: 10.5430/jha.v2n3p119. [DOI] [Google Scholar]
- 16.Engle JP, et al. ACCP clinical pharmacist competencies:Advocating alignment between student, resident, and practitioner competencies. Journal of the American College of Clinical Pharm. 2020;3(1):124–132. doi: 10.1002/jac5.1200. [DOI] [Google Scholar]
- 17.Murdaugh L, Gomez A. Designing and managing a competence assessment program. Bethesda, MD: Oxford University Press; 2008. [Google Scholar]
- 18.Raichki RS, Nicha V, Panovska TK. [Professional competences, credentialing and continuing professional development in the pharmacy profession] Skopje: Macedonian Pharmaceutical Society; [Google Scholar]
- 19.American College of Clinical Pharmacy. Burke JM, Miller WA, Spencer AP, Crank CW, Adkins L, Bertch KE, Ragucci DP, Smith WE, Valley AW. Clinical pharmacist competencies. Pharmacotherapy. 2008;28(6):806–815. doi: 10.1592/phco.28.6.806. [DOI] [PubMed] [Google Scholar]
- 20.Saseen JJ, Ripley TL, Bondi D, Burke JM, Cohen LJ, McBane S, McConnell KJ, Sackey B, Sanoski C, Simonyan A, Taylor J, Vande Griend JP. ACCP Clinical Pharmacist Competencies. Pharmacotherapy. 2017;37(5):630–636. doi: 10.1002/phar.1923. [DOI] [PubMed] [Google Scholar]
- 21.Ambrose AJ, Lin SY, Chun MB. Cultural competency training requirements in graduate medical education. J Grad Med Educ. 2013;5(2):227–231. doi: 10.4300/jgme-d-12-00085.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47(3):533–543. [PubMed] [Google Scholar]
- 23.Weiss SL, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. 2020;46(Suppl 1):10–67. doi: 10.1007/s00134-019-05878-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pierce D, Peyton C. A historical cross-disciplinary perspective on the professional doctorate in occupational therapy. Am J Occup Ther. 1999;53(1):64–71. doi: 10.5014/ajot.53.1.64. [DOI] [PubMed] [Google Scholar]
- 25.Supapaan T, Low BY, Wongpoowarak P, Moolasarn S, Anderson C. A transition from the BPharm to the PharmD degree in five selected countries. Pharm Pract (Granada) 2019;17(3):1611. doi: 10.18549/pharmpract.2019.3.1611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carter BL. Evolution of Clinical Pharmacy in the USA and Future Directions for Patient Care. Drugs Aging. 2016;33(3):169–177. doi: 10.1007/s40266-016-0349-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Odegard PS, Tadeg H, Downing D, et al. Strengthening pharmaceutical care education in Ethiopia through instructional collaboration. Am J Pharm Educ. 2011;75(7):134. doi: 10.5688/ajpe757134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mekonnen AB, Yesuf EA, Odegard PS, Wega SS. Implementing ward based clinical pharmacy services in an Ethiopian University Hospital. Pharm Pract (Granada) 2013;11(1):51–57. doi: 10.4321/s1886-36552013000100009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Auta A, Strickland-Hodge B, Maz J. Challenges to clinical pharmacy practice in Nigerian hospitals:a qualitative exploration of stakeholders'views. J Eval Clin Pract. 2016;22(5):699–706. doi: 10.1111/jep.12520. [DOI] [PubMed] [Google Scholar]
- 30.Mehmood SI, Kumar A, Al-Binali A, Borleffs JC. Specialty preferences:trends and perceptions among Saudi undergraduate medical students. Med Teach. 2012;34(Suppl1):S51–S60. doi: 10.3109/0142159x.2012.656753. [DOI] [PubMed] [Google Scholar]
- 31.Eltorki Y, Abdallah O, Omar N, Zolezzi M. Perceptions and expectations of health care providers towards clinical pharmacy services in a mental health hospital in Qatar. Asian J Psychiatr. 2019;42:62–66. doi: 10.1016/j.ajp.2019.03.018. [DOI] [PubMed] [Google Scholar]
- 32.Abu-Gharbieh E, Fahmy S, Rasool BA, Abduelkarem A, Basheti I. Attitudes and perceptions of healthcare providers and medical students towards clinical pharmacy services in United Arab Emirates. Trop J Pharm Res. 2010;9(5):61050. doi: 10.4314/tjpr.v9i5.61050. [DOI] [Google Scholar]
- 33.Central Agency for Public Mobilization and Statistics. Homepage. [accessed Jul 1 2020]. www.capmas.gov.eg/default.aspx .
- 34.Egyptian Pharmacists Syndicate. Homepage. [accessed Jul 1 2020]. www.eps-egypt.net .
- 35.Abdel-Latif MM, Sabra K. Clinical pharmacy practice in Egyptian hospitals. Am J Health Syst Pharm. 2016;73(1):e63–e66. doi: 10.2146/ajhp150250. [DOI] [PubMed] [Google Scholar]
- 36.El-Awady el -SE, Moss S, Mottram D, O'Donnell J. Student perspectives on pharmacy curriculum and instruction in Egyptian schools. Am J Pharm Educ. 2006;70(1):9. doi: 10.5688/aj700109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sabry NA, Farid SF. The role of clinical pharmacists as perceived by Egyptian physicians. Int J Pharm Pract. 2014;22(5):354–359. doi: 10.1111/ijpp12087. [DOI] [PubMed] [Google Scholar]
- 38.El-Anor WM. History of Clinical Pharmacy Practice in Egypt (Part 2) Int J Pharm Teach Pract. 2011;2(2):61–63. [Google Scholar]
- 39.Lambert BL. Face and politeness in pharmacist-physician interaction. Soc Sci Med. 1996;43(8):1189–1198. doi: 10.1016/0277-9536(95)00370-3. [DOI] [PubMed] [Google Scholar]
- 40.Ranelli PL, Biss J. Physicians'perceptions of communication with and responsibilities of pharmacists. J Am Pharm Assoc (Wash) 2000;40(5):625–630. doi: 10.1016/s1086-5802(16)31102-0. [DOI] [PubMed] [Google Scholar]
- 41.Bradshaw SJ, Doucette WR. Community pharmacists as patient advocates:physician attitudes. J Am Pharm Assoc (Wash) 1998;38(5):598–602. doi: 10.1016/s1086-5802(16)30373-4. [DOI] [PubMed] [Google Scholar]
- 42.Nesbit F, Chaplin DC, Edwards JA Jr, Fleming GR, Harker MN, Work DR, Neelon FA. Counseling of patients by pharmacists. Blessing or curse? N C Med J. 1995;56(2):115–118. [PubMed] [Google Scholar]
- 43.Matowe L, Abahussain EA, Al-Saffar N, Bihzad SM, Al-Foraih A, Al-Kandery AA. Physicians'perceptions and expectations of pharmacists'professional duties in government hospitals in Kuwait. Med Princ Pract. 2006;15(3):185–189. doi: 10.1159/000092179. [DOI] [PubMed] [Google Scholar]
- 44.Fahmy SA, Rasool BK, Abdu S. Health-care professionals'perceptions and expectations of pharmacists'role in the emergency department, United Arab Emirates. East Mediterr Health J. 2013;19(9):794–801. [PubMed] [Google Scholar]
- 45.Francis J, Abraham S. Clinical pharmacists:Bridging the gap between patients and physicians. Saudi Pharm J. 2014;22(6):600–602. doi: 10.1016/j.jsps.2014.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tahaineh LM, Wazaify M, Albsoul-Younes A, Khader Y, Zaidan M. Perceptions, experiences, and expectations of physicians in hospital settings in Jordan regarding the role of the pharmacist. Res Social Adm Pharm. 2009;5(1):63–70. doi: 10.1016/j.sapharm.2008.05.003. [DOI] [PubMed] [Google Scholar]
- 47.Awad A, Matowe L, Capps P. Medical doctors'perceptions and expectations of the role of hospital pharmacists in Sudan. Pharm World Sci. 2007;29(5):557–564. doi: 10.1007/s11096-007-9111-5. [DOI] [PubMed] [Google Scholar]


