Abstract
Background
The Covid-19 pandemic has led to the introduction of conservative non-operative approaches to surgical management favouring community driven care. The aim of this study was to determine the effect of these pathways on patients attending a surgical assessment unit (SAU).
Method
This was a retrospective observational cohort study. We included all consecutive attendances to the SAU in April 2020 (Covid-19 period) and April 2019 (pre-Covid-19). The Covid-19 period saw a shift in clinical practice towards a more conservative approach to the management of acute surgical presentations. The primary outcome measure was 30-day readmission. The secondary outcome measures were length of hospital stay, inpatient investigations undertaken and 30-day mortality.
Results
A total of 451 patients were included. This represented 277 and 174 attendances in pre-Covid-19, and Covid-19 groups respectively. The rates of unplanned 30-day readmission rates in the Covid-19 and pre-Covid-19 periods were 16.7% and 12.6% respectively (P = 0.232). There were significantly fewer planned follow-ups in the Covid-19 (36.2%) compared to the pre-Covid-19 group (49.1%; P < 0.01; OR 1.7, 95% CI 1.15–2.51). There were no significant differences in length of hospital stay (P = 0.802), and 30-day mortality rate (P = 0.716; OR 1.9, 95% CI 0.38–9.54) between the two periods.
Conclusion
There were no differences in 30-day readmission rates, length of hospital stay, and 30-day mortality with the changes to pathways. Our findings suggest the resource efficient conservative Covid-19 pathways could potentially continue long-term. However, further multi-centre studies with larger sample sizes and longer follow-up duration will be required to validate our findings.
Keywords: Covid-19, Pandemic, Surgical assessment unit, General surgery
Introduction
The World Health Organisation (WHO) declared a global pandemic from the novel coronavirus, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), also termed COVID-19, on 11th March 2020.1 Patients typically develop symptoms such as cough and fever and the majority have a good prognosis.2 However, its rapid transmissibility and unpredictably high morbidity and mortality risk, particularly on seemingly fit and healthy patients, has led to a global mass casualty incident response.3
In the UK, certain measures were put in place to reduce disease transmission and the impact of the disease burden. This included converting some operating theatres to intensive care units, redeployment of staff, cancellation of elective surgery and routine endoscopy, and implementation of virtual outpatient clinics where possible.2 These drastic measures combined with the government's ‘stay at home’ message have led to an observed reduction in non-Covid-19 attendances to hospital in the last few months.
Patients attending the surgical assessment unit (SAU) were managed in accordance with the intercollegiate guidelines produced by the four Royal College of Surgeons, Association of Surgeons of Great Britain & Ireland, Association of Coloproctology of Great Britain & Ireland, and Association of Upper Gastrointestinal Surgeons on March 27th 2020.4 Table 1 summarises this guidance.
Table 1.
Guidance for surgical management during the Covid-19 pandemic.
| Emergency surgery | Test all for Covid-19. Treat all as positive. CT thorax 24 h preoperatively where possible. Add CT thorax if having CT abdomen. |
| Elective surgery | Risk assessment for Covid-19. |
| Greater risks of surgery. | |
| Consent for greater unknown risk. | |
| Risk reducing strategies eg stoma. | |
| PPE | PPE for all laparotomies. |
| Unless Covid-19 negative (beware of false negatives). | |
| Wear eye protection. | |
| Practice donning and doffing. | |
| Theatre | Minimum staffing levels. |
| All staff wearing full PPE. | |
| Stop positive pressure ventilation. | |
| Smoke extraction. | |
| Intubation/extubation in theatre. | |
| Laparoscopic | Avoid if possible. |
| Filters etc difficult to implement. | |
| Treat appendicitis and cholecystitis with conservative management/open surgery. | |
| Endoscopy | Emergency only. |
| Follow BSG guidance. | |
| Upper GI endoscopy requires full PPE. |
This guidance led to numerous changes to routine surgical practice across the UK. In East Sussex Healthcare Trust patients attending the SAU were treated with conservative measures wherever safely possible. Patients presenting with acute benign pathology (such as biliary colic, mild diverticulitis, non-specific abdominal pain) were promptly discharged and encouraged to manage their condition at home with medication. They were given more ownership over their health and some were provided with 48 h open access straight back to the SAU should their condition deteriorate. Fewer patients had follow-up investigations or routine follow-up clinic appointments arranged. Patients presenting with severe conditions (such as bowel ischaemia and bowel obstruction) were managed as per normal surgical practice. Surgeons were encouraged to minimise use of radiological investigations to allow for the increased demand from medical and intensive care specialties. All elective (non-cancerous) and laparoscopic operating had ceased by the end of March 2020. Access to endoscopy was significantly reduced, limited to emergency procedures and for those patients with a high degree of suspicion for colorectal cancer. All patients requiring emergency life-threatening operations were continued as normal. Elective colorectal cancer operating continued, however operating lists were reduced to twice weekly with two consultants operating on each case.
Covid-19 has brought about unprecedented changes to surgical admissions and the management of patients with surgical presentations. The aim of this study is to determine the impact of these changes on patient outcomes. Some of these management approaches may have no negative effect on outcomes, and potentially reduce unnecessary use of clinical resources if considered safe.
Methodology
This was a retrospective observational cohort study. We included all consecutive adult (>16 years) general surgical emergency patients who attended the SAU at Conquest Hospital, East Sussex Healthcare NHS Trust at two different periods. The time periods were April 2019 and April 2020 representing the pre-Covid-19 and Covid-19 periods respectively. The East Sussex Healthcare Trust cares for a population of approximately 555 000 people.5 Referral pathways to the SAU during the Covid-19 period remained the same as the pre-Covid-19 time period. All vascular referrals were sent directly from A&E to the nearest vascular centre. All referrals from primary care settings (general practice, urgent care and walk-in centres) and Accident and Emergency (A&E) were discussed with the registrar on call. Direct referrals were also taken from paramedics and discussed with a senior nurse in charge at the SAU.
Data was gathered from the hospital's electronic patient records. The following data was collected: patient demographics, diagnosis, clinical investigations (including Covid-19 status), management, readmission, follow-up, and mortality.
Patients were excluded if they had attended the SAU for an elective procedure or if they were accepted for review on the SAU by a different speciality (such as Orthopaedics, Urology or Gynaecology). Patients were also excluded if notes were not available.
The age-adjusted Charlson Comorbidity Index (CCI) was calculated for each patient using the online MedCalc tool. This scoring system estimates 10-year survival in patients with multiple co-morbidities. It was selected as it is widely used amongst surgical and non-surgical specialties to predict adverse outcomes.6
Readmission to the SAU was categorised into planned follow-up and unplanned readmission. Patients categorised as planned follow-up were discharged with a pre-arrangement to return for a scan, repeat blood tests or simple review either on the SAU or in outpatient clinic. Unplanned readmissions relate to those who were discharged and re-presented unexpectedly within the 30-day follow-up; this also includes patients who were discharged with 48-h’ ‘open access’ and re-presented. Length of hospital stay was calculated by the number of days patients were admitted under the general surgical team during first presentation only. Readmission and mortality rates were followed up for 30 days after first presentation.
During the Covid-19 period patients at Conquest Hospital were nasally swabbed for viral RNA detection by quantitative RT-PCR if there was clinical suspicion of Covid-19 infection. This suspicion was based on the UK government's symptomatic criteria: high fever or continuous new cough.7 A positive swab or radiological evidence of Covid-19 on a CT thorax was used to confirm diagnosis.
A cost analysis during pre-Covid-19 and Covid-19 eras was conducted using cost estimates provided by the East Sussex Healthcare costing team. For radiological or endoscopic procedures costs have been provided for the most commonly used for example, CT scan with contrast of abdomen and pelvis. There was no difference in cost for inpatient or outpatient procedures.
Data was analysed using Microsoft Excel and SPSS. Chi squared (χ2), T-Tests and Fisher Exact tests were used to calculate statistical significance of the primary outcome, 30-day unplanned readmissions and the secondary outcomes, length of hospital stay, number of inpatient investigations and 30-day mortality.
The study was conducted according to STROBE guidelines for observational studies.8 Continuous data were tested for distribution with normally distributed data presented as mean and standard deviation. Demographic differences between the pre-Covid-19 and peri-Covid-19 groups were tested using the independent T test. The χ2 and Fisher's exact tests were used for categorical data. Odds ratios with 95% confidence intervals were calculated for statistically significant relationships with a significance of P < 0.05.
The study was approved by the hospital's clinical effectiveness unit (QIP 160). Ethical approval was not required as the study method was retrospective and the design did not involve any changes to patients' care, treatment or services.
Results
A total of 638 patients presented to the SAU during the two time periods. 129 patients were excluded as they were initially referred from primary care or A&E to another speciality and were reviewed on the SAU by that speciality. A further 58 were excluded, as electronic notes were not available. As a result, 451 patients were included in our study. 277 patients attended the SAU in the pre-Covid-19 group and 174 in Covid-19 group.
As shown in Table 2 the mean age was 57 years in both patient groups with a standard deviation of 20.7 and 21.6 respectively. There was no statistical difference in the ages of the two groups (P = 0.879). 161 (58%) of the pre-Covid-19 group and 100 (57.5%) of the Covid-19 group were of female gender; this was not statistically significant between the groups; P = 0.892. There was no significant difference between the comorbidities of the groups as the CCI average was 73.8 and 71.9 (P = 0.562).
Table 2.
Comparison of patient demographics and outcome measures between the pre-Covid-19 and Covid-19 groups.
| Pre-Covid-19 Period N = 277 (%) |
Covid-19 Period N = 174 (%) |
P value | Odds ratiob | ||
|---|---|---|---|---|---|
| Age (years) | Mean (SD) | 57.1 (20.7) | 57.5 (21.6) | 0.879 | |
| Female | 161 (58.1) | 100 (57.5) | 0.892 | ||
| Charlson comorbidity index % | Mean (SD) | 73.8 (32.0) | 71.9 (33.4) | 0.562 | |
| Total number of patients who had inpatient investigations | 170 (61.4) | 122 (70.1) | 0.059 | ||
| Total number of inpatient investigations | 205 | 161 | |||
| Inpatient | X-Ray | 29 (10.5) | 43 (24.7) | ||
| Ultrasound | 35 (12.6) | 27 (15.5) | |||
| CT scan | 131 (47) | 82 (47) | 0.973 | ||
| OGD | 0 (0) | 1 (0.6) | |||
| MRCP | 4 (1.4) | 3 (1.7) | |||
| ERCP | 6 (2.2) | 5 (2.9) | |||
| Total number of patients who had outpatient investigations | 94 (33.9) | 33 (19.0) | 0.001 | 2.19 (1.39–3.45) | |
| Total number of outpatient investigations | 105 | 35 | |||
| Outpatient | X-Ray | 1 (0.3) | 0 (0) | ||
| Ultrasound | 19 (6.9) | 5 (2.9) | |||
| CT scan | 19 (6.9) | 5 (2.9) | |||
| OGD | 11 (4.0) | 3 (1.7) | |||
| Colonoscopy | 33 (11.9) | 16 (9.2) | |||
| MRI | 20 (7.2) | 6 (3.4) | |||
| ERCP | 2 (0.7) | 0 (0) | |||
| Length of hospital stay (days) | Mean (SD) | 3.9 (8.9) | 4.1 (5.9) | 0.802 | |
| Unplanned readmission to the SAU | 35 (12.6) | 29 (16.7) | 0.232 | ||
| Unplanned readmission to another speciality | 0 (0) | 5 (2.9) | 0.008a | ||
| Planned follow-up | 136 (49.1) | 63 (36.2) | 0.007 | 1.7 (1.15–2.51) | |
| Planned follow-up to another speciality | 7 (2.5) | 15 (8.6) | 0.003 | 0.27 (0.11–0.69) | |
| 30-day mortality | 6 (2.2) | 2 (1.2) | 0.716a | 1.9 (0.38–9.54) | |
| Swabbed for Covid-19 | Not applicable | 43 (24.7) | Not applicable | ||
| Positive for Covid-19 | Not applicable | 1 (0.6) | Not applicable |
Fisher's exact test used to calculate significance.
Values in parentheses are 95 per cent confidence intervals.
There were 43 patients who were suspected to have the Covid-19 virus and had a swab taken for quantitative PCR testing. This was either during the primary admission or subsequent admissions within the 30-day follow up. Only one of these 43 was found to be positive.
Unplanned readmission within 30-days was slightly higher in the Covid-19 group at 16.7% compared to 12.6% in the pre-Covid-19 group but this was not found to be statistically significant (P = 0.232). However, if unplanned readmissions to all specialities (as 5 patients who represented went to medicine or urology) were included, this was statistically significant (P < 0.05).
There were statistically significant increased planned follow-ups in the pre-Covid-19 group compared to the Covid-19 group (P < 0.01; OR 1.7, 95% CI 1.15–2.51).
Inpatient imaging and endoscopic procedures were carried out in 170 (61.4%) patients in the pre-Covid-19 group compared to 122 (70.1%) in the Covid-19 group. This was not found to be statistically significant (p = 0.059). The number of outpatient investigations was significantly lower in the Covid-19 group when compared to the pre-Covid-19 group (p < 0.001; OR 2.19, 95% CI 1.39–3.45).
Length of hospital stay was similar between the pre-Covid-19 and Covid-19 groups with a mean value of 3.9 and 4.1 days respectively. This was not statistically significant (p = 0.802).
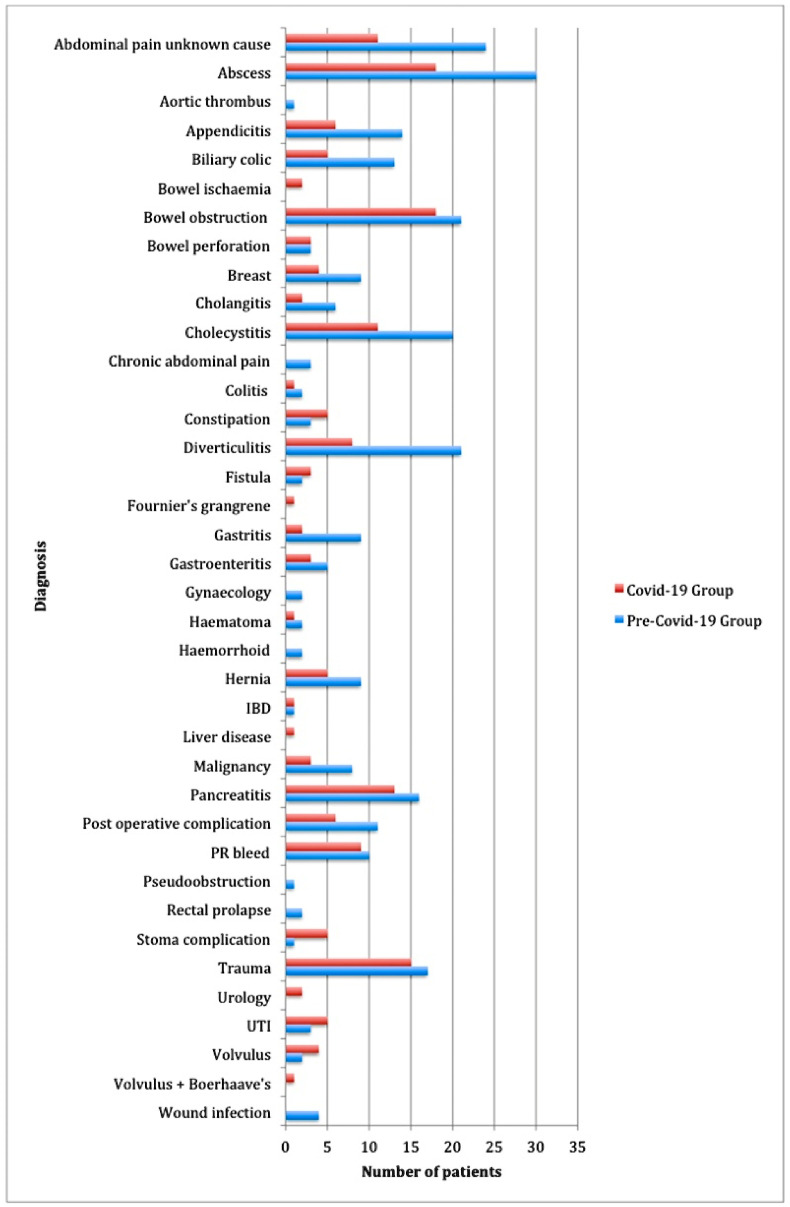
Figure 1 illustrates the various presentations seen in the two groups. As demonstrated, presentations of abdominal pain with unknown cause, appendicitis, biliary colic, diverticulitis and gastritis were considerably reduced in number in the Covid-19 compared to pre-Covid-19 group.
Fig. 1.
Patient diagnoses during pre-Covid-19 and Covid-19 timeframes.
The 30-day mortality did not differ between the two time periods (P = 0.716; OR 1.9 95% CI 0.38–9.54).
Table 3 shows the average unit costs for attendance to hospital, readmission, follow-up and radiological or endoscopic procedures. Using these figures and the results in Table 2 the pre-Covid-19 total cost is £378840.50. The Covid-19 total cost is £243 542. This yields a total cost saving of £135298.50 during the Covid-19 period.
Table 3.
Average unit costs at East Sussex Healthcare Trust.
| Unit | Cost (£) |
|---|---|
| 24-h hospital stay | 285 |
| Review on the SAU | 260 |
| Outpatient follow up | 75 |
| X-ray | 31 |
| Ultrasound | 53 |
| CT scan | 94 |
| OGD | 415 |
| MRI | 164 |
| ERCP | 1219 |
| Colonoscopy | 470 |
Discussion
This study aimed to determine the effects of generalised measures taken during the Covid-19 pandemic on outcomes in general surgical patients. We found no difference in 30-day readmission rates, length of hospital stay or 30-day mortality rates between the Covid-19 group and the pre-Covid-19 group. The total number of outpatient radiological investigations requested per patient was lower in the Covid-19 group compared to the pre-Covid-19 group and there was also considerable reduction in planned follow-ups in the Covid-19 group. This highlights the conservative approach, with fewer resources used during the Covid-19-time period. These results suggest consideration should be given to implementing some of the current conservative practices long term to reduce unnecessary use of clinical resources.
Another important comparison was 30-day readmission rates. During the pandemic, new guidance issued by the four Royal Colleges of Surgeons, advised a non-operative approach to managing acute surgical presentations where possible.4 One might conclude that this more conservative approach could have led to higher numbers of readmissions, longer hospital stays and increased mortality rates but this is not what was observed in our data.
As yet there is no other data pertaining to the clinical outcomes of measures used during the Covid-19 pandemic. Recent data published by CovidSurg 2020 concludes a 30-day mortality of 23.8% in patients who test positive for Covid-19.9 Given the sensitivity of testing is not yet 100%, and current pre-operative guidelines of a 14-day isolation period pre- and post-operatively4 are difficult to enforce, ensuring patients are Covid-19 negative in the peri-operative period is extremely difficult and will likely remain so for some time. With no observed increase in 30-day readmission or mortality rates, we would suggest an initial trial of conservative management is better for not only for efficient use of resources but for patient outcomes, particularly for the remainder of the pandemic duration. A study conducted by Prachand et al. describes a novel scoring system. It considers resource limitations and risk of Covid-19 transmission to triage elective (medically necessary time-sensitive) procedures.10 This may be a scoring system the UK should look to implement to aid surgical decision-making and manage resources more efficiently.
In our study, six patients had appendicitis during the Covid-19 group. Five of these patients were initially managed conservatively as per the intercollegiate guidelines.4 Two of these patients did not improve on antibiotics and progressed to an open appendicectomy. In the pre-Covid-19 group, 14 patients presented with appendicitis, all except one had a laparoscopic appendicectomy during the same admission. The most recent meta-analysis of antibiotics vs surgery for appendicitis concluded that for both uncomplicated and complicated adult appendicitis, non-operative management was associated with significantly fewer operative complications and a shorter length of hospital stay but a higher relapse rate. This implies antibiotic therapy may be a reasonable alternative for some patients as 80.2% of their 1463 patient cohort were effectively treated with antibiotics.11 In our study we observed a 60% success rate in conservative management. While our sample size in this respect is small and should not be used to draw any significant conclusions, it does highlight the effectiveness of the currently less popular conservative management of appendicitis. With early reports suggesting increased morbidity and mortality rates for Covid-19 positive patients undergoing an operation,9 trialling conservative instead of operative management for an initial presentation of acute appendicitis may produce improved outcomes for patients.
A cost analysis of the pre-Covid-19 period and the Covid-19 period has shown a cost saving of £135298.50 during the Covid-19 period. This is without including operative costs, which would show a further cost-saving as considerably fewer operative procedures were conducted during Covid-19 period, particularly appendicectomies and cholecystectomies. However, this was not a thorough analysis and a more detailed methodological approach identifying each individual cost would be required to accurately provide the true cost-saving of implementing these conservative methods.
There were a few limitations in our study. One such limitation is that we were unable to capture patients who contracted an acute surgical pathology without presenting to hospital. During the month of April 2020, we saw a reduction in the number of acute presentations to the SAU; this is likely due to government advice to stay at home and public fear of the Covid-19 pandemic. As such, it is entirely possible patients suffered from an acute surgical pathology at home and either their condition improved spontaneously without medical intervention or led to their death.
Should we continue this conservative approach long-term it would involve encouraging patients to seek primary care services and over the counter therapies for conditions such as mild abdominal pain, biliary colic, diverticulitis and gastritis. We could risk assess those with possible acute appendicitis and offer patients with uncomplicated appendicitis antibiotics as the first line treatment. We could see fewer patients as a planned follow up and encourage them to take more ownership of their health and to seek medical attention should they need it.
A further limitation is our follow-up period. We chose a 30-day readmission and 30-day mortality for our study, however invariably there will be patients who re-present to hospital with a complication outside of this time frame. Additionally, this study was designed as a retrospective cohort study therefore is inevitably prone to confounding factors and reliance on accurate recordkeeping. Furthermore, the study was conducted in East Sussex, which has a less ethnically diverse population than other parts of the UK. Of the 11 120 workforce in 2018, 9836 (88.5%) were White British.5 This may impede the generalisability of our results. Moreover, this study was conducted in a UK hospital with a dedicated SAU. This consists of an individual assessment room with basic treatment facilities and a separate waiting room with capacity for up to 10 more patients. Patients are reviewed here after having been discussed with a member of the surgical team and can be admitted onto the surgical ward in the SAU should they require admission. This streamlines the route for adult emergency surgical referrals and allows for rapid diagnosis and earlier access to theatre.12 It is possible our results may not be replicable in a hospital without a SAU as it enables surgeons to review and re-review patients at their ease however, adopting some of the conservative measures used in our study may well still allow for resource savings across all hospitals.
Nevertheless our results indicate that there is a need for a longer-term multicentre study, ideally prospective in design with a larger population and longer-term follow-up duration. This would serve to more accurately display any adverse clinical outcomes in patients on these new, conservative, Covid-19 pathways.
Conclusion
Measures used during the Covid-19 pandemic have resulted in fewer hospital admissions to the East Sussex SAU and promoted more community driven care. These could potentially be continued even after the resolution of the pandemic without significant adverse clinical outcomes, and in so doing allow resource savings. However, further multi-centre studies of standardised conservative approaches with larger sample sizes and a longer duration of follow-up need to be conducted.
Declaration of competing interest
None.
References
- 1.WHO Director-General’s opening remarks at the media briefing on COVID-19. 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-themedia-briefing-on-covid-19---11-march-2020 Available from: [Google Scholar]
- 2.De Simone B., Chouillard E., Di Saverio S., Pagani L., Sartelli M., Biffl W.L. Emergency surgery during the COVID-19 pandemic: what you need to know for practice. Ann R Coll Surg Engl. 2020 May;102(5):323–332. doi: 10.1308/rcsann.2020.0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Coccolini F., Perrone G., Chiarugi M., Di Marzo F., Ansaloni L., Scandroglio I. Surgery in COVID-19 patients: operational directives. World J Emerg Surg. 2020 04 7;15(1):25. doi: 10.1186/s13017-020-00307-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Intercollegiate General Surgery Guidance on COVID-19- 27 March 2020. https://www.rcsed.ac.uk/news-public-affairs/news/2020/march/intercollegiate-general-surgery-guidance-on-covid-19-update Available from:
- 5.East Sussex County Council. http://www.eastsussexinfigures.org.uk/webview/index.jsp?catalog=http%3A%2F%2Fwww.eastsussexinfigures.org.uk%3A80%2Fobj%2FfCatalog%2FCatalog6&submode=catalog&mode=documentation&top=yes (accessed 17 June 2020).
- 6.St-Louis E., Iqbal S., Feldman L.S., Sudarshan M., Deckelbaum D.L., Razek T.S. Using the age-adjusted Charlson comorbidity index to predict outcomes in emergency general surgery. J Trauma Acute Care Surg. 2015 Feb;78(2):318–323. doi: 10.1097/TA.0000000000000457. [DOI] [PubMed] [Google Scholar]
- 7.PM statement on coronavirus. 12 March 2020. https://www.gov.uk/government/speeches/pm-statement-on-coronavirus-12-march-2020 [Google Scholar]
- 8.Vandenbroucke J.P., von Elm E., Altman D.G., Gøtzsche P.C., Mulrow C.D., Pocock S.J. Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. Ann Intern Med. 2007 10 16;147(8):W163–W194. doi: 10.7326/0003-4819-147-8-200710160-00010-w1. [DOI] [PubMed] [Google Scholar]
- 9.COVIDSurg Collaborative Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020 Jul 4;396(10243):27–38. doi: 10.1016/S0140-6736(20)31182-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Prachand V.N., Milner R., Angelos P., Posner M.C., Fung J.J., Agrawal N. Medically necessary, time-sensitive procedures: scoring system to ethically and efficiently manage resource scarcity and provider risk during the COVID-19 pandemic. J Am Coll Surg. 2020 Aug;231(2):281–288. doi: 10.1016/j.jamcollsurg.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yang Z., Sun F., Ai S., Wang J., Guan W., Liu S. Meta-analysis of studies comparing conservative treatment with antibiotics and appendectomy for acute appendicitis in the adult. BMC Surg. 2019 Aug 14;19(1):110. doi: 10.1186/s12893-019-0578-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mohamed M.S., Mufti G.R. The surgical assessment unit--effective strategy for improvement of the emergency surgical pathway? J R Soc Med. 2005 Jan;98(1):14–17. doi: 10.1258/jrsm.98.1.14. [DOI] [PMC free article] [PubMed] [Google Scholar]