Abstract
Background and study aims Early studies have shown that artificial intelligence (AI) has the potential to augment the performance of gastroenterologists during endoscopy. Our aim was to determine how gastroenterologists view the potential role of AI in gastrointestinal endoscopy.
Methods In this cross-sectional study, an online survey was sent to US gastroenterologists. The survey included questions about physician level of training, experience, and practice characteristics and physician perception of AI. Descriptive statistics were used to summarize sentiment about AI. Univariate and multivariate analyses were used to assess whether background information about physicians correlated to their sentiment.
Results Surveys were emailed to 330 gastroenterologists nationwide. Between December 2018 and January 2019, 124 physicians (38 %) completed the survey. Eighty-six percent of physicians reported interest in AI-assisted colonoscopy; 84.7 % agreed that computer-assisted polyp detection (CADe) would improve their endoscopic performance. Of the respondents, 57.2 % felt comfortable using computer-aided diagnosis (CADx) to support a “diagnose and leave” strategy for hyperplastic polyps. Multivariate analysis showed that post-fellowship experience of fewer than 15 years was the most important factor in determining whether physicians were likely to believe that CADe would lead to more removed polyps (odds ratio = 5.09; P = .01). The most common concerns about implementation of AI were cost (75.2 %), operator dependence (62.8 %), and increased procedural time (60.3 %).
Conclusions Gastroenterologists have strong interest in the application of AI to colonoscopy, particularly with regard to CADe for polyp detection. The primary concerns were its cost, potential to increase procedural time, and potential to develop operator dependence. Future developments in AI should prioritize mitigation of these concerns.
Introduction
The term artificial intelligence (AI) describes the ability of computers to perform tasks that would normally require human intelligence 1 . Fueled by growth in computational speed and power as well as improvement in machine learning algorithms, AI has now been applied to a variety clinical tasks in medicine ranging from diagnosis of diabetic retinopathy to identification of cutaneous malignancies 2 3 . In gastroenterology, deep learning systems have recently shown tremendous potential to improve endoscopic performance 4 5 , and recent studies have reported effective use of AI for computer-aided polyp detection (CADe) 6 7 , classification of polyp histology (CADx) 8 9 , and differentiation of endoscopically resectable polyps (superficial) versus invasive cancer 5 10 .
Despite the early success of AI in performing and assisting with clinical tasks, there is still skepticism about the potential of this technology. Although the scientific literature supporting AI and machine learning in clinical medicine is accumulating quickly, few previous studies have described how physicians perceive the advent of this technology 11 . In this study, we survey gastroenterologists in different practice settings and levels of training to assess current sentiment toward AI, with a particular focus on two themes: 1) whether gastroenterologists expect AI to improve aspects of endoscopic performance; and 2) what potential barriers may exist for widespread adoption of AI in gastrointestinal endoscopy.
Materials and methods
In this cross-sectional observational study, an online survey questionnaire was sent via email to 330 practicing gastroenterologists in the United States. Participants were chosen to represent a diversity of training backgrounds, experience levels, and practice settings. Inclusion criteria included being a gastroenterology fellow or attending physician and having performed at least one colonoscopy. The subjects were recruited through email communication with gastroenterology divisions at two major academic hospitals with numerous ambulatory endoscopy centers around the country. No compensation was offered and participation was voluntary. The study received an exemption by the Beth Israel Deaconess Medical Center Institutional Review Board.
All participants provided consent prior to beginning the survey questionnaire. The survey was hosted online and consisted of a variety of question types. Questions were asked about physician level of training, physician experience, practice characteristics, and physician perception of AI. Survey results were stored in Microsoft Excel.
Descriptive statistics were then used to summarize the survey findings, including whether physicians believed that AI would improve procedure performance and their concerns about implementation of AI tools in endoscopy. Chi-squared test (or Fisher’s exact test when appropriate) was used to assess the association between physician characteristics and views on AI in gastroenterology. Finally, a multivariate logistic regression model was created to determine the physician characteristics that most predicted a positive sentiment toward AI.
A P < 0.05 was considered statistically significant. All data analyses were conducted using SAS version 9.4.
Results
A total of 330 gastroenterologists including private practitioners, academic practice physicians, and gastroenterology fellows across the United States were invited by email to participate in this survey. From December 2018 to January 2019, 124 physicians (38 %) completed the online survey and all of these participants were included in the final analysis.
Physician characteristics
Our sample population included 99 gastroenterology (gastrointestinal) attendings (79.8 %), 16 advanced endoscopy attendings (12.9 %) and six gastroenterology fellows (4.8 %). Almost half of the participants (45.2 %) performed between 20 and 40 colonoscopies per week ( Fig. 1 ). A majority of physicians (54.9 %) had more than 15 years of post-fellowship experience ( Fig. 1 ). The primary practice setting was private practice (51.6 %), while the remainder of the surveyed doctors were in academic practice ( Fig. 1 ). 57.3 % of participants considered themselves “early adopters” for new technologies in gastro-enterology, 67.8 % of gastroenterologists regularly used at least one enhanced imaging technique for polyp detection, most commonly narrow-band imaging (61.3 %), and 67.0 % reported calculating their adenoma detection rate (ADR) in the past 5 years ( Fig. 2 ). Most physicians reported their ADRs to be 20 % to 60 % ( Fig. 2 ). Only 41.9 % of physicians believed that a polyp can be reliably classified as adenomatous or hyperplastic based on itsr endoscopic appearance and only 40.3 % would feel comfortable leaving behind a polyp they thought to be hyperplastic ( Table 1 ).
Fig. 1.
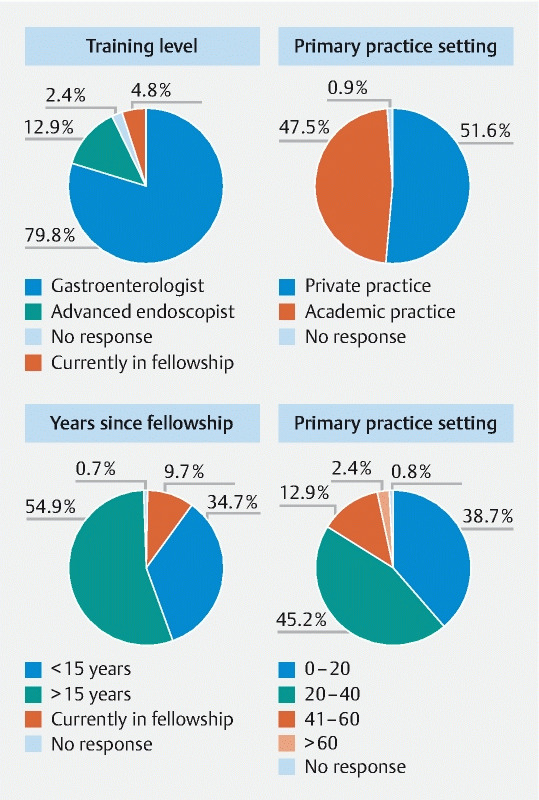
Participant characteristics in percentages, including training, primary practice site, years practicing since fellowship, colonoscopies per week.
Fig. 2.
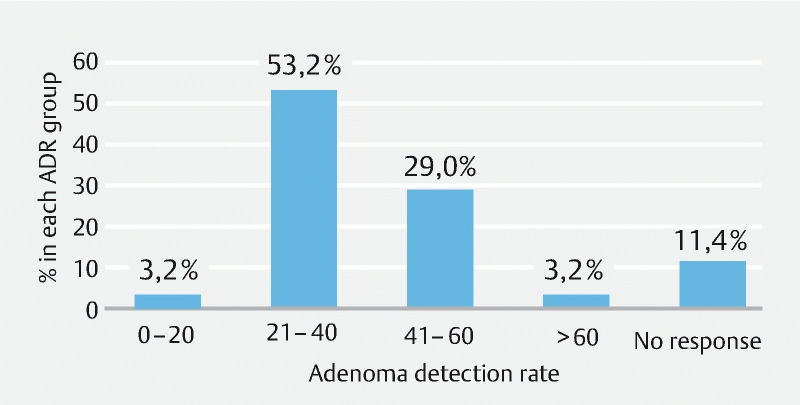
Percentage of participating physicians in each adenoma detection rate group. %, percentage; ADR, adenoma detection rate.
Table 1. Responses to survey questions; academic vs. private practitioners.
| Survey Response | Academic | Private | < 15 years | > 15 years | Overall |
| Interested in new CADe technology | 92.3 % | 82.5 % | 83.8 % | 86.8 % | 85.5 % |
| ADR would increase with CADe | 76.9 % | 71.8 % | 82.1 % | 70.6 % | 75.8 % |
| CADe would increase number of polyps removed | 89.8 % | 73.3 % | 91.1 % | 72.0 % | 80.6 % |
| Endoscopist can reliably classify polyps as hyperplastic vs adenomatous based on endoscopist appearance | 47.5 % | 37.5 % | 46.4 % | 38.2 % | 41.9 % |
| Feel comfortable leaving a hyperplastic polyp | 32.7 % | 45.3 % | 44.6 % | 36.8 % | 40.3 % |
| Feel comfortable leaving a hyperplastic polyp with assistance from AI | 48.0 % | 64.0 % | 55.4 % | 58.8 % | 57.2 % |
| CADe will result in higher patient satisfaction | 45.8 % | 28.1 % | 42.9 % | 30.9 % | 36.3 % |
| CADe will result in higher endoscopist satisfaction | 81.4 % | 48.4 % | 67.9 % | 60.3 % | 63.7 % |
| How important is cost in decision to use CADe | 63.5 % | 87.5 % | 78.6 % | 76.8 % | 77.4 % |
| CADe will prolong the time per colonoscopy | 59.3 % | 67.2 % | 66.1 % | 60.3 % | 62.9 % |
| CADe will increase cost to the practice per procedure | 65.3 % | 81.7 % | 70.4 % | 78.8 % | 75.2 % |
| CADe will increase the total time required per procedure | 57.1 % | 63.4 % | 59.3 % | 62.1 % | 60.3 % |
| Affect the physician-patient relationship | 0.0 % | 0.0 % | 0.0 % | 0.0 % | 0.0 % |
| CADe will cause higher number of false positive detections | 36.5 % | 31.0 % | 38.9 % | 30.3 % | 33.9 % |
| CADe will create operator dependence on the technology | 67.3 % | 56.3 % | 66.7 % | 59.1 % | 62.8 % |
CADe, computer-assisted polyp detection; ADR, adenoma detection rate; AI, artificial intelligence
Perception regarding the benefits of artificial intelligence
Of the participants, 85.5 % reported interest in new technologies to assist in colonic polyp detection ( Table 1 ). A total of 75.8 % agreed that CADe tools would increase their ADR and 80.6 % believed that they would lead to removal of more polyps ( Table 1 ). Many participants (45.6 %) believed that practitioners with a low ADR would benefit the most from this new technology, and 82.0 % of physicians reported that they would be satisfied by technology that increases their ADR by 1 % to 10 %. Although participants were unsure if AI would improve patient satisfaction (46.8 % were neutral), the majority (63.7 %) did believe it would improve endoscopist satisfaction ( Table 1 ).
Academic practice physicians were more likely than private practice physicians to believe that CADe would lead to removal of more polyps (88.5 % vs 73.4 %; P < 0.04), but they were both in agreement that CADe would increase ADR (76.9 % vs. 71.9 %; P = 0.54).
While only 40.3 % of gastroenterologists felt comfortable leaving behind a polyp that they believed to be hyperplastic based on endoscopic appearance, use of a validated CADx tool increased this comfort level to 57.2 % ( P = 0.008).
Perception regarding the barriers to implementation of artificial intelligence
The most common concerns about implementation of AI in gastrointestinal endoscopic procedures were increased cost (75.2 %), operator dependence (62.8 %), and increased procedural time (60.3 %)( Table 1 ). Cost was a significant concern for private practice physicians when compared to academic practice physicians (87.5 % vs. 63.5 %; P = 0.002).
Most physicians (62.9 %) believed that CADe would prolong colonoscopy time, while 77.4 % of physicians felt that cost would be a very important factor when deciding whether to adopt a CADe tool ( Table 1 ).
Univariate analysis
Univariate analysis ( Table 2 ) showed no difference between academic physicians and private practice physicians in expectation that AI would improve ADR between (76.9 % vs 71.9 %; P = 0.5). Univariate analysis showed that academic physicians were more likely than private practice physicians to believe that AI-assisted endoscopy will lead to removal of more polyps (88.5 % vs 73.4 %; P < 0.04).
Table 2. Univariate analysis of whether physicians believe CADe will improve endoscopic performance.
| Factor | Private | N % | Academic | N % | P value |
| Increase adenoma detection rate | 0.5369 | ||||
|
46 | 71.9 | 40 | 76.9 | |
|
18 | 28.1 | 12 | 23.1 | |
| More removed polyps | 0.0436 | ||||
|
47 | 73.4 | 46 | 88.5 | |
|
17 | 26.6 | 6 | 11.5 | |
| Training background | 0.0451 | ||||
|
57 | 91.9 | 41 | 78.9 | |
|
5 | 8.1 | 11 | 21.2 | |
| Average # of colonoscopies per week | < 0.0001 | ||||
|
11 | 17.2 | 33 | 63.5 | |
|
39 | 60.9 | 15 | 28.9 | |
|
14 | 21.9 | 4 | 7.7 | |
| Years in practice after fellowship | < 0.0001 | ||||
|
17 | 26.6 | 35 | 67.3 | |
|
47 | 73.4 | 17 | 32.7 | |
| Teach fellows how to perform colonoscopies | < 0.0001 | ||||
|
60 | 95.2 | 17 | 32.7 | |
|
3 | 4.8 | 35 | 67.3 | |
| Estimated adenoma detection rate | 0.1846 | ||||
|
0 | 0.0 | 3 | 7.3 | |
|
39 | 62.9 | 24 | 58.5 | |
|
22 | 34.4 | 13 | 31.7 | |
|
3 | 4.7 | 1 | 2.5 | |
CADe, computer-aided polyp detection
Gastroenterologists in private practice were more likely than those in academic practice to believe cost is an important factor when adopting AI in their practices (87.5 % vs. 63.5 %; P = 0.002), while physicians in academic practice compared to private practice more often believed that CADe would improve endoscopist satisfaction (81.4 % vs 48.4 %; P < 0.01). When comparing academic physicians to private practice physicians, there was no significant difference in interest in AI (92 % vs 82 %; P = 0.12) or in whether they felt comfortable leaving polyps they believed to be hyperplastic (45.3 % vs. 32.7 %; P = 0.17). When comparing physicians with more than 15 years of post-fellowship experience and those with less than 15 years, there was no significant difference in their interest in AI.
Multivariate analysis
In multivariate analysis, practice setting, years in practice, training level, number of colonoscopies per week, and whether a respondent taught fellows how to perform colonoscopies were not associated with believing that CADe will increase ADR ( Table 3 ).
Table 3. Multivariate logistic regression analysis for improvement in adenoma detection rate by using CADe tools.
| Effect | Odds Ratio | 95 % CI | P Value |
| Practice setting (academic) | 1.36 | (0.32 – 5.81) | 0.6745 |
| Years in practice (≤ 15) | 1.88 | (0.68 – 5.14) | 0.2223 |
| Training (advanced endoscopy fellowship) | 0.59 | (0.15 – 2.38) | 0.4562 |
| Average no. colonoscopies per week | |||
| 0 – 20 vs. > 40 | 1.18 | (0.32 – 4.42) | 0.8031 |
| 21 – 40 vs. > 40 | 1.76 | (0.53 – 5.78) | 0.3547 |
| Teach fellows how to perform colonoscopies (Y) | 2.17 | (0.20 – 2.88) | 0.6757 |
CADe, computer-aided polyp detection
In a multivariate analysis, post-fellowship experience of less than 15 years compared to post-fellowship experience of greater than 15 years was associated with believing that CADe will lead to removal of more polyps (OR = 5.09; P = .01)( Table 4 ).
Table 4. Multivariate logistic regression analysis for removal of more polyps by using CADe tools.
| Effect | Odds Ratio | 95 % CI | P Value |
| Practice setting (academic) | 1.58 | (0.28 – 9.08) | 0.6089 |
| Years in practice (≤ 15) | 5.09 | (1.33 – 19.51) | 0.0177 |
| Training (advanced endoscopy fellowship) | 0.74 | (0.14 – 3.95) | 0.7200 |
| Average no. colonoscopies per week | |||
| 0 – 20 vs. > 40 | 0.64 | (0.14 – 2.95) | 0.5650 |
| 21 – 40 vs. > 40 | 1.28 | (0.33 – 5.02) | 0.7233 |
| Teach fellows how to perform colonoscopies (Y) | 2.55 | (0.29 – 8.35) | 0.6134 |
CADe, computer-aided polyp detection
Discussion
While recent studies have shown that AI holds the potential to improve endoscopic performance with regard to polyp detection and characterization, the pathway toward widespread adoption of new technologies is complex and physician perceptions are likely to play a significant role in the pace of technology adoption in clinical practice. To our knowledge, this study is the first to assess the perceptions of US gastroenterologists regarding AI adoption in endoscopic practice.
Our results demonstrate that AI assistance during colonoscopy is an area of robust interest for practicing gastroenterologists. More than 84 % of surveyed gastroenterologists believed that CADe would improve their endoscopic performance and 75.8 % of gastroenterologists agreed that CADe would increase their ADR. Academic practice physicians were significantly more likely than private practice physicians to believe that CADe would lead to removal of more polyps, although both groups agreed that CADe would increase their ADR. In our multivariate analysis, 15 or less years of post-fellowship experience was associated with believing that CADe will lead to removal of more polyps. It is possible that gastroenterologists with less than 15 years of independent experience have more optimism regarding AI’s ability, which would also explain why they believed CADe would result in higher endoscopist satisfaction. There were no factors associated with the belief that CADe will improve ADR on multivariate analysis, but there was a trend toward statistical significance ( P = 0.14) among gastroenterologists with 15 or less years of post-fellowship experience who believed that CADe would improve ADR.
We chose to compare endoscopists with less than 15 years of post-training experience with more than 15 years of independent experience, given the increasing emphasis on quality indicators, specifically ADR, during the past two decades. In 2002, the United States Multi-Society Task Force on Colorectal Cancer recommended use of ADR which was later re-emphasized in the American Society for Gastrointestinal Endoscopy (ASGE) guidelines published a few years later 12 13 . Of our physician population, 45 % had less than 15 years of post-fellowship experience, and seemed to be more optimistic about the effects of CADe on gastrointestinal performance than those with 15 or more years of independent experience.
CADx is a second important application of AI for colonoscopy, particularly with regard to classifying hyperplastic vs. adenomatous polyps 8 14 . The ASGE PIVI proposals surrounding a “diagnose and leave” strategy for diminutive hyperplastic polyps have been an area of intense discussion for several years, and recent work by Mori and colleagues has promoted use of CADx to support a “diagnose and leave strategy” for diminutive rectosigmoid polyps 8 14 15 . A recent international survey by Willems et al reported that currently 48 % of gastroenterologists felt that leaving diminutive polyps would increase colorectal cancer risk 16 . Similarly, in our survey, only 41.9 % of gastroenterologists agreed that an endoscopist can reliably classify polyps as adenomatous or hyperplastic on endoscopic appearance alone and only 40.3 % of gastroenterologists felt comfortable using a “diagnose and leave” approach for a polyp they believed was hyperplastic. Physicians indicated that if a validated computer CADx tool identified a polyp as hyperplastic, then the level of comfort for “diagnose and leave” only increased to 57.2 %. Therefore, while an accurate CADx tool may provide an additional level of confidence, nearly half of practicing gastroenterologists would still not be comfortable adopting a “diagnose and leave” strategy with CADx support for polyp classification.
The cost of AI technology was also a significant area of concern for gastroenterologists. (75.2 %), especially for private practice physicians compared to academic practice physicians. No studies thus far have looked at the cost associated with AI assistance in colonoscopy screening, and predicted costs for AI products currently in development have not yet been announced or determined. It is worth noting that for other recent technologies shown to improve ADR, including the distal scope tip attachments Endocuff and EndoRings, adoption has been slower than might have been suspected 17 18 . While the specific effect of the incremental cost of these devices on the pattern of clinical adoption has not been evaluated, such devices provide a helpful reference point for expectations surrounding adoption of CADe technology.
Surveyed gastroenterologists also indicated concern with developing operator dependence on CADe and the potential for increased procedural time during screening colonoscopy. Concerns that operator dependence could lead to less skillful and meticulous endoscopic practice have been voiced in the past as potential disadvantages of AI in colonoscopy 19 . Similar concerns have been expressed about the use of automated electrocardiogram analysis and computer-aided detection for mammography, but no evidence of “operator dependence” on these technologies has been reported. Ultimately the most important measure for any new technology in healthcare is whether relevant patient outcomes actually improve, and rigorous prospective studies of CADe in colonoscopy will be the only path forward in this regard. With regards to the effect of AI on colonoscopy procedure duration and efficiency, one prospective study reported an increase in procedure time by 35 to 47 seconds per polyp when applying CADx for polyp classification, but data on the effect of polyp detection (CADe) on procedural duration during colonoscopy have not been reported 8 .
Our study had several limitations. First, our sample of gastroenterologists may not be representative of all US endoscopists because participation was voluntary and sampling was selective. Gastroenterologists interested in AI may have been more inclined to participate in the survey as evidenced by the fact that 67.8 % of gastroenterologists in this study regularly used at least one enhanced imaging technique for polyp detection. However, the survey sample included a similar number of academic and private practice physicians, and post-gastrointestinal fellowship experience was also represented evenly. Another limitation is self-reporting, which lends itself to response and recall bias.
Conclusion
In conclusion, there is strong interest among US gastroenterologists about AI assistance during endoscopic procedures and they believe it would improve their performance, specifically with regard to CADe polyp detection. Gastroenterologists reported less willingness to change practice toward a “diagnose and leave strategy,” using CADx technology for polyp classification. As CADe and CADx tools continue to develop at a rapid pace, we expect that adoption of CADe for colonoscopy in the US gastroenterology community will outpace adoption of CADx.
Footnotes
Competing interests Dr. Berzin is a consultant for Wision AI and Medtronic.
References
- 1.Ruffle J K, Farmer A D, Aziz Q. Artificial intelligence-assisted gastroenterology- promises and pitfalls. Am J Gastroenterol. 2019;114:422–428. doi: 10.1038/s41395-018-0268-4. [DOI] [PubMed] [Google Scholar]
- 2.Ting D SW, Cheung C Y, Lim G et al. Development and validation of a deep learning system for diabetic retinopathy and related eye diseases using retinal images from multiethnic populations with diabetes. JAMA. 2017;318:2211–2223. doi: 10.1001/jama.2017.18152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Esteva A, Kuprel B, Novoa R A et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542:115–118. doi: 10.1038/nature21056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Togashi K. Applications of artificial intelligence to endoscopy practice: The view from Japan Digestive Disease Week 2018. Digest Endosc. 2019;31:270–272. doi: 10.1111/den.13354. [DOI] [PubMed] [Google Scholar]
- 5.Cohen J, Desilets D J, Hwang J H et al. Gastrointestinal Endoscopy Editorial Board top 10 topics: advances in gastrointestinal endoscopy in 2018. Gastrointest Endosc. 2019;90:35–43. doi: 10.1016/j.gie.2019.03.020. [DOI] [PubMed] [Google Scholar]
- 6.Misawa M, Kudo S E, Mori Y et al. Artificial intelligence-assisted polyp detection for colonoscopy: initial experience. Gastroenterology. 2018;154:2027–INF. doi: 10.1053/j.gastro.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 7.Urban G, Tripathi P, Alkayali T et al. Deep Learning localizes and identifies polyps in real time with 96% accuracy in screening colonoscopy. Gastroenterology. 2018;155:1069–INF. doi: 10.1053/j.gastro.2018.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mori Y, Kudo S E, Misawa M et al. Real-time use of artificial intelligence in identification of diminutive polyps during colonoscopy: a prospective study. Annals Internal Med. 2018;169:357–366. doi: 10.7326/M18-0249. [DOI] [PubMed] [Google Scholar]
- 9.Chen P J, Lin M C, Lai M J et al. Accurate classification of diminutive colorectal polyps using computer-aided analysis. Gastroenterology. 2018;154:568–575. doi: 10.1053/j.gastro.2017.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Alagappan M, Brown J RG, Mori Y et al. Artificial intelligence in gastrointestinal endoscopy: The future is almost here. World J Gastrointest Endosc. 2018;10:239–249. doi: 10.4253/wjge.v10.i10.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sarwar S, Dent A, Faust K et al. Physician perspectives on integration of artificial intelligence into diagnostic pathology. NPG Digit Med. 2019;2:28. doi: 10.1038/s41746-019-0106-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rex D K, Bond J H, Winawer S et al. Quality in the technical performance of colonoscopy and the continuous quality improvement process for colonoscopy: recommendations of the U. S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol. 2002;97:1296–1308. doi: 10.1111/j.1572-0241.2002.05812.x. [DOI] [PubMed] [Google Scholar]
- 13.Rex D K, Petrini J L, Baron T H et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2006;63:S16–S28. doi: 10.1016/j.gie.2006.02.021. [DOI] [PubMed] [Google Scholar]
- 14.Kochhar G, Wallace M B. Virtual histology in everyday gastrointestinal endoscopy. Clin Gastroenterol Hepatol. 2018;16:1556–1561. doi: 10.1016/j.cgh.2018.02.045. [DOI] [PubMed] [Google Scholar]
- 15.Abu Dayyeh B K, Thosani N, Konda V et al. ASGE Technology Committee systematic review and meta-analysis assessing the ASGE PIVI thresholds for adopting real-time endoscopic assessment of the histology of diminutive colorectal polyps. Gastrointest Endosc. 2015;81:INF–INF. doi: 10.1016/j.gie.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 16.Willems P, Orkut S, Ditisheim S et al. A239 Clinical management of colorectal polyps: results of an international survey. J Can Assoc Gastroenterol. 2019;2:467–469. [Google Scholar]
- 17.van Doorn S C, van der Vlugt M, Depla A et al. Adenoma detection with Endocuff colonoscopy versus conventional colonoscopy: a multicentre randomised controlled trial. Gut. 2017;66:438–445. doi: 10.1136/gutjnl-2015-310097. [DOI] [PubMed] [Google Scholar]
- 18.Hassan C, Senore C, Manes G et al. Diagnostic yield and miss rate of EndoRings in an organized colorectal cancer screening program: the SMART (Study Methodology for ADR-Related Technology) trial. Gastrointest Endosc. 2019;89:583–INF. doi: 10.1016/j.gie.2018.10.019. [DOI] [PubMed] [Google Scholar]
- 19.Vinsard D G, Mori Y, Misawa M et al. Quality assurance of computer-aided detection and diagnosis in colonoscopy. Gastrointest Endosc. 2019;1:55–63. doi: 10.1016/j.gie.2019.03.019. [DOI] [PubMed] [Google Scholar]


