Abstract
Purpose
Adolescents with opioid use disorder are less likely than adults to receive medication for opioid use disorder (MOUD), yet we know little about facilities that provide adolescents addiction treatment. We sought to describe adolescent-serving addiction treatment facilities in the US and examine associations between facility characteristics and offering MOUD, leading to informed recommendations to improve treatment access.
Methods
This cross-sectional study used the 2017 National Survey of Substance Abuse Treatment Services. Facilities were classified by whether they offered a specialized adolescent program. Covariates included facility ownership, hospital affiliation, insurance/payments, government grants, accreditation/licensure, location, levels of care, and provision of MOUD. Descriptive statistics and logistic regression compared adolescent-serving versus adult-focused facilities, and identified characteristics associated with offering maintenance MOUD.
Results
Among 13,585 addiction treatment facilities in the US, 3,537 (26.0%) offered adolescent programs. Adolescent-serving facilities were half as likely to offer maintenance MOUD as adult-focused facilities (odds ratio, 0.53; 95% confidence interval, 0.49–0.58), which was offered at 23.1% (816) of adolescent-serving versus 35.9% (3,612) of adult-focused facilities. Among adolescent-serving facilities, characteristics associated with increased unadjusted odds of offering maintenance MOUD were non-profit status, hospital affiliation, accepting insurance (particularly, private insurance), accreditation, Northeastern location, or offering inpatient services.
Conclusions and Relevance
The one-quarter of US addiction treatment facilities that serve adolescents are half as likely to provide MOUD as adult-focused facilities, which may explain why adolescents are less likely than adults to receive MOUD. Strategies to increase adolescent access to MOUD may consider insurance reforms/incentives, facility accreditation, and geographically-targeted funding.
Keywords: Opioid Use Disorder, Adolescent, Treatment Facilities, Adolescent Health Services, Substance Abuse Treatment Centers, Medication for addiction treatment, Medication for opioid use disorder, Medication-assisted treatment
INTRODUCTION
Amid rising rates of opioid use disorder (OUD) and opioid overdose,1–5 adolescents remain a group with persistently poor access to treatment for OUD. Despite the evidence-based recommendation that adolescents with OUD receive treatment that includes medication for opioid use disorder (MOUD),6 multiple studies have demonstrated that youth with OUD or who experience opioid overdose are less likely than adults to receive this standard-of-care treatment. In 2014–2015, less than 5% of Medicaid-enrolled adolescents under age 18 who were diagnosed with OUD received timely MOUD, compared to 26.9% of young adults.7 Commercially-insured youth under age 18 have similarly low receipt of MOUD.5 And while 16% of adults receive MOUD within one month of opioid overdose,8 only 1.8% of youth receive MOUD.9 Even among youth who are able to access the addiction treatment system, receipt of MOUD is uncommon, with adolescents in subspecialty treatment for OUD being one-tenth as likely as adults to receive MOUD.10
This disparity in access to treatment for adolescents may substantially exacerbated by the paucity of treatment facilities willing to accept youth and/or provide MOUD. This limited access, in turn, likely reflects both structural barriers and the culture of addiction treatment. To our knowledge there have been no peer-reviewed studies in the last decade examining the characteristics of adolescent-serving addiction treatment facilities as a subset of addiction treatment facilities. Thus, the extent to which addiction treatment facility availability and characteristics contribute to the differential access to MOUD and resultant health inequities for youth is unknown.
This study sought to fill this gap in knowledge, allowing for better understanding of how treatment facility characteristics impact adolescent access to services. Using data from a comprehensive national survey of US addiction treatment facilities, this study’s objectives were to (1) describe the quantity and characteristics of adolescent-serving facilities, and (2) examine associations between facility characteristics and offering maintenance MOUD, leading to informed recommendations to improve treatment access.
METHODS
Study Design and Setting
This cross-sectional study used data from the 2017 National Survey of Substance Abuse Treatment Services (N-SSATS),11 the most recent year of data available at the time of analysis. N-SSATS is an annual survey conducted by the Substance Abuse and Mental Health Services Administration “to collect data on the location, characteristics, and use of alcohol and drug abuse treatment facilities and services throughout the 50 states, the District of Columbia, and other jurisdictions.”12 The 2017 N-SSATS had a response rate of 89% (13,857 of 15,528 eligible facilities); after exclusion of non-treatment halfway houses, solo practitioners, and facilities serving only incarcerated individuals, ultimately 87% of the facilities (13,585) were included in the final N-SSATS data.12 Data were collected between February and December of 2017,12 with the results publicly available in 2018.11 All 13,585 facilities that completed the survey and were included in the final report were analyzed in this study. Study analyses were conducted between January and August 2019. The study was not considered human subjects research by the Johns Hopkins Bloomberg School of Public Health Institutional Review Board.
Study Variable Construction
Facilities were stratified into two mutually exclusive categories by whether they reported offering a specialized program for adolescents. Facilities that self-reported offering a program for adolescents were designated “adolescent-serving,” and facilities without such a program were designated “adult-focused.” The age range for “adolescents” was not specified in the N-SSATS survey, though typically has been considered to be youth under age 18.
Additional facility characteristic covariates included facility ownership (for-profit, non-profit, state/local/tribal government, federal government), hospital affiliation, insurance/payments accepted, acceptance of government grants, accreditation/licensure (by either a state/hospital authority, or a national authority), and location. The categories of payments accepted were condensed to five non-mutually exclusive categories: accepting private insurance, accepting Medicaid, accepting other public insurance (including Medicare, state-financed insurance other than Medicaid, federal military insurance, or Indian Health Service care), offering free or reduced fees (sliding scale or free for those who cannot pay), or accepting only cash/self-pay. The facility location was categorized by state and US census region. For the calculation of odds ratios, a reference category was used for facility ownership and for location. The reference category for facility ownership was private for-profit (thus the odds ratios compare the odds of each other ownership type having the outcome compared to the odds of a private for-profit having the outcome). Similarly for location, northeast US census region was the reference category. For all other odds ratios, the reference category is a facility without that particular characteristic (ie. hospital-affiliated versus not hospital-affiliated; accepting private insurance versus not accepting private insurance).
Facility services covariates included levels of care provided and offering MOUD. Levels of care as defined by the American Society of Addiction Medicine (ASAM) criteria13 were condensed into three variables: inpatient services, residential services, and outpatient services. Facilities reported whether they offered MOUD, and if so, which specific medications, and under what circumstances. A facility was designated as “offering MOUD” if they reported using any of the three US Food & Drug Administration-approved MOUDs (methadone, buprenorphine, extended-release naltrexone) for any circumstance (maintenance, detoxification, or withdrawal after a pre-determined time). Limiting the sample to facilities who reported offering MOUD, facilities were further characterized by types of medication and provision of maintenance versus detoxification only. Facilities were designated as offering “only antagonist MOUD” if they offered only naltrexone (without buprenorphine or methadone). Facilities were designated as offering “any maintenance MOUD” if they reported using any of the three MOUDs for maintenance therapy. Facilities were designated as offering “opioid agonist maintenance MOUD” if they provided either buprenorphine or methadone maintenance. Facilities were designated as offering “only short term opioid agonist MOUD” if they reported using buprenorphine or methadone only for detoxification or required MOUD discontinuation after a pre-determined time.
Statistical Analysis
Descriptive statistics and chi-square tests were used to compare characteristics and services between adolescent-serving and adult-focused facilities. Simple logistic regression was used to identify facility characteristics associated with offering a program for adolescents.
Stratifying by whether the facility was adolescent-serving or adult-focused, descriptive statistics were used to describe characteristics of facilities offering maintenance MOUD. Logistic regression was performed to identify characteristics associated with offering maintenance MOUD; an interaction term was used to test whether the facility characteristic associated with offering MOUD differed between adolescent-serving and adult-focused facilities. No additional analyses were performed for interactions found to be significant, as the goals of these main analyses were to describe the associations as they exist in this near universal representation of treatment facilities, rather than adjust for multiple associations in a sample of facilities. As a sensitivity analysis, multivariable logistic regression was performed (presented in Appendix B) including all covariates selected a priori; we calculated variance inflation ratios to check for collinearity. The stratified multivariable model with all covariates was used to provide regression-adjusted probabilities for the availability of maintenance MOUD (Appendix C).
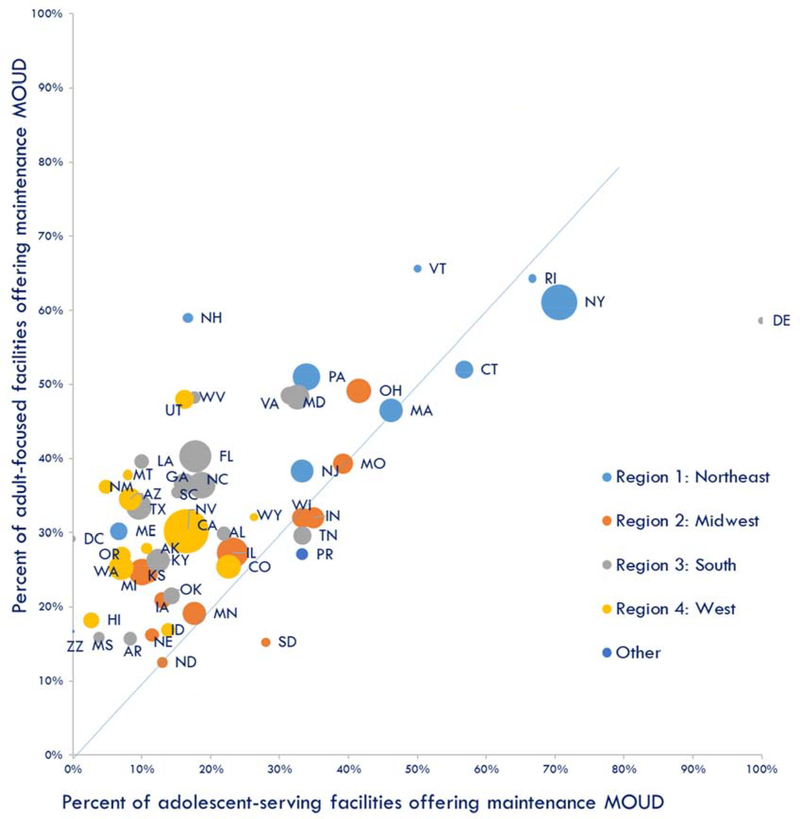
Last, the association between state-level availability of maintenance MOUD for youth versus adults was examined by creating a scatterplot of the proportion of adolescent-serving facilities per state that offer maintenance MOUD versus the proportion of adult-focused facilities per state that offer maintenance MOUD, and calculating a weighted correlation coefficient.
Analyses were conducted using STATA IC Version 15 (StataCorp, College Station, TX). The scatterplot was generated using Microsoft Excel 2016 (Microsoft Corporation, Redmond, WA). All statistical tests were two-sided and considered significant at p<0.05.
RESULTS
Characteristics Associated with Adolescent Programs
Of 13,585 total facilities included in the 2017 N-SSATS, 3,537 (26.0%) reported offering a program for adolescents (“adolescent-serving facilities”); the remaining 10,048 (74.0%) facilities did not offer programs for adolescents (“adult-focused facilities”). Table 1 displays characteristics of the overall sample of all adolescent-serving and adult-focused facilities. Adolescent-serving facilities were more likely than adult-focused facilities to be owned by a non-profit or state/local/tribal government, accept insurance or offer free & reduce services, or receive government grants. Conversely, adult-focused facilities were more likely than adolescent-serving facilities to be owned by a for-profit or the federal government, be affiliated with a hospital, accept cash only, or be accredited by a national authority.
Table 1.
Characteristics of overall sample of 13,585 adult-focused and adolescent-serving facilities
| Characteristic | Adult-focused facilities N (Column %) | Adolescent-serving facilities N (Column %) | p value | ORa for offering program for adolescents (95% CI) |
|---|---|---|---|---|
| All facilities | 10048 (74.0%) | 3537 (26.0%) | ||
| Facility ownership | ||||
| Private for-profit | 3790 (37.7%) | 1141 (32.3%) | <0.001 | Ref |
| Private non-profit | 5169 (51.4%) | 1994 (56.4%) | 1.28 (1.18, 1.39) | |
| State/local/tribal gov | 813 (8.1%) | 389 (11.0%) | 1.59 (1.38, 1.82) | |
| Federal gov | 276 (2.7%) | 13 (0.4%) | 0.16 (0.09, 0.27) | |
| Hospital-affiliated | 1040 (10.4%) | 235 (6.6%) | <0.001 | 0.62 (0.53, 0.71) |
| Payment/insurances accepted | ||||
| Private insurance | 6786 (68.6%) | 2745 (78.5%) | <0.001 | 1.67 (1.52, 1.83) |
| Medicaid | 6045 (61.3%) | 2640 (75.5%) | <0.001 | 1.94 (1.78, 2.12) |
| Other public insurance | 6108 (61.2%) | 2571 (73.1%) | <0.001 | 1.72 (1.58, 1.87) |
| Free & reduced fees | 6926 (68.9%) | 2812 (79.5%) | <0.001 | 1.75 (1.60, 1.92) |
| Cash & self-pay only | 597 (5.9%) | 53 (1.5%) | <0.001 | 0.24 (0.18, 0.32) |
| Accepts government grants | 5130 (53.1%) | 2108 (61.7%) | <0.001 | 1.42 (1.31, 1.54) |
| Certification, licensing, or accreditation | ||||
| By state/hospital authority | 9020 (89.8%) | 3153 (89.1%) | 0.29 | 0.94 (0.83, 1.06) |
| By national authority | 5226 (52.0%) | 1703 (48.1%) | <0.001 | 0.86 (0.79, 0.93) |
| US census regions | ||||
| 1 : Northeast | 2021 (20.1%) | 584 (16.5%) | <0.001 | Ref |
| 2: Midwest | 2426 (24.1%) | 862 (24.4%) | 1.23 (1.09, 1.39) | |
| 3: South | 2993 (29.8%) | 990 (28.0%) | 1.14 (1.02, 1.29) | |
| 4: West | 2517 (25.0%) | 1088 (30.8%) | 1.50 (1.33, 1.68) | |
| Other/territories | 91 (0.9%) | 13 (0.4%) | 0.49 (0.27, 0.89) | |
Odds Ratio reference category for facility ownership type was private for-profit status (thus the odds ratios are the odds of each other ownership type offering an adolescent program compared to the odds of a private for-profit offering a program for adolescents). Similarly for US census regions, northeast location was the reference category. For all other odds ratios, the reference category is a facility without that particular characteristic (ie. hospital-affiliated vs. not hospital-affiliated; accepting private insurance vs. not accepting private insurance).
Table 2 displays services offered by the overall sample of all adolescent-serving and adult-focused facilities. Among the 3,537 adolescent-serving facilities, 23.1% (816, or 6% of all 13,585 facilities in the US) offered maintenance MOUD, compared to 35.9% (3,612) of adult-focused facilities (odds ratio [OR], 0.53; 95% confidence interval [CI], 0.49–0.58). While adolescent-serving and adult-focused facilities were equally likely to offer the opioid antagonist naltrexone as their only MOUD (OR, 0.92; 95% CI, 0.79–1.08), adolescent-serving facilities were approximately half as likely to offer opioid agonist maintenance MOUD (OR, 0.51; 95% CI, 0.46–0.57), with only 15% (531) of adolescent-serving facilities offering this compared to 25.6% (2,574) of adult-focused facilities. Of adolescent-serving facilities, 92.4% (3,267) offered outpatient treatment, 11.7% (413) offered residential treatment, and 3.6% (129) offered inpatient treatment.
Table 2.
Services offered at 13,585 adult-focused and adolescent-serving facilities
| Service Offered | Adult-focused facilities N (Column %) | Adolescent-serving facilities N (Column %) | p value | ORa for offering program for adolescents (95% CI) |
|---|---|---|---|---|
| All facilities | 10048 (74.0%) | 3537 (26.0%) | ||
| Medications offered | ||||
| Offers any MOUDb | 4474 (44.5%) | 1009 (28.5%) | <0.001 | 0.50 (0.46, 0.54) |
| Offers only short term opioid agonist MOUDb | 610 (6.1%) | 106 (3.0%) | <0.001 | 0.48 (0.39, 0.59) |
| Offers any maintenance MOUDb | 3612 (35.9%) | 816 (23.1%) | <0.001 | 0.53 (0.49, 0.58) |
| Offers opioid agonist maintenance MOUDb | 2574 (25.6%) | 531 (15.0%) | <0.001 | 0.51 (0.46, 0.57) |
| Offers only antagonist MOUDb | 698 (6.9%) | 228 (6.4%) | 0.31 | 0.92 (0.79, 1.08) |
| Levels of care | ||||
| Inpatient services | 586 (5.8%) | 129 (3.6%) | <0.001 | 0.61 (0.50, 0.74) |
| Residential services | 2712 (27.0%) | 413 (11.7%) | <0.001 | 0.36 (0.32, 0.40) |
| Outpatient services | 7917 (78.8%) | 3267 (92.4%) | <0.001 | 3.26 (2.85, 3.72) |
Odds Ratio reference category is a facility without that particular characteristic (ie. facility offering any MOUD vs. facility not offering any MOUD; facility offering inpatient services vs. facility not offering inpatient services).
Medication for Opioid Use Disorder (MOUD)
Characteristics Associated with offering Maintenance MOUD
Table 3 shows characteristics of facilities that offer maintenance MOUD stratified by whether they were adolescent-serving or adult-focused; this table displays the number and percent of facilities with each characteristic, and the unadjusted odds ratio for offering maintenance MOUD by each characteristic. Table 3 also shows the p-value testing for a difference in this association between adult versus adolescent facilities, derived from an interaction term in an unadjusted logistic regression model (see Appendix A) that included separate terms for adolescent-serving, the particular characteristic, and their interaction. Facility ownership type was significantly associated with the odds of providing maintenance MOUD, and this relationship significantly differed between adolescent-serving and adult-focused facilities: among adolescent-serving facilities, non-profits were 1.4 times more likely (OR, 1.37; 95% CI, 1.14–1.63) than for-profits to offer maintenance MOUD, whereas among adult-focused facilities, non-profits were approximately half as likely (OR, 0.58; 95% CI, 0.53–0.63) as for-profits to offer maintenance MOUD. Hospital-affiliation was associated with increased odds of offering maintenance MOUD in both adolescent-serving facilities (OR, 3.55; 95% CI, 2.72–4.65) and adult-focused facilities (OR, 2.45; 95% CI, 2.15–2.79), though the relationship was stronger among adolescent-serving facilities. Facilities that accepted any kind of insurance, particularly private insurance, were significantly more likely to provide maintenance MOUD than those not accepting insurance, or those offering free and reduced fee services. Adolescent-serving facilities that were certified, licensed, or accredited by a state/hospital, or a national authority were more likely to offer maintenance MOUD than unaccredited facilities; the association of national accreditation with offering maintenance MOUD was even stronger among adult-focused facilities. Both adolescent-serving and adult-focused facilities in the Midwest, South, and West were less likely to provide maintenance MOUD versus facilities in the Northeast; this negative association was strongest among adolescent-serving facilities in the South and West. Lastly, adolescent-serving facilities offering inpatient services were more likely (OR, 3.59; 95% CI, 2.52–5.12) to offer maintenance MOUD than facilities without this level of care; this association held but was less strong among adult-focused facilities (OR, 1.76; 95% CI, 1.49–2.08).
Table 3.
Number and percent of adult-focused and adolescent-serving facilities that offer maintenance medication for opioid use disorder (MOUD) by facility characteristic,a unadjusted odds of offering maintenance MOUD, and test for difference between adult-focused versus adolescent-serving facilities.
| Adult-focused facilities | Adolescent-serving facilities | Test for difference between adult and adolescent facilitiesc | |||
|---|---|---|---|---|---|
| N (Row %) | Unadjusted ORb for maintenance MOUD (95% CI) | N (Row %) | Unadjusted ORb for maintenance MOUD (95% CI) | p-value | |
| All facilities | 3612 (35.9%) | 816 (23.1%) | |||
| Facility ownership | |||||
| Private for-profit | 1617 (42.7%) | Ref | 226 (19.8%) | Ref | |
| Private non-profit | 1557 (30.1%) | 0.58 (0.53, 0.63) | 503 (25.2%) | 1.37 (1.14, 1.63) | <0.001 |
| State/local/tribal gov | 252 (31.0%) | 0.60 (0.51, 0.71) | 85 (21.9%) | 1.13 (0.85, 1.50) | <0.001 |
| Federal gov | 186 (67.4%) | 2.78 (2.14, 3.60) | 2 (15.4%) | 0.74 (0.16, 3.34) | 0.09 |
| Hospital-affiliated | 577 (55.5%) | 2.45 (2.15, 2.79) | 115 (48.9%) | 3.55 (2.72, 4.65) | 0.02 |
| Payment/insurances accepted | |||||
| Private insurance | 2709 (39.9%) | 1.73 (1.58, 1.90) | 765 (27.9%) | 5.92 (4.34, 8.07) | <0.001 |
| Medicaid | 2377 (39.3%) | 1.47 (1.35, 1.60) | 684 (25.9%) | 2.06 (1.67, 2.54) | 0.003 |
| Other public insurance | 2339 (38.3%) | 1.29 (1.19, 1.41) | 681 (26.5%) | 2.26 (1.85, 2.78) | <0.001 |
| Free & reduced fees | 2200 (31.8%) | 0.56 (0.52, 0.61) | 616 (21.9%) | 0.73 (0.61, 0.89) | 0.01 |
| Cash & self-pay only | 248 (41.5%) | 1.29 (1.09, 1.52) | 7 (13.2%) | 0.50 (0.23, 1.12) | 0.02 |
| Accepts government grants | 1628 (31.7%) | 0.68 (0.63, 0.74) | 479 (22.7%) | 0.97 (0.82, 1.14) | <0.001 |
| Certification, licensing, or accreditation | |||||
| By state/hospital authority | 3227 (35.8%) | 0.93 (0.81, 1.06) | 762 (24.2%) | 1.95 (1.44, 2.63) | <0.001 |
| By national authority | 2684 (51.4%) | 4.43 (4.05, 4.85) | 478 (28.1%) | 1.73 (1.47, 2.02) | <0.001 |
| US census regions | |||||
| 1: Northeast | 1034 (51.2%) | Ref | 285 (48.8%) | Ref | |
| 2: Midwest | 708 (29.2%) | 0.39 (0.35, 0.45) | 208 (24.1%) | 0.33 (0.27, 0.42) | 0.21 |
| 3: South | 1082 (36.2%) | 0.54 (0.48, 0.61) | 182 (18.4%) | 0.24 (0.19, 0.30) | <0.001 |
| 4: West | 764 (30.4%) | 0.42 (0.37, 0.47) | 137 (12.6%) | 0.15 (0.12, 0.19) | <0.001 |
| Other/territories | 24 (26.4%) | 0.34 (0.21, 0.55) | 4 (30.8%) | 0.47 (0.14, 1.53) | 0.64 |
| Levels of care provided | |||||
| Inpatient | 286 (48.8%) | 1.76 (1.49, 2.08) | 65 (50.4%) | 3.59 (2.52, 5.12) | <0.001 |
| Residential | 841 (31.0%) | 0.74 (0.67, 0.81) | 93 (22.5%) | 0.97 (0.76, 1.23) | 0.048 |
| Outpatient | 3044 (38.4%) | 1.72 (1.55, 1.91) | 759 (23.2%) | 1.13 (0.83, 1.53) | 0.01 |
Chi-square p-value statistically significant at <0.05 for all bolded OR’s
Odds Ratio reference category for facility ownership type was private for-profit status (thus the odds ratios are the odds of each other ownership type offering an maintenance MOUD compared to the odds of a private for-profit offering maintenance MOUD). Similarly for US census regions, northeast location was the reference category. For all other odds ratios, the reference category is a facility without that particular characteristic (ie. Hospital-affiliated vs. not hospital-affiliated; accepting private insurance vs. not accepting private insurance).
P-Value is derived from an interaction coefficient in an unadjusted logistic regression model that included separate terms for adolescent-serving, the particular characteristic, and their interaction; this allowed for testing whether the association with the particular characteristic differed between adolescent-serving and adult-focused facilities. No additional analyses were performed for interactions found to be significant, as the goal was to describe associations as they exist in this near universal representation of treatment facilities.
Appendix B displays the results of the sensitivity analysis demonstrating adjusted odds ratios for offering maintenance MOUD by facility characteristic; the results are substantially similar to the unadjusted model with the exception of a change in the coefficient for cash &self-pay adolescent-serving facilities. Checks for collinearity were negative, with all variance inflation ratios under 2.5. Appendix C demonstrates the regression-adjusted percent of facilities offering maintenance MOUD by facility characteristic. This table demonstrates that after adjusting for all facility characteristics, 35.3% (95% CI, 34.4%−36.2%) of adult-focused facilities provide maintenance MOUD versus 22.8% (95% CI, 21.3%−24.3%) of adolescent-serving facilities, similar to percentages in the unadjusted analyses.
State-Level Availability of Maintenance MOUD
Figure 1 displays a scatterplot of the percent of facilities with versus without adolescent programs that offer maintenance MOUD by state and US census region (R2 = 0.4676). Most Northeast states (8 of 9; 89%) were clustered in the top-right quadrant with the highest percentages of both adolescent- and adult-serving facilities providing maintenance MOUD. Conversely, most Midwest (7 of 12; 58%) and Southern states (15 of 17; 88%) and all Western states (13 of 13; 100%) fell above the line of symmetry, with a higher percent of adult-focused facilities offering maintenance MOUD in these states compared to adolescent-serving facilities.
Figure 1. Scatterplot of the percent of adolescent-serving vs adult-focused facilities that offer maintenance medication for opioid use disorder (MOUD), by state.
* Size of dots proportional to number of facilities per state
* The 45 degree line represents the line of symmetry; states that fall above this line have a higher percentage of adult-serving facilities that offer MOUD than youth-serving facilities
DISCUSSION
In this comprehensive study of 13,585 US addiction treatment facilities, only one-quarter offered programs for adolescents in 2017. Of these adolescent-serving facilities, only 3.6% and 11.7% offered inpatient or residential services, respectively. Adolescent-serving facilities were half as likely as adult-focused facilities to offer any maintenance MOUD, with only 6% of all U.S. facilities offering both programs for adolescents and maintenance MOUD. Among adolescent-serving facilities, characteristics associated with increased unadjusted odds of offering maintenance MOUD were non-profit status, hospital-affiliation, accepting insurance (particularly, private insurance), accreditation, Northeast location, or offering inpatient services.
This study contributes several key findings and possible targets for policy approaches. First, to our knowledge this study is the first in the last decade to fully describe the paucity of addiction treatment facilities available to adolescents throughout the US. Youth who require a higher level of care (residential or inpatient services) based on the ASAM treatment criteria guidelines13 may not be able to access such services given the limited number of adolescent-serving treatment facilities, with only 413 residential facilities for youth in the US versus 2712 residential facilities for adults. Priority investment in increasing the number of beds for youth may be necessary to improve access to higher levels of care for adolescents.
Second, this study demonstrates that in addition to the relatively few treatment facilities available for adolescents, it may be even harder for youth to access MOUD because adolescent-serving facilities are half as likely to offer MOUD as adult-focused facilities. While prior literature has explored the availability of MOUD throughout the country, to our knowledge, this is the first study specifically examining how this may differ among adolescent-serving facilities. The patterns of poor MOUD availability in adolescent-serving facilities found in this study is likely the result of combined societal and financial factors. Beliefs against using medication have been able to persist due to the longstanding separation of addiction treatment from mainstream medicine resulting in a tension between a medical model of illness versus a recovery model.14–17 This widespread stigma against MOUD within the healthcare and recovery communities sometimes results in MOUD being inaccurately viewed as “replacing one drug with another,”14 with a failure to recognize the chronic illness nature of OUD and the substantial effectiveness of medication.14–17 This stigma may be even stronger regarding prescribing adolescents MOUD, where a common view is that “medications should be used as a last resort,”17 despite evidence-based guidelines from the American Academy of Pediatrics that recommend its use.6 The bias against prescribing opioid agonists (buprenorphine and methadone) in particular to adolescents may be evidenced by adolescent-serving facilities being half as likely as adult-focused facilities to offer opioid agonists, yet equally likely to offer only the opioid-antagonist naltrexone. While it is unclear from this study whether these facilities are actually providing naltrexone to adolescents, the irony is that naltrexone is not FDA-approved for adolescents under 18 due to insufficient pediatric data.18 Anti-MOUD views may be impacting the availability of MOUD both through individual facilities choosing to not offer MOUD, or through wider state-level policymaking and Medicaid restrictions.19 Moreover, there is an insufficient number of youth-serving MOUD prescribers, with only a small number of pediatricians waivered to prescribe buprenorphine;20 this could be improved by targeting youth-serving providers in educational and stigma-reduction campaigns as well as federal funding efforts to train MOUD providers.21,22
Third, this study suggests several underlying financial and reimbursement-based factors that may be contributing to the availability of MOUD, which may also stem from the fragmentation of behavioral health service financing from other medical services.16 Some of the associations found in this study were universal to both adolescent-serving and adult-focused facilities, including the increased likelihood of MOUD provision among facilities that were hospital-affiliated, licensed/certified/accredited, or accepted insurance. Prior studies not distinguishing between adolescent-serving and adult-focused facilities found similar associations of MOUD being more common among facilities that were hospital-affiliated, accredited, or accepted insurance, and less common among those offering free/reduced-fee services.23,24
It is thus useful to know that these associations remain true among adolescent-serving facilities, such that broad-based policy approaches designed to target these associations could also benefit adolescents. The positive association of accreditation with MOUD has led to the recommendation that licensing/accreditation can be leveraged as tools to increase facility provision of evidence-based MOUD through quality improvement initiatives, incentivizing innovation, and standard-setting.24 Regarding the role of insurance, substantial research has been performed specifically evaluating the role of Medicaid in the availability of MOUD. Many state Medicaid plans have medication restrictions and utilization controls such as requirements for prior authorizations, or “fail-first” restrictions that require proof of a patient having failed other therapies before approving medications.25,26 Multiple studies have demonstrated that facilities located in states with more stringent Medicaid restrictions/utilization controls are less likely to accept Medicaid,27 and those that do accept Medicaid are less likely to offer MOUD than facilities in states with more comprehensive Medicaid coverage.19,23 Facilities may view these Medicaid or private insurance restrictions and procedures as too great a barrier and an unprofitable process, and thus may choose to not offer MOUD.19 These strong associations demonstrate that state-level Medicaid policies may have a substantial impact upon facilities’ choices regarding services offered; liberalizing restrictions might result in significant improvement in the availability of MOUD.24,27 Access to MOUD for youth with Medicaid could be improved by including MOUD in the early periodic screening, detection, and treatment (EPSDT) benefits that all state Medicaid plans must cover.10,28
This study also elucidates important differences between the adolescent-serving and adult-focused facilities. While prior studies have found greater MOUD prescribing among for-profit facilities compared to non-profits,23,24 this study demonstrates that this association holds true only among adult-focused facilities, whereas among adolescent-serving facilities, non-profits were more likely than for-profits to offer MOUD. Similarly, while cash-only adolescent-serving facilities are less likely to provide MOUD, cash-only adult-focused facilities are more likely to provide MOUD. Future research should seek to understand this difference in the apparent profitability of MOUD in order to inform strategies to improve youth access to MOUD, which may include ensuring parity in insurance reimbursement for all ages, and lifting fail-first restrictions on certain medications for youth.
Lastly, this study points to several key disparities for certain youth with OUD in accessing care. Because facilities that offer free and reduced fee services are less likely to provide MOUD, adolescents who are uninsured or underinsured face even poorer access to MOUD than other youth. This inequity leaves some of the most vulnerable youth unable to receive the care they need, or might be able to get with more financial resources. This raises concern for violation of the fundamental right of all to the “highest attainable standard of health and to facilities for the treatment of illness” as described in the United Nations Convention on the Rights of the Child.29 Similarly, the inequality in MOUD provision among Northeastern states compared to Southern, Midwestern, and Western states is striking: facilities in Southern states are 80% less likely than Northeastern facilities to provide medication. This geographic variation observed is congruent with what has been previously described in the literature regarding overall access to MOUD, with many counties (particularly rural counties) in the Midwest and South having no available Medicaid-accepting MOUD providers or facilities.30 Thus it may be necessary to target these specific areas of the country for priority funding, insurance reforms, recruitment of youth-serving addiction providers, and incorporation of adolescent-friendly services31 at traditionally adult-focused facilities.
Limitations
There were several limitations to this study. First, while the N-SSATS represents a near universal capture of treatment facilities throughout the U.S., it does not include office-based provision of buprenorphine, and thus likely underestimates the full availability of MOUD.23 However, given that only a small number of pediatricians are waivered to prescribe buprenorphine,20 the number of adolescent-serving office-based MOUD providers not included in N-SSATS is likely very small.22 Second, N-SSATS is a self-report survey, thus there is no external verification of the answers provided by the addiction treatment facilities regarding their characteristics and the services they offer. It is possible that facilities reporting the provision of MOUD may not in fact offer these services, or do so only rarely; the same is possible for other services such as offering programs for adolescents. Thus these findings likely represent a more optimistic view than what is available in reality.
CONCLUSION
This large study of addiction treatment centers throughout the US demonstrates that adolescents have less access than adults to standard-of-care addiction treatment, and specifically to inpatient or residential levels of care, or to MOUD. This is especially true of adolescents who rely on free and reduced fee services, or who live in the US South and West. This study may explain why adolescents are considerably less likely than adults to receive MOUD by demonstrating that the few facilities that serve them are significantly less likely to provide MOUD. Based on the results of this study, strategies to increase access to addiction treatment to youth may consider possible mechanisms including insurance reforms and incentives, facility accreditation, and geographically-targeted funding.
Supplementary Material
IMPLICATIONS AND CONTRIBUTIONS.
1 in 4 addiction treatment facilities in the US serve adolescents <18 years. Compared to facilities that only offer adult services, adolescent-serving facilities were half as likely to provide medications for opioid use disorder (MOUD), likely contributing to why adolescents are less likely than adults to receive MOUD.
Acknowledgements
Dr. Alinsky was supported by T32HD052459 (NIH/NICHD)
Dr.Hadland was supported by K23DA045085 (NIH/NIDA), L40DA042434 (NIH/NIDA), the Thrasher Research Fund Early Career Award, and the Academic Pediatric Association Young Investigator Award
Dr. Matson was supported by K01DA035387 (NIH/NIDA)
Dr. Cerda was supported by 1R01DA045872-01A1 (NIH/NIDA)
Dr. Saloner was supported by K01DA042139-01A1 (NIH/NIDA)
Funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Abbreviations
- OUD
Opioid Use Disorder
- MOUD
Medications for Opioid Use Disorder
- N-SSATS
National Survey of Substance Abuse Treatment Services
- ASAM
American Society of Addiction Medicine
Footnotes
Conflict of Interest Statement
The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Unick GJ, Rosenblum D, Mars S, Ciccarone D. Intertwined Epidemics: National Demographic Trends in Hospitalizations for Heroin- and Opioid-Related Overdoses, 1993–2009. PLoS One. 2013;8(2). doi: 10.1371/journal.pone.0054496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Murthy VH. Surgeon General’s Report on Alcohol, Drugs, and Health. Washington, DC; 2016. doi: 10.1001/jama.2016.18215 [DOI] [PubMed] [Google Scholar]
- 3.Gaither JR, Leventhal JM, Ryan SA, Camenga DR. National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr. 2016;170(12):1195–1201. doi: 10.1001/jamapediatrics.2016.2154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaither JR, Shabanova V, Leventhal JM. US National Trends in Pediatric Deaths From Prescription and Illicit Opioids, 1999–2016. JAMA Netw Open. 2018;1(8):e186558. doi: 10.1001/jamanetworkopen.2018.6558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hadland SE, Frank Wharam JW, Schuster MA, Zhang F, Samet JH, Larochelle MR. Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA Pediatr. 2017;171(8):747–755. doi: 10.1001/jamapediatrics.2017.0745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Committee on Substance Use and Prevention. Medication-Assisted Treatment of Adolescents With Opioid Use Disorders. Pediatrics. 2016;138(3):e20161893–e20161893. doi: 10.1542/peds.2016-1893 [DOI] [PubMed] [Google Scholar]
- 7.Hadland SE, Bagley SM, Rodean J, et al. Receipt of Timely Addiction Treatment and Association of Early Medication Treatment With Retention in Care Among Youths With Opioid Use Disorder. JAMA Pediatr. 2018;172(11):1029–1037. doi: 10.1001/jamapediatrics.2018.2143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ali MM, Mutter R. Patients Who Are Privately Insured Receive Limited Follow-Up Services After Opioid-Related Hospitalizations. Rockville, MD: Substance Abuse and Mental Health Services Administration (US), Center for Behavioral Health Statistics and Quality; 2016. http://www.ncbi.nlm.nih.gov/pubmed/27054227. [PubMed] [Google Scholar]
- 9.Alinsky RH, Zima BT, Rodean J, et al. Receipt of Addiction Treatment after Opioid Overdose among Medicaid-Enrolled Adolescents and Young Adults. JAMA Pediatr. January 2020:e195183. doi: 10.1001/jamapediatrics.2019.5183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feder KA, Krawczyk N, Saloner B. Medication-Assisted Treatment for Adolescents in Specialty Treatment for Opioid Use Disorder. J Adolesc Heal. 2017;60(6):747–750. doi: 10.1016/j.jadohealth.2016.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Substance Abuse and Mental Health Services Administration. DASIS: Drug & Alcohol Services Information; https://wwwdasis.samhsa.gov. Accessed April 2, 2019. [Google Scholar]
- 12.Substance Abuse and Mental Health Services Administration. National Survey of Substance Abuse Treatment Services (N-SSATS): 2017. Data on Substance Abuse Treatment Facilities. Rockville, MD; 2018. https://wwwdasis.samhsa.gov/dasis2/nssats/2017_nssats_rpt.pdf. Accessed July 4, 2019. [Google Scholar]
- 13.Mee-Lee D, Shulman GD, Fishman MJ, et al. The ASAM Criteria: Treatment Criteria for Addictive, Substance-Related, and Co-Occurring Conditions. Third Edit. (Mee-lee D, ed.). Chevy Chase, MD: American Society of Addiction Medicine [Google Scholar]
- 14.Wakeman SE. Using Science to Battle Stigma in Addressing the Opioid Epidemic: Opioid Agonist Therapy Saves Lives. Am J Med. 2016;129(5):455–456. doi: 10.1016/j.amjmed.2015.12.028 [DOI] [PubMed] [Google Scholar]
- 15.Olsen Y, Sharfstein JM. Confronting the Stigma of Opioid Use Disorder — and Its Treatment. 2014;21218. doi: 10.1001/jama.2014.2147.Conflict [DOI] [PubMed] [Google Scholar]
- 16.National Academies of Sciences Engineering and Medicine. Ending Discrimination Against People with Mental and Substance Use Disorders. National Academies Press; 2016. doi: 10.17226/23442 [DOI] [PubMed] [Google Scholar]
- 17.Bagley SM, Hadland SE, Carney BL, Saitz R. Addressing Stigma in Medication Treatment of Adolescents with Opioid Use Disorder. J Addict Med. 2017;11(6):415–416. doi: 10.1097/ADM.0000000000000348 [DOI] [PubMed] [Google Scholar]
- 18.Food and Drug Administration. Labeling-Medication Guide: VIVITROL (naltrexone for extended-release injectable suspension), for intramuscular use. https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/021897s045lbl.pdf. Published 2019. Accessed September 12, 2019.
- 19.Andrews CM, Abraham AJ, Grogan CM, Westlake MA, Pollack HA, Friedmann PD. Impact of Medicaid Restrictions on Availability of Buprenorphine in Addiction Treatment Programs. 2019;109(3):2018–2020. doi: 10.2105/AJPH.2018.304856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosenblatt RA, Andrilla CHA, Catlin M, Larson EH. Geographic and Specialty Distribution of US Physicians Trained to Treat Opioid Use Disorder. Ann Fam Med. 2015;13(1):23–26. doi: 10.1370/afm.1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Saloner B, Feder KA, Krawczyk N. Closing the medication-assisted treatment gap for youth with opioid use disorder. JAMA Pediatr. 2017;171(8):729–731. doi: 10.1001/jamapediatrics.2017.1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hadland SE, Wood E, Levy S. How the paediatric workforce can address the opioid crisis. Lancet. 2016;388(10051):1260–1261. doi: 10.1016/S0140-6736(16)31573-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mojtabai R, Mauro C, Wall MM, Barry CL, Olfson M. Medication Treatment For Opioid Use Disorders In Substance Use Treatment Facilities. Health Aff. 2019;38(1):14–23. doi: 10.1377/hlthaff.2018.05162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Heinrich CJ, Cummings GR. Adoption and diffusion of evidence-based addiction medications in substance abuse treatment. Health Serv Res. 2014;49(1):127–152. doi: 10.1111/1475-6773.12093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.American Society of Addiction Medicine. Advancing Access to Addiction Medications: Implications for Opioid Addiction Treatment. Rockville, MD; 2013. https://www.asam.org/docs/default-source/advocacy/advancing-access-to-addiction-medications-report.pdf?sfvrsn=2aa870c2_0. [Google Scholar]
- 26.Legal Action Center. Confronting an Epidemic: The Case for Eliminating Barriers to Medication- Assisted Treatment of Heroin and Opioid Addiction. 2015;(March). www.lac.org.
- 27.Andrews CM, Grogan CM, Westlake MA, et al. Do benefits restrictions limit Medicaid acceptance in addiction treatment ? Results from a national study. J Subst Abuse Treat. 2018;87:50–55. doi: 10.1016/j.jsat.2018.01.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wachino V, Hyde PS. Coverage of Behavioral Health Service for Youth with Substance Use Disorders; 2015. https://www.medicaid.gov/federal-policy-guidance/downloads/cib-01-26-2015.pdf. Accessed November 19, 2019.
- 29.MacPherson S The Convention on the Rights of the Child. Soc Policy Adm. 1989;23(1):99–101. doi: 10.1111/j.1467-9515.1989.tb00500.x [DOI] [Google Scholar]
- 30.Haffajee RL, Lin LA, Bohnert ASB, Goldstick JE. Characteristics of US Counties With High Opioid Overdose Mortality and Low Capacity to Deliver Medications for Opioid Use Disorder. 2019;2(6):1–15. doi: 10.1001/jamanetworkopen.2019.6373 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.World Health Organization. Making Health Services Adolescent Friendly: Developing National Quality Standards for Adolescent Friendly Health Services. Geneva, Switzerland; 2012. doi:ISBN 978 92 4 150359 4 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.