Abstract
Objective:
Nutrition backlash is a disposition defined by negative feelings about dietary recommendations. Past research has measured nutrition backlash using the nutrition backlash scale (NBS), and found that it is negatively related to fruit and vegetable consumption. The present study examined several aspects of the NBS, including factor structure, discriminant validity, and relationship to demographics and health behaviors.
Research Methods & Procedures:
Adults were recruited to participate in two studies. Study 1 (N = 480) included measures of nutritional backlash, information overload, worry, fatalism, and nutrition-related behaviors. Study 2 (N = 399) was a follow-up that examined the factor structure of the NBS in a separate sample.
Results:
In Study 1, a six-item version of the NBS was found to be a good fit for the data and discriminant from overload, worry, and fatalism. NBS was higher for those with less education, non-White participants, and males. Individuals with higher backlash were also less likely to look at nutritional labels and to use sunscreen. Study 2 confirmed the factor structure from Study 1.
Conclusions:
A six-item version of NBS was found to be reliable, discriminant from related measures, higher in underserved groups (less educated, non-White, and male participants), and related to nutrition label use.
Keywords: Nutrition backlash, cancer information overload, cancer worry, cancer fatalism
Introduction
At the beginning of the 21st century, Goldberg (2000) argued that a pressing issue for nutrition was how audiences would “respond to mass health communication.” She noted that there was a need for nutrition research that “expanded understanding and respect for the multiple factors that drive human behavior” and recognition that “one of those factors is not necessarily knowledge.” Even though nutrition recommendations had remained stable, Goldberg pointed out that the public seemed confused, frustrated, and convinced that “nutritionists were always changer their minds” (p. 644).
Two decades have passed, yet Goldberg’s concerns remain at the forefront of nutrition science. Given the lack of progress at promoting healthy lifestyles, Hill (2018) stressed the need for more nutrition research on perception, behavior change, and motivation. Other researchers have echoed this call (Grunert, 2018), with Rowe (2018) adding that nutrition research needed to move beyond the simple communication of findings – referred to as the deficit model – toward models and frameworks that considered individual beliefs and perceptions of nutrition communication. Indeed, the communication environment has become, if anything, even more complex and challenging for nutrition science; research has shown that health-related news rarely has an author or clearly identifiable source (Capli et al., 2018), and that traditional news reporting practices can cultivate negative audience response such as beliefs that dietary behaviors do not impact health outcomes (i.e., fatalistic thinking) and negative perceptions of nutrition recommendations (i.e., nutrition backlash; Jensen et al., 2011; Jensen et al., 2017).
Responding to these calls, the current study examines nutrition backlash and its relationship with fatalism, information overload, and nutrition-related behaviors.
Nutrition Backlash
Consumer interest in health, fitness, and dietary information is high, with health and medical coverage comprising the majority of science news in U.S. media (Pellechia, 1997; Suleski & Ibaraki, 2010). But while interest may be high, data from the National Health and Nutrition Examination Survey (NHANES) shows that Americans consistently struggle to meet dietary recommendations, a situation that is especially pronounced for low-income families (Guenther et al., 2008; Kirkpatrick, Dodd, Reedy, Krebs-Smith, 2012; Schuster, Szpak, Klein, Sklar, & Dickin, 2019).
One of the reasons for this discrepancy may lie in the complexities of communicating nutrition research to the public. Individuals interested in nutrition information must navigate a diverse array of sources, the rapid pace of nutrition research and guideline updates, and the sometimes-contradictory framing of nutrition research by the media, all of which contribute to a landscape of public confusion about dietary recommendations (Goldberg & Sliwa, 2011).
Patterson and colleagues (2001) proposed nutrition backlash, caused by message confusion, as a possible mechanism underlying public dismissal of dietary recommendations. Nutrition backlash is an aversive disposition that refers to “a broad gamut of negative feelings about dietary recommendations, which could include skepticism, anger, guilt, worry, fear, and helplessness,” and which result from “inconsistent and confusing diet and health messages” (Patterson et al., 2001, pg. 38). In Patterson et al.’s study, nutrition backlash correlated with lower levels of fruit and vegetable consumption, and higher levels of fat consumption. Subsequent research has drawn on Patterson et al.’s construct to examine the role of conflicting media coverage in public acceptance of nutrition recommendations (Greiner, Clegg, Smith & Guallar, 2010; Nagler, 2014), and to inform research into other health arenas where conflicting media reports may lead to confusion or dismissal of health recommendations (Chang, 2015; Im & Huh, 2017). Concerning the latter, nutritional backlash has been utilized to study reactions to cancer prevention messages, serving as an outcome alongside cancer-related constructs such as cancer information overload, cancer worry, and cancer fatalism (Jensen, 2008; Jensen et al., 2011; Jensen et al., 2017).
The current study advances our understanding of nutrition backlash by (1) examining the psychometric qualities of Patterson et al.’s scale, (2) its relationship to demographic variables and health outcomes, and (3) discriminant validity from similar constructs which also measure public skepticism in the face of confusing health messages. In particular, this study considers discriminant validity of nutrition backlash from three other constructs also linked to contradictory or confusing public health messages: cancer information overload (feeling overwhelmed by cancer information), cancer worry (the fear of developing cancer), and cancer fatalism (the belief that nothing can be done to prevent or treat cancer) (Jensen et al., 2014; Jensen et al., 2017; Powe & Finnie, 2003). These questions are explored across two studies with U.S. adults.
Study 1
Study 1 examines the psychometric qualities of the nutrition backlash scale and compares it to the constructs of overload, worry, and fatalism. The current study also examines the relationship between backlash and health behaviors. Patterson and colleagues (2001) observed that backlash was negatively related to fruit and vegetable consumption. Given the importance of fruit and vegetable consumption, and identifying underlying correlates (Chapman et al., 2017), we replicate this analysis. In addition, we examine the relationship between backlash and food label use. Researchers have identified food labels as a key source of health information for consumers (Soederberg Miller & Cassady, 2015), and a driver of healthier food selections (Bucher, Murawski, Duncanson, Labe, & Van der Horst, 2018; Kim et al., 20016; Mhurchu, Eyles, Jiang, & Blakely, 2018; Nikolaou et al., 2017). Important to the present study, past work has suggested that food-related motivation might be a key moderator for meaningful label use (Mulders, Corneille, & Klein, 2018; Tanner, McCarthy, & O’Reilly, 2019). Thus, understanding whether backlash is related to label use advances our understanding of both. Finally, we explore whether nutritional backlash is related to other health behaviors, notably other behaviors that prevent cancer. The goal is to identify whether nutritional backlash is isolated to the context of nutrition or if it represents negative feelings about a larger domain. For instance, cancer information overload, cancer worry, and cancer fatalism all focus on cancer in general rather than a particular type of cancer or behavioral domain. Nutrition backlash is conceptualized as nutrition specific, but perhaps it is representative of a larger construct such as health recommendation backlash or cancer prevention backlash. As a first step in this direction, we examine the relationship between backlash and sunscreen/tanning behaviors (Aspinwall et al., 2014). Sunscreen/tanning behaviors are an ideal non-nutrition behavior for this analysis as (1) there is no direct nutrition component and (2) researchers often include both fruit/vegetable consumption and sun sunscreen/tanning in studies focused on cancer prevention behaviors in general (e.g., Spring, King, Pagoto, Van Horn, & Fisher, 2015).
Method
Design
Adults (18 and older) were recruited at a large U.S. shopping center (N = 480). The research team had a long table and 12 chairs set up in a central intersection of the shopping center. Banners advertised the study opportunity and the corresponding incentive ($10 gift cards). Participants approached the research team, were informed about the study, and, if they opted to participate, sat down at the table, and completed a paper survey instrument. After completing the survey, participants were provided with a paper debriefing, an opportunity to answer questions, and their gift card.
The protocol was approved and monitored by a university institutional research board (IRB). The IRB approved of the location site, banner recruitment method, gift card compensation, and data collection procedures. After data was collected, the lead-author deidentified each survey, and then another member of the research team manually entered data into SPSS for analysis. The data is available via Mendeley at http://dx.doi.org/10.17632/n9hsr98tpf.2
Participants
More females (64.8%) participated than males (35.2%). Participants ranged from 18 – 84 years of age, with a mean age of 35.31 years (SD = 15.75). The participants were predominantly Caucasian: 76.1% Caucasian, 8.7% African American, 4.4% Hispanic, Latino, or Spanish Origin, 4.6% Asian or Pacific Islander, 1.2% American Indian or Native American, and 4.0% described themselves as mixed race or other (participants could check more than one category). In regards to education level, 37.6% had a 12th grade education or less and 60.5% had more than a 12th grade education (1.9% missing). The mean household income was $49,948.47 (SD = $73,241.83). Participant political ideology was measured on a 7-point scale ranging from extremely liberal to extremely conservative (M = 4.17, SD = 1.51).
Measures
Nutrition Backlash.
To assess negative feelings (e.g., skepticism, worry, guilt, fear, anger and helplessness) associated with dietary recommendations, we used the 11-item nutrition backlash scale (NBS) developed by Patterson et al. (2001). Each item had four response options (strongly disagree to strongly agree), with higher scores equating to greater backlash. Examples of items include, “I am annoyed when there are no healthful food choices at a restaurant,” and “Scientists really don’t know whether a low-fat diet is good for you.” Previously, the NBS was found to be a reliable instrument (Cronbach’s α = .77; Patterson et al., 2001). Psychometric properties of the NBS in the current studies are reported in the results sections.
Cancer Information Overload (CIO).
CIO was measured using an 8-item scale from Jensen et al. (2013). Each item had four response options (strongly disagree to strongly agree), with higher scores equating to greater information overload (M = 2.46, SD = .50, Cronbach’s α = .81). Sample items included, “There are so many different recommendations about preventing cancer, it’s hard to know which ones to follow,” and “It has gotten to the point where I don’t even care to hear new information about cancer.”
Cancer Worry.
Cancer worry was assessed using eight items. Responses were measured on a seven-point scale (ranging from not at all to very much), with higher scores indicating greater worry. For this study, cancer worry was divided into two dimensions: cancer worry frequency (CWF) and cancer worry severity (CWS). CWS was measured using four items examining the extent to which individuals worry about cancer (M = 3.56, SD = 1.78, Cronbach’s α = .90). Sample items included, “I am afraid of the physical consequences of getting cancer,” and “I worry about my health because of my chances of getting cancer.” CWF frequency was measured using four items from the Revised Impact of Events Scale (RIES-Intrusive) examining the amount individuals worried about cancer in the past seven days (Horowitz, Wilner, & Alverez, 1979) (M = 1.72, SD = 1.23, Cronbach’s α = .85). Sample items included “I have dreams about cancer,” and “Pictures about cancer have popped into my mind.”
Cancer Fatalism.
This study used the 15-item Powe fatalism inventory (PFI) to evaluate cancer fatalism (Powe & Finnie, 2003; Powe, 1996). Five response options (strongly disagree, disagree, neutral, agree, strongly agree) were available for each item and scored from 1–5, with higher scores indicating greater fatalism. Past research has demonstrated that the PFI has two dimensions: prevention-focused cancer fatalism and treatment-focused cancer fatalism. Cancer fatalism – prevention (CFP) was measured using seven items conveying the message that there is nothing that can be done to prevent cancer (M = 2.52, SD = .89, Cronbach’s α = .89). Sample items included, “I believe that if someone is meant to have cancer it doesn’t matter what they eat, they will get cancer anyway,” Cancer fatalism – treatment (CFT) was measured using six items expressing the idea that death from cancer is unavoidable (M = 1.98, SD = .81, Cronbach’s α = .83). Sample items include, “I believe if someone gets cancer a lot of different treatments won’t make any difference.”
Health Behaviors.
Fruit and vegetable consumption questions were modeled after standard items included in the NCI Foods Attitudes and Behaviors (FAB) Survey (e.g., Erinosho, Moser, Oh, Nebeling, & Yaroch, 2012) and the Health Information National Trends Survey (HINTS) (e.g., Kiviniemi, Orom, & Giovino, 2011). Participants were asked, “How many cups of fruit do you eat per day?” (M = 1.35, SD = 1.01) and “How many cups of vegetables do you eat per day?” (M = 1.72, SD = 1.18). Other health behaviors were evaluated using modified versions of items from Grunert, Wills, and Fernández-Celemín, (2010) and Glanz and colleageus (2003) with a five-point scale indicating how frequently participants engaged in that behavior (not at all to very much) with higher scores indicating more frequent participation. Participants reported three other health behaviors: “look at nutrition labels on food products,” (M = 3.21, SD = 1.29) “put on sunscreen,” (M = 2.61, SD = 1.35) and “use a tanning bed” (M = 1.57, SD = 1.05).
Results
Exploratory Factor Analysis
Howard (2016) argued that exploratory factor analysis should be performed using principal axis factoring (PAF), direct oblimin rotation (specifically, direct quartimin), parallel analysis for factor extraction, and a .40-.30-.20 rule for factor loading cut-offs. Concerning the latter, an item should be retained only if it loads at .40 or higher on its primary factor, below .30 on all other factors, with at least a .20 loading difference between the load on the primary factor and all other factors loadings for that item.
Accordingly, we performed PAF with direct oblimin rotation on the original eleven items of the nutrition backlash scale (henceforth NBack11). NBack11 had three factors with an eigenvalue greater than one (see Table 1). However, Howard (2016) argued that the “greater than one” eigenvalue rule should be replaced with parallel analysis (for more details, see Patil, Singh, Mishra, & Donovan, 2008). Parallel analysis establishes eigenvalue cut-off points based on the number of variables to be analyzed and the sample size. In this case, parallel analysis (11 items, N = 481) suggested the following cut-off points for eigenvalues: 1.32 (factor1), 1.22 (factor 2), 1.17 (factor3). Thus, only the first two factors have eigenvalues above their parallel analysis cut-off points.
Table 1.
Principal Axis Analysis of Nutrition Backlash Scale.
| Factor Analysis | |||||
|---|---|---|---|---|---|
| NBack11 | NBack6 | ||||
| Items | 1 | 2 | 3 | 1 | M(SD) |
| I am annoyed when there are no health food choices at a restaurant. (back1) | .662 | 2.34 (1.04) | |||
| There should be warning labels on high fat foods. (back2) | .744 | 2.07 (.96) | |||
| Research on nutrition is going to help me live longer. (back3) | .637 | 1.88 (.87) | |||
| The government should not tell people what to eat. (back4) | .505 | 2.85 (1.02) | |||
| Americans are obsessed about the fat in their diet. (back5) | .403 | 2.58 (.96) | |||
| I am tired of hearing about what I should or should not eat. (back6) | .684 | .520 | 2.44 (.99) | ||
| Dietary recommendations should be taken with a grain of salt. (back7) | .467 | .491 | 2.19 (.91) | ||
| I have decided to stop worrying about my fat intake. (back8) | .600 | .701 | 1.89 (.91) | ||
| Eating low fat foods takes the pleasure out of eating. (back9) | .507 | .503 | 2.16 (.94) | ||
| All the new low fat foods on the market are not going to improve anyone’s health. (back10) | .707 | .651 | 2.02 (.88) | ||
| Scientists really don’t know whether a low fat diet is good for you. (back11) | .628 | .671 | 2.03 (.89) | ||
| Eigenvalue | 3.43 | 1.58 | 1.14 | 2.75 | |
| % variance explained | 31.02 | 14.38 | 10.32 | 45.79 | |
Note. N = 480. Principal axis factor analysis of the eleven item model (NBack11) and six item model (NBack6). Means and standard deviations for each item reported in the final column.
An examination of the pattern structure revealed that the first factor was items back7-back11. For the most part, those items referred to beliefs about low fat diets. The second factor consisted of items back1-back3. Those items are reverse-coded which raises concerns about the veracity of this factor. Factor three included back4-back6. Two of those items (back4, back5) seemed to refer to tertiary beliefs that were not focused directly on nutrition backlash. Yet, the third item in that factor (back6) does seem relevant to nutrition backlash.
Given concerns about factors two and three, we dropped five items (back1-back5) and conducted a follow-up factor analysis on the remaining six items (back6-back11; henceforth NBack6). NBack6 had one factor with an eigenvalue greater than one (Eigenvalue = 2.75) which explained 45.79% of the variance. Parallel analysis suggested that a factor should be retained for this design (6 items, N = 481) if the eigenvalue was greater than 1.21. Thus, the single factor model was retained. Loadings within that factor were all greater than .40 (Howard, 2016).
Reliability analysis revealed that both models (NBack11, NBack6) had identical reliability (Cronbach’s α = .76). In light of the conceptual clarity of the six item model, and equivalent reliability, we opted to utilize NBack6 as the primary model for this analysis, however, we also included NBack11 in bivariate analysis so that readers can compare the two.
Bivariate Analysis
Bivariate relationships were examined between all study variables (see Table 2). NBack6 was positively correlated with NBack11 (r = .89, p < .001) as well as CIO, CFP, and CFT. NBack6 was higher for those with less education, non-White participants, and males. Individuals with higher backlash were less likely to look at nutrition labels and to use sunscreen.
Table 2.
Bivariate Correlations.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | 18. | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | NBack6 | ---- | |||||||||||||||||
| 2. | NBack11 | .89* | ---- | ||||||||||||||||
| 3. | CIO | .27* | .20* | ---- | |||||||||||||||
| 4. | CWF | −.06 | −.12* | .13* | −---- | ||||||||||||||
| 5. | CWS | −.02 | −.09† | .11* | .45* | ---- | |||||||||||||
| 6. | CFP | .24* | .26* | .21* | .06 | .13* | ---- | ||||||||||||
| 7. | CFT | .34* | .28* | .15* | .04 | .07 | .49* | ---- | |||||||||||
| 8. | Age | −.03 | −.06 | −.12* | −.15* | −.02 | −.03 | −.10* | ---- | ||||||||||
| 9. | Edu | −.19* | −.17* | .05 | .01 | −.09† | −.08† | −.25* | −.05 | ---- | |||||||||
| 10. | Race | −.11* | −.03 | −.08† | −.19* | −.05 | −.11* | −.22* | .19* | .00 | ---- | ||||||||
| 11. | Income | −.02 | −.03 | −.01 | −.02 | −.03 | −.03 | −.04 | .00 | .12* | .05 | ---- | |||||||
| 12. | Sex | −.16* | −.20* | −.04 | .12* | .07 | −.05 | −.12* | .05 | .09* | .02 | .06 | ---- | ||||||
| 13. | Pol. Ideology | .05 | .07 | .06 | −.11* | −.06 | .07 | −.08 | .20* | .01 | .21* | .08 | −.04 | ---- | |||||
| 14. | Fruit | −.06 | −.11* | −.06 | −.03 | −.01 | −.13* | −.08 | −.04 | .07 | .02 | .02 | .16* | .05 | ---- | ||||
| 15. | Vegetables | −.06 | −.08† | −.08† | −.01 | −.07 | −.19* | −.13* | .04 | .05 | −.02 | .10* | .11* | .07 | .57* | ---- | |||
| 16. | Look at Label | −.35* | −.44* | −.13* | .07 | .03 | −.26* | −.23* | .10* | .18* | .05 | .07 | .24* | −.01 | .26* | .20* | ---- | ||
| 17. | Sunscreen | −.12* | −.16* | −.12* | −.03 | −.08† | −.13* | −.19* | .01 | .16* | .17* | .09† | .27* | .04 | .17* | .17* | .29* | ---- | |
| 18. | Tanning | .02 | .02 | .00 | .10* | .03 | .08† | .09† | −.23* | −.10* | .12* | .02 | .16* | −.04 | .04 | .07 | −.07 | .00 | ---- |
Note. N = 480. Education: Less/more than high school (0/1), Race: non-White/White (0/1). Sex: male/female (0/1). Political ideology: liberal/conservative (0/1).
p < .10,
p < .05
There were some differences between NBack6 and NBack11. The latter was negatively related to CWF and CWS. It was unrelated to race and negatively correlated with fruit and vegetable consumption.
Discriminant Analysis
Discriminant validity assess whether constructs are distinct (Henseler, Ringle, & Sarstedt, 2015). We assessed discriminant validity using the heterotrait-monotrait (HTMT) method (Henseler et al., 2015). SmartPLS software was utilized to calculate HTMT (Ringle, Wende, & Becker, 2015). Using a threshold of .85 (Henseler et al., 2015; Kline, 2011), NBack6 was significantly different than CIO, CWS, CWF, CFP, and CFT (see Table 3). Of note, all the other variables were also discriminant from one another.
Table 3.
Discriminant Validity.
| NBack6 | CIO | CWF | CWS | CFP | CFT | |
|---|---|---|---|---|---|---|
| NBack6 | .34 | .10 | .05 | .29 | .29 | |
| CIO | .16 | .15 | .24 | .20 | ||
| CWF | .50 | .07 | .08 | |||
| CWS | .13 | .10 | ||||
| CFP | .57 | |||||
| CFT |
Note. N = 480. Heterotrait-monotrait (HTMT) ratio for calculating discriminant validity. Loadings above .85 are indicative of discriminant validity concerns.
Hierarchical Regression
Past research has shown that nutrition backlash is related to dietary intake, even after controlling for demographics (Patterson et al., 2001). Three hierarchical linear regressions were conducted and blocked as follows: demographics (block1), related constructs (block 2), and NBack6 (block3). The results are reported in Table 4. NBack6 was not significantly related to fruit [R = .27, R2 change = .001, Fchange (1, 374) = .36, p = .55] or vegetable consumption [R = .30, R2 change = .001, Fchange (1, 374) = .39, p = .53], but it was significantly related to look at labels [R = .45, R2 change = .029, Fchange (1, 372) = 13.67, p < .001]. Backlash explained 2.9% of the variance in look at labels above and beyond demographics and other related constructs.
Table 4.
Hierarchical Regressions.
| Fruit | Vegetables | Look at Label | ||||
|---|---|---|---|---|---|---|
| β | R2 Δ | β | R2 Δ | β | R2 Δ | |
| Block1 | .04* | .05** | .10*** | |||
| Age | −.05 | .05 | .10* | |||
| Age | −.05 | .05 | .10* | |||
| Education | .05 | .01 | .14** | |||
| Race | −.05 | −.09 | .00 | |||
| Income | −.01 | .11* | .04 | |||
| Sex | .17*** | .14** | .24*** | |||
| Pol. Ideology | .06 | .06 | −.03 | |||
| Block 2 | .03* | .05** | .07*** | |||
| CIO | −.05 | −.09 | −.05 | |||
| CWF | −.08 | −.03 | .09 | |||
| CWS | .06 | −.02 | .01 | |||
| CFP | −.17*** | −.19*** | −.23*** | |||
| CFT | .10 | .04 | −.03 | |||
| Block 3 | .00 | .00 | .03*** | |||
| NBack6 | −.03 | −.03 | −.19*** | |||
Note.N = 480. Hierarchical regression with demographics in the first block, other related constructs in the second block, and NBack6 in the third block. Education: Less/more than high school (0/1), Race: non-White/White (0/1). Sex: male/female (0/1). Political ideology: liberal/conservative (0/1).
p < .05,
p< .01,
p < .001
Two additional details are of note. First, an identical set of hierarchical regressions were conducted with NBack11 as the variable of interest. In that analysis, NBack11 produced the same results as NBack6 (no relationship to fruit and vegetable consumption, a negative relationship with look at labels). Second, nutrition backlash aside, CFP was negatively related to fruit and vegetable consumption such that individuals with higher fatalism reported less fruit and vegetable consumption.
Study 2
Study 1 identified six items that loaded on a single factor. Study 2 sought to confirm that factor structure in a separate sample recruited from different locations.
Method
Design
Adults (18 and older) were recruited from seven large U.S. shopping centers (N = 399). Recruitment was identical to Study 1. The protocol was approved and monitored by a university IRB. After data collection, the lead-author de-identified all surveys and another member of the research team entered the data into SPSS for analysis. The data is available via Mendeley at http://dx.doi.org/10.17632/2tnygp8hf4.2
Participants
More females (66.2%) participated than males (31.6%; 2.2% missing) Participants ranged from 18 – 84 years of age, with a mean age of 36.68 years (SD = 16.33). The participants were predominantly Caucasian: 83.2% Caucasian, 11.7% African American, 3.1% Hispanic, Latino, or Spanish Origin, 1.0% Asian or Pacific Islander, 1.8% American Indian or Native American, and 2.3% described themselves as “other” (participants could check more than one category). The breakdown of education levels was 55.4% had a 12th grade education or less and 41.6% had more than a 12th grade education (3.3% missing). The mean household income was $51,769.46 (SD = $42,954.35).
Measures
Nutrition backlash was measured using the 11 items described in Study 1.
Results
Confirmatory factor analysis is sensitive to multivariate non-normality, and past research has shown that most datasets are non-normal (Micceri, 1989). That is, even though researchers are taught to expect multivariate normality, the reality is that most datasets violate this assumption. Consistent with this research, the nutrition backlash items exhibited significant multivariate abnormality, skewness = 9.64, Z-score = 14.12, p < .001, and kurtosis = 175.49, Z-score = 12.89, p < .001.
If a dataset is non-normal, researchers should utilize the asymptotic covariance matrix when conducting a CFA to calculate a Satorra-Bentler (S-B) χ2 (Satorra & Bentler, 2010). Lisrel 9.30 was utilized to conduct a CFA adjusting for multivariate non-normality. Six indicators were utilized to assess model fit: S-B χ2, CFI, RMSEA, SRMR, and Model AIC (Akaike, 1987; Hu & Bentler, 1999; Holbert & Stephenson, 2008; Kline, 2011).
Confirmatory Factor Analysis
Study 1 supported a six-item model for measuring nutrition backlash (NBack6), but Patterson and colleagues (2001) originally advocated for an 11-item model (NBack11). As a first step, we assessed NBack11 (one latent variable and eleven indicators). NBack11 was not a good fit for the data, S-B χ2 (44, N = 481) = 327.56, p < .001, CFI = .84, RMSEA = .12 (90% CI: .10, .13), SRMR = .09, Model AIC = 371.56.
Given the lack of fit, we next tested NBack6. Model fit was better, but still below standards: S-B χ2 (9, N = 481) = 39.60, p < .001, CFI = .97, RMSEA = .08 (90% CI: .06, .11), SRMR = .05, Model AIC = 63.60.
An examination of the modification indices revealed that model fit for NBack6 would be enhanced by allowing error-term correlations for items back10 and back11. Bentler (2010) noted that correlated error-terms should be explained, though he also argued that they may be unavoidable. In this case, the correlation is logical for back10 and back11 as the items contain similar language (e.g., “low fat”) and were the last two items in the battery (i.e., item order was not randomized) which likely led to spurious correlations independent of the latent construct. A revised model was tested allowing for an error-term correlation between back10 and back11. The revised model was an excellent fit for the data, S-B χ2 (8, N = 481) = 7.50, p = .48, CFI = 1.00, RMSEA = .00 (90% CI: .00, .05), SRMR = .02, Model AIC = 33.50 (see Figure 1). Thus, CFA supported NBack6.
Figure 1.
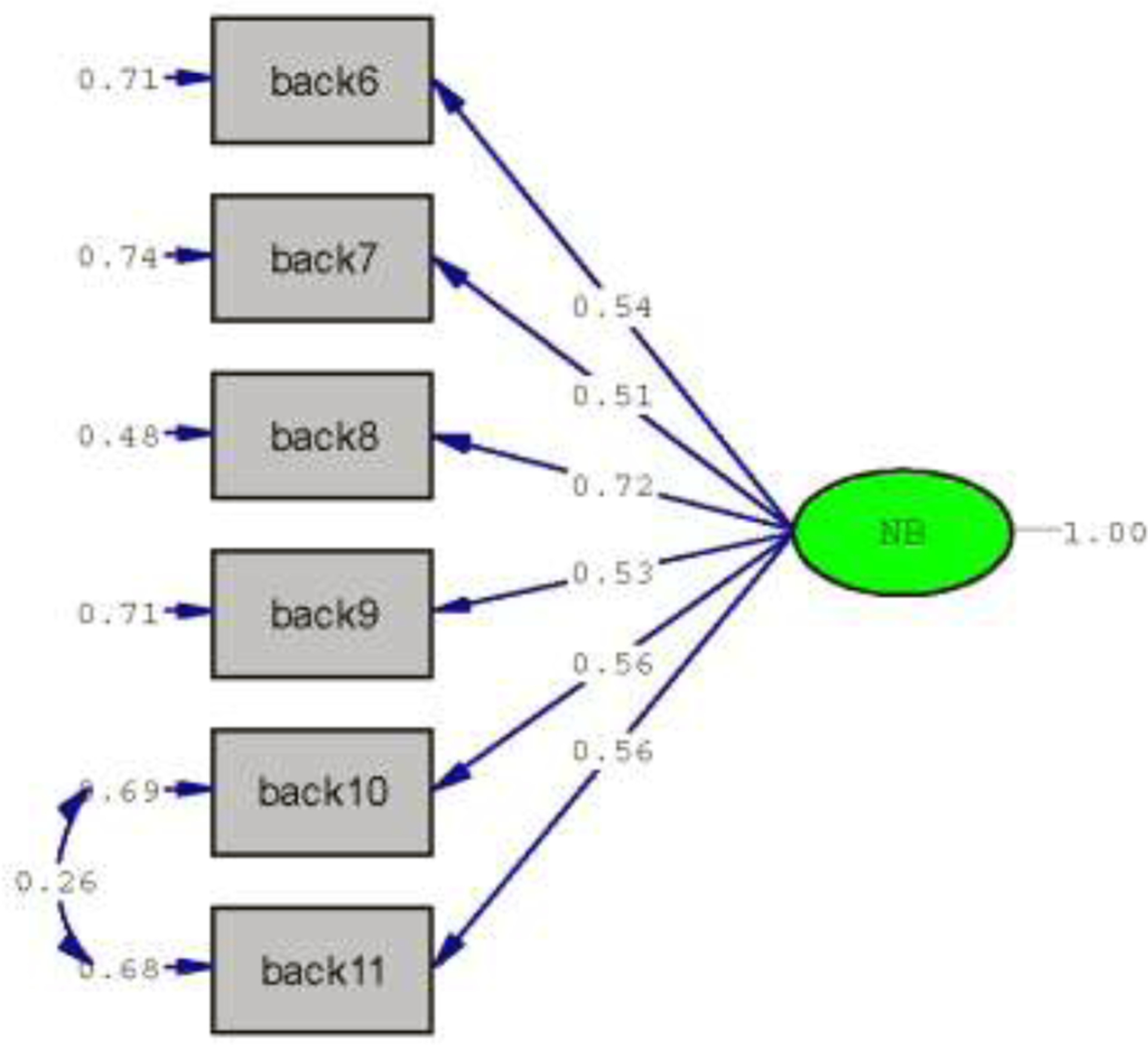
N = 399. Confirmatory factor analysis (CFA) of NBack6.
Discussion
A six-item version of the NBS (Nback6) was demonstrated to be reliable, and scores were higher in less educated, non-White, and male participants. Backlash was also discriminant from overload, worry, and fatalism, and related to nutrition label and sunscreen use. Therefore, our analysis confirmed nutrition backlash as a distinct construct which is related to demographic variables and can explain variance in health behaviors.
Moreover, our analysis demonstrated that nutrition backlash is related to meaningful health behaviors and may explain some demographic variance in adoption or dismissal of health recommendations. Nutrition backlash was higher in male, low-income, and non-White participants which makes sense given that the NHANES survey has shown that these demographic variables are associated with poorer adoption of nutrition recommendations (Guenther et al., 2006; Guenther et al., 2008). Additionally, participants with higher levels of nutrition backlash were less likely to consult food labels. Food label use is associated with healthier food selection (Kim et al., 2016; Mhurchu et al., 2018; Nikolaou et al., 2017) which suggests that individuals with higher nutrition backlash may have lower nutrient profile scores. Future research could consider the relationship between nutrition backlash, label use, and nutrition knowledge as the latter is a key predictor of meaningful label use (Soederberg Miller & Cassady, 2015). Interestingly, nutrition backlash was also associated with a failure to follow recommendations on sunscreen use, a relationship that hints at the possibility of a larger underlying construct. For example, it is possible that nutrition backlash is just one part of a larger construct focused on health recommendation backlash, cancer prevention backlash, or perhaps backlash against authority. To examine this possibility, researchers could develop a set of items to represent these larger constructs and examine whether nutritional backlash is discriminant from each. An alternative interpretation of the relationship between nutritional backlash and sun safe behaviors is that it could suggest the presence of an underlying negativity directed at public health messengers (O’Key & Hugh-Jones, 2010; Satter, 2007).
However, in contradiction to previous studies, we found no significant relationship between fruit and vegetable consumption and nutrition backlash. It’s possible that participant confusion about the measurements used in our study—in particular, what constitutes a cup—may have impacted this result. While brief instruments can be valid measures of longer fruit and vegetable measures (Cook et al., 2015) previous research also has shown that different measurement systems may produce quite different self-reports of food consumption (Michels, Welch, Luben, Bingham, & Day, 2005). We should also note that when the original 11-item scale was used, nutrition backlash did replicate Patterson et al.’s (2001) findings for fruit at the bivariate level, although that finding did not hold at the multivariate level.
Our study, then, suggests several possible directions for future research. First, researchers should attempt to replicate the results herein using an alternative measure of fruit and vegetable consumption. Secondly, while our studies confirmed Patterson et al.’s findings that nutrition backlash explains some of the variance in the public’s willingness to adopt dietary recommendations, our studies also suggest a benefit to revisiting the original scale. Our six-item version of the scale (NBack6) operated as a better-fitting measure than the full, original scale (NBack11), but that psychometric gain comes with a potential loss, in that the resulting scale focuses almost entirely on low-fat diets. Third, several nutrition-related constructs that could be related to backlash were not measured, such as nutrition knowledge (Soederberg Miller & Cassady, 2015), food neophobia (Damsbo-Svendsen, Bom Frøst, & Olsen, 2017), and psychosocial predictors of fruit and vegetable consumption (Satia et al., 2002). Future research should consider measuring all three constructs. Fourth, nutrition backlash research could benefit from an investigation into the origins of backlash and its cultivation over time. Qualitative research, perhaps focused on high-risk groups identified in the current study or elsewhere (see, e.g., Monge-Rojas et al., 2013; Rosa, Ortolano, & Dickin, 2018), would be especially meaningful, in that it could identify the precursors of the disparity in perception and reaction to dietary recommendations.
As explicated, nutrition backlash seems to refer to backlash against nutrition information in general, rather than against a single set of recommendations (low-fat diets). Additionally, since the creation of this scale, public perception of dietary recommendations may have moved beyond a perceived focus on low-fat diets. This shift, and a surge of nutrition primitivism (Knight, 2011, 2015), suggests a complex perceptual geography that is far from static. Indeed, nutrition backlash is likely a dynamic construct that is best measured by a diverse set of items in order to fully capture its underlying variance. The diversity of the original scale may partially explain why NBack11 is significantly related to fruit consumption at the bivariate level, while our revised six-item scale, despite being more psychometrically-sound, is not. This all suggests that future nutrition backlash research may benefit from a revised and expanded measure. The creation and validation of additional items has the potential to yield a psychometrically-sound scale that also captures additional variance and is less sensitive to shifts in actual or perceived dietary recommendations.
The results of the current study underscore three recommendations for government and public stakeholders. First, nutrition backlash should be routinely measured, and tracked, as part of a larger data collection effort. For example, the Health Communication and Informatics Research Branch of the National Cancer Institute has routinely measured cancer information overload and fatalism as part of the Health Information National Trends Survey (HINTS; Finney Rutten et al., 2020). Nutrition backlash could be added to HINTS, or to a similar data collection effort. Second, the higher levels of backlash observed for male, low-income, and non-White participants suggests there is a need for additional programming and interventions targeting these groups. Third, when constructing interventions and programs, both government and public stakeholders should consider whether they are trying to fill a knowledge deficit, counter a negative backlash, or both. There is a tendency in interventions/programs to focus on providing knowledge alone (Rowe, 2018); the current data suggests that communicators may benefit from spending equal or additional time countering backlash.
Though not the primary focus of the current study, a number of interesting findings emerged for cancer information overload, cancer worry, and cancer fatalism. All three constructs were found to be discriminant from nutritional backlash and from each other. This is noteworthy as past research has often utilized several of these constructs in the same study and assumed they are distinct (e.g., Jensen et al., 2017). Our results support that assumption. Discriminant validity aside, our results also revealed that prevention-oriented cancer fatalism is negatively related to nutritional outcomes, including fruit/vegetable consumption and looking at nutrition labels.
Limitations
The current research had several limitations. Participants were drawn from a single state, and therefore may not be representative of individuals living in other areas. Fruit and vegetable consumption can be measured in a variety of ways, and alternative measures than those used here may be more meaningful for participants. Finally, our research was cross-sectional, and therefore causality cannot be established between nutrition backlash and health outcomes.
Conclusion
Given the public’s perennial interest in health and dietary recommendations and the large amount of media coverage health and diet receive, there is a puzzling disconnect between dietary recommendations and the actual behavior of U.S. consumers. That disconnect likely has a variety of causes, from the individual to the systemic, but one possible underlying mechanism is nutrition backlash. Research has shown that nutrition backlash has the potential to explain some demographic variance in the adoption of health and diet behaviors, representing a promising area for future nutrition research. The development of an enduring and diverse scale to measure nutrition backlash will help those researchers as they continue to explicate the causes of dietary disparities.
Highlights.
A six-item nutrition backlash scale was found to be reliable across two studies.
Nutrition backlash was discriminant from fatalism, overload, and worry.
Nutrition backlash was higher for male, low-income, and non-White participants.
Individuals with higher backlash were also less likely to look at nutritional labels.
Individuals with higher backlash were also less likely to use sunscreen.
Acknowledgments:
Jakob D. Jensen is a Professor and Elizabeth A. Giorgi, Jennifer Jackson, Julia Berger, and Rachael Katz are graduate students in the Department of Communication at the University of Utah. Dr. Jensen is also a member of the Huntsman Cancer Institute. Dr. Amy Mobley is an Associate Professor in the Department of Health Education & Behavoir at the University of Florida. This manuscript was written with support from NIH grant 1DP2EB022360-01 (PI: J. Jensen) and 3P30CA042014-29S7 (PI: J. Jensen). Correspondence concerning this article should be addressed to Jakob D. Jensen, Department of Communication, University of Utah, 2618 LNCO, 255 S. Central Campus Drive, Salt Lake City, Utah, 84112
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Akaike H (1987). Factor Analysis and AIC. Psychometrika, 52, 317–332. [Google Scholar]
- Aspinwall LG, Taber JM, Kohlmann W, Leaf SL, & Leachman SA (2014). Unaffected family members report improvements in daily routine sun protection 2 years following melanoma genetic testing. Genetics in Medicine, 16(11), 846–853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentler PM (2010). SEM with simplicity and accuracy. Journal of Consumer Psychology, 20, 215–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucher T, Murawski B, Duncanson K, Labbe D, & Van der Horst K (2018). The effect of the labelled serving size on consumption: A systematic review. Appetite, 128, 50–57. 10.1016/j.appet.2018.05.137 [DOI] [PubMed] [Google Scholar]
- Capli DB, Ozaydin SK, & Ozturk S (2018). Ethical issues in health communication: health-related news sourcing practices. Nutrition, 55–56, S14–S15. [Google Scholar]
- Chang C (2015). Motivated processing: How people perceive news covering novel or contradictory health research findings. Science Communication, 37(5), 602–634. [Google Scholar]
- Chapman K, Goldsbury D, Watson W, Havill M, Wellard L, Hughes C, Bauman A, & Allman-Farinelli M (2017). Exploring perceptions and beliefs about the cost of fruit and vegetables and whether they are barriers to higher consumption. Appetite, 113, 310–319. 10.1016/j.appet.2017.02.043 [DOI] [PubMed] [Google Scholar]
- Cook A, Roberts K, O’Leary F, & Allman-Farinelli MA (2015). Comparison of single questions and brief questionnaire with longer validated food frequency questionnaire to assess adequate fruit and vegetable intake. Nutrition, 31, 941–947. [DOI] [PubMed] [Google Scholar]
- Damsbo-Svendsen M, Bom Frøst M, & Olsen A (2017). A review of instruments developed to measure food neophobia. Appetite, 113, 358–367. [DOI] [PubMed] [Google Scholar]
- Erinosho TO, Moser RP, Oh AY, Nebeling LC, & Yaroch AL (2012). Awareness of the Fruits and Veggies-More Matters campaign, knowledge of the fruit and vegetable recommendation, and fruit and vegetable intake of adults in the 2007 Food Attitudes and Behaviors (FAB) Survey. Appetite, 59(1), 155–160. [DOI] [PubMed] [Google Scholar]
- Finney Rutten LJ, Blake KD, Skolnick VG, Davis T, Moser RP, & Hesse BW (2020). Data resource profile: The National Cancer Institute’s Health Information National Trends Survey (HINTS). International Journal of Epidemiology, 49 17–17j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Schoenfeld E, Weinstock MA, Layi G, Kidd J, & Shigaki DM (2003). Development and reliability of a brief skin cancer risk assessment tool. Cancer Detection and Prevention, 27, 311–315. [DOI] [PubMed] [Google Scholar]
- Goldberg JP (2000). Nutrition communication in the 21st century: what are the challenges and how can we meet them? Nutrition, 16, 644–646. [DOI] [PubMed] [Google Scholar]
- Goldberg JP & Sliwa SA (2011). Communicating actionable nutrition messages: Challenges and opportunities. Proceedings of the Nutrition Society, 70(1), 26–37. [DOI] [PubMed] [Google Scholar]
- Greiner A, Clegg Smith K, & Guallar E (2010). Something fishy? News media presentation of complex health issues related to fish consumption guidelines. Public Health Nutrition, 13(11), 1786–1794. [DOI] [PubMed] [Google Scholar]
- Grunert KG (2018). Drivers of food choice: A cognitive structure approach to the determinants of food choice and implications for affecting behavior change. Nutrition, 55–56, S4–S5. 10.1016/j.nut.2018.07.004 [DOI] [Google Scholar]
- Grunert KG, Wills JM, & Fernández-Celemín L (2010). Nutrition knowledge, and use and understanding of nutrition information on food labels among consumers in the U.K. Appetite, 55(2), 177–189. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Dodd KW, Reedy J, & Krebs-Smith SM (2006). Most Americans eat much less than recommended amounts of fruits and vegetables. Journal of the American Dietetic Association, 106, 1371–1379. [DOI] [PubMed] [Google Scholar]
- Guenther PM, Juan W, Lino M, Hiza HA, Fungwe T, & Lucas R (2008). Diet quality of low-income and higher income Americans in 2003–2004 as measured by the healthy eating index-2005 Nutrition Insight 42 Alexandria, VA: USDA Center for Nutrition Policy and Promotion. [Google Scholar]
- Hill JO (2018). Why aren’t we making progress in promoting healthy lifestyles? Nutrition, 55–56, S2–S3. [Google Scholar]
- Henseler J, Ringle CM, & Sarstedt M (2015). A new criterion for assessing discriminant validity in variance-based structural equation modeling. Journal of the Academy of Marketing Science, 43, 115–135. [Google Scholar]
- Holbert RL, & Stephenson MT (2008). Commentary on the uses and misuses of structural equation modeling in communication research In Hayes AF, Slater MD, & Snyder LB (Eds.), The Sage sourcebook of advanced data analysis methods for communication research (pp. 185–218). Thousand Oaks, CA: Sage. [Google Scholar]
- Howard MC (2016). A review of exploratory factor analysis decisions and overview of current practices: What we are doing and how can we improve? International Journal of Human-Computer Interaction, 32(1), 51–62. [Google Scholar]
- Hu L, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. [Google Scholar]
- Im H, & Huh J (2017). Does health information in mass media help or hurt patients? Investigation of potential negative influence of mass media health information on patients’ beliefs and medication regimen adherence. Journal of Health Communication, 22(3), 214–222. [DOI] [PubMed] [Google Scholar]
- Jensen JD (2008). Scientific uncertainty in news coverage of cancer research: Effects of hedging on scientists’ and journalists’ credibility. Human Communication Research, 34, 347–369. [Google Scholar]
- Jensen JD, Carcioppolo N, King AJ, Bernat JK, Davis L, Yale RN, & Smith J (2011). Including limitations in news coverage of cancer research: Effects of news hedging on fatalism, medical skepticism, patient trust, and backlash. Journal of Health Communication, 16(5), 486–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen JD, Carcioppolo N, King AJ, Scherr CL, Jones CL, & Niederdeppe J (2014). The cancer information overload (CIO) scale: Establishing predictive and discriminant validity. Patient Education & Counseling, 94(1), 90–96. [DOI] [PubMed] [Google Scholar]
- Jensen JD, Pokharel M, Scherr CL, King AJ, Brown N, & Jones C (2017). Communicating uncertain science to the public: How amount and source of uncertainty impact fatalism, backlash, and overload. Risk Analysis, 37(1), 40–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H-S, Oh C, & No J-K (2016). Can nutrition label recognition or usage affect nutrition intake according to age? Nutrition, 32, 56–60. [DOI] [PubMed] [Google Scholar]
- Kiviniemi MT, Orom H, & Giovino GA (2011). Race/ethnicity, psychological distress, and fruit/vegetable consumption: The nature of the distress-behavior relation differs by race/ethnicity. Appetite, 56(3), 737–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkpatrick SI, Dodd KW, Reedy J, & Krebs-Smith SM (2012). Income and race/ethnicity are associated with adherence to food-based dietary guidance among U.S. adults and children. Journal of the Academy of Nutrition and Diet, 112(5), 624–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB (2011). Principles and practice of structural equation modeling. 2nd ed. New York, NY: Guildford. [Google Scholar]
- Knight C (2011). The food nature intended you to eat.’ Nutritional primitivism and low-carbohydrate dieting. Appetite, 56(2), 534. [Google Scholar]
- Knight C (2015). “We can’t go back a hundred million years”: Low-carbohydrate dieters’ response to nutritional primitivism. Food, Culture & Society, 18(3), 441–461. [Google Scholar]
- Mhurchu CN, Eyles H, Jiang Y, & Blakely T (2018). Do nutrition labels influence healthier food choices? Analysis of label viewing behavior and subsequent food purchases in a labelling intervention trial. Appetite, 121, 360–365. 10.1016/j.appet.2017.11.105 [DOI] [PubMed] [Google Scholar]
- Micceri T (1989). The unicorn, the normal curve, other improbable creatures. Psychological Bulletin, 105, 156–166. doi:10.1037/0033-2909.105.1.156 [Google Scholar]
- Michels KB, Welch AA, Luben R, Bingham SA, & Day NE (2005). Measurement of fruit and vegetable consumption with diet questionnaires and implications for analyses and interpretation. American Journal of Epidemiology, 161(10), 987–994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monge-Rojas R, Smith-Castro V, Colón-Ramos U, Aragón MC, & Herrera-Raven F (2013). Psychosocial factors influencing the frequency of fast-food consumption among urban and rural Costa Rican adolescents. Nutrition, 29(7–8), 1007–1012. [DOI] [PubMed] [Google Scholar]
- Mulders MDGH, Corneille O, & Klein O (2018). Label reading, numeracy and food and nutrition involvement. Appetite, 128, 214–222. 10.1016/j.appet.2018.06.003 [DOI] [PubMed] [Google Scholar]
- Nagler RH (2014). Adverse outcomes associated with media exposure to contradictory nutrition messages. Journal of Health Communication, 19(1), 24–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaou CK, McPartland M, Demkova L, & Lean MEJ (2017). Supersize the label: The effect of prominent calorie labeling on sales. Nutrition, 35, 112–113. [DOI] [PubMed] [Google Scholar]
- O’Key V, & Hugh-Jones S (2010). I don’t need anybody to tell me what I should be doing: A discursive analysis of maternal accounts of (mis)trust of healthy eating information. Appetite, 54(3), 524–532. 10.1016/j.appet.2010.02.007 [DOI] [PubMed] [Google Scholar]
- Patil VH, Singh SN, Mishra S, & Donovan DT (2008). Efficient theory development and factor retention criteria: A case for abandoning the ‗eigenvalue greater than one’ criterion. Journal of Business Research, 61, 162–170. [Google Scholar]
- Patterson RE, Satia JA, Kristal AR, Neuhouser ML, & Drewnowski A (2001). Is there a consumer backlash against the diet and health message? Journal of the American Dietetic Association, 101, 37–41. [DOI] [PubMed] [Google Scholar]
- Pellechia MG (1997). Trends in science coverage: A content analysis of three U.S. newspapers. Public Understanding of Science, 6, 49–68. [Google Scholar]
- Powe BD (1996). Cancer fatalism among African-Americans: A literature review. Nursing Outlook, 44(1), 18–21. [DOI] [PubMed] [Google Scholar]
- Powe BD, & Finnie R (2003). Cancer fatalism: The state of the science. Cancer Nursing, 26(6), 454–467. [DOI] [PubMed] [Google Scholar]
- Ringle CM, Wende S, & Becker J-M (2015). SmartPLS 3 [Computer software]. Bönningstedt: SmartPLS. Retrieved from http://www.smartpls.com [Google Scholar]
- Rosa TL, Ortolano SE, & Dickin KL (2018). Remembering food insecurity: Low-income parents’ perspectives on childhood experiences and implications for measurement. Appetite, 121, 1–8. 10.1016/j.appet.2017.10.035 [DOI] [PubMed] [Google Scholar]
- Rowe SB (2018). Today’s food landscape: Not a pretty picture. Nutrition, 55–56, S16–S17. [Google Scholar]
- Satia JA, Kristal AR, Patterson RE, Neuhouser ML, & Trudeau E (2002). Psychosocial factors and dietary habits associated with vegetable consumption. Nutrition, 18, 247–254. [DOI] [PubMed] [Google Scholar]
- Satorra A, & Bentler PM (2010). Ensuring positiveness of the scaled difference chi-square test statistic. Psychometrika, 75, 243–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satter E (2007). Eating competence: Definition and evidence for the Satter Eating Competence Model. Journal of Nutrition Education and Behavior, 39(5), S142–S153. 10.1016/j.jneb.2007.01.006 [DOI] [PubMed] [Google Scholar]
- Schuster RC, Szpak M, Klein E, Sklar K, & Dickin KL (2019). “I try, I do”: Child feeding practices of motivated, low-income parents reflect trade-offs between psychosocial- and nutrition-oriented goals. Appetite, 136, 114–123. 10.1016/j.appet.2019.01.005 [DOI] [PubMed] [Google Scholar]
- Soederberg Miller LM, & Cassady DL (2015). The effects of nutrition knowledge on food label use. A review of the literature. Appetite, 92(1), 207–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spring B, King AC, Pagoto SL, Van Horn L, & Fisher JD (2015). Fostering multiple healthy lifestyle behaviors for primary prevention of cancer. American Psychologist, 70(2), 75–90. 10.1037/a0038806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suleski J, & Ibaraki M (2010). Scientists are talking, but mostly to each other: a quantitative analysis of research represented in mass media. Public Understanding of Science, 19(1), 115–125. [Google Scholar]
- Tanner SA, McCarthy MB, & O’Reilly SJ (2019). Exploring the roles of motivation and cognition in label-usage using a combined eye-tracking and retrospective think aloud approach. Appetite, 135, 146–158. 10.1016/j.appet.2018.11.015 [DOI] [PubMed] [Google Scholar]


