Abstract
Purpose
The coronavirus disease 2019 (COVID-19) pandemic may increase demand for healthcare professionals (HCPs), either because of a HCP shortage due to illness or because of the need to increase surge capacity. Final-year medical students are one of the resources potentially available to expand the workforce. There is a need to explore the willingness of final-year medical students to meet this demand, examine their perceived competence, and determine how their overall perceived competence correlates with their willingness.
Methods
A cross-sectional study using a self-administered electronic questionnaire was used. The questionnaire included demographic data, students’ self-perceived competence derived from the patient care theme of the Saudi Medical Education Directives (SaudiMED) framework, and their willingness to be measured on a 5-point Likert scale. The study targeted final-year medical students at King Saud University, Riyadh, Saudi Arabia.
Results
The number of participants was 134 (56.1% response rate), of whom 47 students (34.3%) were willing to work, while 31 (23.1%) were somewhat willing. The mean total self-perceived-competence score was 58.36/88 (66.3%). Demonstration of essential clinical skills had the highest mean score 11.48/16 (71.8%) among learning outcomes. There was a positive moderate correlation between willingness and mean perceived-competence score (Spearman correlation coefficient=0.45, p<0.001).
Conclusion
Fifty-seven percent of medical students were willing to work as part of the healthcare workforce during the COVID-19 pandemic. Better overall self-perceived competence appeared to correlate with more willingness. Students perceive themselves to be more competent in essential clinical skills. Appropriate training and supervision are suggested in all tasks assigned to them, with additional care required in areas with a lower perceived competence, such as prescription writing and essential clinical procedures.
Keywords: medical education, disaster medicine, health personnel, professional competence
Introduction
On March 12, 2020, the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak a pandemic.1 One of the hallmarks of this pandemic is the infection of healthcare providers, which consequently leads to a shortage in the workforce.2 In addition, the occurrence of large-scale community transmission necessitates a larger healthcare workforce. This has led countries to adopt multiple strategies to increase the surge capacity.3 China dispatched 41,600 healthcare workers to its epicenter in the city of Wuhan in Hubei province,4 while the UK called on 65,000 retired physicians and nurses to re-register and become part of the healthcare task force.5
The WHO office for Europe recommends that final-year medical students within their limits of competence should be considered to join the task force.3 The Association of American Medical Colleges (AAMC) stresses that medical students should only care directly for patients, providing that student participation is voluntary, if there is a critical healthcare workforce need, it causes no disruption to their learning activities, and it falls within their level of competence.6 Medical students are clinicians-in-training in addition to their role as learners, and can serve in many clinical roles.7
In severely hit central Switzerland, medical students expressed great willingness to participate as part of a swab team. They participated voluntarily after training, taking a total of 6700 swabs with no incidence of COVID-19 among them.8 Likewise, a university hospital in Denmark employed final-year medical students as temporary residents, ventilator therapy assistants, and nursing assistants.9
When medical students were compared with nursing and pharmacy students, they were found to be more willing to work during contagious diseases outbreaks. Being more knowledgeable about contagious diseases might have contributed to their increased willingness.10 There are some suggestive, if inconsistent, findings that knowledge and training influence willingness to work during a disaster; however, the association between competency and willingness is unclear.11
Despite being near or at graduation, research has suggested that medical students still have deficiencies in essential competencies. For example, even after graduation, medical students have difficulties obtaining symptom-based medical history.12 Furthermore, a systematic review found that final-year medical students lack self-confidence, knowledge, and skills when it comes to prescribing.13 When 27 medical students performed simulations of the removal of contaminated gloves, only two demonstrated correct donning and doffing techniques.14
It has been suggested that the participation of students should be voluntary and within their level of competence. However, it is necessary to explore the willingness of final-year medical students to work in the case of critical healthcare workforce need. Additionally, an understanding of the areas in which students perceive themselves to be most competent would guide how much training and supervision they should receive before deploying them in case a need emerges. Finally, the association between willingness, self-perceived competence, and demographic factors was explored.
Methods
Study Setting and Population
This was a cross-sectional study using a self-administered electronic questionnaire. It was conducted during the month of May 2020 targeting final (fifth)-year medical students at the College of Medicine at King Saud University (KSU), which is a public university located in Riyadh, Saudi Arabia. There were 239 students (58.4% of whom are males) enrolled in the final year.
Study Instruments
KSU College of Medicine applies a competency-based curriculum in accordance with the SaudiMED Framework. This framework consists of six major themes describing expected physician duties and obligations. The second theme, “patient care”, contains five learning outcomes concerned with essential clinical and interpersonal skills, and these outcomes are further broken down into 22 enabling competencies.15 In this study, the self-perceived competence part of the questionnaire was measured using a 4-point Likert scale (1=incompetent, 2=somewhat incompetent, 3=somewhat competent, 4=competent) for each of the 22 competencies; giving a total score in the range 22–88 for self-perceived competence. Willingness to report to work was assessed using a 5-point Likert scale (1=not willing, 2=somewhat not willing, 3=undecided, 4=somewhat willing, 5=willing). Demographic variables included age, gender, marital status, grade point average (GPA), history of chronic medical problems, volunteering experience, and previous summer clinical training.
The questionnaire included a pilot test for 10 fourth-year students. Pilot testing showed no problems with access to the survey. There were some typographic errors and disarrangement of answer choices, which were corrected. Also, students did not understand the word “amelioration” in one of the questions, which was then clarified by insertion of the synonym “improvement” in parenthesis.16 After the pilot testing, the questionnaire was sent to final-year students’ emails and electronic messaging groups, with a weekly reminder over a period of three weeks.
Statistical Analysis
Data were analyzed using SPSS 21.0 statistical software (IBM Corporation, Armonk, NY, USA). Internal consistency of the 22-item self-perceived competence part of the questionnaire was measured using Cronbach’s alpha. Descriptive statistics (frequencies, percentages, mean, median, and standard deviation [SD]) were used to describe categorical and quantitative variables. Student’s t-test and a one-way analysis of variance (ANOVA) test were used to compare the mean values of quantitative variables in relation to the categorical outcome variable. Spearman correlation test was used to measure the linear association between the willingness Likert scale score and mean perceived-competence scores. A p-value of ≤0.05 was used to report statistical significance.
Ethical Considerations
Ethical approval (No. E-20-4935) was obtained from the institutional review board (IRB) at the KSU College of Medicine on May 12, 2020. Participants were informed about the rationale for the research, and that the information provided would be treated confidentially. The survey contained the informed consent form at the top of the page, to be viewed prior to voluntary participation. To enhance participation, students were incentivized with the option to participate in a raffle for five (200 Saudi Riyal) gift cards.17
Results
Sociodemographic Characteristics
In total, 134 students participated, representing a response rate of 56.1%. Ninety-five (70.9%) respondents were male and only one participant (0.3%) was married. Most of the participants (n=71, 53.0%) had a very good grade point average (GPA). Twenty students (14.9%) had chronic diseases, seven (5.2%) had respiratory illnesses, and five (3.7%) took medications that suppressed immunity. The distribution of sociodemographic characteristics of study participants is shown in Table 1.
Table 1.
Distribution of Sociodemographic Characteristics of Study Participants (n=134)
| Sociodemographic Characteristics | Number of Students (%) | Mean Perceived Competence Scores±SD, P-Value | Mean Willingness Scores±SD, P-Value |
|
|---|---|---|---|---|
| Gender | Male | 95 (70.9) | 59.85±11.75 | 3.66±1.23 |
| Female | 39 (29.1) | 54.72±11.58 | 3.72±1.23 | |
| p=0.023* | p=0.815 | |||
| GPA | Excellent | 36 (26.9) | 57.53±13.82 | 3.78±1.31 |
| Very good | 71 (53) | 58.42±11.71 | 3.72±1.16 | |
| Good | 27 (20.1) | 59.3±9.76 | 3.44±1.28 | |
| p=0.843 | p=0.526 | |||
| Have any chronic medical problems | Yes | 20 (14.9) | 60.2±11.12 | 3.5±1.4 |
| No | 114 (85.1) | 58.04±12.04 | 3.71±1.2 | |
| p=0.455 | p=0.48 | |||
| Have previous volunteering experience | Yes | 104 (77.6) | 59.4±11.84 | 3.72±1.25 |
| No | 30 (22.4) | 54.73±11.54 | 3.53±1.14 | |
| p=0.058 | p=0.46 | |||
| Previously took clinical summer training | Yes | 109 (81.3) | 59.16±11.89 | 3.77±1.22 |
| No | 25 (18.7) | 54.88±11.51 | 3.28±1.17 | |
| p=0.105 | p=0.07 | |||
| Willingness to work in case of critical healthcare workforce need | Not willing | 7 (5.2) | 47.71±10.28 | – |
| Somewhat not willing | 18 (13.4) | 51.67±14.02 | – | |
| Undecided | 32 (23.9) | 55.91±10.45 | – | |
| Somewhat willing | 31 (23.1) | 57.61±6.66 | – | |
| Willing | 46 (34.3) | 64.8±11.92, | – | |
| p<0.001 | ||||
| Total | 134 | 58.36±11.89 | 3.68±1.22 | |
Note: *p<0.05.
Abbreviations: GPA, grade point average; SD, standard deviation.
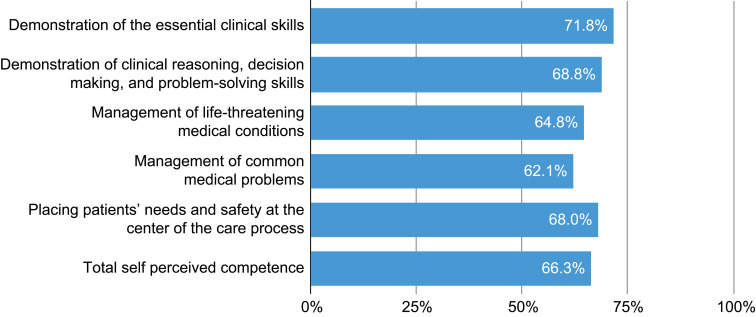
Willingness and Self-Perceived Competence
Forty-seven medical students (34.3%) were willing to work, while 31 (23.1%) were somewhat willing. The internal consistency for the 22-item self-perceived competence part of the questionnaire was high (Cronbach’s alpha=0.93). The mean total score was 58.36/88 (66.3%) ±11.89, with a median of 59/88. Demonstration of essential clinical skills had the highest mean score of 11.48/16 (71.8%) among learning outcomes, while management of common medical problems had the lowest mean score of 19.87/32 (62.1%). Figure 1 shows mean score percentages in learning outcomes. Within those learning outcomes, the competency with the highest mean score (3.31/4) was obtaining an accurate and comprehensive medical history, while the lowest (2.06/4) was demonstrating the skills of writing an appropriate prescription. Table 2 shows the distribution of students’ self-perceived competence for each enabling competency.
Figure 1.
Learning outcomes mean score percentages (n=134).
Table 2.
Distribution of Students’ Self-Perceived Competence for Each Enabling Competency (n=134)
| Learning Outcome, Mean Score (%) | Enabling Competency | Incompetent (%) |
Somewhat Incompetent (%) | Somewhat Competent (%) | Competent (%) | Mean Score (%) |
|---|---|---|---|---|---|---|
| 1. Demonstration of essential clinical skills 11.48/16 (71.78) | 1.1. Obtain an accurate and comprehensive medical history | 1 (0.7) | 16 (11.9) | 58 (43.3) | 59 (44) | 3.31 (82.8) |
| 1.2. Perform a complete systematic physical examination | 6 (4.5) | 31 (23.1) | 63 (47) | 34 (25.4) | 2.93 (73.3) | |
| 1.3. Perform competently the essential clinical procedures | 29 (21.6) | 53 (39.6) | 39 (29.1) | 13 (9.7) | 2.27 (56.8) | |
| 1.4. Critically analyze clinical data obtained through history, physical examination, and investigation |
1 (0.7) | 31 (23.1) | 72 (53.7) | 30 (22.4) | 2.98 (74.5) | |
| 2. Demonstration of clinical reasoning, decision making, and problem-solving skills 5.5/8 (68.75) | 2.1. Demonstrate reasoning skills to formulate and prioritize a differential diagnosis | 5 (3.7) | 23 (17.5) | 73 (54.5) | 33 (24.6) | 3 (75) |
| 2.2. Develop a management strategy taking into consideration the priorities of the patient’s problem (s) | 15 (11.2) | 54 (40.3) | 48 (35.8) | 17 (12.7) | 2.5 (62.5) | |
| 3. Management of life-threatening medical conditions 5.18/8 (64.75) | 3.1. Recognize and assess life or organ threatening conditions | 18 (13.4) | 35 (26.1) | 58 (43.3) | 23 (17.2) | 2.64 (66) |
| 3.2. Manage common medical emergencies | 21 (15.7) | 43 (32.1) | 47 (35.1) | 23 (17.2) | 2.54 (63.5) | |
| 4. Management of common medical problems 19.87/32 (62.09) | 4.1. Demonstrate the importance of psychosocial, spiritual, religious, and cultural factors in patient management | 5 (3.7) | 26 (19.4) | 65 (48.5) | 38 (28.4) | 3.01 (75.3) |
| 4.2. Select and apply the most appropriate and cost-effective diagnostic procedures | 25 (18.7) | 52 (38.8) | 43 (32.1) | 14 (10.4) | 2.34 (58.5) | |
| 4.3. Manage appropriately patients with acute and chronic physical and mental problems | 23 (17.2) | 60 (44.8) | 43 (32.1) | 8 (6) | 2.27 (56.8) | |
| 4.4. Recognize the need for multiple therapeutic modalities to address patient conditions | 18 (13.4) | 51 (38.1) | 51 (38.1) | 14 (10.4) | 2.46 (61.5) | |
| 4.5. Demonstrate the skills to write an appropriate prescription | 36 (26.9) | 60 (44.8) | 32 (23.9) | 6 (4.5) | 2.06 (51.5) | |
| 4.6. Recognize the principles of the amelioration of suffering and disability rehabilitation and palliative care, including appropriate pain management | 29 (21.6) | 61 (45.5) | 34 (25.4) | 10 (7.5) | 2.19 (54.8) | |
| 4.7. Make decisions in partnership with patients and/or their carers | 14 (10.4) | 39 (29.1) | 58 (43.3) | 23 (17.2) | 2.67 (66.8) | |
| 4.8. Demonstrate effective counseling skills | 7 (5.2) | 31 (23.1) | 69 (51.5) | 27 (20.1) | 2.87 (71.8) | |
| 5. Placing patients’ needs and safety at the center of the care process 16.33/24 (68.04) | 5.1. Demonstrate knowledge and skills in the area related to patient safety eg, root-cause analyses, safe prescription and procedures | 12 (9) | 50 (37.3) | 54 (40.3) | 18 (13.4) | 2.58 (64.5) |
| 5.2. Analyze the aftermath of medical errors | 25 (18.7) | 53 (39.6) | 40 (29.9) | 16 (11.9) | 2.35 (58.8) | |
| 5.3. Demonstrate reflection and learning from errors | 16 (11.9) | 23 (17.2) | 60 (44.8) | 35 (26.1) | 2.85 (71.3) | |
| 5.4. Identify and manage clinical risks | 13 (9.7) | 47 (35.1) | 58 (43.3) | 16 (11.9) | 2.57 (64.3) | |
| 5.5. Apply the essential principles of infection prevention and control in health care settings | 6 (4.5) | 27 (20.1) | 59 (44) | 42 (31.3) | 3.02 (75.5) | |
| 5.6. Report any concurrent physical, social, or mental ailment that would affect patient care to appropriate authorities | 9 (6.7) | 31 (23.1) | 52 (38.8) | 42 (31.3) | 2.95 (73.8) |
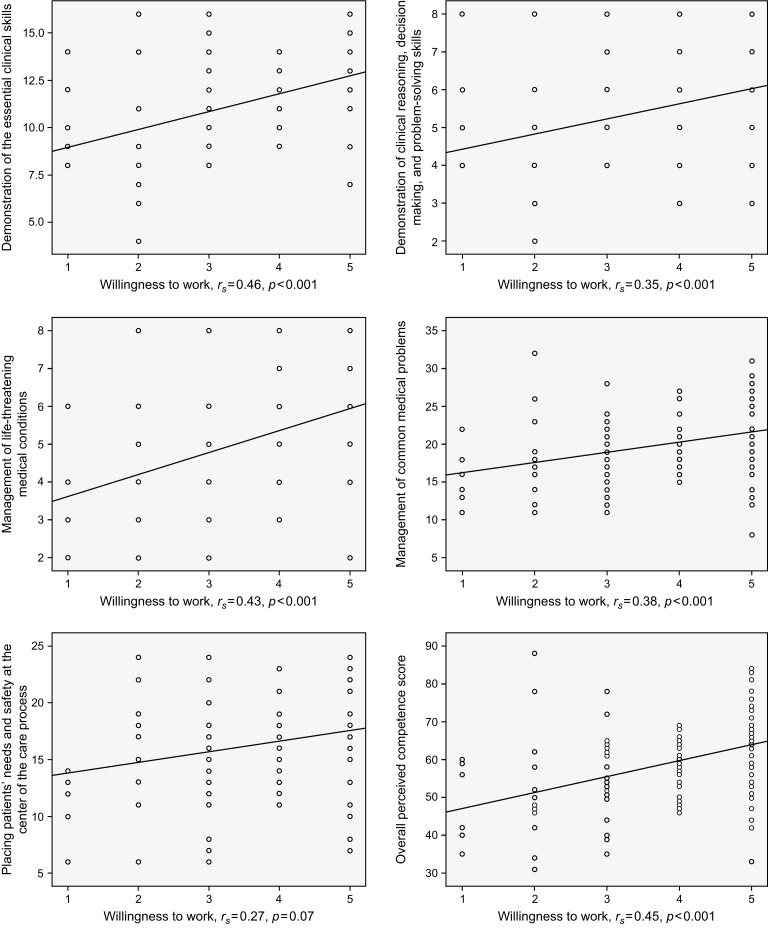
Correlation Between Willingness and Self-Perceived Competence
There was a positive moderate correlation between willingness and mean total perceived-competence score (Spearman correlation coefficient [rs]=0.45, p<0.001). Comparing the correlation of different learning outcomes with willingness, demonstration of the essential clinical skills had the highest correlation (rs =0.46, p<0.001). Figure 2 shows scatterplots illustrating the correlation between willingness to work and overall perceived competence and individual learning outcomes.
Figure 2.
Correlation between willingness to work and overall perceived competence and individual learning outcomes.
Discussion
The results of this study showed that 57.4% of the medical students were willing to work in the case of critical healthcare workforce need caused by the COVID-19 pandemic. When healthcare students’ attitudes towards Middle East respiratory syndrome coronavirus (MERS-CoV) were examined, 39.2% disagreed with the statement about their willingness to do clinical rotations at a hospital where MERS-CoV patients were treated.19 On the other hand, a high proportion (74%.2) of Spanish medical and nursing students expressed willingness to take care of patients with COVID-19 if required.20 Similarly, 80% of Ugandan medical students from all the years of study expressed willingness to participate in the frontline response to the COVID-19 pandemic.21 Of note, there were differences in the targeted population, timing of data collection in relation to the state of the pandemic or epidemic in the country, and phrases and Likert scale questions used to assess willingness. These factors should be taken into consideration when attempting to compare and contrast the aforementioned studies.
Willingness correlated moderately with level of self-perceived competence in essential clinical and interpersonal skills. This finding might support the hypothesis that medical students with a better self-perceived competence are more willing to work in the case of a large-scale outbreak with respiratory transmission, such as with COVID-19. Nevertheless, such a notion needs to be supported by objective measurement of competence and a longitudinal study to establish the direction of the association.
A previous study on medical students showed that objectively measured and self-perceived competence correlated better with “soft” skills, while there was a poorer correlation with clinical skills.18 History taking was the competency in which students perceived themselves to be most competent. Fortunately, history taking does not necessarily have to be carried out face-to-face, as it can be done through virtual visits. Applying essential principles of infection prevention and control was second in terms of perceived-competence scores. A previous study on medical students in eastern Saudi Arabia revealed poor knowledge of infection control and standard precautions.22 The same study also found that study year correlated with a higher level of knowledge.22 This might explain why high scores were found in our study, since only final-year students were included.
In central Switzerland, students helped during the surge by carrying out the swabbing procedure.8 However, performing essential clinical procedures was one of the competencies with the lowest scores in this study. Furthermore, the skills of writing a prescription had the lowest perceived competency; however, prescribing can be done electronically and this, therefore, provides the opportunity to engage the help of students. The literature indicates that the correlation between self-perceived competence and objectively assessed performance is either absent or discordant for essential clinical procedures, and it is weak for prescribing skills.13,23,24 However, these findings, and the fact that both competencies were among the lowest in perceived competence, should not discourage the assignment of students to these tasks, but raises the need for additional care in training and supervision in this instance.
Interestingly, students with higher GPAs had higher willingness scores and lower perceived-competence scores, although neither difference was statistically significant. There is evidence that medical students who volunteered at a free clinic had higher cumulative GPAs than those who did not.25 Further, Carr et al found a weak correlation between medical students’ GPAs and their performance as junior doctors.26
Few students with chronic medical illnesses, such as respiratory illnesses, or who required medications that suppresses immunity, were included in this study. Therefore, it is important to identify vulnerable students in order to protect them. For instance, they could be assigned to lower risk tasks and areas. While previous research on healthcare providers has indicated that the presence of personal health issues is a barrier to willingness to work in a public health emergency, there were no significant differences in willingness between students with and without chronic medical problems in our study.11 Students who had undergone previous clinical summer training had a significantly higher willingness to work, which is reasonable as both activities are consistent in that they are elective.
Limitations
This study has multiple limitations. For example, the study relied on self-perceived competence, it measured association at a single point in time, and it included students from a single medical college. In addition, study participants were sampled using a non-probability sampling technique.
Conclusions
In summary, more than one-third of medical students are willing to work as part of the healthcare workforce during the COVID-19 pandemic. Better overall self-perceived competence appears to correlate with greater willingness. Students perceive themselves to be more competent in some areas than others. Appropriate training and supervision are suggested for all tasks assigned to them, with additional care required in some tasks with a lower perceived competence. Some students are vulnerable to serious infection, and it is, therefore, essential to identify them to protect them. Recommendations for future research include measuring competence objectively, following the association between willingness and competence longitudinally for better ascertainment of the direction of the association, further exploring the reasons why some students were less willing or not willing to work, and incorporating qualitative methods for better insight into students’ thoughts and feelings with regard to their willingness.
Acknowledgments
We would like to thank the final-year medical students who participated in this study. We also appreciate the help from KSU College of Medicine Students’ Council in sending the questionnaires to the students, and the Deanship of Scientific Research and the researcher support unit at KSU for their technical support. In addition, we would like to express our gratitude to the peer reviewers’ comments, which helped improve this manuscript and clarify the description of our study. English language review was provided by The Charlesworth Group (www.cwauthors.com).
Funding Statement
This study was funded by the College of Medicine Research Center, Deanship of Scientific Research, King Saud University, Riyadh, KSA.
Abbreviations
AAMC, Association of American Medical Colleges; ANOVA, Analysis of variance; GPA, Grade point average; HCP, healthcare professional; IRB, Institutional review board; KSU, King Saud University; MERS-CoV, Middle East respiratory syndrome coronavirus; WHO, World Health Organization.
Data Sharing Statement
The authors declare that they had full access to all of the data in this study, and the authors take complete responsibility for the integrity of the data and the accuracy of the data analysis. All original data are available in the Department of Family and Community Medicine, KSU, Riyadh, Saudi Arabia. Data used to support the findings of this study are available from the corresponding author upon request.
Author Contributions
All authors made substantial contributions to the conception and design of the study, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.WHO director-general’s opening remarks at the media briefing on COVID-19; 2020. Available from: https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020. Accessed May3, 2020.
- 2.3387 cases of healthcare workers infected with novel coronavirus disease 2019; 2020. Available from: https://news.ifeng.com/c/7uKe45oGSZM. Accessed May3, 2020 Chinese.
- 3.Strengthening the health system response to COVID-19 recommendations for the WHO European region. Copenhagen: WHO Regional Office for Europe; 2020. 2:5 Available from: https://www.euro.who.int/__data/assets/pdf_file/0003/436350/strengthening-health-system-response-COVID-19.pdf. Accessed May3, 2020. [Google Scholar]
- 4.Wang J, Zhou M, Liu F. Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105:100–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Former docs and nurses told “Your NHS needs you” to tackle greatest global health threat in history. National Health Service England; 2020. Available from: https://www.england.nhs.uk/2020/03/former-docs-and-nurses-told-your-nhs-needs-you-to-tackle-greatest-global-health-threat-in-history/. Accessed May3, 2020. [Google Scholar]
- 6.Whelan A, Prescott J, Young G, Catanese V, McKinney R Guidance on medical students’ participation in direct patient contact activities; 2020. Available from: https://www.aamc.org/system/files/2020-04/meded-April-14-Guidance-on-Medical-Students-Participation-in-Direct-Patient-Contact-Activities.pdf. Accessed May4, 2020.
- 7.Miller DG, Pierson L, Doernberg S. The role of medical students during the COVID-19 pandemic [published online ahead of print, 2020 Apr 7]. Ann Intern Med. 2020;M20–1281. [Google Scholar]
- 8.Klasen JM, Meienberg A, Nickel C, Bingisser R. SWAB team instead of SWAT team: medical students as a frontline force during the COVID-19 pandemic [published online ahead of print, 2020 May 13]. Med Educ. 2020. doi: 10.1111/medu.14224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rasmussen S, Sperling P, Poulsen MS, Emmersen J, Andersen S. Medical students for health-care staff shortages during the COVID-19 pandemic. Lancet. 2020;395:e79–e80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel R, Wattamwar K, Kanduri J, et al. Health care student knowledge and willingness to work in infectious disease outbreaks. Disaster Med Public Health Prep. 2017;11(6):694–700. [DOI] [PubMed] [Google Scholar]
- 11.Chaffee M. Willingness of health care personnel to work in a disaster: an integrative review of the literature. Disaster Med Public Health Prep. 2009;3(1):42–56. [DOI] [PubMed] [Google Scholar]
- 12.Bachmann C, Roschlaub S, Harendza S, Keim R, Scherer M. Medical students’ communication skills in clinical education: results from a cohort study. Patient Educ Couns. 2017;100(10):1874–1881. [DOI] [PubMed] [Google Scholar]
- 13.Brinkman DJ, Tichelaar J, Graaf S, Otten RHJ, Richir MC, van Agtmael MA. Do final-year medical students have sufficient prescribing competencies? A systematic literature review. Br J Clin Pharmacol. 2018;84(4):615–635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.John A, Tomas ME, Hari A, Wilson BM, Donskey CJ. Do medical students receive training in correct use of personal protective equipment? Med Educ Online. 2017;22(1):1264125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.The Committee of Deans of the Colleges of Medicine in the Kingdom of Saudi Arabia. Saudi medical education directives framework’ (saudimed framework); 2017. 15 Available from: https://etec.gov.sa/en/productsandservices/NCAAA/AccreditationProgrammatic/Pages/Medical-Colleges.aspx. Accessed May3, 2020.
- 16.Amelioration. Stedman’s online website. Wolters Kluwer Health; Available from: https://stedmansonline.com/. Accessed May4, 2020. [Google Scholar]
- 17.Singer E, Ye C. The use and effects of incentives in surveys. Ann Am Acad Pol Soc Sci. 2012;645(1):112–141. [Google Scholar]
- 18.Lai NM, Teng CL. Self-perceived competence correlates poorly with objectively measured competence in evidence based medicine among medical students. BMC Med Educ. 2011;11:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Elrggal ME, Karami NA, Rafea B, et al. Evaluation of preparedness of healthcare student volunteers against Middle East respiratory syndrome coronavirus (MERS-CoV) in Makkah, Saudi Arabia: a cross-sectional study. Z Gesundh Wiss. 2018;26(6):607–612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cervera-Gasch Á, González-Chordá VM, Mena-Tudela D. COVID-19: are Spanish medicine and nursing students prepared? [published online ahead of print, 2020 May 28]. Nurse Educ Today. 2020;92:104473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Olum R, Kajjimu J, Kanyike AM, et al. Perspective of medical students on the COVID-19 pandemic: survey of nine medical schools in Uganda. JMIR Public Health Surveill. 2020;6(2):e19847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amin TT, Al Noaim KI, Bu Saad MA, Al Malhm TA, Al Mulhim AA, Al Awas MA. Standard precautions and infection control, medical students’ knowledge and behavior at a Saudi university: the need for change. Glob J Health Sci. 2013;5(4):114–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Barnsley L, Lyon PM, Ralston SJ, et al. Clinical skills in junior medical officers: a comparison of self-reported confidence and observed competence. Med Educ. 2004;38(4):358–367. [DOI] [PubMed] [Google Scholar]
- 24.Katowa-Mukwato P, Banda S. Self-perceived versus objectively measured competence in performing clinical practical procedures by final year medical students. Int J Med Educ. 2016;7:122–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vaikunth SS, Cesari WA, Norwood KV, et al. Academic achievement and primary care specialty selection of volunteers at a student-run free clinic. Teach Learn Med. 2014;26(2):129–134. [DOI] [PubMed] [Google Scholar]
- 26.Carr SE, Celenza A, Puddey IB, Lake F. Relationships between academic performance of medical students and their workplace performance as junior doctors. BMC Med Educ. 2014;14:157. [DOI] [PMC free article] [PubMed] [Google Scholar]