Highlights
-
•
A double caecal appendix is an uncommon anatomical variation with significant surgical implications.
-
•
Patients with double appendix are usually asymptomatic.
-
•
When symptomatic, the problems that may arise from a missed diagnosis have serious health consequences.
-
•
The double appendix can be classified using the Cave-Wallbridge classification.
Keywords: Double caecal appendix, Appendix vermiformis duplex, Appendiceal duplication, Caecum
Abstract
Introduction
A double caecal appendix is an uncommon anatomical variation with significant surgical implications. A few cases of the double caecal appendix have been reported worldwide, mostly in adults. The diagnosis is, usually incidental, typically made intraoperatively.
Case report
We present the case of a 6-month-old boy with an incidental diagnosis of the double appendix during laparotomy for intussusception.
Discussion
The double appendix can be classified using the Cave-Wallbridge classification, which identifies three types of the duplicated appendix: A, B, and C. The complication of appendiceal duplications includes acute appendicitis, colonic perforation, obstruction, bleeding, pain, failure to thrive, abdominal mass. In the case of abdominal pain with diagnostic uncertainty, with appropriate patient selection (without hemodynamic instability), diagnostic laparoscopy may be offered as an initial intraoperative evaluation, and if the procedure cannot be safely completed laparoscopically, it can be converted to a laparotomy.
Conclusion
Although uncommon, knowledge of appendiceal duplication is of great significance in the surgical patient, as a missed diagnosis or delay in diagnosis in symptomatic patients may result in increased morbidity and possibly mortality secondary to sepsis, with its medico-legal ramifications in today's practice of medicine.
1. Introduction
Double caecal appendix was first observed by Picoli in 1892; with a reported incidence ranging from 0.004% to 0.009% [4,5]. Patients with double appendix are usually asymptomatic with the majority diagnosed intraoperatively, a few diagnosed during an autopsy examination, and rarely preoperatively on barium enema [6]. When symptomatic, the problems that may arise from a missed diagnosis have serious health consequences [5]. Here, we present the case of a 6-month-old boy with an incidental diagnosis of the double appendix during laparotomy for intussusception; we aim to highlight the rarity of the condition and the potential surgical implications.
This work has been reported in line with the SCARE criteria [7].
2. Case report
A 6-month-old boy presented with a history of excessive crying, bilious vomiting, and abdominal distension for 48 h and constipation for nearly 24 h. He had a prior diagnosis of upper respiratory tract infection and was recently started formula milk feeds. On examination, he was febrile, temperature 37.9 °C (axilla), dehydrated. The abdomen was distended, with hypoactive bowel sound, and peritonitic to palpation, with a palpable mass in the right lower quadrant. Digital rectal examination revealed bloody mucoid stool. Complete blood count documented elevated white cell count (30,000/mm3), hematocrit of 35 g/dl, and plain radiography of the abdomen and pelvis revealed air-fluid level. The patient was resuscitated, started on broad-spectrum antibiotic and then taken urgently to the operating room for exploration with a working diagnosis of bowel obstruction secondary to intussusception.
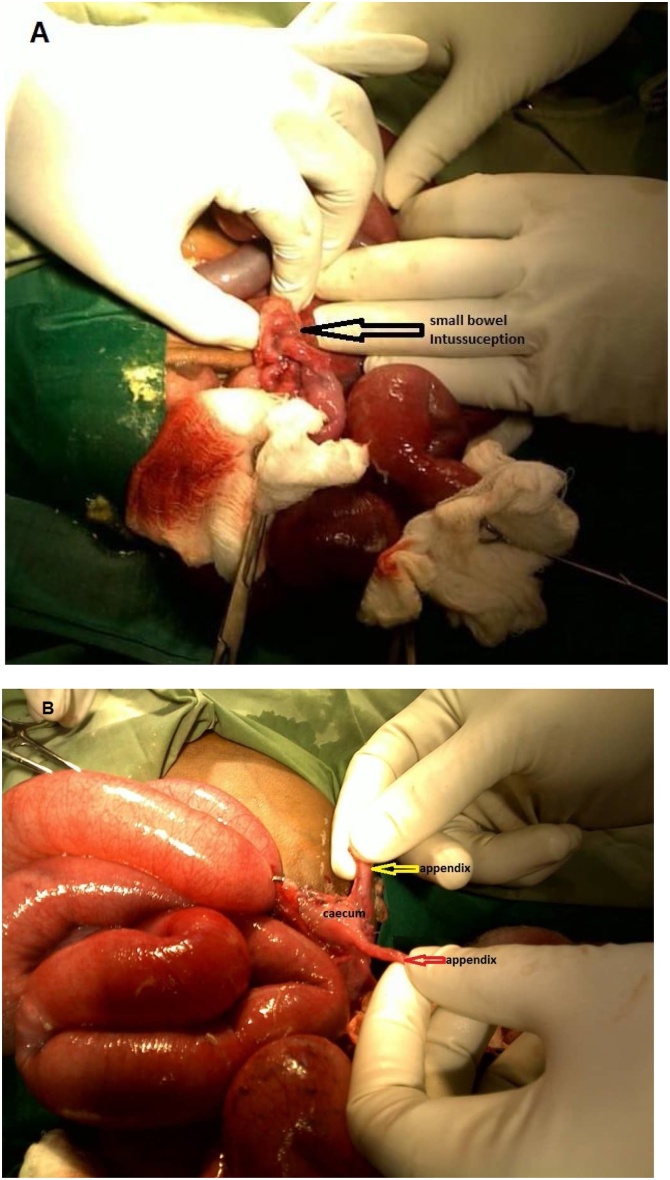
At laparotomy, the patient was found to have an ileo- ileal intussusception (10 cm from the ileocaecal junction), with enlarged mesenteric lymph nodes. Also noted was a single caecum with two completely separate appendices (Fig. 1). The portion of the bowel involved in the intussusception appeared ischemic and the intussusception was unable to be reduced. Ileocaecal resection was performed, and intestinal continuity was restored via a hand-sewn, end-to-end single layer ileocolic anastomosis with absorbable sutures. The anastomosis was then inspected for patency and integrity. The mesenteric defect was closed with a running absorbable suture.
Fig. 1.
A: Intraoperative photo demonstrating an ileo-ileal intussusception (indicated by arrow). B: Intraoperative photo demonstrating a Type B(1) duplication of the appendix, single caecum (labeled) with two appendices (indicated by arrows), each originating at different locations.
Postoperatively, the patient did well and was discharged home on postoperative day seven.
Histopathological examination revealed compact arranged small lymphocytes frequently intermingled with enlarged follicles, a normal cecum, and also confirmed our macroscopic diagnosis of the double appendix, which were normal appearing.
3. Discussion
Double caecal appendix is an extremely uncommon malformation. It is found in 2 in 50,000 cases that have had surgery for appendicitis [4]. About 141 cases of the double caecal appendix have been reported worldwide [8]. It is usually diagnosed incidentally. When double appendix is diagnosed in childhood, the patient should be screened for associated congenital anomalies including genitourinary, intestinal, vertebral, or other malformations [9,10].
The double appendix can be classified using the Cave-Wallbridge classification, which identifies three types of the duplicated appendix: A, B, and C [3,11]. In type A duplication, both appendices have a common base (single caecum). It is also referred to as incomplete duplication. Type B duplication involves a single caecum with two appendices, each originating at different locations. This is a complete appendiceal duplication. Type B classification can be subdivided into Type B1 and Type B2; with type B1 involving two appendices symmetrically placed on either side of the ileocecal valve, and type B2 also known as the “taenia colic” type in which one appendix comes off the caecum at the typical site while the other arises from the caecum along the lines of the taenia at a varying distance from the first. Finally, Type C duplication, involves duplicity of the caecum, with each caecum bearing its proper appendix [3,11].
The complication of appendiceal duplications includes acute appendicitis [[1], [2], [3]], colonic perforation in case of colonic duplication [12], other complications include obstruction, bleeding, pain, failure to thrive, abdominal mass [9,13].
In our case, as with most published cases, the diagnosis of double appendix was made intraoperatively during laparotomy for acute abdomen secondary to intussusception. In the case of abdominal pain with diagnostic uncertainty, in the right clinical setting, i.e., appropriate patient selection (without hemodynamic instability), a surgeon with laparoscopic expertise, and facility with the laparoscopic infrastructure, exploratory laparoscopy may be offered as an initial intraoperative evaluation, and if the procedure cannot be safely completed laparoscopically, it can be converted to a laparotomy [14]. Laparoscopic procedures are associated with less postoperative pain, faster recovery, and lower wound infection rates compared to laparotomy [15,16]. However, this should be a shared decision between the doctor and patient. We did not consider exploratory laparoscopy because the facility in which the operation was performed was not equipped for laparoscopic procedures.
4. Conclusion
Although uncommon, knowledge of appendiceal duplication is of great significance in the surgical patient, as a missed diagnosis or delay in diagnosis in symptomatic patients may result in increased morbidity and possibly mortality secondary to sepsis, with its medico-legal ramifications in today's practice of medicine.
Declaration of Competing Interest
MIO, KS and GOO have nothing to disclose.
Funding
GOO is supported by National Institutes of HealthT32 CA 009599 and the MD Anderson Cancer Center support grant (P30 CA016672).
Ethical approval
This study is exempt from ethnical approval from my institution
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
MIO contributed in the study concept and writing of the manuscript.
KS contributed in the writing of the manuscript.
GOO contributed in the writing of the manuscript.
Registration of research studies
N/A.
Guarantor
Dr. Mojirola I. Olarinoye-Alegbejo.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Contributor Information
Mojirola I. Olarinoye-Alegbejo, Email: kamisuccess@yahoo.com.
Kache Steve, Email: kachesteve@yahoo.com.
Gabriel O. Ologun, Email: goologun@mdanderson.org.
References
- 1.Ayoub Kusay, Kayali Sadallah, Fateh Dabbagh M., Banjah Bassel. Acute single appendicitis in a female with a duplicated appendix. J. Surg. Case Rep. 2018;2018 doi: 10.1093/JSCR/RJY132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mushtaque M., Mehraj A., Khanday S.A., Dar R.A. Double appendicitis. Int. J. Clin. Med. 2012;03:60–61. doi: 10.4236/ijcm.2012.31013. [DOI] [Google Scholar]
- 3.Wallbridge P.H. Double appendix. Br. J. Surg. 1962;50:346–347. doi: 10.1002/bjs.18005022124. [DOI] [PubMed] [Google Scholar]
- 4.Collins D.C. A study of 50,000 specimens of the human vermiform appendix. Surg. Gynecol. Obstet. 1955;101:437–445. [PubMed] [Google Scholar]
- 5.Kjossev K.T., Losanoff J.E. Duplicated vermiform appendix. Br. J. Surg. 1996;83:1259. http://www.ncbi.nlm.nih.gov/pubmed/8983623 (accessed March 10, 2020) [PubMed] [Google Scholar]
- 6.Kothari A.A., Yagnik K.R., Hathila V.P. Duplication of vermiform appendix. J. Postgrad. Med. 2004;50:285–286. http://www.ncbi.nlm.nih.gov/pubmed/15623973 (accessed March 10, 2020) [PubMed] [Google Scholar]
- 7.Agha R.A., Borrelli M.R., Farwana R., Koshy K., Fowler A.J., Orgill D.P., Zhu H., Alsawadi A., Noureldin A., Rao A., Enam A., Thoma A., Bashashati M., Vasudevan B., Beamish A., Challacombe B., De Wilde R.L., Machado-Aranda D., Laskin D., Muzumdar D., D’cruz A., Manning T., Healy D., Pagano D., Goel P., Ranganathan P., Pai P.S., Raja S., Ather M.H., kadioäžlu H., Nixon I., Mukherjee I., Gómez Rivas J., Raveendran K., Derbyshire L., Valmasoni M., Chalkoo M., Raison N., Muensterer O., Bradley P., Roberto C., Afifi R., Rosin D., Klappenbach R., Wynn R., Giordano S., Basu S., Surani S., Suman P., Thorat M., Kasi V. The SCARE 2018 statement: Updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2018;60:132–136. doi: 10.1016/j.ijsu.2018.10.028. [DOI] [PubMed] [Google Scholar]
- 8.Nageswaran H., Khan U., Hill F., Maw A. Appendiceal duplication: a comprehensive review of published cases and clinical recommendations. World J. Surg. 2018;42:574–581. doi: 10.1007/s00268-017-4178-1. [DOI] [PubMed] [Google Scholar]
- 9.Eroglu E., Erdogan E., Gundogdu G., Dervisoglu S., Yeker D. Duplication of appendix vermiformis: a case in a child. Tech. Coloproctol. 2002;6:55–57. doi: 10.1007/s101510200010. [DOI] [PubMed] [Google Scholar]
- 10.Arda I.S., Şenocak M.E., Hiçsönmez A. Duplication of vermiform appendix: case report and review of the literature. Pediatr. Surg. Int. 1992;7:221–222. doi: 10.1007/BF00175847. [DOI] [Google Scholar]
- 11.Cave A.J.E. Appedix Vermiformis Duplex. J. Anat. 1936;70:283–292. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1249127/ (accessed March 10, 2020) [PMC free article] [PubMed] [Google Scholar]
- 12.Bulut S.P., Cabioǧlu N., Akinci M. Perforated double appendicitis: horseshoe type. Turkish J. Surg. 2016;32:134–136. doi: 10.5152/UCD.2015.2857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim E.P., McClenathan J.H. Unusual duplication of appendix and cecum: extension of the Cave-Wallbridge classification. J. Pediatr. Surg. 2001;36:18. doi: 10.1053/jpsu.2001.26400. [DOI] [PubMed] [Google Scholar]
- 14.Agrusa A., Romano G., Di Buono G., Giuseppe F., Chianetta D., Sorce V., Billone V., Cucinella G., Gulotta G. Acute appendicitis and endometriosis: retrospective analysis in emergency setting. GIOG. 2013;35:728–732. doi: 10.11138/giog/2013.35.6.728. [DOI] [Google Scholar]
- 15.Chung R.S., Rowland D.Y., Li P., Diaz J. A meta-analysis of randomized controlled trials of laparoscopic versus conventional appendectomy. Am. J. Surg. 1999;177:250–256. doi: 10.1016/S0002-9610(99)00017-3. [DOI] [PubMed] [Google Scholar]
- 16.Li X., Zhang J., Sang L., Zhang W., Chu Z., Li X., Liu Y. Laparoscopic versus conventional appendectomy - a meta-analysis of randomized controlled trials. BMC Gastroenterol. 2010;10 doi: 10.1186/1471-230X-10-129. [DOI] [PMC free article] [PubMed] [Google Scholar]