Abstract
Background and purpose
Wide-necked bifurcation aneurysms pose a significant challenge to the treating clinician. The Contour Neurovascular System embolization device is a novel tool for the treatment of such intracranial aneurysms. We report on our experience with this device.
Methods
Prospective clinical and radiological data were collected for all patients treated with the Contour device at our center. All our patients were treated on an elective basis.
Results
We have treated 11 patients successfully with the Contour device to date. All patients were women with a mean (SD) age of 65.0 (6.4) years. In total, four basilar tip, two internal carotid artery, three middle cerebral artery, one anterior communicating artery, and one superior cerebellar artery aneurysms were treated. At 1-year follow-up, complete occlusion (Raymond Class 1) was seen in 55.56% (5/9) of cases, with 44.44% (4/9) having small neck remnants (Raymond Class 2). One patient declined 1-year catheter angiography and another had no further follow-up due to an unrelated medical condition. For six patients, 2-year radiological follow-up is available and shows stability. At 6 weeks, nine of the 11 patients had a modifed Rankin Scale score of 0, with two patients scoring 1 for headaches. Two patients had thromboembolic events, but there were no complications leading to permanent neurological disability or death. We additionally had three patients where the Contour device was attempted but was unable to be successfully used.
Conclusion
Initial results are promising although larger case numbers and longer follow-up are necessary to draw further conclusions on the utility and risk profile of this new device.
Keywords: aneurysm, device, angiography
Introduction
Endovascular treatment (EVT) is currently recognized as the preferred therapeutic modality for intracranial aneurysms, and since the initial introduction of Guglielmi detachable coils over two decades ago, its position has been solidified by several notable studies.1–5 A plethora of new medical devices with varying indications have been developed for EVT.6–9 However, despite all these options, wide-necked bifurcation aneurysms (WNBA) still pose a significant challenge to the treating clinician. A recent meta-analysis found that complete occlusion rates following EVT of WNBA at 1 year were only 39.8%, suggesting a continuing need for better treatment options.10
The Cerus Endovascular Contour Neurovascular System (CNS; Cerus Endovascular, Fremont, California, USA) is a novel intrasaccular technology for treating intracranial aneurysms of varying morphology including WNBA. The device, shown in figure 1, is a dual-layer radiopaque nitinol memory mesh. Due to its unique shape, it acts as both a flow disrupter and a flow diverter and is designed to reconstruct the natural bifurcation of the artery. It can be deployed using current microcatheter technology and specifically targets the neck of the aneurysm. Figure 2 illustrates the authors’ suggested target zone of the device which, when placed accurately, avoids manipulation of what the authors believe to be the fragile dome of the aneurysm. Additionally, it has no parent vessel component and can be easily resheathed intraoperatively if desired by the operator. Detachment is achieved using an electrolytic device. Sizing is based primarily on the aneurysm neck size and maximum diameter, as shown in table 1. We report here our experience with the device, commenting on the angiographic and clinical outcomes, and discuss the efficacy and safety of the Contour device in relation to other devices available. To the best of our knowledge, this is the first human series with this new device.
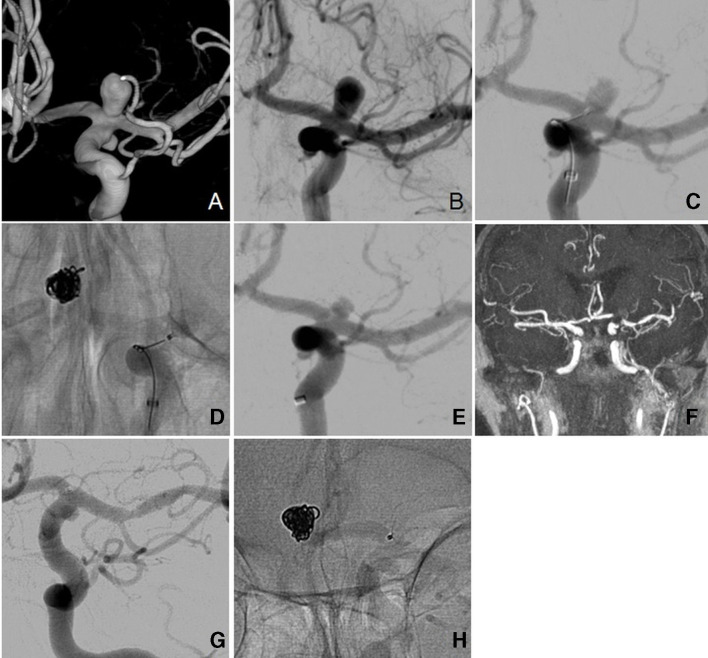
Figure 1.
The Cerus Endovascular Contour Neurovascular System (A–C) including angiographic view (D) showing detachment zone (arrow).
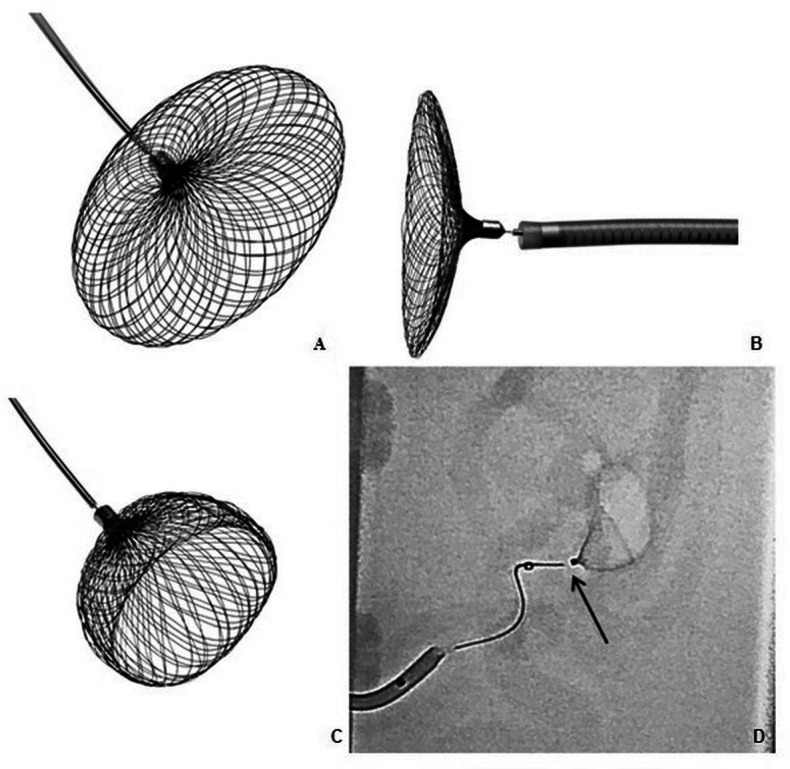
Figure 2.
(A) Target zone of Contour Neurovascular System (CNS) device deployment at the intracranial aneurysm neck and within the equatorial plane. (B) Schematic representation of the CNS device with catheter attached. (C) Schematic representation of the CNS device deployed in the aneurysm showing expected flow diversion. (D) Schematic representation of angiographic view of the CNS device.
Table 1.
Sizing guide for the Contour Neurovascular System
| Catalogue number | Aneurysm neck (mm) | Aneurysm width (mm) |
| CNS05 −5 mm | 2.0–3.0 | 2.0–3.5 |
| CNS07 −7 mm | 3.0–5.0 | 3.0–5.5 |
| CNS09 −9 mm | 4.0–6.0 | 5.0–7.5 |
| CNS11 –11 mm | 5.0–8.0 | 7.0–8.5 |
Materials and methods
Case selection
We collected prospective clinical and radiological data for all patients treated with the CNS. Prior to treatment, all cases were discussed at our neurovascular multidisciplinary team meeting. An aneurysm was considered for treatment if it was unruptured, had a wide neck, and the CNS was considered to be a viable treatment option among other options such as standard coiling. We defined wide-necked aneurysms as having a neck diameter of ≥4 mm or a dome-to-neck ratio of <2.11 12 If felt suitable for treatment with the CNS, the clinician proposing treatment met with and explained the treatment and all available alternatives to patients, including clipping, Woven Endobridge (WEB; Sequent Medical, California, USA) and/or stent-assisted coiling. If, after discussion, patients agreed to proceed with the new device, they were scheduled for treatment. All cases were treated on an elective basis and informed consent was obtained along with local ethics board approval.
To date, 14 patients have been treated with the CNS. Of these, three patients had attempted treatment using the CNS, but due to inability to use the device in those instances, other treatment methods were used. The specifics of these cases are described in more detail in the Results section.
Analysis
Baseline clinical data in the form of patient demographics, baseline Glasgow Coma Scale (GCS), and modified Rankin Scale (mRS) were collected. Follow-up mRS at 6 weeks and any complications were recorded, along with immediate post-treatment, 6-month, 1-year, and 2-year radiological follow-up in the form of catheter angiography. In some circumstances contrast-enhanced MR angiography was used as well, but we currently do not routinely use CT angiography as part of our follow-up. Occlusion was quantified using the recognized Raymond–Roy Class classification,.13 Class 1 denotes complete occlusion, Class 2 denotes neck remnant, and Class 3 is a residual aneurysm. Class 1 and Class 2 occlusion were considered satisfactory given the good clinical outcomes described in recent studies, although this is in relation to aneurysms treated with coils and not intrasaccular devices,.14 15
Procedural technique
All cases were performed by the senior author under general anesthetic via standard common femoral artery puncture and an 8F sheath insertion. We do not currently prep patients with antiplatelets prior to the procedure. Intraoperatively, all patients received 5000 units of IV heparin and the activated clotting time was monitored and kept within 2–2.5 times the patient’s baseline. Typically a 6F NeuroMax (Penumbra, Alameda, California, USA) guide sheath was navigated into the target main artery (eg, internal carotid). Distal access catheters comprised either 6F Navien (Covidien, Mansfield, Massachusetts, USA), Cat6 (Stryker Neurovascular, Kalamazoo, Michigan, USA), or Benchmark (Penumbra, Alameda, California, USA). Microcatheter work was done with an XT-27 (Stryker Neurovascular) or a Headway-27 (Microvention Neurovascular, Aliso Viejo, USA) microcatheter and a Synchro 14 guide wire (Stryker Neurovascular). All work was done using biplane imaging. After initial diagnostic runs, aneurysm sizing was done using an intraoperative three-dimensional rotational angiogram. This allowed CNS sizing and access planning. The device was oversized to the equatorial plane of the aneurysm using the sizing chart in table 1. The correctly sized CNS device was carefully inserted and deployed at the aneurysm neck once in a stable position. If incorrectly deployed, the device was resheathed and redeployed in the correct position. This is done to prevent manipulation of the device once deployed. After deployment, post-procedural (immediate and delayed) angiographic runs were performed to assess device placement and for flow/stasis within the aneurysm and to monitor for any immediate complications. We did not routinely use post-procedural dyna CT. Intraoperatively, 500 mg of IV aspirin was given and the patient was discharged on 6 weeks of 75 mg aspirin. Follow-up catheter angiography was subsequently arranged at 6 months, 1 year and 2 years.
Cerus Endovascular provided our institution with the Contour Neurovascular Devices for evaluation, but was not involved in the production of the manuscript.
Results
In our series of 11 patients treated with the CNS device since February 2017, all our patients were women with a mean (SD) age of 65.0 (6.4) years. All patients were treated on an elective basis for incidentally found aneurysms, with one patient (Case 1) having suffered a previous subarachnoid hemorrhage. All patients had a pretreatment GCS of 15 and an admission mRS of 0. In total, four basilar tip, two internal carotid artery (ICA), three middle cerebral artery (MCA), one anterior communicating artery (ACOM) and one superior cerebellar artery (SCA) aneurysms were treated. All aneurysms apart from those of patients 2 and 3 met our criteria for wide-necked aneurysms. These two were included in our series as they were on the borderline of our definition and still felt to be appropriate for treatment with the CNS device. In all 11 cases only one CNS device was used and no adjuvant devices were required. At 6 weeks, nine of the 11 patients had an mRS score of 0, with the other two having an mRS score of 1 for headaches. At 6 months only one patient had an mRS score of 1 for residual headaches. Immediate postoperative angiography demonstrated stasis in all aneurysms, however with still some evidence of filling in the aneurysm (Raymond Class 3). On 6-month catheter angiography, complete occlusion (Raymond Class 1) was seen in four of the 11 patients, with four having small residual necks (Raymond Class 2). The remaining three cases showed persistent filling in the aneurysm at 6 months. For patient 6, intraoperatively it was felt that the device was attached to the wall on deployment and therefore in a good position, but on follow-up imaging it was apparent that this had been misjudged resulting in continued filling of the aneurysm. Later this patient was diagnosed with new frontal lobe dementia and so further follow-up imaging and retreatment was not possible. For patients 8 and 9, 1-year catheter angiography showed progressive occlusion of the aneurysm so no further treatment was required. Apart from cases 7, 8 and 9, we also have 2-year catheter angiography results available which show stability in the occlusion of the aneurysms with the CNS device.
We therefore demonstrated a complete occlusion rate at 1 year of 55.56% (5 out of 9 cases) with 44.44% with small neck remnants (4 out of 9 cases). Additionally, none of the follow-up imaging to date showed any device movement in any of the cases, suggesting the implant is stable once placed in the aneurysm. A summary of the results for our series is shown in table 2.
Table 2.
Summary of clinical and radiological results of Contour Neurovascular System series
| ID | Lesion location | Aneurysm dimensions | AR | DNR | Device size |
Raymond–Roy class | ||||
| Neck (mm) | Width (mm) | Height (mm) | Month 6 | Month 12 | Month 24 | |||||
| 01 | ICA | 2.4 | 3.5 | 4.3 | 1.8 | 1.5 | 7 | Class 1 | Class 1 | Class 1 |
| 02 | ICA | 3.9 | 8.7 | 9.1 | 2.3 | 2.2 | 9 | Class 2 | Class 2 | Class 2 |
| 03 | Basilar | 3.2 | 6.7 | 7.8 | 2.4 | 2.1 | 11 | Class 1 | Class 1 | Class 1 |
| 04 | SCA | 3.6 | 5.1 | 6.7 | 1.9 | 1.4 | 9 | Class 2 | Class 2 | Class 2 |
| 05 | Basilar | 2.7 | 4.2 | 5.5 | 2.0 | 1.6 | 9 | Class 1 | Class 1 | Class 1 |
| 06 | Basilar | 3.5 | 5.9 | 6.5 | 1.9 | 1.7 | 11 | Class 3 | n/a | n/a |
| 07 | ACOM | 3.2 | 4.3 | 5.8 | 1.8 | 1.3 | 7 | Class 1 | Class 1 | n/a |
| 08 | MCA | 5.4 | 10.2 | 12.0 | 2.2 | 1.9 | 11 | Class 3 | Class 1 | n/a |
| 09 | MCA | 4.4 | 7.5 | 13.0 | 3.0 | 1.7 | 11 | Class 3 | Class 2 | n/a |
| 10 | MCA | 4.8 | 6.5 | 7.1 | 1.5 | 1.4 | 11 | Class 2 | n/a* | n/a |
| 11 | Basilar | 4.0 | 3.8 | 6.1 | 1.5 | 1.0 | 7 | Class 2 | Class 2 | Class 2 |
*Occluded on 1 year MR angiography.
ACOM, anterior communicating artery; AR, aspect ratio (height/neck); DNR, dome/neck ratio (width/neck)); ICA, internal carotid artery; MCA, middle cerebral artery; SCA, superior cerebellar artery.
There have been no cases of postoperative ipsilateral major stroke, aneurysmal rupture, or death due to neurological causes. There were, however, a few cases in which problems were encountered. Patient 5 re-presented to our department a week after the procedure with transient ischemic attack-like symptoms and, on investigation with MRI, was found to have two small cerebellar infarcts. All symptoms completely resolved and the patient had no residual neurology and was discharged on 6 weeks of aspirin and 3 months of clopidogrel. Patient 10 had a difficult procedure with two failed attempts at CNS placement before the final 11 mm device was suitably sited. Soon after waking up the patient was found to have focal neurology suspicious of a thromboembolic event. Immediate repeat angiography demonstrated a clot in the MCA, which was treated with 5 mg IV abciximab. The patient woke with no deficits and was discharged on 2 months of aspirin and clopidogrel. This patient was troubled with post-procedural headaches and subsequently chose to leave the study and declined further follow-up catheter angiograms. It was felt that these symptoms were not related to the CNS device and the patient was subsequently diagnosed with generalised anxiety disorder following neurology review. The adverse events are summarised in table 3.
Table 3.
Summary of adverse events
| ID | Thromboembolic events | Intraprocedural rupture | Morbidity | Mortality | ||
| A | SS | SWS | ||||
| 01 | No | No | No | No | No | No |
| 02 | No | No | No | No | No | No |
| 03 | No | No | No | No | Headaches | No |
| 04 | No | No | No | No | No | No |
| 05 | No | No | Yes | No | No | No |
| 06 | No | No | No | No | No | No |
| 07 | No | No | No | No | No | No |
| 08 | No | No | No | No | No | No |
| 09 | No | No | No | No | No | No |
| 10 | No | No | Yes | No | Headaches | No |
| 11 | No | No | No | No | No | No |
A, asymptomatic; SS, symptomatic with sequelae; SWS, symptomatic without sequelae.
In table 4 we have detailed the three cases that were attempted to be treated unsuccessfully with the CNS along with the encountered problems. Case 12 was initially recommended for either clipping or stent-assisted coiling but declined. This was not an ideal case for the CNS device, but it was attempted nonetheless. Achieving a working projection was difficult due to intracranial artery geometry and there was difficulty in catheterizing with the XT 27 catheter so coils were attempted, although unsuccessfully, instead. In case 13, the difficulty was the aneurysm was too far for the catheter to reach and the vessels were tortuous. Following the procedure it was felt in hindsight this case was also not an appropriate one for the CNS device due to difficult anatomy. In case 14, the CNS did not fit the wall of the aneurysm correctly and would have given suboptimal results if left in situ. Therefore the decision was made to revert to a WEB device. Following the procedures, on reflection, it was felt by the authors, while the aneurysms themselves might be amenable to the CNS, if the vessels themselves are tortuous they may not be easily navigable with a 0.027 microcatheter. There were no other specific variables affecting treatment failure that we have come across so far. These particular cases formed part of the learning process going forward at our unit.
Table 4.
Summary of failed cases with the Contour Neurovascular System
| ID | Lesion location | Aneurysm dimensions | AR | DNR | Procedural difficulties | ||
| Neck (mm) | Width (mm) | Height (mm) | |||||
| 12 | MCA | 3.3 | 4.6 | 4.4 | 1.3 | 1.4 | Unable to catheterize with XT 27 catheter so coils were attempted. Despite eventual catheterization with Echelon 10 microcatheter, balloon inflation and attempts with multiple coils, the procedure was felt to be high risk of stroke and abandoned |
| 13 | Pericallosal | 3.7 | 6.6 | 5.5 | 1.5 | 1.8 | Inability to catheterize aneurysm with XT 27 catheter therefore successfully reverted to coiling |
| 14 | MCA | 5.1 | 6.3 | 7.2 | 1.4 | 1.2 | An XT 27 was navigated into the aneurysm. There were two failed trials with two 11 mm Contour devices. Subsequently a 9×4 mm WEB was used but was not suitable and an 8×3 mm WEB was used instead with good clinical and radiological outcomes |
AR, aspect ratio (height/neck); DNR, dome/neck ratio (width/neck); MCA, middle cerebral artery.
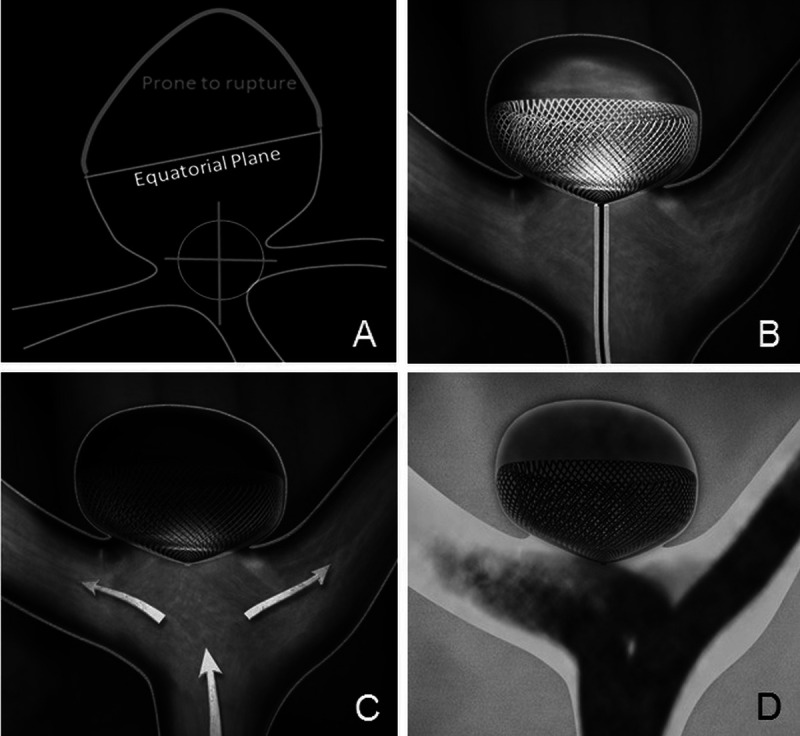
As an illustrative case, patient 1 initially presented with a subarachnoid hemorrhage from an ACOM aneurysm. On angiography the patient was also found to have an incidental terminal ICA aneurysm, which was being managed conservatively. Following 2 years since the original treatment, the ICA aneurysm had slightly increased in size so the MDT decision was to offer treatment. The patient consented and underwent treatment with the CNS. At 6 months, 1 year and 2 years, imaging showed complete occlusion and the patient remained GCS 15 with no neurology. The pre- and post-angiographic images are shown in figure 3.
Figure 3.
Case 1. (A) Three-dimensional reconstruction of the internal carotid artery aneurysm. (B) Angiographic view of untreated aneurysm. (C) Microcatheter at aneurysm neck. (D) 7 mm Contour Neurovascular System deployed within aneurysm. (E) Early angiographic view showing signs of stasis. (F) Six-month follow-up MRI showing complete occlusion, although with artefact. (G) Six-month follow-up angiogram showing complete occlusion and flow diversion. (H) Angiographic view showing device remains in good position.
Discussion
WNBAs continue to be technically difficult targets for the endovascular clinician.10 16 A recent multicenter American core laboratory-adjudicated study of 115 patients demonstrated adequate occlusion rates of between 40% and 63% with retreatment rates during their follow-up period of 8.7%.17 This study was limited as it reviewed only wide-necked MCA or basilar tip aneurysms treated with simple coils, balloon or stent-assisted coiling. Treatment of WNBAs using simple coils alone without adjuncts has disadvantages of coil instability and prolapse over time, risking the parent artery.7 16
Over the years, as previously alluded to, various adjuncts such as balloons and stents to assist the coiling process have been used with varying results.18–20 Devices such as the PulseRider (Pulsar Vascular, California, USA) and the pCONus (Phenox GmbH, Bochum, Germany) have been used to assist in stabilization of the coil mass in WNBAs.7 21 A recent systematic review of the PulseRider found that, in 63 patients, there was a 61.3% complete occlusion rate with a 7.9% complication rate.22 Two recent series on the pCONus device have described their results in wide-necked MCA and ACOM aneurysms.21 23 Labeyrie et al report that in their series of 36 patients with wide-necked ACOM aneurysms, their complete occlusion rate was 56% with a complication rate of 11%.21 Gory et al report on their series of 40 MCA aneurysms with a 67% complete occlusion rate and complication rate of 2.5%.23 Both had significant retreatment and recanalization rates. In comparison, our series show similar complete occlusion rates. It is important to note that these devices cannot be directly compared with the CNS given the differing modes of action, but instead highlight a benefit of the CNS which is designed to provide flow diversion the neck of the aneurysm due to the double braiding device structure. While long-term antiplatelets for flow diverters can be reduced or stopped after a few years, the CNS in our experience needs antiplatelet therapy only for a short term in the periprocedural period. It also removes the need for additional coils to occlude the aneurysm. Interestingly, we have also observed progressive occlusion of the aneurysms treated with the CNS in our series, which is similar to findings in aneurysms treated with flow diverters24 and is an advantage over the WEB device in our personal experience.
Lawson et al have previously reported on the WEB device, which is a similar intrasaccular embolization device that has been increasingly used for the treatment of WNBAs due to its flow diversion and flow disruption properties.6 The results showed adequate occlusion of between 73% and 77%. Other early results from other centers showed adequate occlusion rates between 75% and 89%. One series reported an aneurysm occlusion worsening rate of 7% and another quoted a retreatment rate of 16.7%, but these series also included ruptured aneurysms in the case mix.25 26 A recent multicenter series of 113 patients treated with the WEB reported complete occlusion rates of 56% with a complication rate of 2.7% at 1 year.27
In comparison, our results indicate modest complete occlusion rates of 55.56%, with some patients having small neck remnants. The significance of these neck remnants requires longer follow-up, but so far on our initial 2-year data, these appear to remain stable. With this caveat in mind, our results so far demonstrate all our patients have either Raymond–Roy Class 1 or 2 occlusion at follow-up, which suggests early evidence for better adequate occlusion rates than the WEB device. In our opinion, one of the main advantages the CNS offers over other available devices is that it is comparatively easy to size. For the WEB device, the height of the aneurysm has to be factored in along with the anteroposterior and lateral dome width, and while the aneurysm neck width is not required for sizing, it can sometimes affect the choice of WEB device size as well. With the CNS device, only the widest diameter of the aneurysm and neck width are needed for sizing and, in our experience, we suggest that if there is any sizing doubt, to oversize the device to the equatorial plane. Consequently, a range of aneurysm morphologies can be treated with a relatively small number of device sizes, as shown in table 1. Additionally, the device allows the treatment of WNBAs without the need for adjuvant devices due to its ability to disrupt flow in the aneurym as well as divert flow at the neck of the aneurysm, resulting in reduced operative time. As it has no major parent vessel component, this removes the need for lifelong antiplatelet therapy, which is a distinct advantage over devices such as the PulseRider and pCONus and, indeed, any stent-assisted coiling technology. The radio-opaque marker at the detatchment zone that sits in the parent vessel could be reasonably considered to be a nidus of thrombus formation, but in our experience with this device and the WEB (which has a similar marker), we have not seen this happen. Indeed, for appropriate placement of the device, the marker should ideally be seen in the parent vessel to ensure complete exclusion of the aneurysm neck. The device is also technically relatively simple to use and can use standard 0.027 microcatheter technology. This specific aspect could be considered a disadvantage by some readers given the relatively large size of the 0.027 microcatheter and, indeed, as evidence in our three failed cases, but it is hopeful that compatible 0.017 microcatheters will soon be available for use.
In our series we also found no evidence of device compression over time, which is a known problem that can occur with coils and the WEB device.28 The device position and shape remained unchanged in all cases. We believe that oversizing the device to the aneurysm is crucial to this as it subsequently prevents displacement and migration of the device into the aneurysm following deployment. In our limited experience we believe the device should not be manipulated once deployed in the aneurysm to adjust position, and if it is felt the placement is suboptimal, then it should be resheathed and redeployed in a more satisfactory position.
One of the limitations of the device is that it has not yet been used in the acute setting. However, the WEB device, which was initially used in an elective setting, was subsequently shown to have benefit in the acute setting.25–27 Similarly, while the authors think it is still very premature to use the CNS in an acute setting, more data and studies will be needed to assess the role of the CNS in the management of ruptured aneurysms. One disadvantage of the device we found is that MRI is not as useful as catheter angiography currently to follow up the CNS device due to the presence of some artefact on MRI due to the detachment zone (figure 3F).
The study limitations are that, with the small sample size, the clinical and radiological outcomes, while encouraging, need to be reassessed once more long-term data are available on larger sample sizes. While there were thromboembolic complications reported in two patients, these had no residual clinical implications and all patients had an mRS score of 0–1 at 6 weeks with no reported changes at 6 months. Our initial protocol was to put all patients on a 6-week course of aspirin postoperatively, although this may need to be altered over time as more data become available. We are also considering if routine premedication with antiplatelet agents may be helpful in the run-up to the procedure and, in particular with the failed cases, in retrospect this may have been helpful as it could have allowed the utilization of other devices in the case of failure of CNS deployment. Longer term follow-up is essential, but despite this, we do not foresee the need for lifelong antiplatelets with the CNS. Additionally, aside from our experiences with the CNS device, it is important to note that surgical clipping is still a viable treatment option for the treatment of wide-necked aneurysms and should always be considered.12
The device has been found to be stable at 2-year catheter angiography with good occlusion and acceptable safety outcomes in our patients, suggesting it could be a good alternative to the existing intrasaccular WEB device and other embolization technology.
Conclusions
Our early experience with the Contour device in the treatment of WNBAs looks promising and our series represents some of the first patients ever treated with the new device. The sizing of the device is relatively easy, making procedural planning simple, and the device is stable and relatively safe to use. It is also easy to navigate into the aneurysm using current 0.027 microcatheters. Long-term follow-up data will be crucial to assess this novel technology in the treatment of WNBAs as a safe and effective alternative to existing technology.
Footnotes
Contributors: CYA-F: Acquisition, analysis, interpretation of data, drafting, and revision of submitted manuscript. KD: Interpretation of data, critical review, and final approval of manuscript. AKT: Interpretation of data, critical review, and final approval of submitted manuscript. TP: Conception, design, analysis, interpretation of data, critical review, and final approval of submitted manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: TP is Consultant for Cerus Endovascular, Investor in Cerus Endovascular, and Proctor for Contour.
Patient consent for publication: Not required.
Ethics approval: West Midlands - South Birmingham Research Ethics Committee; Dr John Cochrane The Old Chapel Royal Standard Place, Nottingham NG1 6 FS; E-mail : nrescommittee.westmidlands-southbirmingham@nhs.net; EC approval REC reference number 16/WM/0271
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
References
- 1. Guglielmi G, Viñuela F, Dion J, et al. . Electrothrombosis of saccular aneurysms via endovascular approach. Part 2: preliminary clinical experience. J Neurosurg 1991;75:8–14. 10.3171/jns.1991.75.1.0008 [DOI] [PubMed] [Google Scholar]
- 2. Guglielmi G, Viñuela F, Sepetka I, et al. . Electrothrombosis of saccular aneurysms via endovascular approach. Part 1: electrochemical basis, technique, and experimental results. J Neurosurg 1991;75:1–7. 10.3171/jns.1991.75.1.0001 [DOI] [PubMed] [Google Scholar]
- 3. McDougall CG, Spetzler RF, Zabramski JM, et al. . The Barrow Ruptured Aneurysm trial. J Neurosurg 2012;116:135–44. 10.3171/2011.8.JNS101767 [DOI] [PubMed] [Google Scholar]
- 4. Molyneux A, Kerr R, Stratton I, et al. . International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet 2002;360:1267–74. 10.1016/S0140-6736(02)11314-6 [DOI] [PubMed] [Google Scholar]
- 5. Wiebers DO, Whisnant JP, Huston J, et al. . Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet 2003;362:103–10. 10.1016/S0140-6736(03)13860-3 [DOI] [PubMed] [Google Scholar]
- 6. Lawson A, Goddard T, Ross S, et al. . Endovascular treatment of cerebral aneurysms using the Woven EndoBridge technique in a single center: preliminary results. J Neurosurg 2017;126:17–28. 10.3171/2015.4.JNS142456 [DOI] [PubMed] [Google Scholar]
- 7. Mukherjee S, Chandran A, Gopinathan A, et al. . PulseRider-assisted treatment of wide-necked intracranial bifurcation aneurysms: safety and feasibility study. J Neurosurg 2017;127:61–8. 10.3171/2016.2.JNS152334 [DOI] [PubMed] [Google Scholar]
- 8. Raymond J, Guilbert F, Roy D. Neck-bridge device for endovascular treatment of wide-neck bifurcation aneurysms: initial experience. Radiology 2001;221:318–26. 10.1148/radiol.2212010474 [DOI] [PubMed] [Google Scholar]
- 9. Stapleton CJ, Torok CM, Patel AB. Early experience with the Penumbra smart coil in the endovascular treatment of intracranial aneurysms: safety and efficacy. Interv Neuroradiol 2016;22:654–8. 10.1177/1591019916663479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Fiorella D, Arthur AS, Chiacchierini R, et al. . How safe and effective are existing treatments for wide-necked bifurcation aneurysms? Literature-based objective performance criteria for safety and effectiveness. J Neurointerv Surg 2017;9:1197–201. 10.1136/neurintsurg-2017-013223 [DOI] [PubMed] [Google Scholar]
- 11. Hendricks BK, Yoon JS, Yaeger K, et al. . Wide-neck aneurysms: systematic review of the neurosurgical literature with a focus on definition and clinical implications. J Neurosurg 2019;66:1–7. 10.3171/2019.3.JNS183160 [DOI] [PubMed] [Google Scholar]
- 12. Mascitelli JR, Lawton MT, Hendricks BK, et al. . Analysis of wide-neck aneurysms in the Barrow Ruptured Aneurysm trial. Neurosurgery 2019;85:622–31. 10.1093/neuros/nyy439 [DOI] [PubMed] [Google Scholar]
- 13. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke 2001;32:1998–2004. 10.1161/hs0901.095600 [DOI] [PubMed] [Google Scholar]
- 14. Mascitelli JR, Oermann EK, De Leacy RA, et al. . Angiographic outcome of intracranial aneurysms with neck remnant following coil embolization. J Neurointerv Surg 2015;7:484–9. 10.1136/neurintsurg-2014-011226 [DOI] [PubMed] [Google Scholar]
- 15. Stapleton CJ, Torok CM, Rabinov JD, et al. . Validation of the modified Raymond–Roy classification for intracranial aneurysms treated with coil embolization. J Neurointerv Surg 2016;8:927–33. 10.1136/neurintsurg-2015-012035 [DOI] [PubMed] [Google Scholar]
- 16. Zhao B, Yin R, Lanzino G, et al. . Endovascular coiling of wide-neck and wide-neck bifurcation aneurysms: a systematic review and meta-analysis. AJNR Am J Neuroradiol 2016;37:1700–5. 10.3174/ajnr.A4834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. De Leacy RA, Fargen KM, Mascitelli JR, et al. . Wide-neck bifurcation aneurysms of the middle cerebral artery and basilar apex treated by endovascular techniques: a multicentre, core lab adjudicated study evaluating safety and durability of occlusion (branch). J Neurointerv Surg 2019;11:31–6. 10.1136/neurintsurg-2018-013771 [DOI] [PubMed] [Google Scholar]
- 18. Baldi S, Mounayer C, Piotin M, et al. . Balloon-assisted coil placement in wide-neck bifurcation aneurysms by use of a new, compliant balloon microcatheter. AJNR Am J Neuroradiol 2003;24:1222–5. [PMC free article] [PubMed] [Google Scholar]
- 19. McDonald JS, Norgan AP, McDonald RJ, et al. . In-hospital outcomes associated with stent-assisted endovascular treatment of unruptured cerebral aneurysms in the USA. J Neurointerv Surg 2013;5:317–20. 10.1136/neurintsurg-2012-010349 [DOI] [PubMed] [Google Scholar]
- 20. McLaughlin N, McArthur DL, Martin NA. Use of stent-assisted coil embolization for the treatment of wide-necked aneurysms: a systematic review. Surg Neurol Int 2013;4:43 10.4103/2152-7806.109810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Labeyrie PE, Gory B, Aguilar-Perez M, et al. . The pCONus device for treatment of complex wide-neck anterior communicating artery aneurysms. World Neurosurg 2017;101:498–505. 10.1016/j.wneu.2017.02.045 [DOI] [PubMed] [Google Scholar]
- 22. Aguilar-Salinas P, Brasiliense LBC, Walter CM, et al. . Current status of the PulseRider in the treatment of bifurcation aneurysms: a systematic review. World Neurosurg 2018;115:288–94. 10.1016/j.wneu.2018.04.102 [DOI] [PubMed] [Google Scholar]
- 23. Gory B, Aguilar-Pérez M, Pomero E, et al. . One-year angiographic results after pCONus stent-assisted coiling of 40 wide-neck middle cerebral artery aneurysms. Neurosurgery 2017;80:925–33. 10.1093/neuros/nyw131 [DOI] [PubMed] [Google Scholar]
- 24. Bhogal P, Martinez Moreno R, Ganslandt O, et al. . Use of flow diverters in the treatment of unruptured saccular aneurysms of the anterior cerebral artery. J Neurointerv Surg 2017;9:283–9. 10.1136/neurintsurg-2016-012648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Clajus C, Strasilla C, Fiebig T, et al. . Initial and mid-term results from 108 consecutive patients with cerebral aneurysms treated with the WEB device. J Neurointerv Surg 2017;9:411–7. 10.1136/neurintsurg-2016-012276 [DOI] [PubMed] [Google Scholar]
- 26. Lubicz B, Klisch J, Gauvrit J-Y, et al. . WEB-DL endovascular treatment of wide-neck bifurcation aneurysms: short- and midterm results in a European study. AJNR Am J Neuroradiol 2014;35:432–8. 10.3174/ajnr.A3869 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Pierot L, Spelle L, Molyneux A, et al. . Clinical and anatomical follow-up in patients with aneurysms treated with the WEB device: 1-year follow-up report in the cumulated population of 2 prospective, multicenter series (WEBCAST and French Observatory). Neurosurgery 2016;78:133–41. 10.1227/NEU.0000000000001106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cognard C, Januel AC. Remnants and recurrences after the use of the web intrasaccular device in large-neck bifurcation aneurysms. Neurosurgery 2015;76:522–30. 10.1227/NEU.0000000000000669 [DOI] [PubMed] [Google Scholar]