Version Changes
Revised. Amendments from Version 2
In this version, we revised the manuscript in accordance with the reviewers’ suggestions. In introduction section, we have revised the statement regarding the stone free rate, the risk of recurrence and the complication rate of PCNL and ESWL along with the original citation of the statement. In the method section, we have added a comment regarding the inclusion of case control study in the meta-analysis. In the result section, we have revised Figure 1 accordingly, and added a comment regarding the separate analysis of complication rate. Since Figure 1 is updated, we have revised the PRISMA file in our common database, which can be visited in the link: https://doi.org/10.17605/OSF.IO/GDH3R. Furthermore, we also revised the study characteristic table and separate the suggested details of each study included into Table 2 and Table 3 so that the table is not too large when combined. In addition, the discussion section has been re-arranged to be more logical and we also added more detail into the sections.
Abstract
Background: The decision for using supine or prone position in percutaneous nephrolithotomy (PCNL) is still debatable. The aim of this study is to compare the efficacy and safety profile of the supine and prone position when performing PCNL.
Methods: A systematic electronic search was performed using the database from MEDLINE, Cochrane library and Google Scholar from January 2009 to November 2019. The outcomes assessed were stone free rate, major complication rate, length of hospital stay and mean operation time.
Results: A total of 11 articles were included in qualitative and quantitative analysis. The efficacy of PCNL in supine position as determined by stone free rate is significantly lower than in prone position (OR: 0.74; 95% CI: 0.66 – 0.83; p<0.00001), However, major complication rate is also lower in the supine group compared with the prone group (OR: 0.70; 95% CI: 0.51 – 0.96; p=0.03). There is no statistically significant difference in the length of hospital stay and mean operation time between both groups.
Conclusion: Prone position leads to a higher stone free rate, but also a higher rate of major complication. Thus, the decision of using which position during PCNL should be based on the surgeon’s experience and clinical aspects of the patients.
Keywords: Complication rate, Percutaneous nephrolithotomy, Prone, Stone free rate, Supine
Introduction
Nephrolithiasis is one of the most common urological diseases worldwide. It is defined as a condition where mineral deposits are found in the kidney, either free in the renal calyces and pelvis or attached on the renal papillae 1. The prevalence is varied between regions, ranging between 7–13% in North America, 5–9% in Europe, and 1–5% in Asia 2. The most common stone composition is calcium, comprising about 80% of all urolithiasis 3.
Depending on stone burden, the treatment of nephrolithiasis also has a wide range of options. Active management includes extracorporeal shockwave lithotripsy (ESWL), retrieval by ureteroscopy (URS), and percutaneous nephrolithotomy (PCNL). The current guideline generally recommends ESWL for smaller stones (up to 20 mm) and PCNL for larger stones (>20 mm) regardless of the location inside the kidney 4.
In addition, PCNL is also effective in treating rare stone cases such as calyceal diverticula stone 5. Despite the efficacy, this procedure needs various preparations including the guiding system, the anesthesia, and the positioning of the patient 6. The conventional position of PCNL is prone, which allows direct access to the posterior calyx with minimal risk of bowel puncture. However, this positioning method limits the possibility of switching anesthesia from regional to general. The alternative position is supine, which allows general anesthesia switching and combination technique of antegrade and retrograde approaches. Moreover, this position is also more preferred in patients with cardiac comorbidity. However, working space and the possibility of multiple channels are limited 6. The aim of this study is to determine whether one position is more superior than the other, by comparing efficacy and safety profiles using a systematic review and meta-analysis approach.
Methods
Description of condition and intervention
The target population in this study is patients with renal stone of 20 mm or more in size who underwent PCNL. The intervention to the patients is PCNL in prone position, compared with PCNL in supine position. Prone is a classic position in PCNL procedure, described in 1976 when PCNL was first introduced. The original prone position consists of a two-stage procedure. The first stage is in supine position, where anesthesia is given and retrograde access to the upper urinary tract is established. The patient is then repositioned to a prone position, and supports are placed under the thorax and upper abdomen. All pressure points are also padded 7.
In contrast, a supine prone only needs one stage, in which the patient is placed supine with ipsilateral flank held up with a 3-liter saline bag. This original position was first introduced by Valdivia-Uria et al. and has been modified over time 8. One popular modification of Valdivia position is the Galdakao modification. This position is slightly more lateral; the contralateral leg of the patient is flexed and abducted, while the ipsilateral leg is extended. A 3-liter bag is also placed to raise the flank 7.
Apart from the Valdivia position and its modifications, a complete supine position was also introduced by Falahatkar et al. 9 This position does not require an elevation of the flank. The patient is simply put in a supine position at the edge of the table, with legs extended. The patient’s arms are stretched, abducted and supported.
The outcome of this study is the efficacy of both positions, determined by stone free rate and safety profile, determined by the occurrence of major complications.
Database searching and literature screening
A systematic search was carried out with the date last searched in 14 February 2020, using the database from MEDLINE, with keywords of “(((supine[Title/Abstract]) AND prone[Title/Abstract])) AND ((PCNL[Title/Abstract]) OR percutaneous nephrolithotomy[Title/Abstract])”, and Cochrane library, with keywords of “prone in Title Abstract Keyword AND supine in Title Abstract Keyword AND PCNL in Title Abstract Keyword”, and Google Scholar with keywords of “prone AND supine AND percutaneous nephrolithotomy”. After we identified the articles, we removed the duplicates and further screened the articles. The reporting is based on Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) algorithm.
Study selection
Two reviewers (PB and WT) independently appraised the articles, and a discussion was conducted when disagreement occurred. The relevance of the articles is determined by reading through the titles and abstracts. The inclusion criteria are a comparative study between the supine and prone position in PCNL procedure in adult patients with age of 18 years old or more, the articles were written in English, and the design of the study was randomized clinical trial (RCT), cohort or case control. The exclusion criteria are non-comparative studies, studies that combine PCNL with other techniques of stone extraction such as URS or retrograde intrarenal surgery, not focused on comparing supine and prone position in PCNL, and inclusion of confounding factors such as a difference in guiding method when performing PCNL in each position, since this difference will lead to intervention bias. The quality of each article included were then tested using Jadad scale for RCTs and Newcastle-Ottawa scale for non-RCTs 10, 11.
Data extraction
Data extraction from the articles was performed by two authors (NR and WA), and any disagreement was settled by consensus. The variables extracted from the articles included the first author’s name, year of publication, stone free rate, percentage of major complications, length of hospital stay, and mean operation time. Stone free condition is defined as the absence of residual fragments of ≤ 4 mm after procedure. Major complications are defined as those with a Clavien score of III or more 12.
Statistical analysis
Meta-analysis was performed by Review Manager 5.3. The results were described as odds ratio (OR) with 95% confidence interval (CI) for dichotomous variables, and as a mean difference with 95% CI for continuous variables. Heterogeneity was analyzed using a Chi square and I 2 test. The data was analyzed using the random-effect model when I 2 >25%, and fixed-effect model when I 2 is less than 25%. The analysis is considered statistically significant when p value is less than 0.05. For studies that provided the minimum and maximum value instead of standard deviation (SD) for the mean difference analysis, estimated SD were calculated with the formula derived from a study by Walter and Yao (2007) 13. In addition, for studies that provided 95% Confidence Interval (CI) instead of SD, the value of SD was calculated using the formula described in the Cochrane Handbook 14.
Results
Literature search
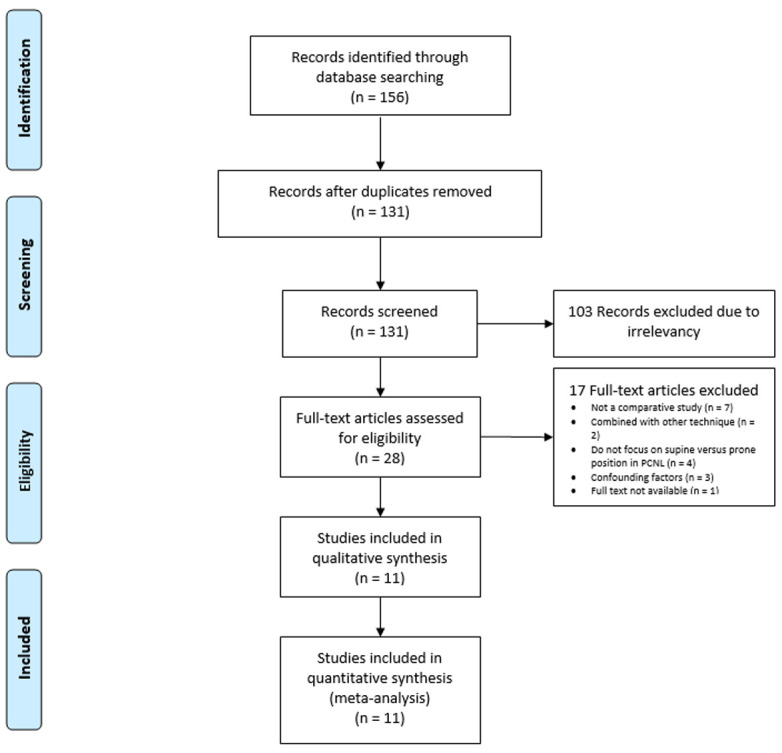
Following the result of article screening and the application of exclusion criteria, a total of 156 articles were found from the three databases. After removing duplicates, a total of 131 studies were screened. Among these, 28 studies were found to be relevant based on the studies’ titles and abstracts in which the full text were assessed. Eventually, there were 11 articles were included in qualitative and quantitative analysis ( Figure 1).
Figure 1. PRISMA method of article screening.
Study characteristics
There were 2 RCTs assessed with Jadad scale, in which one of them showed a poor quality. However, the remaining 9 studies were cohort studies and had a good quality score in Newcastle-Ottawa scale. We did not find any case control studies that fulfill our inclusion criteria ( Table 1). Study characteristics, including the number of patients, mean age, stone burden, stone free rate, complication rate the definition of stone free rate and follow up time are shown in Table 2. In addition, the anomaly status of the patients and the used surgery tools along with the need of second look in the studies included are presented in Table 3.
Table 1. Quality assessment of the articles included.
RCT, randomized controlled trial.
| Articles | Study
design |
Quality assessment | |
|---|---|---|---|
| Jadad
scale |
Newcastle-
Ottawa scale |
||
| Melo PAS, et al. (2019) 9 | Cohort | - | 8 |
| Gokce MI, et al. (2017) 15 | Cohort | - | 8 |
| Mahmoud M, et al. (2017) 16 | RCT | 2 | - |
| Wood GJA, et al. (2017) 17 | Cohort | - | 7 |
| Astroza G, et al. (2013) 18 | Cohort | - | 6 |
| Kan RW, et al. (2013) 19 | Cohort | - | 8 |
| Karami H, et al. (2013) 20 | RCT | 1 | - |
| Sanguedolce F, et al. (2013) 21 | Cohort | - | 6 |
| Arrabal-Martin M, et al. (2012) 22 | Cohort | - | 7 |
| Wang Y, et al. (2012) 23 | Cohort | - | 8 |
| Valdivia JG, et al. (2011) 8 | Cohort | - | 8 |
Table 2. Characteristics of studies included.
| Articles | Cases (n) | Mean age
(years) |
Stone size (mm/
mm 2) |
Mean number of
stone |
Stone free rate
(%) |
Complication
rate (%) |
Definition of Stone Free
Rate |
Follow
up time |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Supine | Prone | Supine | Prone | Supine | Prone | Supine | Prone | Supine | Prone | Supine | Prone | |||
| Melo PAS,
et al.
(2019) |
294 | 99 | 49.14 | 47.66 | 29.76 | 30.34 | - | - | 42.1 | 37.4 | 13.6 | 23.2 | Residual stones ≤ 4 mm | 1 day |
| Gokce MI,
et al.
(2017) |
39 | 48 | 47.5 | 49.2 | 47.3 | 45.6 | - | - | 64.1 | 60.4 | 15.4 | 29.2 | Absence of residual
fragments in postoperative NCCT |
30 days |
| Mahmoud M,
et al. (2017) |
20 | 20 | 42.35 | 41.15 | 27.1 | 25.7 | Single
or multiple |
Single
or multiple |
80 | 85 | 15 | 10 | Absence of residual stone | - |
| Wood GJA,
et al.
(2017) |
28 | 104 | 45.89 | 44.98 | - | - | - | - | 71.4 | 63.5 | 28.6 | 39.4 | Residual stones ≤ 3 mm on
first postoperative CT scan |
1 day |
| Astroza G,
et al.
(2013) |
232 | 1079 | 51.8 | 49.8 | - | - | - | - | 48.4 | 59.2 | 10.4 | 8 | - | - |
| Kan RW,
et al.
(2013) |
25 | 35 | 67 | 63 | 36.9 | 44.8 | - | - | 46 | 68 | 24 | 11.4 | Absence of residual stone | - |
| Karami H,
et al.
(2013) |
50 | 50 | 44.4 | 41.5 | 28.2 | 28.3 | 2 | 2.3 | 86 | 92 | 24 | 20 | Residual stones ≤ 3 mm | 1 month |
| Sanguedolce F,
et al. (2013) |
65 | 52 | 53 | 49 | 20.6 | 18.1 | Single
or multiple |
Single
or multiple |
89.2 | 92.3 | 7.7 | 7.6 | Absence of fragments of
asymptomatic residual fragment ≤ 2 mm |
3 months |
| Arrabal-Martin
M, et al. (2012) |
24 | 32 | 49 | 47 | 510 | 530 | - | - | 79.2 | 75 | 29.1 | 31.2 | - | - |
| Wang Y,
et al.
(2012) |
6 | 12 | 44.8 | 43.8 | 36 | 33 | - | - | 83.3 | 91.7 | 0 | 0 | No residual stone of > 4 mm | 3 months |
| Valdivia JG, et al. (2011) | 1138 | 4637 | 51 | 48.8 | 470.6 | 449.1 | - | - | 70.2 | 77 | 19.2 | 20.8 | Stone free on radiography,
renal ultrasound, or CT scan |
30 days |
| Total patients | 1921 | 6168 | - | - | - | - | - | - | - | - | - | - | - | - |
Table 3. Anomaly status and the used surgery tools of included studies.
| Articles | Congenital Anomalies | Intraoperative
imaging modality |
Sheath
Caliber |
Lithotripsy
technique |
Second
Look |
|---|---|---|---|---|---|
| Melo PAS, et al. (2019) | No | Fluoroscopy | 30 Fr | Ultrasonic
lithotripter |
No |
| Gokce MI, et al. (2017) | No | Fluoroscopy | 30 Fr | Ballistic
lithotripter |
No |
| Mahmoud M,
et al.
(2017) |
No | - | - | - | - |
| Wood GJA, et al. (2017) | No | Fluoroscopy | - | - | No |
| Astroza G, et al. (2013) | No | - | - | - | No |
| Kan RW, et al. (2013) | No | Fluoroscopy | 24-30 Fr | Ultrasonic
lithotripter |
No |
| Karami H, et al. (2013) | No | Fluoroscopy | 30 Fr | Pneumatic
lithotripter |
No |
| Sanguedolce F, et al. (2013) | No | - | - | - | Yes in 6 patients |
| Arrabal-Martin M,
et al.
(2012) |
No | - | - | Ultrasonic
or kinetic lithotripter |
No |
| Wang Y, et al. (2012) | Solitary kidney in 23.3% (4
patients) |
Fluoroscopy | 18 or 26 Fr | Holmium
lithotripter |
No |
| Valdivia JG, et al. (2011) | 1. Ectopic kidney (0.8% and
0.4% in supine and prone group, respectively) 2. Horseshoe kidney (1.2% and 2.0% in supine and prone group, respectively) 3. Malrotation kidney (2.0% and 1.2% in supine and prone group, respectively) |
Fluoroscopy,
ultrasound, or both |
- | - | No |
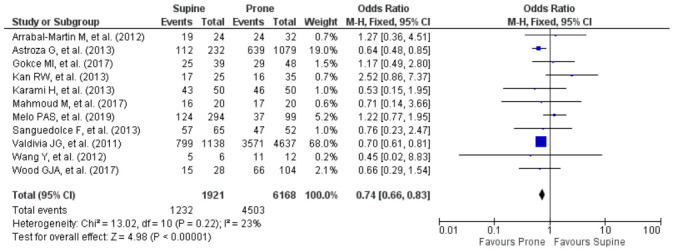
Stone free rate
All 11 studies reported the stone free rate of both supine and prone groups. A meta-analysis of these studies showed that there was a low heterogeneity and a statistically significant lower stone free rate in the supine group (OR: 0.74; 95% CI: 0.66 – 0.83; p<0.00001; Figure 2).
Figure 2. Forest plot comparing stone free rate in prone and supine groups.
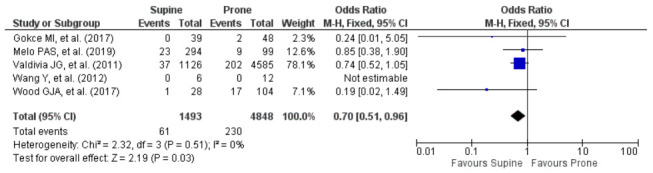
Major complication rate
Major complication rate is defined as Clavien score of 3 of more in this study. There were only 5 articles that reported the complication rate using Clavien score in which there was no heterogeneity found of these studies. Figure 3 showed that there is a statistically significant lower complication rate in the supine group (OR: 0.70; 95% CI: 0.51 – 0.96; p=0.03).
Figure 3. Forest plot comparing major complication rate in prone and supine groups.
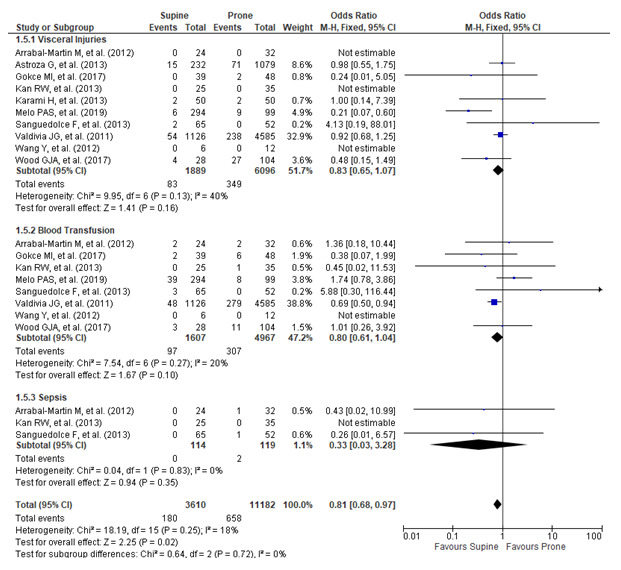
The subgroup analysis of complication parameters such as visceral injuries including pleural effusion and organ perforation, the need of blood transfusion, and infection which lead to sepsis revealed that there is no significant difference between groups when analyzed separately (p=0.16; p=0.10; p=0.35, respectively). However, the combined analysis of those specific complications lead to a significant difference in which the risk is lower in the supine group (OR: 0.81; 95% CI: 0.68 – 0.97; p=0.02; Figure 4).
Figure 4. Comparison of the complications subgroup between supine and prone groups.
Length of hospital stay
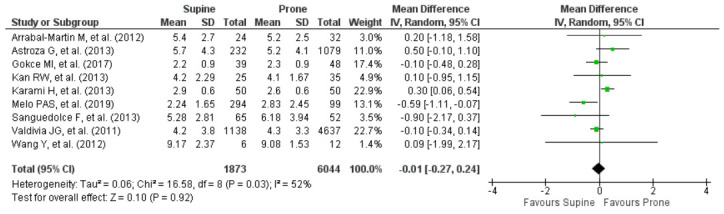
There were nine studies that reported mean days of hospital stay in both groups. The forest plot in Figure 5 shows that there is no difference in the length of hospital stay between groups (Mean difference: -0.01; 95% CI: -0.27 – 0.24; p=0.92). However, there was heterogeneity in this parameter.
Figure 5. Forest plot comparing length of hospital stay in prone and supine groups.
Mean operation time
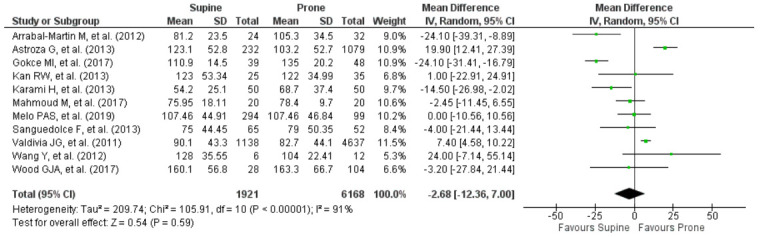
Mean operation time was reported in all studies and the I 2 analysis showed that the studies were heterogenous. The meta-analysis in this parameter showed that there is no difference in mean operation time between these two groups (Mean difference: -2.68; 95% CI: -12.36 – 7.00; p=0.59; Figure 6).
Figure 6. Forest plot comparing mean operation time in prone and supine groups.
Discussion
The authors choose stone free rate and major complication as the main outcome of this article to help identify which position is safe in PCNL and whether there is a difference in the efficacy. Regarding the stone free rate, one of the studies included in this meta-analysis mentioned the need of second look for the patients after PCNL (Sanguedolce F, et al.) 21. It is in our interest that the risk of residual stones in which the second look was needed was not significantly different between supine and prone position (p=0.12). However, the pooled analysis of stone free rate revealed that the stone free rate was significantly higher in prone position. The possible explanation is that in this position, the lumbar area is fully exposed which allows a possibility of several puncture sites, and easier access to the upper pole kidney. Moreover, the working area is greater, providing enough space for instrument manipulation 7.
Nevertheless, the two-stage nature of this position usually prolongs the operating time, and a prone position makes it difficult for the anesthetists to attend cardio-respiratory emergency. The risk of ocular complications has also been described because of the increase in intra-ocular pressure 7.
Our study found that the supine position had a lower major complication rate than prone position. The subgroup analysis of the blood transfusion need, risk of sepsis and visceral injuries also showed the lower rate of complications in the supine group when compared to the prone group despite the individual analysis of each complication showed no difference between groups. This fact is in accord with the literature which revealed that the original (Valdivia) position is reportedly safe, and endoscopic instruments can be moved more freely because the puncture site of the abdominal wall is performed more laterally and away from the lumbar muscles. The tract in this position also preserves a low pressure in the renal pelvis, reducing the risk of fluid absorption. Moreover, risk of colonic puncture might be reduced because the bowel is not pressed towards the kidney. Should a rigid ureteroscopy be needed simultaneously with PCNL, a modified Valdivia position can be performed by flexing and supporting the patient’s ipsilateral leg, and the contralateral leg descended. The supine position also has the advantage of easier management of cardiac and respiratory emergencies 7.
Moreover, the Galdakao-modified position allows more instrument manipulation than the original supine position. Furthermore, it also enables simultaneous retrograde access to the kidney and there is no need to reposition thus the asepsis and antisepsis procedure needs to be performed only once 7.
In the complete supine position, the lack of flank support allows more feasible access to the upper pole of the kidney because there is no risk of cephalad sliding of the kidney, as observed in the supine position with flank support 7. The supine position also has the advantages of easier access to the upper pole after lower pole puncture 24.
However, it should also be noted that while there are many advantages to the supine position regarding the complication rate, the state of low compressed abdomen in this position allows the kidney to move more freely, making the navigation of the instrument towards the kidney more challenging, and the chance of failed access is higher 7, 8, 17.
The secondary outcomes of our study are mean operation time and duration of hospital stay. According to our review, supine and prone position during PCNL share a similar result in these parameters. This result is important so that the surgeons will be able to confidently decide the position based on their experiences and the patient’s comorbidities.
The previous meta-analysis by Yuan et al. stated that the stone free rate was higher in prone position, which was similar to our study 25. However, the complication rate between the two groups was similar which was slightly different in our findings. Another meta-analysis performed by Falahatkar, et al. showed a similar complication and stone free rate between supine and prone position, but lower need of blood transfusion in the supine group which might implicate the benefit of supine position 26. These results are somewhat similar to our study, which show a better stone free rate in the prone position, but a lower complication rate in supine position, suggesting a better safety profile in the supine position.
The limitation in our study is that the number of articles providing data of major complication rate in terms of Clavien score was limited and there were too many heterogeneities in the length of hospital stay and mean operation time variables. Therefore, the authors believe that another comprehensive study should be performed in urology centers in which the surgeons excel in both supine and prone position when performing PCNL and have a larger sample size.
The implication of this study is that it exposed the benefit and disadvantages of both supine and prone position, which in turn can be used as a decision guide for clinicians who want to perform PCNL.
Conclusion
In conclusion, the prone position leads to a higher stone free rate than supine position. However, in terms of safety profile, supine position provides a better choice than the prone position. There is no difference in both the length of hospital stay and mean operation time between prone and supine position. Therefore, it can be inferred that there is no position that has absolute superiority and it is important to note that both supine and prone position in PCNL procedure have their respective advantages and disadvantages. Thus, the decision of choosing the position when performing PCNL should be based on clinical status of the patient and the experience of the surgeon.
Data availability
Underlying data
All data underlying the results are available as part of the article and no additional source data are required.
Reporting guidelines
Open Science Framework: PRISMA checklist for article ‘Supine versus prone position in percutaneous nephrolithotomy: a systematic review and meta-analysis’, https://doi.org/10.17605/OSF.IO/GDH3R 27.
Data are available under the terms of the Creative Commons Zero "No rights reserved" data waiver (CC0 1.0 Public domain dedication).
Acknowledgements
The authors would like to thank you to the Cipto Mangunkusumo National Hospital for the support and permission for the authors to finish the production of this article.
Funding Statement
The author(s) declared that no grants were involved in supporting this work.
[version 3; peer review: 2 approved]
References
- 1. Khan SR, Pearle MS, Robertson WG: Kidney stones. Nat Rev Dis Primers. 2016;2:16008. 10.1038/nrdp.2016.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sorokin I, Mamoulakis C, Miyazawa K, et al. : Epidemiology of stone disease across the world. World J Urol. 2017;35(9):1301–20. 10.1007/s00345-017-2008-6 [DOI] [PubMed] [Google Scholar]
- 3. Alelign T, Petros B: Kidney Stone Disease: An Update on Current Concepts. Adv Urol. 2018;2018: 3068365. 10.1155/2018/3068365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Turk C, Skolarikos A, Neisius A, et al. : EAU Guidelines on Urolithiasis. The Netherlands: EAU Guidelines Office;2019. [Google Scholar]
- 5. Turna B, Raza A, Moussa S: Management of calyceal diverticular stones with extracorporeal shock wave lithotripsy and percutaneous nephrolithotomy: long-term outcome. BJU Int. 2007;100(1):151–6. 10.1111/j.1464-410X.2007.06911.x [DOI] [PubMed] [Google Scholar]
- 6. Ganpule AP, Vijayakumar M, Malpani A, et al. : Percutaneous nephrolithotomy (PCNL) a critical review. Int J Surg. 2016;36(Pt D):660–664. 10.1016/j.ijsu.2016.11.028 [DOI] [PubMed] [Google Scholar]
- 7. Karaolides T, Moraitis K, Bach C, et al. : Positions for percutaneous nephrolithotomy: Thirty-five years of evolution. Arab J Urol. 2012;10(3):307–16. 10.1016/j.aju.2012.06.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Valdivia JG, Scarpa RM, Duvdevani M, et al. : Supine versus prone position during percutaneous nephrolithotomy: a report from the clinical research office of the endourological society percutaneous nephrolithotomy global study. J Endourol. 2011;25(10):1619–25. 10.1089/end.2011.0110 [DOI] [PubMed] [Google Scholar]
- 9. Falahatkar S, Moghaddam AA, Salehi M, et al. : Complete supine percutaneous nephrolithotripsy comparison with the prone standard technique. J Endourol. 2008;22(11):2513–7. 10.1089/end.2008.0463 [DOI] [PubMed] [Google Scholar]
- 10. Cho HJ, Chung JH, Jo JK, et al. : Assessments of the quality of randomized controlled trials published in International Journal of Urology from 1994 to 2011. Int J Urol. 2013;20(12):1212–9. 10.1111/iju.12150 [DOI] [PubMed] [Google Scholar]
- 11. Luchini C, Stubbs B, Solmi M, et al. : Assessing the quality of studies in meta-analyses: advantages and limitations of the newcastle ottawa scale. World J Meta Anal. 2017;5(4):80–4. 10.13105/wjma.v5.i4.80 [DOI] [Google Scholar]
- 12. Melo PAS, Vicentini FC, Perrella R, et al. : Comparative study of percutaneous nephrolithotomy performed in the traditional prone position and in three different supine positions. Int Braz J Urol. 2019;45(1):108–17. 10.1590/S1677-5538.IBJU.2018.0191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Walter SD, Yao X: Effect sizes can be calculated for studies reporting ranges for outcome variables in systematic reviews. J Clin Epidemiol. 2007;60(8):849–52. 10.1016/j.jclinepi.2006.11.003 [DOI] [PubMed] [Google Scholar]
- 14. Higgins JPT, Green S: Cochrane Handbook for Systematic Reviews of Interventions.Version 5.1.0 [updated March 2011]. The Cochrane Collaboration;2011. Reference Source [Google Scholar]
- 15. Gokce MI, Ibis A, Sanci A, et al. : Comparison of supine and prone positions for percutaneous nephrolithotomy in treatment of staghorn stones. Urolithiasis. 2017;45(6):603–8. 10.1007/s00240-017-0977-y [DOI] [PubMed] [Google Scholar]
- 16. Mahmoud M, Abdel AA, Abdel AM, et al. : Flank suspended supine position versus standard supine and prone position in percutaneous nephrolithotomy. J Endourol. 2017;31:A95–A98. [Google Scholar]
- 17. Wood GJA, Torricelli FCM, Vicentini FC, et al. : Supracostal punctures in supine percutaneous nephrolithotomy are safe. Can J Urol. 2017;24(2):8749–53. [PubMed] [Google Scholar]
- 18. Astroza G, Lipkin M, Neisius A, et al. : Effect of supine vs prone position on outcomes of percutaneous nephrolithotomy in staghorn calculi: results from the Clinical Research Office of the Endourology Society Study. Urology. 2013;82(6):1240–4. 10.1016/j.urology.2013.06.068 [DOI] [PubMed] [Google Scholar]
- 19. Kan RW, Fu KK, Wong BT, et al. : Percutaneous nephrostomy, nephrolithotomy and combined ureteroscopic lithotripsy using the supine approach. Hong Kong Med J. 2013;19(2):142–9. [PubMed] [Google Scholar]
- 20. Karami H, Mohammadi R, Lotfi B: A study on comparative outcomes of percutaneous nephrolithotomy in prone, supine, and flank positions. World J Urol. 2013;31(5):1225–30. 10.1007/s00345-012-0889-y [DOI] [PubMed] [Google Scholar]
- 21. Sanguedolce F, Breda A, Millan F, et al. : Lower pole stones: prone PCNL versus supine PCNL in the International Cooperation in Endourology (ICE) group experience. World J Urol. 2013;31(6):1575–80. 10.1007/s00345-012-0941-y [DOI] [PubMed] [Google Scholar]
- 22. Arrabal-Martin M, Arrabal-Polo MA, Lopez-Leon V, et al. : The oblique supine decubitus position: technical description and comparison of results with the prone decubitus and dorsal supine decubitus positions. Urol Res. 2012;40(5):587–92. 10.1007/s00240-012-0471-5 [DOI] [PubMed] [Google Scholar]
- 23. Wang Y, Hou Y, Jiang F, et al. : Percutaneous nephrolithotomy for staghorn stones in patients with solitary kidney in prone position or in completely supine position: a single-center experience. Int Braz J Urol. 2012;38(6):788–94. 10.1590/1677-553820133806788 [DOI] [PubMed] [Google Scholar]
- 24. Sofer M, Giusti G, Proietti S, et al. : Upper Calyx Approachability through a Lower Calyx Access for Prone Versus Supine Percutaneous Nephrolithotomy. J Urol. 2016;195(2):377–82. 10.1016/j.juro.2015.07.101 [DOI] [PubMed] [Google Scholar]
- 25. Yuan D, Liu Y, Rao H, et al. : Supine versus prone position in percutaneous nephrolithotomy for kidney calculi: a meta-analysis. J Endourol. 2016;30(7):754–63. 10.1089/end.2015.0402 [DOI] [PubMed] [Google Scholar]
- 26. Falahatkar S, Mokhtari G, Terimoori. M: An update on supine versus prone percutaneous nephrolithotomy: a meta-analysis. Urol J. 2016;13(5):2814–22. 10.22037/uj.v13i5.3677 [DOI] [PubMed] [Google Scholar]
- 27. Tendi W: Supine versus Prone Position in Percutaneous Nephrolithotomy: A Systematic Review and Meta-Analysis.2020. 10.17605/OSF.IO/GDH3R [DOI] [PMC free article] [PubMed]


