Abstract
Excessive daytime sleepiness (EDS) is the tendency to sleep at inappropriate times during the day. It can interfere with day-to-day activities and lead to several health issues. The objective of this study was to investigate the association between income, housing conditions, and incidence of EDS in adults living in two Cree First Nations communities. The data for this study involved 317 individuals aged 18 years and older who participated in baseline and follow-up evaluations (after four years) of the First Nations Lung Health Project, which was conducted in Saskatchewan in 2012–2013 and 2016. Both at baseline and follow-up survey after four years, an Epworth Sleepiness Scale (ESS) score >10 was considered to be abnormal. Logistic regression models were used to assess relationships between abnormal ESS and covariates at baseline. In 2016, 7.6% (24/317) of the participants reported an ESS >10 with the mean being 12.8 ± 2.0. For the same group, the mean ESS at baseline was 6.9 ± 2.2. The incidence of subjective EDS based on the ESS >10 was estimated at 7.6% over four years. This study showed an association between incidence of subjective EDS and less money left over at end of the month, having a house in need of repairs, having water or dampness in the past 12 months, and damage caused by dampness.
Keywords: subjective excessive daytime sleepiness, First Nations, house in need of repairs, dampness, money left over at the end of the month
1. Introduction
Excessive daytime sleepiness (EDS) is the tendency to sleep at inappropriate times during the day. It can interfere with day-to-day activities such as work, school and/or relationships [1] and is associated with several health issues such as diabetes [2,3], heart disease [4,5], stroke [6], depression [7], and gastroesophageal reflux disease [8]. Motor vehicle accidents are the most dramatic consequence of EDS [9,10,11,12,13,14], with EDS accounting for 20% of total accidents. The prevalence of EDS in the general population varies from 9 to 28% [15]. Results from a pilot study reported subjective EDS prevalence to be 20.0% among rural Canadians [16]. Another study of rural Canadians reported the prevalence of subjective EDS was 15.9% in a population of adults (mean age 55 years) [17]. However, the prevalence of subjective EDS in two rural First Nations communities in Canada was reported to be 11% in a population of adults although younger than those in the rural population (mean age 35 years) [18].
Socio-economic factors impact daytime sleepiness [19,20]. Stringhini et al. [19] showed that women with a low position in their occupation (mainly unskilled workers) have a higher risk of subjective EDS. There was clear evidence of individuals with a lower socioeconomic gradient reporting greater daytime sleepiness [20].
Research has also shown that exposures to mold or dampness have been associated with adverse respiratory outcomes [21,22,23] and sleep problems [24,25,26] in both adults and children. In a study of adults living in England, participants living in damp buildings were more likely to report sleep disturbances [24]. In a study of Northern European adults, participants living in houses with reported signs of building dampness had a higher prevalence of insomnia and the association was strongest for floor dampness [25]. Two studies, one from Taiwan and one from Brazil, demonstrated an association between insomnia and EDS [27,28]. A recent study using the baseline data from this study [18] showed that a house in need of repairs, low annual household income and overcrowding were significantly associated with the prevalence of subjective EDS in First Nations communities.
To our knowledge, the association between socio-economic status including income, housing conditions, and incidence of subjective EDS in First Nations adults has not been investigated. Thus, this study aimed to investigate the association between income, housing conditions and incidence of subjective EDS in adults living in two First Nations communities.
2. Results
Descriptive characteristics of the study population of 18 years and older (n = 317) can be found in Table 1. Of those who participated at baseline, the mean (±SD) age of men was 34.4 (±13.1) years and for women the mean age was 37.0 (±14.3) years. Twenty four percent of participants completed high school (Grade 12). Thirty one percent of participants were overweight and 36% were obese. Current smoking was present in 83.6%, ex-smoking in 6.9% and never smoking in 9.5% of participants. Loud snoring was reported by 16.1% of participants. In 2016, 7.6% (24/317) of participants reported an ESS > 10 with a mean subjective ESS of 12.8 ± 2.0 (Male: 13.2 ± 2.4; Female: 12.4 ± 1.6). For the same group, the mean subjective ESS at baseline was 6.9 ± 2.2 (Male: 6.8 ± 1.7; Female: 6.9 ± 2.6). The incidence of subjective EDS based on the ESS > 10 was estimated as 7.6% (Male: 7.9%; Female: 7.2%) over four years.
Table 1.
Univariable association between newly identified subjective EDS and demographic factors, co-morbid conditions, socio economic factors and housing environment.
| Variables | Total n (%) | Newly Diagnosed Subjective EDS | p Value | Crude OR (95% CI) | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Demographics | |||||
| Sex | |||||
| Male | 151 (47.6) | 12 (50.0) | 139 (47.4) | 0.812 | 1.11 (0.48, 2.55) |
| Female | 166 (52.4) | 12 (50.0) | 154 (52.6) | 1.00 | |
| Age group | |||||
| 18–35 years | 170 (53.6) | 12 (50.0) | 158 (53.9) | 0.866 | 0.87 (0.18, 4.32) |
| 36–55 years | 122 (38.5) | 10 (41.7) | 112 (38.2) | 0.976 | 1.02 (0.20, 5.15) |
| >55 years | 25 (7.9) | 2 (8.3) | 23 (7.8) | 1.00 | |
| Education level | |||||
| Less than high school | 156 (49.4) | 14 (58.4) | 142 (48.6) | 0.425 | 1.54 (0.53, 4.41) |
| Completed high school | 77 (24.4) | 5 (20.8) | 72 (24.7) | 0.907 | 1.08 (0.30, 3.93) |
| Post-secondary (university/technical or some) | 83 (26.2) | 5 (20.8) | 78 (26.7) | 1.00 | |
| Marital status | |||||
| Married/common law | 119 (39.0) | 8 (33.3) | 111 (39.5) | 0.550 | 0.77 (0.32, 1.83) |
| Widowed/divorced/separated/single | 186 (61.0) | 16 (66.7) | 170 (60.5) | 1.00 | |
| Body mass index | |||||
| Neither overweight nor obese | 102 (31.1) | 5 (20.8) | 97 (34.2) | 0.341 | 0.58 (0.19, 1.77) |
| Overweight | 95 (30.9) | 10 (41.7) | 85 (29.9) | 0.547 | 1.33 (0.52, 3.39) |
| Obese | 111 (36.0) | 9 (31.5) | 102 (35.9) | 1.00 | |
| Home crowding status | |||||
| More than one person per room | 99 (32.6) | 7 (31.8) | 92 (32.6) | 0.937 | 0.96 (0.39, 2.41) |
| One or less person per room | 205 (67.4) | 15 (68.2) | 190 (67.4) | 1.00 | |
| Alcohol consumption (5 or more drinks at a time) | |||||
| Never | 61 (19.3) | 4 (16.7) | 57 (19.5) | 0.675 | 0.78 (0.24, 2.51) |
| Occasionally | 122 (38.6) | 9 (37.5) | 113 (38.7) | 0.792 | 0.88 (0.35, 2.34) |
| Regularly | 133 (42.1) | 11 (45.8) | 122 (41.8) | 1.00 | |
| Smoking status | |||||
| Current smoking | 265 (83.6) | 20 (83.3) | 245 (83.6) | 0.638 | 0.74 (0.20, 2.64) |
| Ex-smoker | 22 (6.9) | 1 (4.2) | 21 (7.2) | 0.482 | 0.43 (0.04, 4.53) |
| Never smoker | 30 (9.5) | 3 (12.5) | 27 (9.2) | 1.00 | |
| Employment Status | |||||
| Employed (full-time/part-time/seasonally/self-employment) | 73 (23.1) | 3 (12.5) | 70 (24.0) | 0.182 | 0.42 (0.12, 1.49) |
| Student (part-time/full-time) | 24 (7.6) | 1 (4.2) | 23 (7.9) | 0.422 | 0.43 (0.05, 3.37) |
| Unemployed | 219 (69.3) | 20 (83.3) | 199 (68.1) | 1.00 | |
| Co-morbid conditions | |||||
| Shortness of breath | |||||
| Yes | 156 (49.2) | 13 (54.2) | 143 (48.8) | 0.607 | 1.24 (0.54, 2.83) |
| No | 161 (50.8) | 11 (45.8) | 150 (51.2) | 1.00 | |
| Loud snoring | |||||
| Yes | 51 (16.1) | 3 (12.5) | 48 (16.4) | 0.163 | 0.73 (0.21, 2.55) |
| No | 265 (83.9) | 21 (87.5) | 244 (75.4) | 1.00 | |
| Ever Dr. said | |||||
| Chronic lung diseases * | |||||
| Yes | 81 (25.6) | 9 (37.5) | 72 (24.8) | 0.163 | 1.84 (0.78, 4.35) |
| No | 236 (74.4) | 15 (62.2) | 221 (75.2) | 1.00 | |
| Sinus trouble | |||||
| Yes | 85 (30.8) | 7 (31.8) | 78 (30.7) | 0.908 | 1.05 (0.43, 2.58) |
| No | 191 (69.2) | 15 (68.2) | 176 (69.3) | 1.00 | |
| Heart problem | |||||
| Yes | 25 (8.1) | 1 (4.2) | 24 (8.5) | 0.456 | 0.47 (0.07, 3.39) |
| No | 283 (91.9) | 23 (95.8) | 260 (91.5) | 1.00 | |
| Tuberculosis | |||||
| Yes | 24 (8.9) | 1 (4.5) | 23 (9.3) | 0.469 | 0.47 (0.06, 3.65) |
| No | 246 (91.1) | 21 (95.5) | 225 (90.7) | 1.00 | |
| Attack of bronchitis | |||||
| Yes | 81 (29.9) | 5 (22.7) | 76 (30.5) | 0.444 | 0.67 (0.24, 1.86) |
| No | 190 (70.1) | 17 (77.3) | 173 (69.5) | 1.00 | |
| Asthma | |||||
| Yes | 47 (14.8) | 4 (16.7) | 43 (14.7) | 0.794 | 1.16 (0.38, 3.57) |
| No | 270 (85.2) | 20 (83.3) | 250 (85.3) | 1.00 | |
| Diabetes | |||||
| Yes | 42 (13.8) | 5 (20.8) | 37 (13.2) | 0.310 | 1.74 (0.60, 5.04) |
| No | 263 (86.2) | 19 (79.2) | 244 (86.8) | 1.00 | |
| Depression | |||||
| Yes | 61 (19.9) | 7 (29.2) | 54 (19.1) | 0.238 | 1.75 (0.69, 4.42) |
| No | 246 (80.1) | 17 (70.8) | 229 (80.9) | 1.00 | |
| Ear infection | |||||
| Yes | 44 (14.1) | 4 (16.7) | 40 (13.9) | 0.716 | 1.24 (0.39, 3.88) |
| No | 268 (85.9) | 20 (83.3) | 248 (86.1) | 1.00 | |
| Heart burn/Stomach Reflex | |||||
| Yes | 50 (16.0) | 5 (21.7) | 45 (15.5) | 0.440 | 1.51 (0.53, 4.31) |
| No | 263 (84.0) | 18 (78.3) | 253 (84.5) | 1.00 | |
| Socio-economic factors | |||||
| Money left over at the end of month | |||||
| Not enough money | 156 (51.7) | 17 (77.3) | 139 (49.6) | 0.072 | 3.09 (0.91, 10.57) |
| Just enough money | 67 (22.2) | 2 (9.1) | 65 (23.2) | 0.784 | 0.78 (0.13, 4.60) |
| Some money | 79 (26.1) | 3 (13.6) | 76 (27.1) | 1.00 | |
| Housing conditions | |||||
| House in need of repairs | |||||
| Yes (major repair) | 123 (41.4) | 10 (45.5) | 113 (41.1) | 0.086 | 3.86 (0.83, 18.04) |
| Yes (minor repair) | 85 (28.6) | 10 (45.5) | 75 (27.3) | 0.026 | 5.82 (1.23, 27.52) |
| No (only regular maintenance) | 89 (30.0) | 2 (9.1) | 87 (31.6) | 1.00 | |
| In past 12 months, water or dampness in home | |||||
| Yes | 182 (63.4) | 18 (85.7) | 164 (61.7) | 0.035 | 3.73 (1.10, 12.66) |
| No | 106 (36.6) | 3 (14.3) | 102 (38.3) | 1.00 | |
| Damage caused by dampness | |||||
| Yes | 153 (48.3) | 16 (66.7) | 137 (46.8) | 0.061 | 2.28 (0.96, 5.39) |
| No | 164 (51.7) | 8 (33.3) | 156 (53.2) | 1.00 | |
| Mildew/moldy odor or musty smell | |||||
| Yes | 153 (53.9) | 16 (72.7) | 137 (52.3) | 0.075 | 2.43 (0.91, 6.46) |
| No | 131 (46.1) | 6 (27.3) | 125 (47.7) | 1.00 | |
| Signs of mold or mildew in home | |||||
| Yes | 133 (48.0) | 12 (57.1) | 121 (47.3) | 0.385 | 1.49 (0.61, 3.66) |
| No | 144 (52.0) | 9 (42.9) | 135 (52.7) | 1.00 | |
* We used the term “chronic lung diseases” to include one or more of emphysema, chronic bronchitis, chronic cough/chronic phlegm and COPD.
Certain baseline variables associated with the incidence of subjective EDS at p < 0.20 were considered as candidate variables in the multivariable model [29] and included chronic lung diseases, depression, money left over at the end of the month, having a house in need of repairs, water or dampness in the home in the past 12 months, damage caused by dampness, and mildew or moldy odor or musty smell. Table 2 presents the results from the multivariable analysis. The multivariable analysis was divided into three models because of the possible relationship between having a house in need of repairs and the indices of home dampness.
Table 2.
Multivariable association between newly identified subjective daytime sleepiness and risk factors.
| Model 1 † | Model 2 † | Model 3 † | ||||
|---|---|---|---|---|---|---|
| Adjusted OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | Adjusted OR (95% CI) | p Value | |
| Socio-economic factors | ||||||
| Money left over at the end of month | ||||||
| Not enough money | 3.83 (1.02, 14.43) | 0.047 | 4.62 (1.11, 19.32) | 0.036 | 3.32 (0.93, 11.79) | 0.064 |
| Just enough money | 0.85 (0.13, 5.63) | 0.873 | 1.08 (0.16, 7.43) | 0.937 | 0.69 (0.12, 4.12) | 0.684 |
| Some money | 1.00 | 1.00 | ||||
| Housing conditions | ||||||
| House in need of repairs | ||||||
| Yes (major repair) | 4.47 (0.86, 23.14) | 0.074 | ||||
| Yes (minor repair) | 5.72 (1.10, 29.73) | 0.038 | ||||
| No (only regular maintenance) | 1.00 | |||||
| In past 12 months, water or dampness in home | ||||||
| Yes | 3.54 (1.02, 12.22) | 0.046 | ||||
| No | 1.00 | |||||
| Damage caused by dampness | ||||||
| Yes | 2.79 (1.02, 7.65) | 0.046 | ||||
| No | 1.00 | |||||
† Results are presented as adjusted odds ratios (OR) and 95% confidence intervals (95% CI). Adjusted for age, sex, body mass index, smoking status, and variables in the table. Correlation between dampness and repair is 0.356 (Spearman’s rho), and correlation between damage caused by dampness and repair is 0.444 and moderately correlated. Correlation between dampness and damage caused by dampness is 0.612 and highly correlated.
After adjusting for age, sex, BMI, and smoking status at baseline, not having enough money left over at end of the month and house in need of minor repairs were significant predictors for the incidence of subjective EDS (Table 2—Model 1). Also, after adjusting for age, sex, BMI, and smoking status at baseline, not having enough money left over at end of the month and water or dampness in the home in the past 12 months were significant predictors for the development of subjective EDS (Table 2—Model 2). After adjusting for age, sex, BMI, smoking status and money left over at end of the month at baseline, damage caused by dampness was significant predictor for the development of subjective EDS (Table 2—Model 3).
3. Discussion
The four-year incidence of subjective EDS in these two First Nations communities was found to be 7.6%. Not having enough money left over at end of the month, having a house in need of repairs, water or dampness in the home in the past 12 months, and damage caused by dampness were the main predictors of new cases of subjective EDS four years later.
Poor housing is a major concern in First Nations communities in Canada [30,31]. According to the 2016 Canada Census, one quarter (24.2%) of First Nations people lived in a dwelling that was in need of major repairs and 31.8% lived in dwellings that were in need of minor repairs. In 2016, 23.1% of First Nations people lived in crowded homes [30]. In this study, 41.4% of the participants lived in a dwelling that was in need of major repairs and 32.6% of the participants lived in crowded homes. In an earlier Canadian study with two other First Nations communities, First Nations’ houses were shown to be crowded with poor ventilation and the presence of mold [32].
According to the 2011 National Household Survey, the overall median income of First Nations participants was $23,600, and the median income for those with post-secondary qualifications was $33,100 [33]. Many First Nations people live well below the poverty line [34]. In the current study, 51.7% of the participants reported that they do not have enough money left over at the end of the month. Furthermore, those who did not have enough money left over at the end of the month or those who lived in a house in need of minor repairs also had a higher incidence of subjective EDS. Financial stress due to lack of work and poor health status can lead to insomnia [35,36]. Previous studies have shown financial stress and low income have been associated with subjective EDS [18,37].
The domestic environment of people living in poverty can lead to less than optimal sleep quality [38]. For example, poorly controlled temperature or high humidity can cause sleep deprivation [39]. People living in crowded homes where poverty also exists often need to share their meals and beds to sleep. Going to bed hungry or not having enough space for sleeping effects the quality of sleep, and the lack of sleep quality could lead to sleepiness during the day.
In the current study, water or dampness in home during the past 12 months and damage caused by dampness were associated with the incidence of subjective EDS. In previous studies mold and dampness have been shown to be related to insomnia [24,25,26] and additionally, insomnia can lead to subjective EDS [40]. One possible mechanism that could explain the association between insomnia and building dampness is that building dampness can increase the emission of volatile organic compounds, impair air quality, dry mucous membranes, leading to sensory perceptions of worsening sleep quality [25]. Another mechanism that could explain this association is that dampness can cause nasal mucosal swelling and inflammation which could lead to impaired sleep quality [25]. The findings in this study were further supported by a study involving German children [26] in which exposure to visible mold or dampness in the home was observed increase the risk of insomnia related symptoms. It is possible that mold and home dampness could result in subjective EDS, both as a result of sleep deprivation due to insomnia, and/or due to irritation of the mucous membranes of the nose and oropharynx.
Limitations of the Study
This study had sample size of 317 and a less than optimal follow-up rate (45.2%). There were no differences in age and body mass index between follow-up and lost to follow-up participants. But, a significantly higher proportion of male participants were lost to follow-up. According to the Canadian Census of 2016 [41,42], the participants were not representative of the general population of these communities. There were more females and younger people who participated in the study and therefore, results cannot be generalized to populations of these communities. There were several major limitations of this study. Sleep status was measured subjectively by the Epworth Sleepiness Scale (ESS). There are differences between subjective (ESS) and objective sleepiness (e.g., multiple sleep latency test (MSLT)) measures. The ESS and MLST assess distinct aspects of sleepiness [43]. The ESS captured a subject’s self-reported level of sleep tendency in particular situation, on the other hand, MSLT used physiological data to assess the rate of falling asleep in an environment that is considered to be most suitable for sleep [43]. Another major limitation was that major sleep variables such as sleep duration, sleep disorders (as sleep-disordered breathing or insomnia), or the use of psychotropic drugs affecting sleep were not collected in this study. The measures of dampness and mold were self-reported and require objective confirmation. Lastly, although residents were living in the same community at both time points, there was a possibility that the participants were not living in the same home at the time of the second data collection. However, many of the homes of study participants were in need of major repairs. Thus, results should be interpreted with these limitations in mind.
4. Materials and Methods
4.1. Study Sample
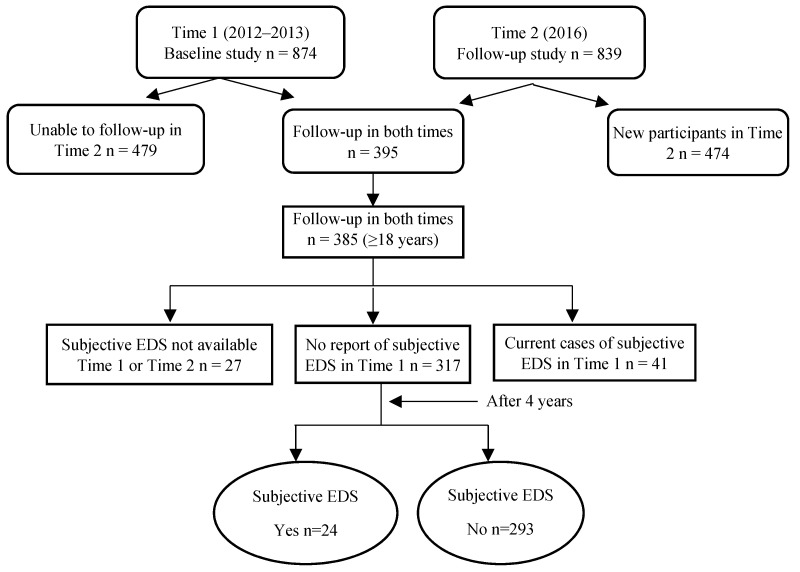
The data for this study came from the baseline assessments and follow-up evaluations (after 4 years) as part of the First Nations Lung Health Project (FNLHP) conducted in two Cree First Nations communities (Community A and Community B) in Saskatchewan in 2012–2013 [44] and 2016. The original purpose of the FNLHP was to examine the predictors of respiratory health in First Nations populations and the investigation of sleep was a secondary consideration. There were 874 individuals who participated in the baseline survey and 839 who participated in a follow-up survey. The follow-up rate of those who participated at baseline and in the follow-up survey was 45.2% (395/874). A questionnaire was interviewer-administered to adult participants. Of those, 385 of them were aged 18 years and older. Data for subjective EDS were not available for 27 individuals at either baseline, follow-up, or both. There were 41 individuals who had been identified as current cases of subjective EDS at baseline. The prevalence of subjective EDS was 10.6% (41/385). After removing those cases (current cases and those lost to follow-up, n = 68), there were 317 individuals with no report of subjective EDS at baseline and who had participated in the follow-up questionnaire (Figure 1). The study was approved by the University of Saskatchewan’s Biomedical Research Ethics Board (Certificate No. Bio #12-89) and adhered to all of the criteria outlined in Chapter 9 entitled Research Involving the First Nations, Inuit, and Metis Peoples of Canada found in the Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans [45]. Written consent was obtained from all participants.
Figure 1.
Study Sample.
4.2. Data Collection
Trained community research assistants conducted the baseline and the follow-up interviews at both time points. Adults 18 years and older were invited to the Community Health Centre to complete the interviewer-administered questionnaires and clinical assessments. This manuscript is based on the data from the questionnaire assessments. The Epworth Sleepiness Scale (ESS) [46,47,48,49] questionnaire was used to assess the degree of EDS. The ESS has not been validated in Australian Indigenous populations [50] or Canadian Indigenous populations. An ESS score >10 [17,46] was considered to be abnormal and was used to identify a case of subjective EDS at both at baseline and at the four-year follow-up. Independent variables of interest at baseline were self-reported age, sex, body mass index (BMI), education level, marital status, smoking status, alcohol consumption and employment status. “Doctor ever diagnosed” conditions included sinus trouble, heart problem, heart attack, tuberculosis, attack of bronchitis, emphysema, chronic bronchitis, COPD, asthma, diabetes, and depression. Other factors obtained through the questionnaire included respiratory symptoms such as chronic cough, chronic phlegm, shortness of breath (SOB), loud snoring, and money left over at end of the month. In addition, presence of environmental conditions in the home included state of house repairs; water or dampness from broken pipes, leaks, heavy rain or floods during the past 12 months; damage caused by dampness; mildew/moldy odor or musty smell; signs of mold or mildew; and number of persons per room as an index of crowding. For the analysis, the term “chronic lung diseases” was used to include one or more of emphysema, chronic bronchitis, chronic cough/chronic phlegm, and COPD.
4.3. Statistical Analysis
Statistical analyses were conducted using SPSS version 24 (IBM SPSS Statistics for Windows. Armonk, NY: IBM Corp., 2017). Logistic regression models were used to assess relationships between abnormal ESS and covariates at baseline. A multilevel logistic regression model using a generalized estimating equations approach was used to develop the model with individuals (first level) clustering within households (second level). The significant contributions of potential risk factors, confounders, and interactive effects were determined by developing a series of multilevel models. Variables with p < 0.20 in the univariate analysis became factors for the multivariable model [29]. In these analyses, the indicators of housing conditions were included separately. The variables retained in the final multivariable model included those that were statistically significant (i.e., p < 0.05) as well as age, sex, BMI, and smoking status. Odds ratios (ORs) and 95% confidence intervals (CIs) were used to present the strength of the associations.
5. Conclusions
The association between the incidence of subjective EDS and not having enough money left over at the end of the month, having a house in need of repairs, water or dampness in homes in past 12 months, and damage caused by dampness were novel findings and may be important public health issues. Further investigation into the mechanisms which influence these associations are necessary, while at the same time, provisions for addressing in-home dampness and mold are critical.
Acknowledgments
The First Nations Lung Health Project Team consists of: James A. Dosman (Designated Principal Investigator, University of Saskatchewan, Saskatoon, SK, Canada); Punam Pahwa (Co-Principal Investigator, University of Saskatchewan, Saskatoon, SK, Canada); Jo-Ann Episkenew (Co-Principal Investigator (deceased), Former Faculty of Indigenous People’s Health Research Centre, University of Regina, SK, Canada), Sylvia Abonyi (Co-Principal Investigator, University of Saskatchewan, Saskatoon, SK, Canada); Co-Investigators: Mark Fenton, John Gordon, Bonnie Janzen, Chandima P. Karunanayake, Malcolm King, Shelley Kirychuk, Niels Koehncke, Joshua A. Lawson, Gregory Marchildon, Lesley McBain, Donna C. Rennie, Vivian R. Ramsden, Ambikaipakan Senthilselvan; Collaborators: Amy Zarzeczny; Louise Hagel, Breanna Davis, John Dosman, Roland Dyck, Thomas Smith-Windsor, William Albritton; External Advisor: Janet Smylie; Project Manager: Kathleen McMullin; Community Partners: Jeremy Seeseequasis; Raina Henderson; Arnold Naytowhow; Laurie Jimmy. We are grateful for the contributions from Elders and community leaders that facilitated the engagement necessary for the study, and all participants who donated their time to participate.
Abbreviations
| EDS | Excessive daytime sleepiness |
| ESS | Epworth Sleepiness Scale |
| FNLHP | First Nations Lung Health Project |
| BMI | Body Mass Index |
| COPD | Chronic Obstructive Pulmonary Disease |
| SOB | Shortness of Breath |
| SD | Standard Deviation |
| MSLT | Multiple Sleep Latency Test |
Author Contributions
C.P.K. authored most of the paper, carried out the statistical analysis, reviewed the literature, reviewed the citations, and created the abstract and manuscript. J.A.D., P.P. and S.A. are the co-principal investigators of the F.N.L.H.P.R.T., C.P.K., D.C.R., J.A.L., S.K., M.F., S.A., J.A.D., and P.P. contributed to grant writing, development of study design, questionnaire development, and study coordination. V.R.R. provided input into the writing of the manuscript; and, edited the manuscript. J.S. served as “content experts” for the research project engaged in document review/editing and support during the data collection phases of the survey. All other co-authors significantly contributed to manuscript preparation. The First Nations Lung Health Project members contributed during the grant writing and questionnaires development and with conducting the survey. All authors read and approved the final manuscript.
Funding
The FNLHP was funded by a grant from the Canadian Institutes of Health Research “Assess, Redress, Re-assess: Addressing Disparities in Respiratory Health among First Nations People”, CIHR MOP-246983-ABH-CCAA-11829.
Conflicts of Interest
The authors declare that there is no conflict of interest regarding the publication of this article. The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, and in the decision to publish the results.
References
- 1.National Sleep Foundation What Is Excessive Sleepiness? [(accessed on 26 April 2018)]; Available online: https://sleepfoundation.org/excessivesleepiness/content/what-excessive-sleepiness.
- 2.Chastens E.R., Olshansky E. Daytime sleepiness, diabetes, and psychological well-being. Issues Ment. Health Nurs. 2008;29:1134–1150. doi: 10.1080/01612840802319878. [DOI] [PubMed] [Google Scholar]
- 3.Mirghani H.O., Elbadawi A.S. Depression, anxiety, and daytime sleepiness among type 2 diabetic patients and their correlation with the diabetes control: A case-control study. J. Taibah Univ. Medical. Sci. 2016;11:374–379. doi: 10.1016/j.jtumed.2016.05.009. [DOI] [Google Scholar]
- 4.Newman A.B., Spiekerman C.F., Enright P., Lefkowitz D., Manolio T., Reynolds C.F., Robbins J. Daytime sleepiness predicts mortality and cardiovascular disease in older adults. The Cardiovascular Health Study Research Group. J. Am. Geriatr. Soc. 2000;48:115–123. doi: 10.1111/j.1532-5415.2000.tb03901.x. [DOI] [PubMed] [Google Scholar]
- 5.Endeshaw Y., Rice T.B., Schwartz A.V., Stone K.L., Manini T.M., Suzanne Satterfield S., Cummings S., Harris T., Pahor M., for the Health ABC Study Snoring, Daytime Sleepiness, and Incident Cardiovascular Disease in The Health, Aging, and Body Composition Study. Sleep. 2013;36:1737–1745. doi: 10.5665/sleep.3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Šiarnik P., Klobučníková K., Šurda P., Putala M., Šutovský S., Kollár B., Turčáni P. Excessive Daytime Sleepiness in Acute Ischemic Stroke: Association with Restless Legs Syndrome, Diabetes Mellitus, Obesity, and Sleep-Disordered Breathing. J. Clin. Sleep Med. 2018;14:95–100. doi: 10.5664/jcsm.6890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chellappa S.L., Schröder C., Cajochen C. Chronobiology, excessive daytime sleepiness and depression: Is there a link? Sleep Med. 2009;10:505–514. doi: 10.1016/j.sleep.2008.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Guda N., Partington S., Shaw M.J., Leo G., Vakil N. Unrecognized GERD symptoms are associated with excessive daytime sleepiness in patients undergoing sleep studies. Dig. Dis. Sci. 2007;52:2873–2876. doi: 10.1007/s10620-007-9768-6. [DOI] [PubMed] [Google Scholar]
- 9.Sergio Garbarino S., Durando P., Guglielmi O., Dini G., Francesca Bersi F., Fornarino S., Toletone A., Chiorri C., Magnavita N. Sleep Apnea, Sleep Debt and Daytime Sleepiness Are Independently Associated with Road Accidents. A Cross-Sectional Study on Truck Drivers. PLoS ONE. 2016;11:e0166262. doi: 10.1371/journal.pone.0166262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Özer C., Etcibaşı S., Öztürk L. Daytime sleepiness and sleep habits as risk factors of traffic accidents in a group of Turkish public transport drivers. Int. J. Clin. Exp. Med. 2014;7:268–273. [PMC free article] [PubMed] [Google Scholar]
- 11.Garbarino S., Nobili L., Beelke M., De Carli F., Ferrillo F. The contributing role of sleepiness in highway vehicle accidents. Sleep. 2001;24:203–206. doi: 10.1093/sleep/24.2.1a. [DOI] [PubMed] [Google Scholar]
- 12.Connor J., Norton R., Ameratunga S., Robinson E., Civil I., Dunn R., Bailey J., Jackson R. Driver sleepiness and risk of serious injury to car occupants: Population based case control study. BMJ. 2002;324:1125. doi: 10.1136/bmj.324.7346.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tefft B.C. Prevalence of motor vehicle crashes involving drowsy drivers, United States, 1999–2008. Accid Anal. Prev. 2012;45:180–186. doi: 10.1016/j.aap.2011.05.028. [DOI] [PubMed] [Google Scholar]
- 14.Gonçalves M., Amici R., Lucas R., Åkerstedt T., Cirignotta F., Horne J., Léger D., McNicholas W.T., Partinen M., Téran-Santos J., et al. Sleepiness at the wheel across Europe: A survey of 19 countries. J. Sleep Res. 2015;24:242–253. doi: 10.1111/jsr.12267. [DOI] [PubMed] [Google Scholar]
- 15.Jaussent I., Morin C.M., Ivers H., Dauvilliers Y. Incidence, worsening and risk factors of daytime sleepiness in a population-based 5-year longitudinal study. Sci. Rep. 2017;7:1372. doi: 10.1038/s41598-017-01547-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pahwa P., Karunanayake C.P., Hagel L., Gjevre J.A., Rennie D., Lawson J., Dosman J.A. Prevalence of high Epworth sleepiness scale in a rural population. Can. Respir. J. 2012;19:e10–e14. doi: 10.1155/2012/287309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gjevre J.A., Pahwa P., Karunanayake C., Hagel L., Rennie D., Lawson J., Dyck R., Dosman J., Saskatchewan Rural Health Study Team Excessive daytime sleepiness among rural residents in Saskatchewan. Can. Respir. J. 2014;21:227–233. doi: 10.1155/2014/921541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van der Spuy I., Karunanayake C.P., Dosman J.A., McMullin K., Zhao G., Abonyi S., Rennie D.C., Lawson J., Kirychuk S., MacDonald J., et al. Determinants of excessive daytime sleepiness in two First Nation communities. BMC Pulm. Med. 2017;17:192. doi: 10.1186/s12890-017-0536-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stringhini S., Haba-Rubio J., Marques-Vidal P., Waeber G., Preisig M., Guessous I., Bovet P., Vollenweider P., Tafti M., Heinzer R. Association of socioeconomic status with sleep disturbances in the Swiss population-based CoLaus study. Sleep Med. 2015;16:469–476. doi: 10.1016/j.sleep.2014.12.014. [DOI] [PubMed] [Google Scholar]
- 20.Jarrin D.C., McGrath J.J., Silverstein J.E., Drake C. Objective and subjective socioeconomic gradients exist for sleep quality, sleep latency, sleep duration, weekend oversleep, and daytime sleepiness in adults. Behav. Sleep Med. 2013;11:144–158. doi: 10.1080/15402002.2011.636112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mendell M.J., Mirer A.G., Cheung K., Tong M., Douwes J. Respiratory and allergic health effects of dampness, mold, and dampness-related agents: A review of the epidemiologic evidence. Environ. Health Perspect. 2011;119:748–756. doi: 10.1289/ehp.1002410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tischer C., Chen C.M., Heinrich J. Association between domestic mould and mould components, and asthma and allergy in children: A systematic review. Eur. Respir. J. 2011;38:812–824. doi: 10.1183/09031936.00184010. [DOI] [PubMed] [Google Scholar]
- 23.Tischer C.G., Hohmann C., Thiering E., Herbarth O., Müller A., Henderson J., Granell R., Fantini M.P., Luciano L., Bergström A., et al. Meta-analysis of mould and dampness exposure on asthma and allergy in eight European birth cohorts: An ENRIECO initiative. Allergy. 2011;66:1570–1579. doi: 10.1111/j.1398-9995.2011.02712.x. [DOI] [PubMed] [Google Scholar]
- 24.Packer C.N., Stewart-Brown S., Fowle S.E. Damp housing and adult health: Results from a lifestyle study in Worcester, England. J. Epidemiol. Community Health. 1994;48:555–559. doi: 10.1136/jech.48.6.555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Janson C., Norbäck D., Omenaas E., Gislason T., Nyström L., Jõgi R., Lindberg E., Gunnbjörnsdottir M., Norrman E., Wentzel-Larsen T., et al. Insomnia is more common among subjects living in damp buildings. Occup. Environ. Med. 2005;62:113–118. doi: 10.1136/oem.2003.011379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tiesler C., Thiering E., Tischer C., Lehmann I., Schaaf B., von Berg A., Heinrich J. Exposure to visible mould or dampness at home and sleep problems in children: Results from the LISAplus study. Environ. Res. 2015;137:357–363. doi: 10.1016/j.envres.2014.11.023. [DOI] [PubMed] [Google Scholar]
- 27.Hara C., Stewart R., Lima-Costa M.F., Rocha F.P., Fuzikawa C., Uchoa E., Firmo J.O.A., Castro-Costa E. Insomnia Subtypes and Their Relationship to Excessive Daytime Sleepiness in Brazilian Community-Dwelling Older Adults. Sleep. 2011;34:1111–1117. doi: 10.5665/SLEEP.1172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kao C.C., Huang C.J., Wang M.Y., Tsai P.S. Insomnia: Prevalence and its impact on excessive daytime sleepiness and psychological well-being in the adult Taiwanese population. Qual. Life Res. 2008;17:1073–1080. doi: 10.1007/s11136-008-9383-9. [DOI] [PubMed] [Google Scholar]
- 29.Hosmer D.W., Lemeshow S., Sturdivant R.X. Applied Logistic Regression. 3rd ed. John Wiley & Sons Inc.; Hoboken, NJ, USA: 2013. Model-building strategies and methods for logistic regression; pp. 89–144. [Google Scholar]
- 30.Statistics Canada . Census in Brief: The Housing Conditions of Aboriginal People in Canada. Statistics Canada; Ottawa, ON, Canada: 2017. [(accessed on 26 April 2018)]. Available online: http://www12.statcan.gc.ca/census-recensement/2016/as-sa/98-200-x/2016021/98-200-x2016021-eng.pdf. [Google Scholar]
- 31.Carrière G.M., Garner R., Sanmartin C. Housing conditions and respiratory hospitalizations among First Nations people in Canada. Health Rep. 2017;28:9–15. [PubMed] [Google Scholar]
- 32.Larcombe L., Nickerson P., Singer M., Robson R., Dantouze J., Mckey L., Orr P. Housing conditions in 2 Canadian First Nations Communities. Int. J. Circumpolar Health. 2011;70:141–153. doi: 10.3402/ijch.v70i2.17806. [DOI] [PubMed] [Google Scholar]
- 33.Statistics Canada Aboriginal Statistics at a Glance: 2nd Edition. [(accessed on 4 May 2018)]; Available online: http://www.statcan.gc.ca/pub/89-645-x/89-645-x2015001-eng.pdf.
- 34.Statistics Canada . 2016 Census of Population, Data Tables, 2016 Census-Aboriginal Identity (9), Employment Income Statistics. Statistics Canada; Ottawa, ON, Canada: 2018. [(accessed on 28 June 2018)]. Available online: https://www12.statcan.gc.ca/census-recensement/2016/rt-td/ap-pa-eng.cfm. [Google Scholar]
- 35.Talala K.M., Martelin T.P., Haukkala A.H., Härkänen T.T., Prättälä R.S. Socio-economic differences in self-reported insomnia and stress in Finland from 1979 to 2002: A population-based repeated cross-sectional survey. BMC Public Health. 2012;12:650. doi: 10.1186/1471-2458-12-650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fernandez-Mendoza J., Vgontzas A.N. Insomnia and Its Impact on Physical and Mental Health. Curr. Psychiatry Rep. 2013;15:418. doi: 10.1007/s11920-013-0418-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Adams R.J., Appleton S.L., Vakulin A., Lang C., Martin S.A., Taylor A.W., McEvoy R.D., Antic N.A., Catcheside P.G., Wittert G.A. Association of daytime sleepiness with obstructive sleep apnoea and comorbidities varies by sleepiness definition in a population cohort of men. Respirology. 2016;21:1314–1321. doi: 10.1111/resp.12829. [DOI] [PubMed] [Google Scholar]
- 38.Chambers E., Pichardo M.S., Rosenbaum E. Sleep and the housing and neighborhood environment of urban Latino adults living in low-income housing: The AHOME Study. Behav. Sleep Med. 2016;14:169–184. doi: 10.1080/15402002.2014.974180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Strøm-Tejsen P., Zukowska D., Wargocki P., Wyon D.P. The effects of bedroom air quality on sleep and next-day performance. Indoor Air. 2016;26:679–686. doi: 10.1111/ina.12254. [DOI] [PubMed] [Google Scholar]
- 40.Wilsmore B.R., Grunstein R.R., Fransen M., Woodward M., Norton R., Ameratunga S. Sleep habits, insomnia, and daytime sleepiness in a large and healthy community-based sample of New Zealanders. J. Clin. Sleep Med. 2013;9:559–566. doi: 10.5664/jcsm.2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Statistics Canada Census Profile. 2016 Census. [(accessed on 29 August 2018)]; Beardy’s 97 and Okemasis 96, IRI [Census subdivision], Saskatchewan and Saskatchewan [Province] (Table). Statistics Canada Catalogue no. 98-316-X2016001. Ottawa. Released November 29, 2017. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E.
- 42.Statistics Canada Census Profile. 2016 Census. [(accessed on 29 August 2018)]; Montreal Lake 106, IRI [Census subdivision], Saskatchewan and New Brunswick [Province] (Table). Statistics Canada Catalogue no. 98-316-X2016001. Ottawa. Released November 29, 2017. Available online: https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/index.cfm?Lang=E.
- 43.Aurora R.N., Caffo B., Crainiceanu C., Punjabi N.M. Correlating Subjective and Objective Sleepiness: Revisiting the Association Using Survival Analysis. Sleep. 2011;34:1707–1714. doi: 10.5665/sleep.1442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pahwa P., Abonyi S., Karunanayake C., Rennie D.C., Janzen B., Kirychuk S., Lawson J.A., Katapally T., McMullin K., Seeseequasis J., et al. A community-based participatory research methodology to address, redress, and reassess disparities in respiratory health among First Nations. BMC Res. Notes. 2015;8:199–209. doi: 10.1186/s13104-015-1137-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Canadian Institutes of Health Research. Natural Sciences and Engineering Research Council of Canada. Social Sciences and Humanities Research Council of Canada Tri-Council Policy Statement: Ethical Conduct for Research Involving Humans. [(accessed on 31 August 2018)];2014 Dec; Available online: http://www.pre.ethics.gc.ca/pdf/eng/tcps2-2014/TCPS_2_FINAL_Web.pdf.
- 46.Johns M.W. A new method for measuring daytime sleepiness: The Epworth Sleepiness Scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 47.Johns M.W. Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep. 1992;15:376–381. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 48.Johns M.W. Daytime sleepiness, snoring, and obstructive sleep apnea: The Epworth Sleepiness Scale. Chest. 1993;103:30–36. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 49.Johns M.W. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep. 1994;17:703–710. doi: 10.1093/sleep/17.8.703. [DOI] [PubMed] [Google Scholar]
- 50.Woods C.E., McPherson K., Tikoft E., Usher K., Hosseini F., Ferns J., Jersmann H., Antic R., Maguire G.P. Sleep Disorders in Aboriginal and Torres Strait Islander People and Residents of Regional and Remote Australia. J. Clin. Sleep Med. 2015;11:1263–1271. doi: 10.5664/jcsm.5182. [DOI] [PMC free article] [PubMed] [Google Scholar]