Abstract
Context:
The Aspiring DOctors PreCollege Program at the Ohio University Heritage College of Osteopathic Medicine Cleveland Campus is unique among other precollege pipeline and mini-medical school programs in that it engages learners from urban underserved communities for an entire academic year as a cocurricular adjunct to their high school course load. One day per month, students are brought to the medical college campus and introduced to the field of osteopathic medicine. Students also participate in activities related to preparing for college admissions, diversity in higher education, mental health and wellness, and financial stewardship. All these activities are done with the goal of increasing the number of underrepresented minority (URM) students in the health care professions.
Objective:
Self-efficacy has been identified as a measure of internal motivation and belief in one’s ability to succeed in the face of challenges. The purpose of this study is to determine what effect, if any, participation in this program has on URM student self-efficacy.
Methods:
Students were asked to complete a validated self-efficacy questionnaire at the start and end of this program to determine their levels of self-efficacy and if there were changes after participating in this program.
Results:
Ten of the 12 seniors completed pre- and post-self-efficacy surveys. Two main discoveries were made through this pilot. First, when tested at the beginning of the program, all students had high levels of self-efficacy (mean score, 4.45 of 5). Second, 2 items were specifically increased by a statistically significant amount. The students increased in self-efficacy concerning the responses “I can learn what is being taught in class this year” (P = .024) and “My ability grows with effort” (P = .015).
Conclusions:
With the competitive standards of acceptance into the Aspiring DOctors PreCollege Program, students enrolled in this program had high levels of self-efficacy from the onset. While there was modest increase across the board, many of these indicators remained consistently high after the program. Using self-efficacy as a screening tool for premedical students may be helpful in identifying candidates likely to succeed in a future medical career.
Keywords: Self-Efficacy, Secondary Education, Premedical Education, Underrepresented Minorities
Introduction
In light of the current and forecasted shortage of health care professionals, medical schools have sought innovative approaches to increase interest in health care professions in students at the early stages of their education. Pipeline and mini-medical school programs are an increasingly popular method to expose high school students to the medical field.1-5 These outreach programs are often targeted toward increasing the number of underrepresented minority (URM) students interested in the medical field.6-10 Many schools, both osteopathic and allopathic, have used these programs to engage with URM students from underresourced communities, both urban and rural, and inspire them to consider a career in medicine.11,12 Increasing the number of URM students is important as students from socioeconomically disadvantaged communities are more likely to choose careers in primary care and return to practices in underserved communities.13,14
The mission of the Ohio University Heritage College of Osteopathic Medicine (OUHCOM) is to train osteopathic primary care physicians and improve the health and well-being of underserved populations. On the Cleveland Campus, with its focus on urban communities, the Aspiring DOctors PreCollege Program was designed to bring the osteopathic medical college experience to high-achieving URM students with interests in health care careers. In contrast to other pipeline programs, the Aspiring DOctors PreCollege Program is a year-long program integrated with the high school curriculum for students selected from a competitive pool of applicants. One day per month, students come to the medical college campus for a variety of educational activities taught by university faculty and staff. This highly competitive program is deliberately limited to only a handful of the most motivated students from each partner school to ensure a high-quality experience and promote one-on-one interactions with the medical faculty.
Self-efficacy
Many measures of program effectiveness employed in the evaluation of pipeline programs center around high school graduation rates, college admissions test scores, and matriculation in health profession training programs. While these indicators are indeed valuable data points, the researchers were interested to see what effect these programs could have on intrinsic factors that would outlast the short-term measures related to test scores and college placement that carry over into the students’ professional lives and beyond. These factors included long-term career preparedness, improved reading and standardized test-taking skills, interpersonal communication, financial literacy, emotional regulation, and self-efficacy.
First described in 1977, self-efficacy is defined as “an individual’s belief in his or her capacity to execute behaviors necessary to produce specific [outcomes],” and “reflects confidence in the ability to exert control over one’s own motivation, behavior, and social environment.”15,16 It is theorized that self-efficacy is an internalized characteristic that can quantify one’s ability to define goals, self-motivate toward a determined outcome, and regulate one’s response to external environmental stressors. People with high self-efficacy—those who believe they can perform well—more likely do view difficult tasks as a challenge to be completed rather than something to be avoided.17
Self-efficacy in the educational field has been described as perceptions of one’s ability to perform at an expected level and achieve goals. Student levels of self-efficacy have been shown to influence motivation in school, learning ability, and achievements.18,19 According to the educational model described by Gaumer Erickson et al,20 the 2 overarching components of self-efficacy that can be built are (1) “Belief in Personal Ability” to meet goals and expectations and (2) “Belief that Ability Grows with Effort.”
As medical school requires significant goal-setting ability and self-motivation, a high level of self-efficacy is a desirable trait in potential medical students. Further, the regulatory response to the external stressor component of the self-efficacy theory could also serve as a predictor for students from socioeconomically disadvantaged backgrounds most likely to succeed in postsecondary education. The objective of this study is to determine what effect, if any, participation in a year-long pipeline program can have on the levels of self-efficacy in URM youth and their desire to pursue careers in the health care field.
Methods
Study population
Students from 4 urban high schools surrounding the OUHCOM Cleveland Campus were invited to apply for the Aspiring DOctors PreCollege Program. Approximately 35% of individuals in these communities are living below the federal poverty guidelines and have an average annual per capita income of US$21 513. Notably, only 17% of the population has earned bachelor’s degree or higher.21 The 4-year graduation rate in the urban communities served is approximately 65%, less than 5% of students are involved in Advanced Placement or Dual Credit college preparatory classes, and less than a third of students meet reading and writing proficiencies on their first attempt.22
From these dispirited environments, highly motivated high school juniors and seniors were given the opportunity to apply to this pipeline program. To apply, prospective students had to indicate an interest in a health care career, write an application essay, obtain a letter of recommendation from a teacher, and maintain a 3.5 or higher grade point average. Once selected, students had to return parental consent forms to participate in this program and this investigation which was approved by the Ohio University Institutional Review Board.
Program design and survey
The Aspiring Doctors Precollege Program was designed to promote osteopathic primary care through immersive, interactive, and hands-on educational experiences designed to expose students to situations common in osteopathic medical curricula and primary care practices. The curriculum develops critical thinking, problem-solving, and conceptual learning skills through activities such as case-based learning, cadaver dissection, osteopathic manipulation, and interacting with standardized patients. Specific educational programming was included that covers topics relevant to URM student experiences such as diversity in higher education, financial literacy, and mental health. In addition, precollege and workplace skills were emphasized to help scholars navigate the collegiate application process.
At the beginning and conclusion of this program, students were asked to complete the Self-Efficacy Formative Questionnaire, a validated, publicly accessible, 13-question survey instrument designed to measure self-efficacy specifically within a secondary education context.23 The instrument is scored on a 5-point Likert-type scale, with a value of 1 (not very like me) to 5 (very like me) designated by the respondent. The instrument has been used in several statewide public school assessment initiatives across the United States and has been included in more than 20 publications.24 This instrument was included in this study as part of a larger survey to assess students’ program experience and career aspirations.
Statistical methods
Survey responses are tabulated to form a single numeric score, with higher values indicating higher levels of self-efficacy. The responses were divided into 2 subscores representing 2 components of the self-efficacy model: belief that ability can grow with effort and belief in your ability to meet specific goals and/or expectations.
The students’ survey responses were paired so that comparisons could be drawn between the participant’s answers before and after program participation. SPSS version 25.0 (IBM Corp, Armonk, NY, USA) was used to analyze the data using Student’s paired t test to test for significance of repeated measures. A value of P < .05 was considered statistically significant.
Results
Ten of the 12 high school seniors who participated in the program in the 2018 to 2019 academic year (83.3%) completed both the preassessment and postassessment. Participants who did not complete the postassessment were excluded from significance testing, but partial responses were reviewed for trends and themes. These students were reflective of their communities in all demographic and socioeconomic categories. All participants (100%) came from families with no members completing a college degree.
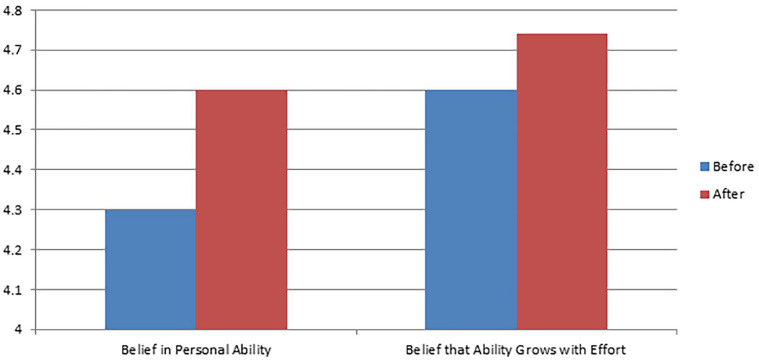
After completing the Aspiring DOctors PreCollege Program, students demonstrated an overall increase in all survey items. There was a statistically significant difference in 2 of the 13 items from the Self-Efficacy Formative Questionnaire (Table 1). Participants were statistically more likely to agree to the statements “I can learn what is being taught in class this year” (P = .024) and “My ability grows with effort” (P = .015). Although there was no statistically significant change overall in either of the 2 subscales, Belief in Personal Ability and Belief that Ability Grows with Effort, modest improvements were noted in both categories (Figure 1). Of particular note, all participants marked the item “I believe hard work pays off” with the highest value (5, Very Like Me) on both the preassessment and postassessment.
Table 1.
Participant responses to Self-Efficacy Formative Questionnaire.
| Preassessment | Postassessment | P value (<.05) | |
|---|---|---|---|
| Belief in Personal Ability | 4.4 | 4.6 | .246 |
| I can learn what is being taught in class this year. | 4.5 | 5 | .024* |
| I can figure out anything if I try hard enough. | 4.1 | 4.6 | .138 |
| If I practiced every day, I could develop just about any skill. | 4.3 | 4.5 | .591 |
| Once I have decided to accomplish something that is important to me, I keep trying to accomplish it, even if it is harder than I thought. | 4.8 | 4.5 | .343 |
| I am confident that I will achieve the goals that I set for myself. | 4.7 | 4.4 | .662 |
| When I am struggling to accomplish something difficult, I focus on my progress instead of feeling discouraged. | 3.8 | 4.4 | .121 |
| I will succeed in whatever career path I choose. | 4.4 | 4.7 | .373 |
| I will succeed in whatever college major I choose. | 4.4 | 4.7 | .168 |
| Belief that Ability Grows with Effort | 4.6 | 4.7 | .276 |
| I believe hard work pays off. | 5 | 5 | – |
| My ability grows with effort. | 4.6 | 5 | .015* |
| I believe that the brain can be developed like a muscle. | 4.5 | 4.9 | .168 |
| I think that no matter who you are, you can significantly change your level of talent. | 4.5 | 4.3 | .872 |
| I can change my basic level of ability considerably. | 4.3 | 4.5 | .394 |
| Total self-efficacy score | 4.5 | 4.7 | .224 |
Indicates statistically significant.
Figure 1.
Self-efficacy subscale scores before and after the Aspiring DOctors PreCollege Program.
Discussion
The first research discovery was that students who participated in the Aspiring DOctors PreCollege Program did show statistically significant change in 2 major components of self-efficacy. With significant curricular instruction and activities focused on critical learning skills and standardized test preparation, these efforts were reflected in the significant student response that “I can learn what is being taught in class this year” falling into the overarching category of “Belief in Personal Ability.” Another objective of this program, in addition to its introduction to the osteopathic profession and primary care, was to promote lifelong learning and confidence to tackle issues both inside and outside the classroom. Team building exercises, mental health discussion groups, and financial literacy workshops were all included as mechanisms to boost students’ confidence to successfully navigate the post-high school transition to higher education. After completion of the program, students were more likely to identify with the statement, “My ability grows with effort” falling into the second overarching category “Belief that Ability Grows with Effort” (see Figure 1).
The second discovery was that although there were some statistically significant changes in certain components of self-efficacy, there was only modest increase on most items. On the preprogram assessment, all the students displayed high levels of self-efficacy from the outset. Although the research team intended to determine if self-efficacy could be raised through participation in a pipeline program, it appears that the students who successfully applied and matriculated into this program already had high levels of self-efficacy. Rather than a metric for improvement, self-efficacy may be an early indicator of potential educational success in the health care field for socioeconomically disadvantaged students.
Supporting this research, the 4-year graduation rate for students at the urban schools who participate in this program is 65%, while all students who participated in this program were accepted to a postsecondary institution. Of those participants, 85% chose to pursue a career path in the health sciences. While an element of self-selection bias cannot be ignored, the use of a self-efficacy scale can be used to quantify the strength of that self-selection. Succeeding in medical education requires a high level of self-motivation and determination. Determining which students possess characteristics necessary to succeed is an important part of the medical school admissions process. By assessing and screening for measures like self-efficacy early, as early as high school, medical schools can direct resources to promising young candidates who otherwise would not have access to the same opportunities as their peers.
This study is limited by its small sample size. However, as a pilot program, it shows the potential effect that this type of programming can have for disadvantaged students. To increase the validity of these findings, large-scale evaluations from communities across the country would be necessary. In addition, longitudinal research on the college graduation rate, standardized test scores, and medical/graduate school admissions rates would be helpful in determining the long-term effects of this pipeline program.
Conclusions
The Aspiring DOctors PreCollege Program, unique in its continuous year-long cocurricular engagement with local urban and underprivileged school districts, was effective in raising some elements of self-efficacy in URM high school students. From the onset, however, these students began the program with high levels of self-efficacy, leaving little room for improvement on validated metrics. These findings suggest that early identification of students with high levels of self-efficacy could be a useful tool in recruiting and supporting exceptional URM high school students from socioeconomically disadvantaged communities in their pursuit of a career in osteopathic medicine.
Footnotes
Funding:The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of conflicting interests:The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Author Contributions: All authors (RR, JM, TN, SB) contributed to the design and implimentation of this program and study. RR and SB oversaw survey administration. JM conducted blinded data analysis. RM and JM drafted the intial manuscript draft. All authors provided substantial edits to produce final manuscript.
References
- 1. Cordell RL, Cordeira KL, Cohen LP, Bensyl DM. Building the pipeline: programs to introduce middle school, high school, medical, and veterinary students to careers in epidemiology and public health. Ann Epidemiol. 2017;27:752-755. doi: 10.1016/j.annepidem.2017.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Lyon GH, Jafri J, St Louis., K Beyond the pipeline: STEM pathways for youth development. Afterschool Matters. https://eric.ed.gov/?id=EJ992152. Published online 2012. Accessed September 28, 2019.
- 3. Blustein DL, Barnett M, Mark S, et al. Examining urban students’ constructions of a STEM/career development intervention over time. J Career Dev. 2013;40:40-67. doi: 10.1177/0894845312441680. [DOI] [Google Scholar]
- 4. Danner OK, Lokko C, Mobley F, et al. Hospital-based, multidisciplinary, youth mentoring and medical exposure program positively influences and reinforces health care career choice: “the reach one each one program early experience.” Am J Surg. 2017;213:611-616. doi: 10.1016/j.amjsurg.2016.12.002. [DOI] [PubMed] [Google Scholar]
- 5. Hamrick LA, Harter SR, Fox CL, Dhir M, Carrier RL. Just say know to drugs! a high school pharmacology enrichment program for a rural population. J Am Osteopath Assoc. 2019;119:199-207. doi: 10.7556/jaoa.2019.031. [DOI] [PubMed] [Google Scholar]
- 6. Hawkins BD. Building a foundation: special programs dedicate themselves to diversifying the pipeline in the field of medicine. Diverse Issues High Educ. 2016;22:10. [Google Scholar]
- 7. Atance J, Mickalis M, Kincade B. Educational intervention in a medically underserved area. J Am Osteopath Assoc. 2018;118:219-224. doi: 10.7556/jaoa.2018.047. [DOI] [PubMed] [Google Scholar]
- 8. Bright CM, Price MA, Morgan RC, Bailey RK. The report of the W. Montague Cobb /NMA health institute consensus panel on the plight of underrepresented minorities in medical education. J Natl Med Assoc. 2018;110:614-623. doi: 10.1016/j.jnma.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 9. Holden L, Berger W, Zingarelli R, Siegel E. After-school program for urban youth: evaluation of a health careers course in New York City high schools. Inf Serv Use. 2015;35:141-160. doi: 10.3233/ISU-150773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Patel SI, RodrÖguez P, Gonzales RJ. The implementation of an innovative high school mentoring program designed to enhance diversity and provide a pathway for future careers in healthcare related fields. J Racial Ethn Health Disparities. 2015;2:395-402. doi: 10.1007/s40615-015-0086-y. [DOI] [PubMed] [Google Scholar]
- 11. Shrum KM. Developing a sustainable rural physician pipeline for Oklahoma. J Am Osteopath Assoc. 2017;117:287-288. doi: 10.7556/jaoa.2017.155. [DOI] [PubMed] [Google Scholar]
- 12. Wines KS. WVSOM anatomy lab tour program: an osteopathic medicine pipeline with student teaching opportunities. J Am Osteopath Assoc. 2019;119:456-463. doi: 10.7556/jaoa.2019.082. [DOI] [PubMed] [Google Scholar]
- 13. Xierali IM, Nivet MA. The racial and ethnic composition and distribution of primary care physicians. J Health Care Poor Underserved. 2018;29:556-570. doi: 10.1353/hpu.2018.0036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Marrast LM, Zallman L, Woolhandler S, Bor DH, McCormick D. Minority physicians’ role in the care of underserved patients: diversifying the physician workforce may be key in addressing health disparities. JAMA Intern Med. 2014;174:289-291. doi: 10.1001/jamainternmed.2013.12756. [DOI] [PubMed] [Google Scholar]
- 15. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84:191-215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- 16. Bandura A. Self-Efficacy: The Exercise of Control. New York, NY: WH Freeman/Times Books/Henry Holt & Co; 1997:ix, 604. [Google Scholar]
- 17. Bandura A. Perceived self-efficacy in cognitive development and functioning. Educ Psychol. 1993;28:117-148. doi: 10.1207/s15326985ep2802_3. [DOI] [Google Scholar]
- 18. Pajares F. Self-efficacy beliefs in academic settings. Rev Educ Res. 1996;66:543-578. doi: 10.2307/1170653. [DOI] [Google Scholar]
- 19. Schunk DH, Pajares F. The development of academic self-efficacy. In: Wigfield A, Eccles J, eds. Development of Achievement Motivation. Elsevier; 2002:15-31. doi: 10.1016/B978-012750053-9/50003-6. [DOI] [Google Scholar]
- 20. Gaumer Erickson AS, Soukup J, Noonan P, McGurn L. Self-efficacy Formative Questionnaire Technical Report. University of Kansas; 2018. http://www.researchcollaboration.org/uploads/Self-EfficacyQuestionnaireInfo.pdf. [Google Scholar]
- 21. U.S. Census Bureau. QuickFacts: Warrensville Heights, Ohio. https://www.census.gov/quickfacts/fact/table/warrensvilleheightscityohio/INC910218#INC910218. Published 2018. Accessed April 13, 2020.
- 22. Ohio Department of Education. Warrensville Heights District Review Report; 2017:1-80. https://education.ohio.gov/getattachment/Topics/School-Improvement/Academic-Distress-Commission/District-Reviews/Warrensville-Heights-City-School-District-Review-Report.pdf.aspx. Accessed March 6, 2020. [Google Scholar]
- 23. Gaumer Erickson AS, Noonan P. Self-Efficacy Formative Questionnaire. In: Gaumer Erickson AS, Noonan PM, eds. The Skills That Matter: Teaching Interpersonal and Intrapersonal Competencies in Any Classroom. Thousand Oaks, CA: Corwin Press; 2018:175-176. [Google Scholar]
- 24. Selected Presentations and Publications. University of Kansas Research Collaboration. http://researchcollaboration.org/page/presentations-and-publications. Published 2020. Accessed April 16, 2020.