Abstract
As HIV has fueled a global resurgence of tuberculosis over the last several decades, there is a growing awareness that HIV-mediated impairments in both innate and adaptive immunity contribute to the heightened risk of tuberculosis in people with HIV. Since early immune responses to Mycobacterium tuberculosis (Mtb) set the stage for subsequent control or progression to active tuberculosis disease, early host–pathogen interactions following Mtb infection can be thought of as establishing a mycobacterial “set point,” which we define as the mycobacterial burden at the point of adaptive immune activation. This early immune response is impaired in the context of HIV coinfection, allowing for a higher mycobacterial set point and greater likelihood of progression to active disease with greater bacterial burden. Alveolar macrophages, as the first cells to encounter Mtb in the lungs, play a critical role in containing Mtb growth and establishing the mycobacterial set point. However, a number of key macrophage functions, ranging from pathogen recognition and uptake to phagocytosis and microbial killing, are blunted in HIV coinfection. To date, research evaluating the effects of HIV on the alveolar macrophage response to Mtb has been relatively limited, particularly with regard to the critical early events that help to dictate the mycobacterial set point. A greater understanding of alveolar macrophage functions impacted by HIV coinfection will improve our understanding of protective immunity to Mtb and may reveal novel pathways amenable to intervention to improve both early immune control of Mtb and clinical outcomes for the millions of people worldwide infected with HIV.
Keywords: Tuberculosis, HIV, Macrophages, Coinfection, Innate immunity
Introduction
Although tuberculosis incidence declined worldwide over the course of the 20th century [1–4], these gains were quickly reversed with the onset of the HIV epidemic in the 1980s [5]. Tuberculosis is now the leading global killer among infectious diseases and the leading cause of death among people with HIV [6]. The profound T cell depletion induced by HIV has long been recognized as a significant driver of the tuberculosis epidemic in people with HIV [7, 8]. However, there is growing awareness that HIV-mediated impairments in innate immunity also contribute to the increased risk of tuberculosis in this vulnerable population. These HIV-mediated impairments in innate immunity are particularly relevant early in Mycobacterium tuberculosis (Mtb) infection, prior to the onset of adaptive immune responses [9] and, by impairing early control of Mtb, set the stage for accelerated progression to active tuberculosis disease.
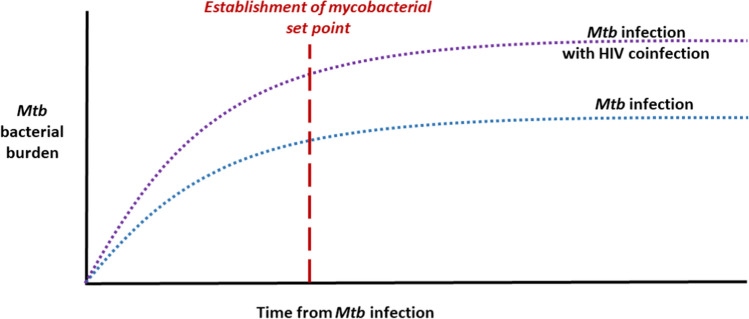
The pattern of early immune control setting the stage for longer term control—and clinically meaningful endpoints—parallels our understanding of the HIV set point. It was first recognized in the late 1990s that the HIV viral load soon after seroconversion, i.e., the HIV set point, is predictive of disease progression [10, 11]. Following infection, HIV replicates unchecked until an initial, albeit ineffective, host immune response develops and the set point is established [12–14]. When viewed through this same lens, early host–pathogen interactions following Mtb infection can be thought of as establishing a “mycobacterial set point” (Fig. 1). Unlike the set point in HIV, which occurs after an ineffective adaptive immune response, the mycobacterial set point is established before the onset of adaptive immunity.
Fig. 1.
Graphical depiction of the mycobacterial set point as a theoretical construct, represented as the Mycobacterium tuberculosis (Mtb) bacterial burden after infection, either alone or in the context of HIV coinfection. After infection, Mtb bacterial burden increases until adaptive immunity is activated, thereby establishing the mycobacterial set point. Alveolar macrophages, the first cells to encounter Mtb, are an important component of the early innate immune response to Mtb. As reviewed in the main text, the mycobacterial burden at the point of adaptive immune activation plays a important role in the subsequent control of infection and progression to active tuberculosis disease. In the case of HIV coinfection, impairments in alveolar macrophage functions lead to poor early immune control of Mtb which, in turn, leads to a higher mycobacterial set point and greater Mtb bacterial burden at the time when adaptive immunity is activated
Although we currently lack the tools to measure the mycobaterial set point clinically, this theoretical construct provides a framework for understanding early immune responses to Mtb, particularly those of the alveolar macrophage. While a multitude of cell types, including recruited interstitial macrophages, dendritic cells, and neutrophils, are infected prior to the onset of adaptive immunity [15], work by Cohen and others has confirmed the importance of the alveolar macrophage to the early Mtb response [16]. As we will emphasize in this review, a focus on this critical early period and the mycobacterial set point are useful in understanding the relative impacts, both on a cellular and clinical level, of various host and pathogen impairments that occur in the context of coinfection with Mtb and HIV. The concept of a mycobacterial set point also provides us with an overall index of immune health in the context of HIV/Mtb coinfection and thereby offers a useful gauge of efficacy when specific pathways are manipulated for therapeutic benefit. Host immunity to Mtb remains poorly understood, but a focus on the role of alveolar macrophages in establishing a mycobacterial set point and on alterations in macrophage control in the context of HIV coinfection has the potential to yield great insight into some of the earliest immune events in Mtb infection.
Although Mtb- and HIV-mediated impairments in pulmonary innate immunity and alveolar macrophage function have been reviewed elsewhere [17, 18], the impact of these impairments in the context of coinfection has not been well described. In this review, we will explore how HIV coinfection makes alveolar macrophages, the first cells to encounter Mtb, more permissive of early mycobacterial growth and is therefore likely to increase the mycobacterial burden at the point at which adapative immunity is activated and the mycobacterial set point is established [16]. By curtailing early immune control and delaying the onset of adaptive immunity, HIV coinfection leads to a higher mycobacterial set point and, consequently, a greater bacterial burden (Fig. 1).
In order to demonstrate the utility of the mycobacterial set point framework, we will first review epidemiologic data supporting the importance of innate immunity in people with tuberculosis and HIV coinfection. We will then discuss some of the model systems that are used to study macrophage responses to Mtb and HIV and animal model findings in support of a mycobacterial set point. We will then highlight existing data on alveolar macrophage functions—from macrophage phenotype, key cytokines, and oxidative stress, to pathogen recognition and phagocytosis, cell death pathways, and activation of adaptive immunity—that are impacted by either Mtb infection, HIV infection, or coinfection. The examples we provide, which come from a range of cell types and organ systems, including primary alveolar macrophages, monocyte-derived macrophages, and cell lines, are not meant to be exhaustive or comprehensive. Rather, our goal is to provoke further inquiry and investigation into this critical area by offering a framework by which to contextualize studies in the field. We will close the review by highlighting several promising avenues for studying the mycobacterial set point in humans, in order to underscore the potential benefit of this concept as a framework for clinically relevant research.
Epidemiologic data for the role of innate immunity in HIV and tuberculosis
From the earliest days of the HIV epidemic it has been clear that tuberculosis outcomes were markedly worse in people with HIV. In a series of nosocomial tuberculosis outbreaks among people with HIV in the early 1990s, the overwhelming majority of patients died, often within a month or two of their diagnosis [19–21]. These individuals had very advanced HIV, which undoubtedly contributed to their high mortality rates [21]. However, their rapid progression from exposure to active disease, in a time frame prior to the expected onset of adaptive immunity, suggests that impaired innate immunity was likely a contributing factor. Similarly, in a study of South African gold miners newly infected with HIV, the risk of tuberculosis disease was found to increase very early in the course of HIV infection, when CD4 counts would still be in a normal range [22]. Another study from South Africa found that people with HIV on antiretroviral therapy (ART) with normal CD4 counts had four times the risk of tuberculosis than people without HIV [23]. Likewise, in Italy, a setting with a low burden of both HIV and tuberculosis, nearly a third of patients diagnosed with HIV-associated tuberculosis in one study had been receiving ART for a median of 27 months, at which point CD4 counts would typically have reached a normal range [24]. Taken together, these data offer epidemiologic evidence that defects in both innate and adaptive immunity are likely to contribute to the greater risk of tuberculosis in people with HIV. While these clinical observations cannot establish mechanism or causality, they do provide a rationale for pursuing further basic science and translational studies to better understand the role of innate immunity in controlling Mtb infection.
Model systems for studying alveolar macrophage responses to Mtb and HIV
Over the last century, scientists from successive eras have made remarkable discoveries by bringing the newest available techniques to bear on their investigations of Mtb, with various model systems employed over time. While each system has distinct advantages and disadvantages in addressing particular questions, the sheer volume of data derived from the many available systems can make it hard to develop a coherent narrative regarding Mtb infection in humans. Although a full review of these features of the tuberculosis literature is beyond the scope of this review, we will offer a brief overview of the main characteristics of some of the major models to provide context for the reader [25, 26].
Despite their inability to model sophisticated cellular interactions, in vitro systems have long been used as tools for studying Mtb [27]. A variety of myeloid cell lines have been employed, and are often helpful in quantifying cytokine and other signaling responses to Mtb. In addition, due to the ease with which in vitro systems can be manipulated, studies with primary macrophages from animal models have enabled investigators to dissect the roles of individual proteins and pathways in the Mtb response [28, 29]. Finally, human primary cells have been used in a variety of ways, including induced pluripotent stem cells, human macrophages, granuloma models, and many more. Each system has proven useful in addressing different aspects of the Mtb response, but all are hampered by their inability to coordinate the full spectrum of in vivo responses. An additional challenge is the conflation of different types of macrophages, whether from cell-lines, animal models, or humans, as a homogenous population. Rather, there is a growing appreciation of the distinctions between tissue-derived and bone-marrow derived macrophages, from their ontogeny to functional capacity and self-maintenance [30–32]. These distinctions are highly relevant to this review, as bone-marrow derived macrophages do not become polarized in the same manner as alveolar macrophages following Mtb exposure, and thus cannot be expected to behave the same [33]. However, given challenges in obtaining primary alveolar macrophages, particularly from humans [34], many studies are conducted with derived cells.
With regards to animal systems, ease of use in handling the zebrafish-Mycobacterium marinum model has made it a powerful tool for the study of Mtb [35]. Several key components of the human response to Mtb are present in zebrafish, including the leukotriene A4 hydrolase locus, and it has been used to study everything from treatment strategies for drug-resistant Mtb to vaccine development. The mouse model has the virtue of capturing vertebrate, mammalian immune responses in a reproducible, easily scalable system. However, different mouse strains have different levels of susceptibility to Mtb and mice do not typically form granulomas or cavities [36]. As a result, the mouse model tends to be suited for studies of cell-mediated immunity and drug development, but less useful for studies of human clinical outcomes [37]. Guinea pigs provide another small animal model, with the benefit of recapitulating lung necrosis and other human features, but challenges in measuring their immune responses has historically limited their widespread use [25]. Rabbits have also provided an effective model system for Mtb research, largely due to the fact that the structural similarities between their lungs and human lungs leads to similar pathology in response to Mtb. That said, their larger size and the greater resources required to utilize them has limited their broad applicability [36, 38]. Finally, non-human primates, particularly rhesus and cynomolgus macaques, have marked genetic and immunologic similarities to humans and, as such, have yielded significant advances in our understanding of host–pathogen interactions and the potential for vaccine-induced protection in recent years [39, 40]. However, given the vast resources needed to sustain these animals, there are a limited number of research centers capable of conducting non-human primate studies.
Evidence to date for a “mycobacterial set point”
While in-depth analysis of early immunologic events in human Mtb infection remains challenging for the reasons discussed above, Poulsen and others established over 50 years ago that tuberculin skin test (TST) conversion in humans, an indicator of the onset of the adaptive immune response, generally occurred by 6 weeks after exposure [41–43]. Poulsen also determined that this period prior to TST conversion is not a time of immunologic quiescence; rather, many individuals had evidence of a robust inflammatory response with fever and elevated inflammatory markers.
Since those landmark studies, much of our understanding of these early events has relied on data from animal models. Experiments in rabbits and guinea pigs by Lurie, Smith, and Harding, established that macrophages provide a niche within which Mtb multiplies logarithmically during early infection [44, 45]. Others have demonstrated that the onset of adaptive immunity in response to Mtb is indeed delayed, arising in part from delayed activation of CD4+ T cells within local lymph nodes [46, 47]. This delay of several weeks, as compared to several days with organisms such as Salmonella typhi and Listeria monocytogenes, translates into relatively unchecked bacterial growth during the early phase of infection [48, 49]. After this period of logarithmic growth, which has been demonstrated in rabbits, mice, and guinea pigs, the bacteria enter a relatively stationary phase [50]. During this critical time, Mtb subverts alveolar macrophage defenses, thereby ensuring prolonged intracellular survival and mycobacterial growth within this pulmonary niche. Whether this failure of immunity represents an intrinsic deficiency of macrophages or an insufficient activation of macrophages by T cells remains uncertain [51].
As discussed above, there has been a proliferation of work with non-human primate models in recent years that shed further light on the establishment of the set point, particularly with regards to granuloma formation [52]. Studies of macaques with aerosol exposure to Mtb have found that early mycobacterial dissemination, as reflected by the development of new granulomas in the first 3–6 weeks following infection (i.e., the period during which the set point is established), is associated with subsequent progression to active disease [53, 54]. Conversely, the absence of new granuloma formation, which could be construed as a “low” set point, is associated with immune control and long-term maintenance of latent infection. Granuloma size can also stratify the risk of dissemination, with larger granulomas associated with a greater potential for future mycobacterial spread [55]. By linking early immunologic events to clinically meaningful outcomes, these findings underscore the critical importance of early immune control prior to the onset of adaptive immunity. They also provide evidence to support the longstanding belief that progression to tuberculosis disease is determined at the level of the individual granuloma.
Alveolar macrophage phenotypes in Mtb infection
As the first cell type to encounter Mtb, the alveolar macrophage is a key player in the early stages of infection and Mtb is known to both cause and benefit from certain alterations in macrophage functionality [56]. Several excellent reviews have recently examined the heterogeneity and plasticity of macrophages, in addition to proposing a uniform approach to macrophage nomenclature [31, 32]. Alveolar macrophages play myriad roles in the lungs, from housekeeper to innate immune effector, and their role depends heavily on the microenvironment within the alveolar space. For example, in response to inflammatory stimuli such as lipopolysaccharide (LPS), alveolar macrophages develop an inflammatory phenotype with increased production of cytokines such as TNF-α and IL-6. Conversely, in the setting of IL-4 exposure, alveolar macrophages shift to an immunosuppressive phenotype and increase production of regulatory cytokines such as TGF-β [31]. Although debate continues as to how best to characterize macrophages and how dynamically tissue resident subtypes respond to their local cytokine milieu, it is well known that macrophages respond to different cytokine programs with a variety of functional changes. Most experts agree that these changes exist on a spectrum between the classically activated (or M1, or inflammatory) macrophage and an alternatively activated (or M2, or regulatory) macrophage.
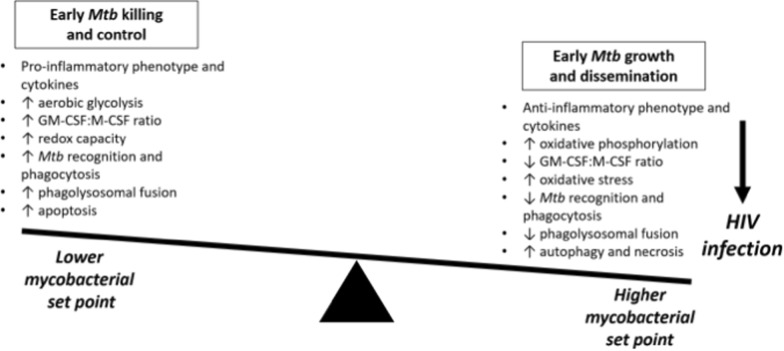
In the context of Mtb infection, the “macrophage polarization ratio,” an indicator of the balance between pro-inflammatory and anti-inflammatory genes, has been employed to explore how macrophage functionality and subsequent granuloma formation affects the probabilities of Mtb control and dissemination (Fig. 2) [57]. With this approach, NF-kB signaling was found to be an essential component of the classical activation profile, which, when triggered early, leads to improved clinical tuberculosis outcomes in a nonhuman primate model [57].
Fig. 2.
The balance of alveolar macrophage polarization and activity. Early Mtb killing and control leads to a lower mycobacterial set point, whereas early Mtb growth and dissemination lead to a higher mycobacterial set point. HIV infection favors early Mtb growth and dissemination and a higher mycobacterial set point
Alveolar macrophages are also severely impacted by the presence of HIV infection and have been shown to be a reservoir for the virus within the lungs [58]. Importantly, coinfection shifts macrophage polarization in a fashion favorable for pathogen survival [59]. Both HIV and Mtb stimulate a cytokine milieu in the alveolar space that pushes macrophages into an inflammatory phenotype optimized for the uptake of foreign microbes. Although these inflammatory cells would ordinarily excel at pathogen killing, the intracellular effects of HIV and Mtb render the macrophages less effective and, as a result, permit ongoing pathogen growth [60]. At the same time, there is ample evidence that Mtb infection of alveolar macrophages creates a permissive environment for HIV infection and replication, through a variety of mechanisms including increased surface expression of the HIV receptors CCR5 and CXCR4, increased HIV transcription and replication, and induction of nanotubes that promote cell-to-cell HIV viral spread between macrophages [61–64]. Taken together, this synergy between Mtb- and HIV-mediated impacts on macrophages enables intracellular growth and survival of both pathogens and, more broadly, fuels the global syndemic of coinfection.
Macrophage function and polarization is also influenced by immunometabolism, the balance of cellular energy utilization. This represents another growing area of inquiry in which Mtb and HIV are likely to have complementary, yet deleterious, effects. Mtb infection of alveolar macrophages has been shown to shift cellular metabolism from oxidative phosphorylation to aerobic glycolysis, a shift associated with a more inflammatory, M1-like phenotype [65]. This shift triggers an increase in cellular IL-1β production along with a decrease in IL-10 production, which, in concert, should increase bacillary killing in vitro. Yet, other investigations suggest that persistence of fatty acid oxidation in alveolar macrophages may permit ongoing intracellular Mtb growth [66]. At the same time, HIV infection also alters cellular energy balance, oxidative stress levels, and mitochondrial bioenergetics, including for infected macrophages [67–70]. Further study of the combined, net effects of Mtb and HIV on alveolar macrophage immunometabolism is needed to expand our understanding of how coinfection impairs early mycobacterial control.
Cytokine expression and innate immunity in Mtb and HIV
Macrophage cytokine expression profiles may also vary according to the stage of Mtb infection, whereby the secreted protein ESAT-6 initially skews macrophages towards a M1 phenotype, potentially to facilitate the establishment of a granuloma, and then later to a more permissive M2 phenotype [71]. IFN-γ, a paradigmatic pro-inflammatory cytokine, drives macrophages towards an inflammatory phenotype and, under normal circumstances, is critical for Mtb control. However, peripheral blood mononuclear cells isolated from people with HIV have depressed IFN-γ production in response to purified protein derivative (PPD) [72, 73]. IL-4, another key cytokine for macrophage polarization, is induced by HIV glycoprotein (gp) 120 [74]. This induction shifts macrophages to an anti-inflammatory phenotype, potentially further reducing early Mtb control. In people without HIV, elevated IL-4 levels have been associated with progression to tuberculosis disease and the development of pulmonary cavities, thus underscoring the clinical impact of these shifts [75–77]. Interestingly, the relative balance of these cytokines may vary according to the stage of HIV infection, which could translate into differential susceptibility to and control of Mtb infection [60].
Several key cytokines important for both macrophage polarization and the response to Mtb are also altered in the presence of HIV coinfection. For example, GM-CSF plays an essential role in cellular control of Mtb [78, 79] and its activity is impaired in monocyte-derived macrophages infected with HIV [80]. The GM-CSF:M-CSF balance is also altered by the presence of Mtb [81] and M-CSF-driven macrophages are more permissive to Mtb replication and dissemination [82]. Similarly, interleukin-1 receptor-associated kinase M (IRAK-M), which is downstream of the GM-CSF-dependent transcription factor PU.1, correlates directly with mycobacterial load in human lung tissue and impacts Mtb survival [83]. Thus, the combined impact of Mtb and HIV on the balance of cytokines within the lungs leads to an environment that permits the growth of both pathogens.
Alveolar macrophage oxidative stress in Mtb and HIV
Another avenue ripe for further exploration is the effects of HIV and Mtb on redox systems, which can also modulate macrophage function [84–86]. HIV is known to impair antioxidant defenses in the alveolar macrophage and raise levels of oxidative stress in the lung more generally [18, 87]. The effects in the lung are likely due, at least in part, to glutathione depletion in the airways of people with HIV [88, 89]. Mtb, on the other hand, has successfully adapted to hostile intracellular conditions, including high oxidative stress [90, 91]. Mtb may also directly contribute to oxidative stress by inducing heme oxygenase (HO)-1, the levels of which directly correlate with treatment outcomes in people with active tuberculosis disease [92]. Several studies have demonstrated improved Mtb control with glutathione supplementation, including one study using macrophages isolated from people with HIV in which supplementation led to enhanced inflammatory cytokine production and restored macrophage capacity to control Mtb growth [89, 93–97]. Of note, the oxidative stress induced by Mtb-infected macrophages is also likely to promote HIV reactivation, further complicating the relationship between these two pathogens [98].
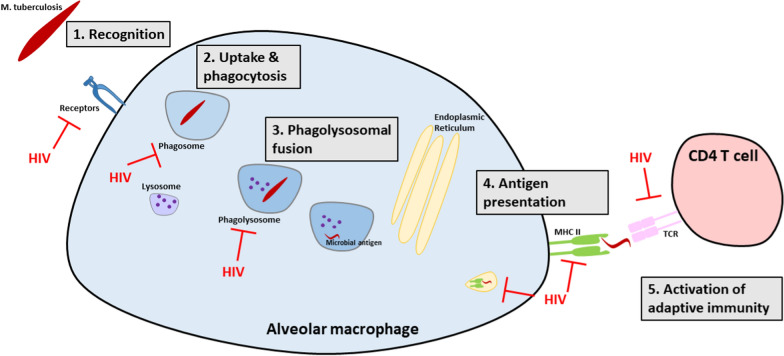
Mtb recognition and phagocytosis by alveolar macrophages in HIV
An important function of macrophages in the alveolar space is the differentiation of friend versus foe via pathogen recognition and phagocytosis (Fig. 3) [99–101]. Particularly germane to the recognition of Mtb is the mannose receptor, which is downregulated in people living with HIV [102]. HIV also leads to reduced expression and activity of toll-like receptors (TLR), another key receptor for macrophage pathogen recognition [103–105]. When combined with shifts in TLR-mediated regulation of nitric oxide production induced by Mtb [104], these impairments have the potential to reduce Mtb uptake by alveolar macrophages and facilitate prolonged extracellular growth.
Fig. 3.
Events in alveolar macrophage uptake and response to Mtb infection that are impacted by HIV coinfection. (1) Recognition: HIV coinfection downregulates alveolar macrophage expression of Mtb recognition receptors including mannose and toll-like receptors. (2) Uptake and phagocytosis: HIV coinfection impairs phagocytosis. (3) Phagolysosomal fusion: HIV coinfection disrupts endosomal trafficking and impairs phagolysosomal maturation. (4) Antigen presentation: HIV coinfection leads to the expression of immature MHC class II complexes and thereby impairs the activation of adaptive immune responses. (5) Activation of adaptive immunity: HIV coinfection reduces the expression of costimulatory molecules for activation of adaptive immunity. The net effect of these HIV-mediated impairments is to enable increased intracellular and extracellular Mtb growth which ultimately leads to a higher mycobacterial set point
Once a pathogen like Mtb has been recognized, it then undergoes phagocytosis [99, 100]. HIV creates favorable conditions for bacteria by impairing phagocytosis of pathogens including Streptococcus [106]. The HIV protein Nef has also been shown to interfere with phagosome formation by impeding endosomal recruitment and remodeling [107]. Of note, impaired phagocytosis has been observed even in alveolar macrophages not directly infected by HIV [58, 108]. While phagocytosis of Mtb in the setting of HIV has not specifically been studied, such impairments would enable further extracellular growth [18, 109].
HIV has also been found in macrophage endosomes and is known to impair phagolysosomal fusion in the macrophage [110, 111]. At least some of these impairments may be mediated through the effects of the HIV-related protein transactivator of transcription (Tat) [112]. Another HIV protein, Vpr, has also been shown to perturb phagolysosomal maturation by altering microtubule-dependent trafficking within macrophages [113]. In addition, HIV has been shown to co-opt the Rag GTPases, resulting in further disruption of endosomal trafficking [114]. This disruption may facilitate HIV replication and simultaneously assist Mtb evasion of lysosomal fusion and killing. IL-10 has also been shown to dysregulate the response to Mtb in the setting of HIV, at least in part by impairing phagosome maturation [115, 116]. However, in one study of alveolar macrophages from humans with active tuberculosis disease, phagolysosomal acidification was equally disrupted among those with and without HIV, highlighting existing uncertainties about the impacts of Mtb and HIV on alveolar macrophage phagocytosis [117]. Thus, although further research is needed to define the relevant mechanisms by which HIV impairs the phagocytic response to Mtb, the bulk of the existing data suggest that endosomes fail to fuse with acidified lysosomes, thereby promoting Mtb survival [118].
Cell death pathways in Mtb-HIV infected macrophages
Alveolar macrophage cell death pathways range from apoptosis to autophagy and necrosis. Mtb is known to shift the balance toward necrosis by actively inhibiting apoptosis, thereby allowing the extracellular release of viable mycobacteria from dying alveolar macrophages [119, 120]. Similarly, HIV, via the viral proteins Tat and glycoprotein-120 (gp-120), stimulates the triggering receptor expressed on myeloid cells-1 (TREM-1), thereby inhibiting apoptosis in a p65-dependent manner [121]. HIV may also directly induce autophagy through the Nef protein, in order to modulate viral replication and survival, albeit in a manner that may be synergistic with Mtb-mediated inhibition of apoptosis [122, 123]. Gp-120 also impairs apoptosis-associated killing of pneumococcus within alveolar macrophages, indicating that this impairment may not be specific to Mtb [124]. Impaired apoptosis of Mtb has been tied by other investigators to IL-10, which is increased in the bronchoalveolar lavage fluid of people with HIV [125]. Additional research is needed to further delineate the impact of these shifts in cell death pathways and to identify whether there are therapeutic opportunities to improve Mtb control in patients with and without HIV. One promising recent report found that all-trans retinoic acid was able to promote autophagy of human alveolar macrophages in the setting of Mtb infection [126].
Activation of adaptive immunity in Mtb-HIV coinfection
The final step required for establishment of the mycobacterial set point is activation of the adaptive arm of the immune system (Fig. 3). Mtb has been shown to delay the activation of adaptive immunity in mice by slowing bacterial transport to local lymph nodes [46]. This delay allows for a prolonged period of unchecked bacterial growth within the lungs, with a 10,000–100,000-fold expansion of the Mtb pulmonary population during this time. At least one driver of this delay is Mtb-mediated inhibition of MHC class II antigen presentation by dendritic cells [127]. Mtb also manipulates antigen presentation by diverting bacterial proteins through a vesicular export pathway, away from MHC class II presentation. In the context of HIV, the viral protein Nef has been shown to promote the expression of immature, functionally incompetent MHC class II complexes [128, 129]. Recent data have more directly linked these two by demonstrating that HIV-infected dendritic cells have reduced ability to upregulate key costimulatory molecules critical for antigen presentation (e.g., CD40, CD80, and CD86) in the presence of Mtb infection [130]. All of this would combine to delay the onset of adapative immunity and further increase the mycobacterial set point.
Net effects: the combined immunologic consequences of coinfection with Mtb and HIV
As should be clear from the preceding sections, studies detailing the effects of Mtb and HIV on the immune responses within the alveolar space have found an abundance of affected cytokines, pathways, and response elements. Although much of the available data suggests ways in which Mtb and HIV each make it more likely for the other to gain ground within an individual’s lungs, the myriad as-yet-unstudied pathways leave open the distinct possibility that some of their particular effects may cumulatively cancel out those of the other pathogen. It is in this key domain that we believe the concept of a mycobacterial set point most clearly demonstrates its worth. Because the set point relates to the mycobacterial burden at the moment in which the adaptive immune system activates, it offers a clinically relevant marker that synthesizes the various effects of coinfections, comorbidities, and therapeutics. As a research tool, then, it will help us understand whether the net effect of a given intervention actually reduces the overall mycobacterial burden, as opposed to fruitfully manipulating a single pathway (with the knowledge that doing so may have deleterious effects on others).
Measuring the mycobacterial set point in human infection and disease
Fortunately, several novel approaches provide hope for expanding our understanding of these early immunologic events in humans. These tools have the potential to vastly enhance our current knowledge by quantifying the functional impact of coinfection on bacterial burden and early human immune responses, while also offering insight into mechanisms underlying early immune control or escape.
The first such tool is 2-deoxy-2-[18F]fluoro-d-glucose ([18F]FDG) positron emission tomography combined with computed tomography (PET–CT), which identifies areas of increased cellular metabolic activity as would occur with an immune response to infection. Several macaque studies have leveraged PET-CT imaging to gain insight into early infection by following the progression of individual granulomas after aerosol infection [53, 54, 131, 132]. PET-CT has also been employed to study tuberculosis in humans, including a cohort of 35 people with HIV and latent tuberculosis infection, 10 of whom had PET-avid lesions suspicious for subclinical disease [133]. Those with PET activity were significantly more likely to develop active tuberculosis disease during the following 6 months, suggesting metabolic activity on PET imaging may be able to identify patients with ineffective early immune responses to Mtb infection.
Blood-based immunologic signatures represent another potential avenue for studying early infection. Recent studies in macaques and humans have identified RNA signatures predictive of progression to active tuberculosis disease [134–136]. Notably, the macaque signature was predictive just 3–6 weeks after aerosol infection, providing compelling evidence for the value of these signatures even very early in infection. This signature also identified a novel gene in tuberculosis pathogenesis, PRDX2, a member of the reactive oxygen species scavenger system. Further studies are warranted to explore the role of PRDX2 in early infection, and how that response may be skewed by HIV and other known tuberculosis risk factors. Similarly, characterization of Mtb-specific T cell responses may provide another means for understanding adaptive immune responses important in early infection. In a recent report of a whole blood assay of T cell responses to 60 Mtb antigens, immunogenic Mtb antigens were successfully identified across a diverse range of populations and infectious states [137]. Longitudinal studies are underway to determine if these T cell signatures correlate with early immune responses—both those that clear infection and those that permit ongoing Mtb growth and dissemination.
Yet another tool for identifying and studying early infection is plasma metabolomics, in which small molecules are identified using high-resolution mass spectrometry. This approach has been successfully employed to identify direct metabolites of Mtb, and may be able to identify low levels even early in infection. Metabolomics has also been used to identify distinct signatures of the host immune response, whereby investigators were able to distinguish between risk-associated metabolites associated with a higher likelihood of progression to tuberculosis disease and disease-associated metabolites that increased in a time-dependent manner among those with progression to active tuberculosis disease [138–140]. Looking ahead, it will be important to determine whether these metabolic signatures are similarly predictive and valid in people with HIV.
Conclusion
Across the scientific community, there is overwhelming consensus over the need to understand protective immunity to Mtb [55]. As a framework for considering early immunologic responses to Mtb, the mycobacterial set point provides a useful construct for understanding the impact of early immune control and clinical outcomes of tuberculosis. Given the disproportionate burden of tuberculosis disease and deaths among people with HIV despite widespread ART [23], it is imperative to study the unique impacts of HIV on Mtb infection and susceptibility. To date, research evaluating the effects of HIV on the alveolar macrophage response to Mtb has been relatively limited, particularly with regard to the critical early events that help to dictate the mycobacterial set point. While we believe that a higher mycobacterial set point is a key contributor to the increased morbidity among people with HIV, additional research is needed to better understand the mechanisms and biological pathways that may be involved in facilitating mycobacterial immune evasion. A greater understanding of the impact of HIV on these earliest responses to Mtb may lead to the development of novel interventions and host-directed therapies to reduce the persistent global burden of tuberculosis in this vulnerable population.
Acknowledgements
We would like to thank our colleague Cheryl L. Day, PhD, for review, thoughtful discussion, and feedback on this manuscript.
Authors’ contributions
SCA and BSS conceived of the review, drafted and revised the manuscript. Both authors read and approved the final manuscript.
Funding
This work was supported by the following grants: NIH/NIAID K23 AI134182 (Auld), NIH/NIAAA K08 AA024512 (Staitieh), the Emory Center for AIDS Research (P30AI050409).
Availability of data and materials
Not applicable.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Murray JF, Schraufnagel DE, Hopewell PC. Treatment of tuberculosis. A historical perspective. Ann Am Thoracic Soc. 2015;12(12):1749–1759. doi: 10.1513/AnnalsATS.201509-632PS. [DOI] [PubMed] [Google Scholar]
- 2.Bayer R, Wilkinson D. Directly observed therapy for tuberculosis: history of an idea. Lancet. 1995;345(8964):1545–1548. doi: 10.1016/s0140-6736(95)91090-5. [DOI] [PubMed] [Google Scholar]
- 3.Enarson DA. Principles of IUATLD collaborative tuberculosis progammes. Bull Int Union Against Tuberc Lung Dis. 1991;66(4):195–200. [PubMed] [Google Scholar]
- 4.Iseman MD. Tuberculosis therapy: past, present and future. Eur Respir J. 2002;20(36 suppl):87S–94s. doi: 10.1183/09031936.02.00309102. [DOI] [PubMed] [Google Scholar]
- 5.Centers for Disease Control Pneumocystis pneumonia–Los Angeles. MMWR Morb Mortal Wkly Rep. 1981;30(21):250–252. [PubMed] [Google Scholar]
- 6.Global Tuberculosis Report. In.: WHO; 2017.
- 7.Kwan CK, Ernst JD. HIV and tuberculosis: a deadly human syndemic. Clin Microbiol Rev. 2011;24(2):351–376. doi: 10.1128/CMR.00042-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pai M, Behr MA, Dowdy D, Dheda K, Divangahi M, Boehme CC, Ginsberg A, Swaminathan S, Spigelman M, Getahun H, et al. Tuberculosis. Nat Rev Dis Primers. 2016;2:16076. doi: 10.1038/nrdp.2016.76. [DOI] [PubMed] [Google Scholar]
- 9.Cadena AM, Flynn JL, Fortune SM. The importance of first impressions: early events in Mycobacterium tuberculosis infection influence outcome. mBio. 2016;7(2):e00342-00316. doi: 10.1128/mBio.00342-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lefrere JJ, Roudot-Thoraval F, Mariotti M, Thauvin M, Lerable J, Salpetrier J, Morand-Joubert L. The risk of disease progression is determined during the first year of human immunodeficiency virus type 1 infection. J Infect Dis. 1998;177(6):1541–1548. doi: 10.1086/515308. [DOI] [PubMed] [Google Scholar]
- 11.Sterling TR, Vlahov D, Astemborski J, Hoover DR, Margolick JB, Quinn TC. Initial plasma HIV-1 RNA levels and progression to AIDS in women and men. N Engl J Med. 2001;344(10):720–725. doi: 10.1056/NEJM200103083441003. [DOI] [PubMed] [Google Scholar]
- 12.Fellay J, Shianna KV, Ge D, Colombo S, Ledergerber B, Weale M, Zhang K, Gumbs C, Castagna A, Cossarizza A, et al. A whole-genome association study of major determinants for host control of HIV-1. Science. 2007;317(5840):944–947. doi: 10.1126/science.1143767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mackelprang RD, Carrington M, Thomas KK, Hughes JP, Baeten JM, Wald A, Farquhar C, Fife K, Campbell MS, Kapiga S, et al. Host genetic and viral determinants of HIV-1 RNA set point among HIV-1 seroconverters from Sub-Saharan Africa. J Virol. 2015;89(4):2104–2111. doi: 10.1128/JVI.01573-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bartha I, McLaren PJ, Brumme C, Harrigan R, Telenti A, Fellay J. Estimating the respective contributions of human and viral genetic variation to HIV control. PLoS Comput Biol. 2017;13(2):e1005339. doi: 10.1371/journal.pcbi.1005339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srivastava S, Ernst JD, Desvignes L. Beyond macrophages: the diversity of mononuclear cells in tuberculosis. Immunol Rev. 2014;262(1):179–192. doi: 10.1111/imr.12217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen SB, Gern BH, Delahaye JL, Adams KN, Plumlee CR, Winkler JK, Sherman DR, Gerner MY, Urdahl KB. Alveolar macrophages provide an early Mycobacterium tuberculosis niche and initiate dissemination. Cell Host Microbe. 2018;24(3):439–446.e434. doi: 10.1016/j.chom.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ernst JD. Mechanisms of M. tuberculosis immune evasion as challenges to TB vaccine design. Cell Host Microbe. 2018;24(1):34–42. doi: 10.1016/j.chom.2018.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Staitieh BS, Egea EE, Guidot DM. Pulmonary innate immune dysfunction in human immunodeficiency virus. Am J Respir Cell Mol Biol. 2017;56(5):563–567. doi: 10.1165/rcmb.2016-0213TR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Disease Control and Prevention Multidrug-resistant tuberculosis outbreak on an HIV ward–Madrid, Spain, 1991–1995. MMWR Morb Mortal Wkly Rep. 1996;45(16):330–333. [PubMed] [Google Scholar]
- 20.Centers for Disease Control and Prevention Nosocomial transmission of multidrug-resistant tuberculosis among HIV-infected persons–Florida and New York, 1988–1991. MMWR Morb Mortal Wkly Rep. 1991;40(34):585–591. [PubMed] [Google Scholar]
- 21.Moro ML, Gori A, Errante I, Infuso A, Franzetti F, Sodano L, Iemoli E. An outbreak of multidrug-resistant tuberculosis involving HIV-infected patients of two hospitals in Milan, Italy. Italian Multidrug-Resistant Tuberculosis Outbreak Study Group. Aids. 1998;12(9):1095–1102. [PubMed] [Google Scholar]
- 22.Sonnenberg P, Glynn JR, Fielding K, Murray J, Godfrey-Faussett P, Shearer S. How soon after infection with HIV does the risk of tuberculosis start to increase? A retrospective cohort study in South African gold miners. J Infect Dis. 2005;191(2):150–158. doi: 10.1086/426827. [DOI] [PubMed] [Google Scholar]
- 23.Gupta A, Wood R, Kaplan R, Bekker LG, Lawn SD. Tuberculosis incidence rates during 8 years of follow-up of an antiretroviral treatment cohort in South Africa: comparison with rates in the community. PLoS ONE. 2012;7(3):e34156. doi: 10.1371/journal.pone.0034156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Girardi E, Antonucci G, Vanacore P, Palmieri F, Matteelli A, Iemoli E, Carradori S, Salassa B, Pasticci MB, Raviglione MC, et al. Tuberculosis in HIV-infected persons in the context of wide availability of highly active antiretroviral therapy. Eur Respir J. 2004;24(1):11–17. doi: 10.1183/09031936.04.00109303. [DOI] [PubMed] [Google Scholar]
- 25.Williams A, Orme IM. Animal models of tuberculosis: an overview. Microbiol Spectrum. 2016;4(4):131–142. doi: 10.1128/microbiolspec.TBTB2-0004-2015. [DOI] [PubMed] [Google Scholar]
- 26.Helke KL, Mankowski JL, Manabe YC. Animal models of cavitation in pulmonary tuberculosis. Tuberculosis. 2006;86(5):337–348. doi: 10.1016/j.tube.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 27.Keiser TL, Purdy GE. Killing Mycobacterium tuberculosis in vitro: what model systems can teach us. Microbiol Spectrum. 2017;5(3):541–556. doi: 10.1128/microbiolspec.TBTB2-0028-2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bogdan C. Nitric oxide synthase in innate and adaptive immunity: an update. Trends Immunol. 2015;36(3):161–178. doi: 10.1016/j.it.2015.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Zinman G, Brower-Sinning R, Emeche CH, Ernst J, Huang GT, Mahony S, Myers AJ, O’Dee DM, Flynn JL, Nau GJ, et al. Large scale comparison of innate responses to viral and bacterial pathogens in mouse and macaque. PLoS ONE. 2011;6(7):e22401. doi: 10.1371/journal.pone.0022401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ginhoux F, Guilliams M. Tissue-resident macrophage ontogeny and homeostasis. Immunity. 2016;44(3):439–449. doi: 10.1016/j.immuni.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 31.Murray PJ, Allen JE, Biswas SK, Fisher EA, Gilroy DW, Goerdt S, Gordon S, Hamilton JA, Ivashkiv LB, Lawrence T, et al. Macrophage activation and polarization: nomenclature and experimental guidelines. Immunity. 2014;41(1):14–20. doi: 10.1016/j.immuni.2014.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gordon S, Plüddemann A, Martinez Estrada F. Macrophage heterogeneity in tissues: phenotypic diversity and functions. Immunol Rev. 2014;262(1):36–55. doi: 10.1111/imr.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Redente EF, Higgins DM, Dwyer-Nield LD, Orme IM, Gonzalez-Juarrero M, Malkinson AM. Differential polarization of alveolar macrophages and bone marrow-derived monocytes following chemically and pathogen-induced chronic lung inflammation. J Leukoc Biol. 2010;88(1):159–168. doi: 10.1189/jlb.0609378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Schwander S, Dheda K. Human lung immunity against Mycobacterium tuberculosis: insights into pathogenesis and protection. Am J Respir Crit Care Med. 2011;183(6):696–707. doi: 10.1164/rccm.201006-0963PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bouz G, Al Hasawi N. The zebrafish model of tuberculosis—no lungs needed. Crit Rev Microbiol. 2018;44(6):779–792. doi: 10.1080/1040841X.2018.1523132. [DOI] [PubMed] [Google Scholar]
- 36.Cooper AM. Mouse model of tuberculosis. Cold Spring Harbor Perspect Med. 2014;5(2):a018556. doi: 10.1101/cshperspect.a018556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Singh AK, Gupta UD. Animal models of tuberculosis: lesson learnt. Indian J Med Res. 2018;147(5):456–463. doi: 10.4103/ijmr.IJMR_554_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Datta M, Via LE, Kamoun WS, Liu C, Chen W, Seano G, Weiner DM, Schimel D, England K, Martin JD, et al. Anti-vascular endothelial growth factor treatment normalizes tuberculosis granuloma vasculature and improves small molecule delivery. Proc Natl Acad Sci USA. 2015;112(6):1827–1832. doi: 10.1073/pnas.1424563112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Darrah PA, Zeppa JJ, Maiello P, Hackney JA, Wadsworth MH, 2nd, Hughes TK, Pokkali S, Swanson PA, 2nd, Grant NL, Rodgers MA, et al. Prevention of tuberculosis in macaques after intravenous BCG immunization. Nature. 2020;577(7788):95–102. doi: 10.1038/s41586-019-1817-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Peña JC, Ho W-Z. Monkey models of tuberculosis: lessons learned. Infect Immun. 2015;83(3):852–862. doi: 10.1128/IAI.02850-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Poulsen A. Some clinical features of tuberculosis. 1. Incubation period. Acta tuberculosea Scandinavica. 1950;24(3–4):311–346. [PubMed] [Google Scholar]
- 42.Gedde-Dahl T. Tuberculous infection in the light of tuberculin matriculation. Am J Hygiene. 1952;56(2):139–214. doi: 10.1093/oxfordjournals.aje.a119547. [DOI] [PubMed] [Google Scholar]
- 43.Wallgren A. The time-table of tuberculosis. Tubercle. 1948;29(11):245–251. doi: 10.1016/S0041-3879(48)80033-4. [DOI] [PubMed] [Google Scholar]
- 44.Lurie MB. Resistance to tuberculosis: experimental studies in native and acquired defensive mechanism. Cambridge: Harvard University Press; 1964. [Google Scholar]
- 45.Smith DW, Harding GE. Animal model of human disease. Pulmonary tuberculosis. Animal model: experimental airborne tuberculosis in the guinea pig. Am J Pathol. 1977;89(1):273–276. [PMC free article] [PubMed] [Google Scholar]
- 46.Wolf AJ, Desvignes L, Linas B, Banaiee N, Tamura T, Takatsu K, Ernst JD. Initiation of the adaptive immune response to Mycobacterium tuberculosis depends on antigen production in the local lymph node, not the lungs. J Exp Med. 2008;205(1):105–115. doi: 10.1084/jem.20071367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dannenberg AM., Jr Delayed-type hypersensitivity and cell-mediated immunity in the pathogenesis of tuberculosis. Immunol Today. 1991;12(7):228–233. doi: 10.1016/0167-5699(91)90035-R. [DOI] [PubMed] [Google Scholar]
- 48.McSorley SJ, Asch S, Costalonga M, Reinhardt RL, Jenkins MK. Tracking salmonella-specific CD4 T cells in vivo reveals a local mucosal response to a disseminated infection. Immunity. 2002;16(3):365–377. doi: 10.1016/S1074-7613(02)00289-3. [DOI] [PubMed] [Google Scholar]
- 49.Kursar M, Bonhagen K, Kohler A, Kamradt T, Kaufmann SH, Mittrucker HW. Organ-specific CD4+ T cell response during Listeria monocytogenes infection. J Immunol. 2002;168(12):6382–6387. doi: 10.4049/jimmunol.168.12.6382. [DOI] [PubMed] [Google Scholar]
- 50.Dannenberg AM, Jr, Collins FM. Progressive pulmonary tuberculosis is not due to increasing numbers of viable bacilli in rabbits, mice and guinea pigs, but is due to a continuous host response to mycobacterial products. Tuberculosis (Edinb) 2001;81(3):229–242. doi: 10.1054/tube.2001.0287. [DOI] [PubMed] [Google Scholar]
- 51.North RJ, Jung YJ. Immunity to tuberculosis. Annu Rev Immunol. 2004;22:599–623. doi: 10.1146/annurev.immunol.22.012703.104635. [DOI] [PubMed] [Google Scholar]
- 52.Capuano SV, Croix DA, Pawar S, Zinovik A, Myers A, Lin PL, Bissel S, Fuhrman C, Klein E, Flynn JL. Experimental Mycobacterium tuberculosis infection of cynomolgus macaques closely resembles the various manifestations of human M. tuberculosis infection. Infect Immun. 2003;71(10):5831–5844. doi: 10.1128/IAI.71.10.5831-5844.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Coleman MT, Maiello P, Tomko J, Frye LJ, Fillmore D, Janssen C, Klein E, Lin PL. Early Changes by (18)Fluorodeoxyglucose positron emission tomography coregistered with computed tomography predict outcome after Mycobacterium tuberculosis infection in cynomolgus macaques. Infect Immun. 2014;82(6):2400–2404. doi: 10.1128/IAI.01599-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Martin CJ, Cadena AM, Leung VW, Lin PL, Maiello P, Hicks N, Chase MR, Flynn JL, Fortune SM. Digitally barcoding Mycobacterium tuberculosis reveals in vivo infection dynamics in the macaque model of tuberculosis. mBio. 2017;8(3):e00312-17. doi: 10.1128/mBio.00312-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Huang L, Russell DG. Protective immunity against tuberculosis: what does it look like and how do we find it? Curr Opin Immunol. 2017;48:44–50. doi: 10.1016/j.coi.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Antonelli LR, Gigliotti Rothfuchs A, Goncalves R, Roffe E, Cheever AW, Bafica A, Salazar AM, Feng CG, Sher A. Intranasal Poly-IC treatment exacerbates tuberculosis in mice through the pulmonary recruitment of a pathogen-permissive monocyte/macrophage population. J Clin Invest. 2010;120(5):1674–1682. doi: 10.1172/JCI40817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Marino S, Cilfone NA, Mattila JT, Linderman JJ, Flynn JL, Kirschner DE. Macrophage polarization drives granuloma outcome during Mycobacterium tuberculosis infection. Infect Immun. 2015;83(1):324–338. doi: 10.1128/IAI.02494-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cribbs SK, Lennox J, Caliendo AM, Brown LA, Guidot DM. Healthy HIV-1-infected individuals on highly active antiretroviral therapy harbor HIV-1 in their alveolar macrophages. AIDS Res Hum Retroviruses. 2015;31(1):64–70. doi: 10.1089/aid.2014.0133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lugo-Villarino G, Verollet C, Maridonneau-Parini I, Neyrolles O. Macrophage polarization: convergence point targeted by mycobacterium tuberculosis and HIV. Front Immunol. 2011;2:43. doi: 10.3389/fimmu.2011.00043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Herbein G, Varin A. The macrophage in HIV-1 infection: from activation to deactivation? Retrovirology. 2010;7:33–33. doi: 10.1186/1742-4690-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Souriant S, Balboa L, Dupont M, Pingris K, Kviatcovsky D, Cougoule C, Lastrucci C, Bah A, Gasser R, Poincloux R, et al. Tuberculosis exacerbates HIV-1 infection through IL-10/STAT3-dependent tunneling nanotube formation in macrophages. Cell Rep. 2019;26(13):3586–3599.e3587. doi: 10.1016/j.celrep.2019.02.091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Kuroda MJ, Sugimoto C, Cai Y, Merino KM, Mehra S, Araínga M, Roy CJ, Midkiff CC, Alvarez X, Didier ES, et al. High turnover of tissue macrophages contributes to tuberculosis reactivation in simian immunodeficiency virus-infected rhesus macaques. J Infect Dis. 2018;217(12):1865–1874. doi: 10.1093/infdis/jix625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan N, Divangahi M. Mycobacterium tuberculosis and HIV coinfection brings fire and fury to macrophages. J Infect Dis. 2018;217(12):1851–1853. doi: 10.1093/infdis/jix626. [DOI] [PubMed] [Google Scholar]
- 64.Waters R, Ndengane M, Abrahams M-R, Diedrich CR, Wilkinson RJ, Coussens AK. The Mtb-HIV syndemic interaction: why treating M. tuberculosis infection may be crucial for HIV-1 eradication. Fut Virol. 2020;15(2):101–126. doi: 10.2217/fvl-2019-0069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gleeson LE, Sheedy FJ, Palsson-McDermott EM, Triglia D, O’Leary SM, O’Sullivan MP, O’Neill LA, Keane J. Cutting edge: Mycobacterium tuberculosis induces aerobic glycolysis in human alveolar macrophages that is required for control of intracellular bacillary replication. J Immunol. 2016;196(6):2444–2449. doi: 10.4049/jimmunol.1501612. [DOI] [PubMed] [Google Scholar]
- 66.Huang L, Nazarova EV, Tan S, Liu Y, Russell DG. Growth of Mycobacterium tuberculosis in vivo segregates with host macrophage metabolism and ontogeny. J Exp Med. 2018;215(4):1135–1152. doi: 10.1084/jem.20172020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Palmer CS, Henstridge DC, Yu D, Singh A, Balderson B, Duette G, Cherry CL, Anzinger JJ, Ostrowski M, Crowe SM. Emerging role and characterization of immunometabolism: relevance to HIV pathogenesis. Serious Non-AIDS Events Cure. 2016;196(11):4437–4444. doi: 10.4049/jimmunol.1600120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Rodriguez-Mora S, Mateos E, Moran M, Martin MA, Lopez JA, Calvo E, Terron MC, Luque D, Muriaux D, Alcami J, et al. Intracellular expression of Tat alters mitochondrial functions in T cells: a potential mechanism to understand mitochondrial damage during HIV-1 replication. Retrovirology. 2015;12:78. doi: 10.1186/s12977-015-0203-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Auld SC, Fernandes J, Ahmed M, Gandhi NR, Yeligar SM, Staitieh BS. Abnormal immunometabolism and gene accessibility in alveolar macrophages in HIV. In: Conference on retroviruses and opportunistic infections (CROI): 2020; Boston, MA; 2020.
- 70.Castellano P, Prevedel L, Valdebenito S, Eugenin EA. HIV infection and latency induce a unique metabolic signature in human macrophages. Sci Rep. 2019;9(1):3941. doi: 10.1038/s41598-019-39898-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Refai A, Gritli S, Barbouche MR, Essafi M. Mycobacterium tuberculosis virulent factor ESAT-6 drives macrophage differentiation toward the pro-inflammatory M1 phenotype and subsequently switches it to the anti-inflammatory M2 phenotype. Front Cell Infect Microbiol. 2018;8:327. doi: 10.3389/fcimb.2018.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hirsch CS, Toossi Z, Othieno C, Johnson JL, Schwander SK, Robertson S, Wallis RS, Edmonds K, Okwera A, Mugerwa R, et al. Depressed T-cell interferon-gamma responses in pulmonary tuberculosis: analysis of underlying mechanisms and modulation with therapy. J Infect Dis. 1999;180(6):2069–2073. doi: 10.1086/315114. [DOI] [PubMed] [Google Scholar]
- 73.Roff SR, Noon-Song EN, Yamamoto JK. The significance of interferon-γ in HIV-1 pathogenesis, therapy, and prophylaxis. Front Immunol. 2014;4:498–498. doi: 10.3389/fimmu.2013.00498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Patella V, Florio G, Petraroli A, Marone G. HIV-1 gp120 Induces IL-4 and IL-13 release from human FcεRI+ cells through interaction with the VH 3 region of IgE. J Immunol. 2000;164(2):589–595. doi: 10.4049/jimmunol.164.2.589. [DOI] [PubMed] [Google Scholar]
- 75.Hussain R, Talat N, Ansari A, Shahid F, Hasan Z, Dawood G. Endogenously activated interleukin-4 differentiates disease progressors and non-progressors in tuberculosis susceptible families: a 2-year biomarkers follow-up study. J Clin Immunol. 2011;31(5):913–923. doi: 10.1007/s10875-011-9566-y. [DOI] [PubMed] [Google Scholar]
- 76.Ordway DJ, Costa L, Martins M, Silveira H, Amaral L, Arroz MJ, Ventura FA, Dockrell HM. Increased Interleukin-4 production by CD8 and gammadelta T cells in health-care workers is associated with the subsequent development of active tuberculosis. J Infect Dis. 2004;190(4):756–766. doi: 10.1086/422532. [DOI] [PubMed] [Google Scholar]
- 77.van Crevel R, Karyadi E, Preyers F, Leenders M, Kullberg BJ, Nelwan RH, van der Meer JW. Increased production of interleukin 4 by CD4+ and CD8+ T cells from patients with tuberculosis is related to the presence of pulmonary cavities. J Infect Dis. 2000;181(3):1194–1197. doi: 10.1086/315325. [DOI] [PubMed] [Google Scholar]
- 78.Rothchild AC, Stowell B, Goyal G, Nunes-Alves C, Yang Q, Papavinasasundaram K, Sassetti CM, Dranoff G, Chen X, Lee J, et al. Role of granulocyte-macrophage colony-stimulating factor production by T cells during Mycobacterium tuberculosis infection. mBio. 2017 doi: 10.1128/mbio.01514-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Chroneos ZCJ, C. Immunoregulatory role of GM-CSF in pulmonary tuberculosis. In: Cardona PJ, editor. Understanding tuberculosis—analyzing the origin of Mycobacterium tuberculosis pathogenicity; 2012.
- 80.Warby TJ, Crowe SM, Jaworowski A. Human immunodeficiency virus type 1 infection inhibits granulocyte-macrophage colony-stimulating factor-induced activation of STAT5A in human monocyte-derived macrophages. J Virol. 2003;77(23):12630–12638. doi: 10.1128/JVI.77.23.12630-12638.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Higgins DM, Sanchez-Campillo J, Rosas-Taraco AG, Higgins JR, Lee EJ, Orme IM, Gonzalez-Juarrero M. Relative levels of M-CSF and GM-CSF influence the specific generation of macrophage populations during infection with Mycobacterium tuberculosis. J Immunol. 2008;180(7):4892–4900. doi: 10.4049/jimmunol.180.7.4892. [DOI] [PubMed] [Google Scholar]
- 82.Lerner TR, Borel S, Greenwood DJ, Repnik U, Russell MR, Herbst S, Jones ML, Collinson LM, Griffiths G, Gutierrez MG. Mycobacterium tuberculosis replicates within necrotic human macrophages. J Cell Biol. 2017;216(3):583–594. doi: 10.1083/jcb.201603040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Shen P, Li Q, Ma J, Tian M, Hong F, Zhai X, Li J, Huang H, Shi C. IRAK-M alters the polarity of macrophages to facilitate the survival of Mycobacterium tuberculosis. BMC Microbiol. 2017;17(1):185. doi: 10.1186/s12866-017-1095-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Morris D, Khurasany M, Nguyen T, Kim J, Guilford F, Mehta R, Gray D, Saviola B, Venketaraman V. Glutathione and infection. Biochem Biophys Acta. 2013;1830(5):3329–3349. doi: 10.1016/j.bbagen.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 85.Allen M, Bailey C, Cahatol I, Dodge L, Yim J, Kassissa C, Luong J, Kasko S, Pandya S, Venketaraman V. Mechanisms of control of Mycobacterium tuberculosis by NK cells: role of glutathione. Front Immunol. 2015;6:508. doi: 10.3389/fimmu.2015.00508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Peterson JD, Herzenberg LA, Vasquez K, Waltenbaugh C. Glutathione levels in antigen-presenting cells modulate Th1 versus Th2 response patterns. Proc Natl Acad Sci USA. 1998;95(6):3071–3076. doi: 10.1073/pnas.95.6.3071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Ivanov AV, Valuev-Elliston VT, Ivanova ON, Kochetkov SN, Starodubova ES, Bartosch B, Isaguliants MG. Oxidative stress during HIV infection: mechanisms and consequences. Oxid Med Cell Longev. 2016;2016:8910396. doi: 10.1155/2016/8910396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cribbs SK, Guidot DM, Martin GS, Lennox J, Brown LA. Anti-retroviral therapy is associated with decreased alveolar glutathione levels even in healthy HIV-infected individuals. PLoS ONE. 2014;9(2):e88630. doi: 10.1371/journal.pone.0088630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Morris D, Guerra C, Khurasany M, Guilford F, Saviola B, Huang Y, Venketaraman V. Glutathione supplementation improves macrophage functions in HIV. J Interferon Cytokine Res. 2013;33(5):270–279. doi: 10.1089/jir.2012.0103. [DOI] [PubMed] [Google Scholar]
- 90.Singh A, Crossman DK, Mai D, Guidry L, Voskuil MI, Renfrow MB, Steyn AJ. Mycobacterium tuberculosis WhiB3 maintains redox homeostasis by regulating virulence lipid anabolism to modulate macrophage response. PLoS Pathog. 2009;5(8):e1000545. doi: 10.1371/journal.ppat.1000545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Trivedi A, Singh N, Bhat SA, Gupta P, Kumar A. Redox biology of tuberculosis pathogenesis. Adv Microb Physiol. 2012;60:263–324. doi: 10.1016/B978-0-12-398264-3.00004-8. [DOI] [PubMed] [Google Scholar]
- 92.Rockwood N, Costa DL, Amaral EP, Du Bruyn E, Kubler A, Gil-Santana L, Fukutani KF, Scanga CA, Flynn JL, Jackson SH, et al. Mycobacterium tuberculosis induction of heme oxygenase-1 expression is dependent on oxidative stress and reflects treatment outcomes. Front Immunol. 2017;8:542. doi: 10.3389/fimmu.2017.00542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Alam K, Ghousunnissa S, Nair S, Valluri VL, Mukhopadhyay S. Glutathione-redox balance regulates c-rel-driven IL-12 production in macrophages: possible implications in antituberculosis immunotherapy. J Immunol. 2010;184(6):2918–2929. doi: 10.4049/jimmunol.0900439. [DOI] [PubMed] [Google Scholar]
- 94.Palanisamy GS, Kirk NM, Ackart DF, Shanley CA, Orme IM, Basaraba RJ. Evidence for oxidative stress and defective antioxidant response in guinea pigs with tuberculosis. PLoS ONE. 2011;6(10):e26254. doi: 10.1371/journal.pone.0026254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Venketaraman V, Millman A, Salman M, Swaminathan S, Goetz M, Lardizabal A, David H, Connell ND. Glutathione levels and immune responses in tuberculosis patients. Microb Pathog. 2008;44(3):255–261. doi: 10.1016/j.micpath.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 96.Ly J, Lagman M, Saing T, Singh MK, Tudela EV, Morris D, Anderson J, Daliva J, Ochoa C, Patel N, et al. Liposomal glutathione supplementation restores TH1 cytokine response to Mycobacterium tuberculosis infection in HIV-infected individuals. J Interferon Cytokine Res. 2015;35(11):875–887. doi: 10.1089/jir.2014.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Guerra C, Morris D, Sipin A, Kung S, Franklin M, Gray D, Tanzil M, Guilford F, Khasawneh FT, Venketaraman V. Glutathione and adaptive immune responses against Mycobacterium tuberculosis infection in healthy and HIV infected individuals. PLoS ONE. 2011;6(12):e28378. doi: 10.1371/journal.pone.0028378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tyagi P, Pal VK, Agrawal R, Singh S, Srinivasan S, Singh A. Mycobacterium tuberculosis reactivates HIV-1 via exosome-mediated resetting of cellular redox potential and bioenergetics. mBio. 2020 doi: 10.1128/mBio.03293-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Luzio JP, Parkinson MD, Gray SR, Bright NA. The delivery of endocytosed cargo to lysosomes. Biochem Soc Trans. 2009;37(Pt 5):1019–1021. doi: 10.1042/BST0371019. [DOI] [PubMed] [Google Scholar]
- 100.Luzio JP, Gray SR, Bright NA. Endosome-lysosome fusion. Biochem Soc Trans. 2010;38(6):1413–1416. doi: 10.1042/BST0381413. [DOI] [PubMed] [Google Scholar]
- 101.Zhang C, Yang L, Zhao N, Zhao Y, Shi C. Insights into macrophage autophagy in latent tuberculosis infection: role of heat shock protein 16.3. DNA Cell Biol. 2018;37(5):442–448. doi: 10.1089/dna.2017.4066. [DOI] [PubMed] [Google Scholar]
- 102.Koziel H, Eichbaum Q, Kruskal BA, Pinkston P, Rogers RA, Armstrong MY, Richards FF, Rose RM, Ezekowitz RA. Reduced binding and phagocytosis of Pneumocystis carinii by alveolar macrophages from persons infected with HIV-1 correlates with mannose receptor downregulation. J Clin Invest. 1998;102(7):1332–1344. doi: 10.1172/JCI560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Richardson ET, Shukla S, Sweet DR, Wearsch PA, Tsichlis PN, Boom WH, Harding CV. Toll-like receptor 2-dependent extracellular signal-regulated kinase signaling in Mycobacterium tuberculosis-infected macrophages drives anti-inflammatory responses and inhibits Th1 polarization of responding T cells. Infect Immun. 2015;83(6):2242–2254. doi: 10.1128/IAI.00135-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.El Kasmi KC, Qualls JE, Pesce JT, Smith AM, Thompson RW, Henao-Tamayo M, Basaraba RJ, Konig T, Schleicher U, Koo MS, et al. Toll-like receptor-induced arginase 1 in macrophages thwarts effective immunity against intracellular pathogens. Nat Immunol. 2008;9(12):1399–1406. doi: 10.1038/ni.1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Nicol MQ, Mathys JM, Pereira A, Ollington K, Ieong MH, Skolnik PR. Human immunodeficiency virus infection alters tumor necrosis factor alpha production via Toll-like receptor-dependent pathways in alveolar macrophages and U1 cells. J Virol. 2008;82(16):7790–7798. doi: 10.1128/JVI.00362-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Gordon SB, Jagoe RT, Jarman ER, North JC, Pridmore A, Musaya J, French N, Zijlstra EE, Molyneux ME, Read RC. The alveolar microenvironment of patients infected with human immunodeficiency virus does not modify alveolar macrophage interactions with Streptococcus pneumoniae. Clin Vaccine Immunol. 2013;20(6):882–891. doi: 10.1128/CVI.00582-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Mazzolini J, Herit F, Bouchet J, Benmerah A, Benichou S, Niedergang F. Inhibition of phagocytosis in HIV-1-infected macrophages relies on Nef-dependent alteration of focal delivery of recycling compartments. Blood. 2010;115(21):4226–4236. doi: 10.1182/blood-2009-12-259473. [DOI] [PubMed] [Google Scholar]
- 108.Jambo KC, Banda DH, Kankwatira AM, Sukumar N, Allain TJ, Heyderman RS, Russell DG, Mwandumba HC. Small alveolar macrophages are infected preferentially by HIV and exhibit impaired phagocytic function. Mucosal Immunol. 2014;7(5):1116–1126. doi: 10.1038/mi.2013.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kedzierska K, Azzam R, Ellery P, Mak J, Jaworowski A, Crowe SM. Defective phagocytosis by human monocyte/macrophages following HIV-1 infection: underlying mechanisms and modulation by adjunctive cytokine therapy. J Clin Virol. 2003;26(2):247–263. doi: 10.1016/s1386-6532(02)00123-3. [DOI] [PubMed] [Google Scholar]
- 110.Jouve M, Sol-Foulon N, Watson S, Schwartz O, Benaroch P. HIV-1 buds and accumulates in “nonacidic” endosomes of macrophages. Cell Host Microbe. 2007;2(2):85–95. doi: 10.1016/j.chom.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 111.Moorjani H, Craddock BP, Morrison SA, Steigbigel RT. Impairment of phagosome-lysosome fusion in HIV-1-infected macrophages. J Acquir Immune Defic Syndr Hum Retrovirol. 1996;13(1):18–22. doi: 10.1097/00042560-199609000-00003. [DOI] [PubMed] [Google Scholar]
- 112.Fields J, Dumaop W, Eleuteri S, Campos S, Serger E, Trejo M, Kosberg K, Adame A, Spencer B, Rockenstein E, et al. HIV-1 Tat alters neuronal autophagy by modulating autophagosome fusion to the lysosome: implications for HIV-associated neurocognitive disorders. J Neurosci. 2015;35(5):1921–1938. doi: 10.1523/JNEUROSCI.3207-14.2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Dumas A, Lê-Bury G, Marie-Anaïs F, Herit F, Mazzolini J, Guilbert T, Bourdoncle P, Russell DG, Benichou S, Zahraoui A, et al. The HIV-1 protein Vpr impairs phagosome maturation by controlling microtubule-dependent trafficking. J Cell Biol. 2015;211(2):359–372. doi: 10.1083/jcb.201503124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Cinti A, Le Sage V, Milev MP, Valiente-Echeverria F, Crossie C, Miron MJ, Pante N, Olivier M, Mouland AJ. HIV-1 enhances mTORC1 activity and repositions lysosomes to the periphery by co-opting Rag GTPases. Sci Rep. 2017;7(1):5515. doi: 10.1038/s41598-017-05410-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Tomlinson GS, Bell LC, Walker NF, Tsang J, Brown JS, Breen R, Lipman M, Katz DR, Miller RF, Chain BM, et al. HIV-1 infection of macrophages dysregulates innate immune responses to Mycobacterium tuberculosis by inhibition of interleukin-10. J Infect Dis. 2014;209(7):1055–1065. doi: 10.1093/infdis/jit621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.O’Leary S, O’Sullivan MP, Keane J. IL-10 blocks phagosome maturation in Mycobacterium tuberculosis—infected human macrophages. Am J Respir Cell Mol Biol. 2011;45(1):172–180. doi: 10.1165/rcmb.2010-0319OC. [DOI] [PubMed] [Google Scholar]
- 117.Mwandumba HC, Russell DG, Nyirenda MH, Anderson J, White SA, Molyneux ME, Squire SB. Mycobacterium tuberculosis resides in nonacidified vacuoles in endocytically competent alveolar macrophages from patients with tuberculosis and HIV infection. J Immunol. 2004;172(7):4592–4598. doi: 10.4049/jimmunol.172.7.4592. [DOI] [PubMed] [Google Scholar]
- 118.Deretic V, Vergne I, Chua J, Master S, Singh SB, Fazio JA, Kyei G. Endosomal membrane traffic: convergence point targeted by Mycobacterium tuberculosis and HIV. Cell Microbiol. 2004;6(11):999–1009. doi: 10.1111/j.1462-5822.2004.00449.x. [DOI] [PubMed] [Google Scholar]
- 119.Behar SM, Martin CJ, Booty MG, Nishimura T, Zhao X, Gan HX, Divangahi M, Remold HG. Apoptosis is an innate defense function of macrophages against Mycobacterium tuberculosis. Mucosal Immunol. 2011;4(3):279–287. doi: 10.1038/mi.2011.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Moraco AH, Kornfeld H. Cell death and autophagy in tuberculosis. Semin Immunol. 2014;26(6):497–511. doi: 10.1016/j.smim.2014.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Yuan Z, Fan X, Staitieh B, Bedi C, Spearman P, Guidot DM, Sadikot RT. HIV-related proteins prolong macrophage survival through induction of Triggering receptor expressed on myeloid cells-1. Sci Rep. 2017;7:42028. doi: 10.1038/srep42028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Campbell GR, Rawat P, Bruckman RS, Spector SA. Human immunodeficiency virus type 1 Nef inhibits autophagy through transcription factor EB sequestration. PLoS Pathog. 2015;11(6):e1005018. doi: 10.1371/journal.ppat.1005018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Mehto S, Antony C, Khan N, Arya R, Selvakumar A, Tiwari BK, Vashishta M, Singh Y, Jameel S, Natarajan K. Mycobacterium tuberculosis and human immunodeficiency virus type 1 cooperatively modulate macrophage apoptosis via toll like receptor 2 and calcium homeostasis. PLoS ONE. 2015;10(7):e0131767. doi: 10.1371/journal.pone.0131767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Collini PJ, Bewley MA, Mohasin M, Marriott HM, Miller RF, Geretti AM, Beloukas A, Papadimitropoulos A, Read RC, Noursadeghi M, et al. HIV gp120 in the lungs of antiretroviral therapy-treated individuals impairs alveolar macrophage responses to pneumococci. Am J Respir Crit Care Med. 2018;197(12):1604–1615. doi: 10.1164/rccm.201708-1755OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Patel NR, Swan K, Li X, Tachado SD, Koziel H. Impaired M. tuberculosis-mediated apoptosis in alveolar macrophages from HIV + persons: potential role of IL-10 and BCL-3. J Leukocyte Biol. 2009;86(1):53–60. doi: 10.1189/JLB.0908574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Coleman MM, Basdeo SA, Coleman AM, Cheallaigh CN, Castro CPd, McLaughlin AM, Dunne PJ, Harris J, Keane J. All-trans retinoic acid augments autophagy during intracellular bacterial infection. Am J Respir Cell Mol Biol. 2018;59(5):548–556. doi: 10.1165/rcmb.2017-0382OC. [DOI] [PubMed] [Google Scholar]
- 127.Wolf AJ, Linas B, Trevejo-Nunez GJ, Kincaid E, Tamura T, Takatsu K, Ernst JD. Mycobacterium tuberculosis infects dendritic cells with high frequency and impairs their function in vivo. J Immunol. 2007;179(4):2509–2519. doi: 10.4049/jimmunol.179.4.2509. [DOI] [PubMed] [Google Scholar]
- 128.Stumptner-Cuvelette P, Morchoisne S, Dugast M, Le Gall S, Raposo G, Schwartz O, Benaroch P. HIV-1 Nef impairs MHC class II antigen presentation and surface expression. Proc Natl Acad Sci USA. 2001;98(21):12144–12149. doi: 10.1073/pnas.221256498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Schindler M, Wildum S, Casartelli N, Doria M, Kirchhoff F. Nef alleles from children with non-progressive HIV-1 infection modulate MHC-II expression more efficiently than those from rapid progressors. Aids. 2007;21(9):1103–1107. doi: 10.1097/QAD.0b013e32816aa37c. [DOI] [PubMed] [Google Scholar]
- 130.Singh SK, Andersson AM, Ellegard R, Lindestam Arlehamn CS, Sette A, Larsson M, Stendahl O, Blomgran R. HIV interferes with Mycobacterium tuberculosis antigen presentation in human dendritic cells. Am J Pathol. 2016;186(12):3083–3093. doi: 10.1016/j.ajpath.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 131.White AG, Maiello P, Coleman MT, Tomko JA, Frye LJ, Scanga CA, Lin PL, Flynn JL. Analysis of 18FDG PET/CT imaging as a tool for studying Mycobacterium tuberculosis infection and treatment in non-human primates. J Vis Exp. 2017;127:e56375. doi: 10.3791/56375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Lin PL, Ford CB, Coleman MT, Myers AJ, Gawande R, Ioerger T, Sacchettini J, Fortune SM, Flynn JL. Sterilization of granulomas is common in active and latent tuberculosis despite within-host variability in bacterial killing. Nat Med. 2014;20(1):75–79. doi: 10.1038/nm.3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Esmail H, Lai RP, Lesosky M, Wilkinson KA, Graham CM, Coussens AK, Oni T, Warwick JM, Said-Hartley Q, Koegelenberg CF, Walzl G. Characterization of progressive HIV-associated tuberculosis using 2-deoxy-2-[18 F] fluoro-d-glucose positron emission and computed tomography. Nat Med. 2016;22:1090–1093. doi: 10.1038/nm.4161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Thompson EG, Shankar S, Gideon HP, Braun J, Valvo J, Skinner JA, Aderem A, Flynn JL, Lin PL, Zak DE. Prospective discrimination of controllers from progressors early after low-dose Mycobacterium tuberculosis infection of cynomolgus macaques using blood RNA signatures. J Infect Dis. 2018;217(8):1318–1322. doi: 10.1093/infdis/jiy006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Suliman S, Thompson E, Sutherland J, Weiner RdJ, Ota MOC, Shankar S, Penn-Nicholson A, Thiel B, Erasmus M, Maertzdorf J, et al. Four-gene pan-African Blood signature predicts progression to tuberculosis. Am J Respir Crit Care Med. 2018;197:1198–1208. doi: 10.1164/rccm.201711-2340OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Zak DE, Penn-Nicholson A, Scriba TJ, Thompson E, Suliman S, Amon LM, Mahomed H, Erasmus M, Whatney W, Hussey GD, et al. A blood RNA signature for tuberculosis disease risk: a prospective cohort study. Lancet. 2016;387(10035):2312–2322. doi: 10.1016/S0140-6736(15)01316-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Whatney WE, Gandhi NR, Lindestam Arlehamn CS, Nizam A, Wu H, Quezada MJ, Campbell A, Allana S, Kabongo MM, Khayumbi J, et al. A high throughput whole blood assay for analysis of multiple antigen-specific T Cell responses in human Mycobacterium tuberculosis infection. J Immunol. 2018;200(8):3008–3019. doi: 10.4049/jimmunol.1701737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Frediani JK, Jones DP, Tukvadze N, Uppal K, Sanikidze E, Kipiani M, Tran VT, Hebbar G, Walker DI, Kempker RR, et al. Plasma metabolomics in human pulmonary tuberculosis disease: a pilot study. PLoS ONE. 2014;9(10):e108854. doi: 10.1371/journal.pone.0108854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Collins JM, Walker DI, Jones DP, Tukvadze N, Liu KH, Tran VT, Uppal K, Frediani JK, Easley KA, Shenvi N, et al. High-resolution plasma metabolomics analysis to detect Mycobacterium tuberculosis-associated metabolites that distinguish active pulmonary tuberculosis in humans. PLoS ONE. 2018;13(10):e0205398. doi: 10.1371/journal.pone.0205398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Weiner J, 3rd, Maertzdorf J, Sutherland JS, Duffy FJ, Thompson E, Suliman S, McEwen G, Thiel B, Parida SK, Zyla J, et al. Metabolite changes in blood predict the onset of tuberculosis. Nat Commun. 2018;9(1):5208. doi: 10.1038/s41467-018-07635-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.