Abstract
OBJECTIVE
To examine the relationship between health care coverage and HbA1c in young adults with youth-onset type 2 diabetes who transitioned to community diabetes care after receiving care during the Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) study.
RESEARCH DESIGN AND METHODS
Participants completed questionnaires annually. HbA1c was measured in a central laboratory. Data from 2 years before and after transitioning to community care (2013–2016) were examined and compared between states with and without expanded Medicaid.
RESULTS
In 2016 (n = 427; mean age 24 years), 2 years after transitioning to community care, 93% of participants in states with Medicaid expansion had health care coverage compared with 68% (P < 0.0001) in states without Medicaid expansion. Mean HbA1c was 9.8% in participants with government coverage, 9.3% with commercial coverage, and 10.1% in those with no coverage (P = 0.0774). Additionally, 32%, 42%, and 66% of those with government coverage, commercially covered, and no coverage, respectively, were not attending outpatient diabetes visits (P < 0.0001). Of those with government coverage, 83% reported they had adequate coverage for insulin syringes/needles/pens, and 89% for glucose-monitoring supplies, with more limited coverage in those with commercial plans. Participants with commercial coverage had higher education attainment (P < 0.0001); 52% had HbA1c ≥9.0% compared with 64% of those who were government covered and 58% with no coverage (P = 0.0646).
CONCLUSIONS
More young adults with type 2 diabetes from the TODAY cohort had health care coverage in states with expanded Medicaid but glycemic control remained poor, regardless of coverage. New therapies and approaches are needed for this vulnerable population.
Introduction
Youth-onset type 2 diabetes is associated with poor glycemic control and accelerated development of diabetes-related complications (1–10). The transition from adolescence to adulthood, which requires leaving pediatric practices and obtaining care in adult primary care or endocrinology/diabetes practices, can be difficult. The transition also often involves a change in the source and payment for health care coverage. Overall, little is known about the impact of this transition in emerging adults with youth-onset type 2 diabetes.
Health care coverage is associated with access to care, use of preventive services, and health outcomes. Adults with diabetes who are not covered by a health care plan have fewer eye and foot examinations and less self-monitoring of blood glucose and testing of glycemic status (e.g., HbA1c) (11). Medication underuse has also been reported in adults with poor health care coverage (12). With Medicaid and private health care coverage expansion under the Affordable Care Act (ACA), there has been a reduction in uninsured rates in the 644 “Diabetes Belt” counties, which are counties in the southern and eastern U.S. that had a ≥11% prevalence of diabetes in 2007–2008 (13). More outpatient care and better self-reported health in adults have also been reported (14,15). In adults with diabetes 18–64 years of age, the ACA was associated with an increase in health care coverage and reduction in out-of-pocket and total medical costs, especially for low-income families (16). For adults with diabetes cared for in safety net health centers, Medicaid expansion was associated with increases in rates of Medicaid-covered visits and recommended laboratory services (17). For low-income individuals followed at federally funded community health centers, Medicaid expansion was associated with a reduction in the rate of those with no coverage, improvement in blood pressure control, and reduction in BMI, but no improvement in glycemic control defined by HbA1c ≤9.0% (18). The health impact of care coverage has not been examined in young adults with youth-onset type 2 diabetes.
Older teens and young adults aged 18–30 years are developmentally distinct from other age groups (19). They face changes in their living, educational, occupational, social, and financial situations as well as a reduction in parental support (19). Struggles with depression, anxiety, substance abuse, and other psychosocial adjustments can negatively impact self-care. These challenges have been associated with worse glycemic control and diabetes-related outcomes in type 1 diabetes, but have not been as well studied in type 2 diabetes (20,21).
The Treatment Options for type 2 Diabetes in Adolescents and Youth (TODAY) and TODAY2 phase 1 studies (2004–2014) enrolled participants with youth-onset type 2 diabetes (19). They received, at no cost, diabetes-related clinical visits, medications, and glucose-monitoring supplies. These participants were racially and ethnically diverse and, in general, had low socioeconomic status (SES) (3,22). In 2014, TODAY2 phase 2 began as an observational follow-up study of the TODAY cohort, with research data collected at annual study visits only. Thus, after the last 2014 TODAY2 phase 1 study visit, participants were no longer provided with clinical care, diabetes medications, or glucose-monitoring supplies and were required to seek their health care, including diabetes care, in the community. Since their mean age was 22 years in 2014, this time was also associated with the transition from adolescence to young adulthood and, under the ACA, the ability to remain on their parents’ health care coverage until 26 years of age. This report examines and compares health care coverage and glycemic control during the 2 years before transition to community care (when participants received diabetes care from the study team at no cost) to the 2 years after the transition to community care in the TODAY2 cohort.
Research Design and Methods
Study Participants
The TODAY randomized trial, which started enrollment in 2004, has been previously described (3,23). TODAY enrolled youth, aged 10–17 years, with new-onset type 2 diabetes (mean duration 7.8 months), who were obese/overweight (BMI ≥85th percentile) and had negative pancreatic autoantibodies (GAD65 and tyrosine phosphatase antibodies). After the randomized treatment ended in 2011 and until 2014 (TODAY2 phase 1), participants received metformin and/or insulin as needed to maintain glycemic control, diabetes-related visits, and glucose-monitoring supplies, at no cost to them. In 2014, TODAY2 phase 1 ended and TODAY2 phase 2 began as an observational follow-up study. No medications, clinical care, or monitoring supplies were provided in TODAY2 phase 2. Participants transitioned to community care. Data from participants in the TODAY2 study who completed annual visits between 2013 and 2016 (2 years before and 2 years after the transition to community care) were examined.
Data Sources
Annual assessments included completion of questionnaires and collection of anthropometric measures, medical history, and laboratory tests, as previously described (3,23). Blood samples for HbA1c were analyzed centrally at the TODAY2 central laboratory (Northwest Lipid Metabolism and Diabetes Research Laboratories, University of Washington, Seattle, WA).
Elevated blood pressure was defined as either a systolic blood pressure ≥130 mmHg or diastolic blood pressure ≥80 mmHg, elevated LDL as an LDL cholesterol ≥130 mg/dL, and albuminuria as a urine albumin-to-creatinine ratio ≥30 mg/g. This study was approved by the Institutional Review Boards of all participating institutions, and all participants provided written informed consent.
Health Care Coverage
At annual visits, participants were asked if they were covered by a health care coverage plan. If they answered no, they were classified as having no coverage. If they answered yes, they were asked about their type of health care coverage. Coverage was categorized as: 1) government-sponsored (Medicaid, Medicare, Children’s Health Insurance Program, state-funded, Indian Health Service, or other federally funded), 2) commercial, or 3) mixed (had more than one coverage type during the time specified). Participants may have changed health care coverage from one year to the next. Each participant contributed between 1 and 4 years of data. When determining the percent of participants with each type of health care coverage each year, the denominator reflects participant responses to the questionnaire for that year. Though this manuscript classified Indian Health Service as government-sponsored coverage, it is important to note that the Indian Health Service is not an insurance but a provision of health care benefits funded yearly through appropriations by the U.S. Congress. Commercial coverage could have been obtained through work or purchased individually by the participant or their parents (the number of participants <26 years of age covered solely by their parents’ health care is not known). Participants were also asked if the health care coverage plan paid for all or part of: 1) diabetes medications, including insulin, 2) insulin syringes, pens, and needles, and 3) glucose-monitoring strips and related supplies. Starting in 2016, participants were asked about the number of outpatient diabetes visits made during the past 6 months as well.
With the implementation of the ACA, many, but not all, states expanded health care coverage to their populations through an expansion of Medicaid eligibility. Participants in TODAY2 were classified as residents of Medicaid expansion states or not based upon policy information summarized by a publication of the Kaiser Family Foundation (24).
Statistical Analyses
Data analyses were largely focused on describing changes in health care coverage, care, and glycemic control as subjects transitioned to community care. Demographic and clinical characteristics were identified and compared among the type of health care plan (no coverage, government, or commercial) using the χ2 test or Cochran-Armitage trend test for categorical variables and the Kruskal-Wallis test for continuous variables. Generalized estimating equations were used to assess group differences (states with and without expanded Medicaid, sex, and race/ethnicity) on the prevalence of health care coverage over repeated time points. Generalized linear mixed models were used to assess differences in mean HbA1c by health care plan type (no coverage vs. government vs. commercial) over time, and generalized estimating equation models were used to assess differences in the prevalence of HbA1c ≥9.0% by health care coverage type over time. Covariates measured repeatedly over time were entered into the models as time-dependent covariates. Statistical significance was defined as P < 0.05.
Results
Participant Characteristics
Participant characteristics during the 2 years before and after the start of TODAY2 phase 2—that is, the transition to community care—are shown in Table 1. In 2013, when participants were receiving their diabetes care from the study sites, the mean age was 21 years (SD 3; range 15–27 years), mean duration of diabetes was 7.3 years (SD 1.5), with 63% female, 20% non-Hispanic White, 34% non-Hispanic Black, and 40% Hispanic, and 5% attended college. Mean HbA1c was 8.8% (SD 2.9; range 4.3–18.1%), with 44% of participants having HbA1c ≥9.0%. Two years after the transition to community diabetes care in 2016, the mean age was 24 years (SD 2; range 18–30 years), mean duration of diabetes 10.3 years (SD 1.4), and 18% attended college. Mean HbA1c increased to 9.6% (SD 3.0; range 4.6–17.2%), with 58% of participants having HbA1c ≥9.0%.
Table 1.
Participant characteristics by year of study
| TODAY2 phase 1 | TODAY2 phase 2 | P value | |||
|---|---|---|---|---|---|
| Study-provided diabetes care | Transition to community diabetes care | Community diabetes care | |||
| Year | 2013 | 2014 | 2015 | 2016 | |
| N | 421 | 439 | 433 | 427 | |
| Age (years) | 21 (3) | 22 (3) | 23 (3) | 24 (2) | — |
| Percent ≥26 years of age | 1 | 4 | 12 | 22 | — |
| Sex (% female) | 63 | 64 | 64 | 64 | 0.9878 |
| Race/ethnicity (%) | 0.9773 | ||||
| Non-Hispanic White | 20 | 19 | 20 | 20 | |
| Non-Hispanic Black | 34 | 34 | 33 | 35 | |
| Hispanic | 40 | 38 | 40 | 38 | |
| Education (%) | <0.0001 | ||||
| Less than high school | 29 | 23 | 13 | 8 | |
| Completed high school or GED | 66 | 69 | 74 | 73 | |
| Attended college | 5‖ | 8 | 13 | 18 | |
| Duration of diabetes (years) | 7.3 (1.5) | 8.4 (1.5) | 9.4 (1.5) | 10.3 (1.4) | — |
| Insulin therapy (%) | 63 | 61 | 53 | 55 | 0.0046 |
| HbA1c in % | 8.8 (2.9) | 9.1 (3.0) | 9.5 (3.2) | 9.6 (3.0) | 0.0003 |
| HbA1c in mmol/mol | 73 (8) | 76 (9) | 80 (11) | 81 (9) | |
| Percent with HbA1c ≥9.0% | 44 | 51 | 55 | 58 | <0.0001 |
| Comorbidities (%) | |||||
| Elevated blood pressure* | 26 | 29 | 33 | 37 | 0.0006 |
| Elevated LDL† | 15 | 16 | 16 | 17 | 0.3112 |
| Albuminuria‡ | 20 | 25 | 28 | 32 | <0.0001 |
| Number of outpatient visits (%)§ | |||||
| 0 | — | — | — | 41 | — |
| 1–2 | — | — | — | 49 | |
| ≥3 | — | — | — | 10 | |
| Health care coverage (% covered) | 76 | 81 | 87 | 84 | 0.0001 |
| Health care coverage type (%) | 0.0006 | ||||
| Government | 37 | 42 | 43 | 43 | |
| Commercial | 38 | 37 | 40 | 38 | |
| Mixed | 1 | 2 | 3 | 3 | |
| No coverage | 24 | 19 | 13 | 16 | |
Data are mean (SD) or percent. P values are from the χ2 test or Cochran-Armitage trend test for categorical variables and Kruskal-Wallis test for continuous variables. There were n = 510 participants who reported their health care coverage status at least once between 2013 and 2016.
Elevated blood pressure defined as systolic blood pressure ≥130 and/or diastolic blood pressure ≥80 mmHg.
Elevated LDL defined as LDL cholesterol ≥130 mg/dL.
Albuminuria defined as a urine albumin-to-creatinine ratio ≥30 mg/g.
“In the past 6 months, how many times did you make an appointment with a doctor or clinic for routine diabetes care?”
Aged 15–27 years.
When compared with the TODAY participants who were not included in the present analyses (n = 189), the cohort was similar in the distribution of sex, race/ethnicity, household education, diabetes duration, BMI, waist circumference, and HbA1c at entry into the TODAY study. However, participants who were included in the analyses were slightly, but significantly, younger with a mean of 13.8 (SD 2.0) years at TODAY baseline compared with nonparticipants with a mean of 14.5 (SD 2.0) years.
Health Care Coverage
There were 510 participants who reported their health care coverage status and type of plan at least once between 2013 and 2016 (range one to four times); 54% had data for all 4 years, 29% for 3 years, 11% for 2 years, and only 6% for 1 year. Between 2013 and 2016, only 29 participants reported having coexisting government and commercial plans. Over this time period, health care coverage increased in the study group. In 2013, prior to transition to community care and prior to the implementation of the ACA, 76% of TODAY2 participants had health care coverage (37% government, 38% commercial, and 1% mixed), whereas 24% had no coverage. Two years after the transition to community care in 2016 (Table 1), 84% of TODAY2 participants had health care coverage (43% government, 38% commercial, and 3% mixed), and 16% reported no coverage, similar to the percent with no coverage in the general population at this age (25). There were 188 participants who reported having no health care coverage at least once between 2013 and 2016, 32 of whom reported no coverage consistently at all visits.
Expanded details on participant characteristics by type of health care coverage are shown in Table 2. One aspect of current commercial plans is that children can receive coverage from parental plans until 26 years of age. In 2016, 22% of the study participants were ≥26 years of age (Table 1); however, coverage through commercial plans did not differ significantly based on age (38% ≥26 years vs. 41% <26 years). Furthermore, in 2016, 19% of participants ≥26 years of age had no health care coverage compared with 15% who were <26 years old (P = 0.3223).
Table 2.
Participant characteristics by health care coverage status and type of plan
| TODAY2 phase 1 | TODAY2 phase 2 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Transition to community diabetes care | Community diabetes care | |||||||||||
| 2014 | 2015 | 2016 | ||||||||||
| Government | Commercial | No coverage | P value | Government | Commercial | No coverage | P value | Government | Commercial | No coverage | P value | |
| N | 184 | 164 | 84 | 187 | 175 | 57 | 186 | 161 | 67 | |||
| Age (years) | 22 (3) | 22 (2) | 22 (2) | 0.2189 | 23 (3) | 23 (2) | 23 (2) | 0.0066 | 24 (3) | 24 (2) | 25 (2) | 0.0184 |
| Sex (% female) | 68 | 65 | 50 | 0.0123 | 68 | 64 | 49 | 0.0354 | 68 | 61 | 61 | 0.4079 |
| Race/ethnicity (%) | 0.0033 | 0.1034 | 0.2037 | |||||||||
| Non-Hispanic White | 14 | 25 | 21 | 16 | 25 | 19 | 18 | 22 | 16 | |||
| Non-Hispanic Black | 32 | 36 | 36 | 35 | 30 | 35 | 34 | 34 | 39 | |||
| Hispanic | 41 | 35 | 39 | 40 | 41 | 44 | 42 | 39 | 31 | |||
| Education (%) | <0.0001 | <0.0001 | <0.0001 | |||||||||
| Less than high school | 34 | 14 | 19 | 22 | 5 | 14 | 13 | 1 | 16 | |||
| Completed high school or GED | 62 | 74 | 74 | 72 | 73 | 81 | 75 | 70 | 75 | |||
| Attended college | 4 | 12 | 7 | 6 | 23 | 5 | 12 | 29 | 9 | |||
| Duration of diabetes (years) | 8.3 (1.4) | 8.6 (1.5) | 8.3 (1.4) | 0.0806 | 9.2 (1.4) | 9.6 (1.5) | 9.3 (1.5) | 0.0265 | 10.1 (1.4) | 10.5 (1.5) | 10.5 (1.4) | 0.0317 |
| Insulin therapy (%) | 61 | 59 | 60 | 0.9026 | 63 | 45 | 46 | 0.0013 | 65 | 51 | 43 | 0.0031 |
| HbA1c in % | 9.3 (2.9) | 8.8 (2.9) | 9.1 (3.0) | 0.2360 | 9.6 (3.1) | 9.1 (3.1) | 10.1 (3.5) | 0.1537 | 9.8 (2.9) | 9.3 (3.1) | 10.1 (3.2) | 0.0774 |
| HbA1c in mmol/mol | 78 (8) | 73 (8) | 76 (9) | 81 (10) | 76 (10) | 87 (15) | 84 (8) | 78 (10) | 87 (11) | |||
| Percent with HbA1c ≥9.0% | 55 | 45 | 52 | 0.1430 | 58 | 50 | 60 | 0.1933 | 64 | 52 | 58 | 0.0646 |
| Comorbidities (%) | ||||||||||||
| Elevated BP* | 28 | 27 | 33 | 0.6258 | 30 | 33 | 39 | 0.5131 | 37 | 37 | 33 | 0.8413 |
| Elevated LDL† | 17 | 17 | 11 | 0.3671 | 13 | 18 | 23 | 0.2127 | 15 | 22 | 16 | 0.1611 |
| Albuminuria‡ | 20 | 23 | 37 | 0.0097 | 27 | 27 | 29 | 0.9324 | 32 | 30 | 33 | 0.9018 |
| Number of outpatient visits (%)§ | ||||||||||||
| 0 | — | — | — | — | — | — | 32 | 42 | 66 | <0.0001 | ||
| 1–2 | — | — | — | — | — | — | 54 | 52 | 27 | |||
| ≥3 | — | — | — | — | — | — | 15 | 6 | 7 | |||
| Health care coverage (%)§ | ||||||||||||
| Diabetes medications | ||||||||||||
| Yes | 81 | 82 | — | 87 | 89 | — | 94 | 88 | — | |||
| Do not know/refused | 18 | 18 | — | 11 | 10 | — | 5 | 9 | — | |||
| Insulin syringes/pens/needles | ||||||||||||
| Yes | 72 | 61 | — | 78 | 73 | — | 83 | 77 | — | |||
| Do not know/refused | 25 | 39 | — | 18 | 25 | — | 13 | 21 | — | |||
| Glucose-monitoring supplies | ||||||||||||
| Yes | 79 | 60 | — | 81 | 79 | — | 89 | 80 | — | |||
| Do not know/refused | 18 | 38 | — | 15 | 16 | — | 7 | 15 | — | |||
Data are mean (SD) or percent for participants who reported health care coverage. Participants who reported mixed coverage were not included (n = 7 in 2014, n = 14 in 2015, and n = 13 in 2016).
BP, blood pressure.
Elevated blood pressure defined as systolic blood pressure ≥130 and/or diastolic blood pressure ≥80 mmHg.
Elevated LDL defined as LDL cholesterol ≥130 mg/dL.
Albuminuria defined as a urine albumin-to-creatinine ratio ≥30 mg/g.
“In the past 6 months, how many times did you make an appointment with a doctor or clinic for routine diabetes care?” Health care coverage (percent of covered). “Yes” is percent of those covered who reported adequate coverage.
Health care coverage type by sex, race/ethnicity, and education is also shown in Table 2. In 2014, 50% of those with no coverage were female. Among those with government coverage or commercial coverage, a greater proportion were female (69% and 65%, respectively, vs. 50% without coverage [P = 0.0123]). This pattern was similar in 2015; however, by 2016, 61% of those with no coverage were female compared with 68% with government and 62% with commercial coverage (P = 0.4079). Differences in health care coverage category by race/ethnicity were significant in 2014 (P = 0.0033) but were not significant in 2015 and 2016. Participants with commercial coverage had higher education attainment than participants with no coverage or in government plans (P < 0.0001 for all 3 years). By education, in 2016, participants with less than high school education were more likely to have no coverage or to have government coverage and less likely to have commercial coverage (P < 0.0001). College-educated participants were proportionally overrepresented in the commercial coverage category and less likely to have no coverage or use government plans.
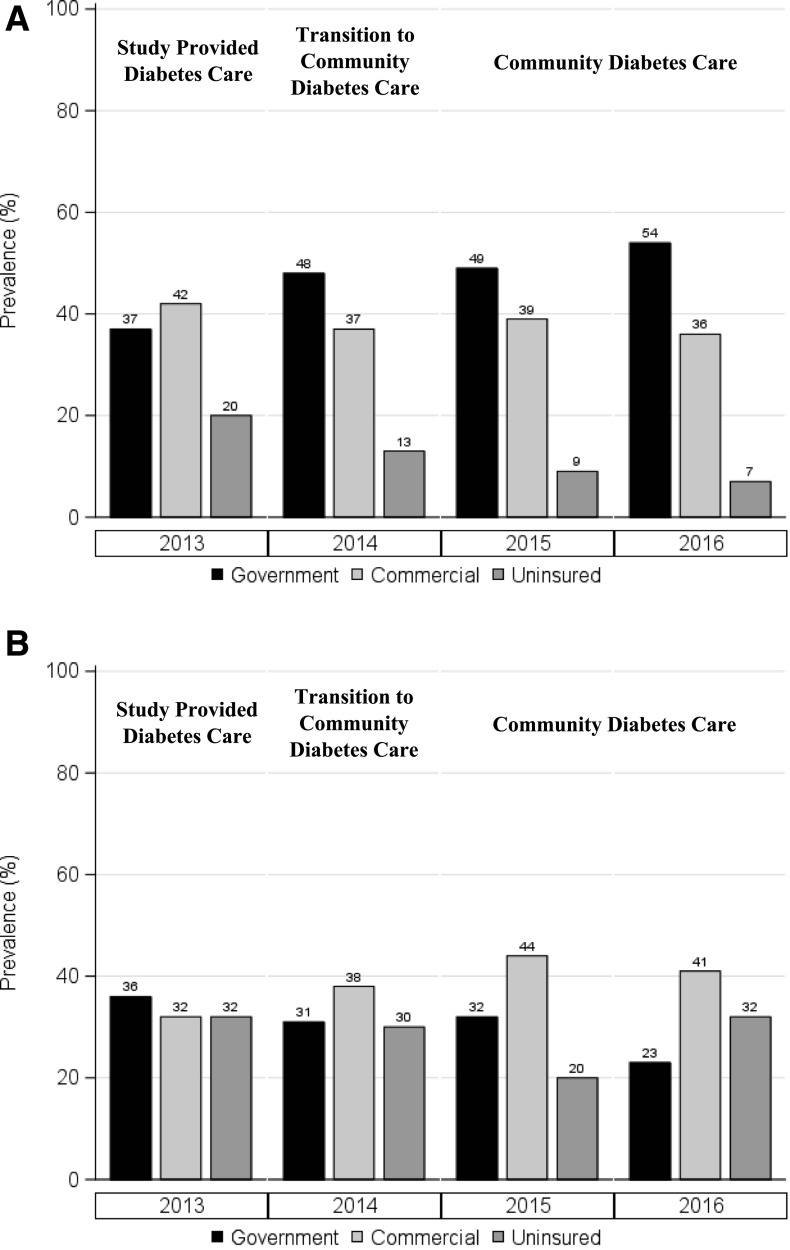
Full implementation of the ACA began in 2014, and many study subjects were resident in states with expanded Medicaid coverage. Notably, CA, CO, CT, IL, MA, NY, and OH enacted expanded Medicaid on 1 January 2014 and PA on 1 January 2015. Health care coverage by participant residency in states with expanded Medicaid and in states that did not have expanded Medicaid (MO, OK, and TX) is shown in Fig. 1. Over the 4 years (2013–2016) of follow-up, the average proportion of those with health care coverage was higher (88% vs. 72%) in states with Medicaid expansion (P < 0.0001). In 2015 and 2016, 26% (one out of every four participants) did not have health care coverage in states without expanded Medicaid compared with 8% in states with expanded Medicaid. The percent with commercial coverage did not significantly change from 2013 to 2016 in states with expanded Medicaid. However, the percent of participants with no coverage decreased, and the percent with government-sponsored coverage increased. Health care coverage in the three states in which subjects did not have availability of Medicaid expansion did not substantially change over time.
Figure 1.
Percent of participants with health care coverage in states with expanded Medicaid (seven states) (A) and not expanded Medicaid (three states) (B). Participants who reported mixed coverage were not included (n = 3 in 2013, n = 7 in 2014, n = 14 in 2015, and n = 13 in 2016).
In 2013, before a respective state expanded Medicaid, 87% of females had health care coverage compared with 68% of males (P = 0.0002). By 2016, after expansion, this sex difference disappeared, with 94% of females and 91% of males having health care coverage in states with expanded Medicaid (P = 0.3754). For participants in states without Medicaid expansion, there were no significant differences in the percent of participants with health care coverage by sex over time (2013–2016; P = 0.3988). In 2013, compared with 2016, 70% versus 68% of females and 65% versus 68% of males, respectively, had health care coverage. There were no significant differences in the percent of participants with health care coverage by race and ethnicity over time (2013–2016) (Table 2) by Medicaid expansion status.
Health care coverage was related to the frequency of outpatient visits for diabetes care. In 2016, 66% of those without coverage did not report any visits in the last 6 months compared with 32% of those with government and 42% of those with commercial coverage plans (P < 0.0001) (Tables 1 and 2). Further, the percent of participants using insulin was similar across coverage types in 2014 (59–61%), but after transitioning to community care and after the ACA, fewer participants with no coverage and fewer commercially covered participants were using insulin compared with those with government coverage (2015: 46% and 45% vs. 63%, P = 0.0007; and 2016: 43% and 51% vs. 65%, P = 0.0007) (Table 2).
For participants with health care coverage, self-reported details on coverage for diabetes medications and supplies were examined (Table 2). Over time, participants reported higher proportions of coverage for these items, most notably for blood glucose–monitoring supplies. This pattern of increasing coverage was seen in both government and commercial coverage plans. However, as shown in Table 2, several participants did not have knowledge of the extent of their coverage or did not share this knowledge.
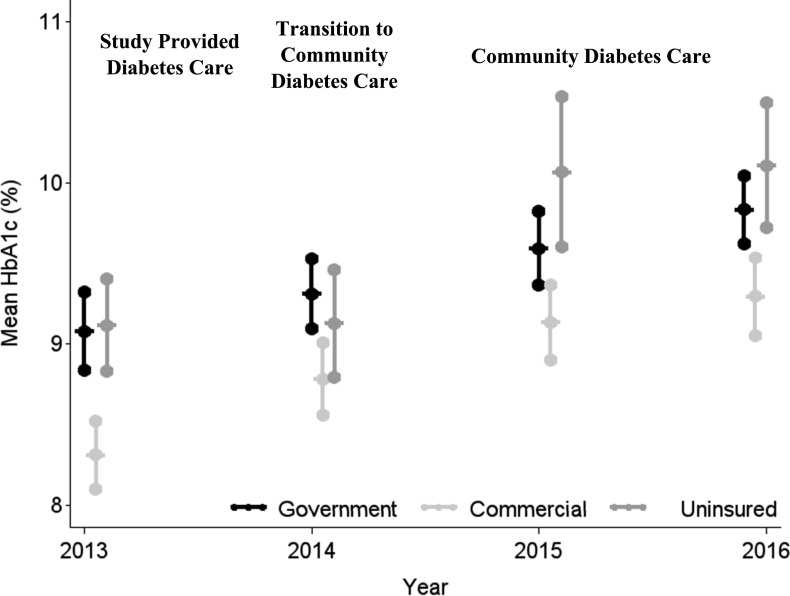
Health Care Coverage and Diabetes-Related Outcomes
The glycemic control (assessed by HbA1c) of the participants by health care coverage status is shown in Tables 1 and 2 and Fig. 2. Overall, and throughout the evaluation, the majority of participants had poor glycemic control (HbA1c ≥9.0%), independent of type of health care coverage. Further, mean HbA1c and the proportion with HbA1c ≥9.0% increased consistently over time. There was a pattern of lower mean HbA1c in participants with commercial coverage, although the differences in means among types of health care coverage were not significant (2014–2016). From 2013 to 2016, mean HbA1c for those who consistently reported having government coverage (n = 130) was 9.4% (SD 2.9), commercial coverage (n = 145) was 8.8% (SD 2.9), and those with no coverage (n = 32) was 9.4% (SD 3.2). In 2016, the mean HbA1c for those with government-sponsored coverage was 9.8%, those with commercial coverage was 9.3%, and those without coverage was 10.1% (P = 0.0774).
Figure 2.
HbA1c of participants by health care coverage (mean ± SD). Participants who reported mixed coverage were not included (n = 3 in 2013, n = 7 in 2014, n = 14 in 2015, and n = 13 in 2016).
These patterns were also found for participants categorized as having extremely poor glycemic control (HbA1c ≥9.0%). There was no significant difference in proportion with HbA1c ≥9.0% by year (2014, 2015, and 2016), but there was a trend over time for those with commercial coverage to have a lower proportion of HbA1c ≥9.0% (average proportion 48%) compared with those with government-sponsored health coverage (55%) and those without coverage (54%; longitudinal unadjusted model, P = 0.0276; adjusted for age, sex, race/ethnicity, and education, P = 0.0224). Education status was not a predictor of HbA1c (P = 0.2361) or prevalence of HbA1c ≥9.0% (P = 0.0583). The mean HbA1c over time for those with less than high school education was 9.2%, in those who completed high school or general education diploma (GED) was 9.3%, and for those who attended college was 9.0% (P = 0.2361).
Other short-term outcomes related to diabetes care were also examined for potential association with health care coverage. The prevalence of participants with elevated blood pressure, elevated LDL, and albuminuria by year and by health care coverage status is shown in Table 2. Overall, there were no significant differences in these comorbidities by health care coverage status after transitioning to community care (2015 and 2016). However, the frequency of elevated blood pressure and albuminuria increased over time in those with government or commercial plans, but not among those without coverage.
Conclusions
Emerging adults with youth-onset type 2 diabetes are a vulnerable population with low SES and a chronic disease that requires ongoing treatment to help prevent premature morbidity and mortality (9). It is important for these low SES individuals to have health care coverage to enable better access to health care, including medications, supplies, and services important for the prevention and treatment of complications. However, this population is also experiencing psychosocial, economic, and environmental challenges. Health care coverage as currently configured and diabetes care as currently provided are not sufficient to meet the needs of this population.
Our study demonstrated that health care coverage increased over time, likely related to the implementation of the ACA, despite this being a period of transition in which many individuals are at greatest risk of not having coverage. Further, it appears that expansion of Medicaid eligibility made it possible for most of our participants to obtain health care coverage. We found that 2 years after transitioning from the TODAY study to community diabetes care (2016), 93% of participants in Medicaid expansion states had health care coverage compared with 68% in states without Medicaid expansion. Those living in Medicaid expansion states were more likely to have government-sponsored health coverage. The increased health care coverage and increased eligibility for Medicaid also appear to benefit this study population in terms of the use of necessary care and the payment for diabetes medications and supplies. Health care coverage for medications and supplies appears to have increased over time with the greater coverage during this period. Use of diabetes outpatient visits was notably higher in those with government coverage plans than those with no coverage. This suggests that Medicaid expansion is particularly important for emerging adults with youth-onset type 2 diabetes. The reported findings are similar in degree to evidence from earlier reports. For young adults with type 2 diabetes in the SEARCH for Diabetes in Youth study, 74% of those without coverage did not receive follow-up health care, compared with 4% of those with private health care coverage and 22% of those with Medicaid/Medicare/other health care coverage (26), confirming the importance of having health care coverage in this at-risk group.
The findings in this report support a relationship between health care coverage and glycemic control (HbA1c ≥9.0%), after adjusting for age, sex, race/ethnicity, and education. Overall, mean HbA1c and the percent of participants with HbA1c ≥9.0% was high in all health care coverage groups and increased over time. Approximately half of commercially covered participants had HbA1c ≥9.0%. There was a trend for TODAY2 participants without coverage to have higher HbA1c levels than those with health care coverage. In adults seen in federally funded health care centers, Medicaid expansion was not associated with improvement in glycemic control defined by HbA1c <9.0% but was associated with improvement in blood pressure control and reduction in BMI (18).
It is well established that glycemic and blood pressure control are associated with the development of chronic life-threatening diabetes complications that can occur prematurely and more rapidly in youth-onset type 2 diabetes (1,5,6,8,9). There is also an increase in pregnancy-related complications and fetal abnormalities (10). The lack of health care coverage in one out of four TODAY2 participants who were in states without Medicaid expansion is therefore of great concern. Thus, although health care coverage is needed for access to care, especially in this low SES population, additional interventions and treatment approaches are needed to improve glycemic control and diabetes outcomes.
Mean HbA1c in TODAY2 phase 2 participants was similar to reports from the youth-onset Type 2 Diabetes Registry of the Pediatric Diabetes Consortium (27). Registry participants with a duration of type 2 diabetes of >4 years (median diabetes duration of 5.5 years; n = 559) had mean HbA1c of 9.2% (SD 2.9) (27). The SEARCH for Diabetes in Youth Study Group reported poor glycemic control (defined as HbA1c ≥9.5%) in 47% of their type 2 diabetes sample ≥19 years of age (28). Lower mean HbA1c (better glycemic control) has been reported in adults with diabetes treated with insulin or oral medications as well as in adults diagnosed with diabetes but untreated (for all adults aged ≥20 years, 7.4% and 6.3%, respectively, and for the subgroup of younger adults aged 20–44 years, 8.1% and 6.4%, respectively) (29). A smaller percent of adults (16% [95% CI 13–18]) aged ≥18 years is also described as having poor glycemic control (defined as HbA1c >9.0%) (30). This highlights important differences between youth-onset and adult-onset type 2 diabetes, with youth onset being associated with worse glycemic control and early development of complications (1–7,10).
The cost of diabetes care for participants with youth-onset type 2 diabetes in TODAY has been described (31). These costs are challenging, if not insurmountable, for many low SES individuals in the absence of health care coverage. Of those who were covered in TODAY2 phase 2, and especially for those with commercial care coverage, there was <100% coverage for diabetes medications, insulin-related supplies, and glucose-monitoring supplies by self-report. For glucose monitoring, inadequate coverage was greater in those covered by commercial compared with government sources. We speculate that this may be due to the greater use of high-deductible commercial policies and higher copayment requirements over time. We have previously reported that the frequency of glucose monitoring was associated with lower HbA1c levels during the TODAY trial (32).
There are several limitations to our study. The TODAY2 study cohort is a selected population in which participants may have been more motivated than non–study participants and may have greater social support, since an inclusion criterion for enrollment in TODAY was the participation of a family support person (3,23). Study staff also provided guidance that may have helped participants obtain health care coverage. These issues favor a higher prevalence of health care coverage in this cohort or attenuated differences between individuals in nonexpansion and expansion states, so it is possible that in the general population of emerging adults with type 2 diabetes, health care coverage status may be worse.
Another limitation is the self-report measurement of health care coverage status. This method of measurement is used frequently to identify the presence or absence of coverage, but published reports note that such an approach may underreport Medicaid enrollment and inflate the proportion of those without coverage (33). Also, self-report information on the details of coverage may be misclassified. Approximately a quarter of respondents were unsure of (or declined to answer) questions about health care coverage related to diabetes medications and supplies. It is also possible that some participants may not have had continuous health care coverage over the year. Finally, with the exception of the St. Louis, MO sites, in which participants were specifically asked about their state of residence, we assumed that participants lived in the same state as their study site. A strength is the annual standardized follow-up of this well-characterized cohort.
In conclusion, Medicaid expansion was associated with a higher presence of health care coverage in emerging adults with type 2 diabetes. However, given the overall poor glycemic control, health care coverage is necessary but not sufficient for the management of this challenging disease and for the prevention of diabetes-related complications. Attention to social and economic determinants of health, strategies to improve adherence, as well as better therapies are needed.
Article Information
Acknowledgments. The authors thank the American Indian partners associated with the clinical center located at the University of Oklahoma Health Sciences Center, including members of the Absentee Shawnee Tribe, Cherokee Nation, Chickasaw Nation, Choctaw Nation of Oklahoma, and Oklahoma City Area Indian Health Service for participation and guidance.
The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the respective tribes and the Indian Health Service.
Funding. This work was completed with funding from the National Institute of Diabetes and Digestive and Kidney Diseases and the National Institutes of Health Office of the Director through grants U01-DK61212, U01-DK61230, U01-DK61239, U01-DK61242, and U01-DK61254. The TODAY Study Group received donations in support of the study’s efforts from Becton Dickinson, Bristol-Myers Squibb, Eli Lilly and Company, GlaxoSmithKline, LifeScan, Inc., Pfizer, and Sanofi.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The National Institute of Diabetes and Digestive and Kidney Diseases project office was involved in all aspects of the study, including design and conduct; collection, management, analysis, and interpretation of the data; review and approval of the manuscript; and decision to submit the manuscript for publication.
Duality of Interest. R.S.W. participates in multicenter clinical trials sponsored by Medtronic, Insulet, Tolerion, Eli Lilly and Company, Diasome Pharmaceuticals, and Boehringer Ingelheim and was a consultant for Insulogic. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. R.S.W. wrote the manuscript. B.H.B. conducted the statistical analyses and wrote sections of the manuscript. T.J.S., W.H.H., S.K., R.A.G.-K., L.L., S.M., M.S., M.V.N., and P.S.Z. wrote sections of the manuscript and reviewed and edited the manuscript. B.H.B. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented as part of a symposium talk at the 79th Scientific Sessions of the American Diabetes Association, San Francisco, CA, 7–11 June 2019.
Footnotes
A complete list of individuals in the TODAY Study Group can be found in the supplementary material.
Clinical trial reg. no. NCT00081328, clinicaltrials.gov
This article contains supplementary material online at https://doi.org/10.2337/figshare.12656921.
Contributor Information
Collaborators: The TODAY Study Group, Ruth S. Weinstock, Barbara H. Braffett, Thomas J. Songer, William H. Herman, Shihchen Kuo, Rose A. Gubitosi-Klug, Lori Laffel, Siripoom McKay, Maggie Siska, Michelle Van Name, and Philip S. Zeitler
Appendix
Writing Committee: Ruth S. Weinstock (State University of New York Upstate Medical University, Syracuse, NY); Barbara H. Braffett (The Biostatistics Center, George Washington University, Rockville, MD); Thomas J. Songer (University of Pittsburgh, Pittsburgh, PA); William H. Herman and Shihchen Kuo (University of Michigan, Ann Arbor, MI); Rose A. Gubitosi-Klug (Case Western Reserve University, Rainbow Babies and Children’s Hospital, Cleveland, OH); Lori Laffel (Joslin Diabetes Center, Harvard Medical School, Boston, MA); Siripoom McKay (Baylor College of Medicine, Houston, TX); Maggie Siska (Saint Louis University Health Sciences Center, St. Louis, MO); Michelle Van Name (Yale School of Medicine, New Haven, CT); Philip S. Zeitler (University of Colorado School of Medicine, Aurora, CO).
References
- 1.Tryggestad JB, Willi SM. Complications and comorbidities of T2DM in adolescents: findings from the TODAY clinical trial. J Diabetes Complications 2015;29:307–312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jensen ET, Dabelea D. Type 2 diabetes in youth: new lessons from the SEARCH study. Curr Diab Rep 2018;18:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zeitler P, Hirst K, Pyle L, et al.; TODAY Study Group . A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med 2012;366:2247–2256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.TODAY Study Group Lipid and inflammatory cardiovascular risk worsens over 3 years in youth with type 2 diabetes: the TODAY clinical trial. Diabetes Care 2013;36:1758–1764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.TODAY Study Group Rapid rise in hypertension and nephropathy in youth with type 2 diabetes: the TODAY clinical trial. Diabetes Care 2013;36:1735–1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.TODAY Study Group Retinopathy in youth with type 2 diabetes participating in the TODAY clinical trial. Diabetes Care 2013;36:1772–1774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Levitt Katz L, Gidding SS, Bacha F, et al.; TODAY Study Group . Alterations in left ventricular, left atrial, and right ventricular structure and function to cardiovascular risk factors in adolescents with type 2 diabetes participating in the TODAY clinical trial. Pediatr Diabetes 2015;16:39–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Eppens MC, Craig ME, Cusumano J, et al.. Prevalence of diabetes complications in adolescents with type 2 compared with type 1 diabetes. Diabetes Care 2006;29:1300–1306 [DOI] [PubMed] [Google Scholar]
- 9.Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol 2018;6:69–80 [DOI] [PubMed] [Google Scholar]
- 10.Klingensmith GJ, Pyle L, Nadeau KJ, et al.; TODAY Study Group . Pregnancy outcomes in youth with type 2 diabetes: the TODAY study experience. Diabetes Care 2016;39:122–129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Nelson KM, Chapko MK, Reiber G, Boyko EJ. The association between health insurance coverage and diabetes care; data from the 2000 Behavioral Risk Factor Surveillance System. Health Serv Res 2005;40:361–372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piette JD, Wagner TH, Potter MB, Schillinger D. Health insurance status, cost-related medication underuse, and outcomes among diabetes patients in three systems of care. Med Care 2004;42:102–109 [DOI] [PubMed] [Google Scholar]
- 13.Lobo JM, Kim S, Kang H, et al.. Trends in uninsured rates before and after Medicaid expansion in counties within and outside of the diabetes belt. Diabetes Care 2020;43:1449–1455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sommers BD, Blendon RJ, Orav EJ, Epstein AM. Changes in utilization and health among low-income adults after Medicaid expansion or expanded private insurance. JAMA Intern Med 2016;176:1501–1509 [DOI] [PubMed] [Google Scholar]
- 15.Lee J, Callaghan T, Ory M, Zhao H, Bolin JN. The impact of Medicaid expansion on diabetes management. Diabetes Care 2020;43:1094–1101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Casagrande SS, McEwen LN, Herman WH. Changes in health insurance coverage under the affordable care act: a national sample of U.S. adults with diabetes, 2009 and 2016. Diabetes Care 2018;41:956–962 [DOI] [PubMed] [Google Scholar]
- 17.Huguet N, Springer R, Marino M, et al.. The impact of the Affordable Care Act (ACA) Medicaid expansion on visit rates for diabetes in safety net health centers. J Am Board Fam Med 2018;31:905–916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cole MB, Galárraga O, Wilson IB, Wright B, Trivedi AN. At federally funded health centers, Medicaid expansion was associated with improved quality of care. Health Aff (Millwood) 2017;36:40–48 [DOI] [PubMed] [Google Scholar]
- 19.Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol 2000;55:469–480 [PubMed] [Google Scholar]
- 20.Garvey KC, Markowitz JT, Laffel LMB. Transition to adult care for youth with type 1 diabetes. Curr Diab Rep 2012;12:533–541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bryden KS, Dunger DB, Mayou RA, Peveler RC, Neil HA. Poor prognosis of young adults with type 1 diabetes: a longitudinal study. Diabetes Care 2003;26:1052–1057 [DOI] [PubMed] [Google Scholar]
- 22.Copeland KC, Zeitler P, Geffner M, et al.; TODAY Study Group . Characteristics of adolescents and youth with recent-onset type 2 diabetes: the TODAY cohort at baseline. J Clin Endocrinol Metab 2011;96:159–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zeitler P, Epstein L, Grey M, et al.; TODAY Study Group . Treatment options for type 2 diabetes in adolescents and youth: a study of the comparative efficacy of metformin alone or in combination with rosiglitazone or lifestyle intervention in adolescents with type 2 diabetes. Pediatr Diabetes 2007;8:74–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kaiser Family Foundation Status of State Medicaid Expansion Decisions and Interactive Map, 2020. Accessed 26 November 2019. Available from https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/
- 25.U.S. Census Bureau Uninsured Rate by Single Year of Age: 2013, 2016, and 2017, 2018. Accessed 9 January 2020. Available from https://www.census.gov/content/dam/Census/library/visualizations/2018/demo/p60-264/figure4.pdf
- 26.Agarwal S, Raymond JK, Isom S, et al.. Transfer from paediatric to adult care for young adults with type 2 diabetes: the SEARCH for Diabetes in Youth Study. Diabet Med 2018;35:504–512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klingensmith GJ, Cheng P, Gal RL, et al. (1336-P): Healthcare utilization in T2D youth in the Pediatric Diabetes Consortium. Poster presented at the Annual Meeting of the American Diabetes Association, 10 June 2019, San Francisco, CA.
- 28.Petitti DB, Klingensmith GJ, Bell RA, et al.; SEARCH for Diabetes in Youth Study Group. Glycemic control in youth with diabetes: the SEARCH for Diabetes in Youth Study. J Pediatr 2009;155:668–672.e1-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Menke A, Knowler WC, Cowie CC. Physical and metabolic characteristics of persons with diabetes and prediabetes. In Diabetes in America, 3rd ed. Cowie CC, Casagrande SS, Menke A, et al., Eds. Bethesda, MD, National Institutes of Health, 2018, Appendix 9.1 (NIH Publ. no. 17–1468) [PubMed] [Google Scholar]
- 30.Centers for Disease Control and Prevention National Diabetes Statistics Report, 2017. Atlanta, GA, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services, 2017, pp. 8. Accessed 25 August 2019. Available from https://www.cdc.gov/diabetes/pdfs/data/statistics/national-diabetes-statistics-report.pdf [Google Scholar]
- 31.Songer TJ, Haymond MW, Glazner JE, et al.; TODAY Study Group . Healthcare and associated costs related to type 2 diabetes in youth and adolescence: the TODAY clinical trial experience. Pediatr Diabetes 2019;20:702–711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Weinstock RS, Braffett BH, McGuigan P, et al.; TODAY Study Group . Self-monitoring of blood glucose in youth-onset type 2 diabetes: results from the TODAY study. Diabetes Care 2019;42:903–909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davern M, Klerman JA, Baugh DK, Call KT, Greenberg GD. An examination of the Medicaid undercount in the current population survey: preliminary results from record linking. Health Serv Res 2009;44:965–987 [DOI] [PMC free article] [PubMed] [Google Scholar]