Chronic conditions such as diabetes have been implicated as risk factors for poor prognosis in hospitalized patients with coronavirus disease 2019 (COVID-19), the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (1–3). A 19 June 2020 report from the Centers for Disease Control and Prevention (CDC) found a significant burden of chronic conditions in reported cases of laboratory-confirmed COVID-19 (4). Most case subjects identified from the CDC COVID-19 surveillance reporting were not hospitalized. The current study compares the prevalence of comorbid conditions in the CDC report to population-representative data. Our objective was to examine the extent to which the prevalence of underlying conditions in patients with laboratory-confirmed COVID-19 exceeded what would be expected in similarly aged adults in the general U.S. population.
We estimated the prevalence of four conditions—diabetes, cardiovascular disease, chronic kidney disease, and chronic obstructive pulmonary disease (COPD)—in the general U.S. adult population (aged ≥20 years) using the most recent National Health and Nutrition Examination Survey (NHANES) cycle (2017–2018, n = 4,757). We compared these estimates to those reported among patients with laboratory-confirmed COVID-19 in the CDC’s June 2020 report.
We used definitions of comorbidities designed to most closely approximate those used in the CDC report. We defined cardiovascular disease as a self-reported history of coronary heart disease, heart failure, heart attack, stroke, or hypertension (mean blood pressure ≥130/≥80 mmHg or use of antihypertensive medication), consistent with the combined definition used in the CDC case reporting form. We defined chronic kidney disease as an estimated glomerular filtration rate <60 mL/min/1.73 m2 or albumin-to-creatinine ratio ≥30 mg/g. Diabetes was defined as a prior diagnosis or calibrated HbA1c ≥6.5%. We defined COPD based on a prior diagnosis.
We applied sample weights to generate estimates representative of the U.S. civilian noninstitutionalized population, overall and stratified by age. All analyses were conducted using Stata 15.1 (StataCorp).
Compared with adults in the 2017–2018 general population, those with laboratory-confirmed COVID-19 had a higher prevalence of diabetes (31.2% vs. 12.7%) and COPD (17.5% vs. 4.6%) but a lower prevalence of cardiovascular disease (52.9% vs. 33.3%) or chronic kidney disease (15.6% vs. 7.9%) (Fig. 1). Differences were more pronounced at older ages, except for COPD.
Figure 1.
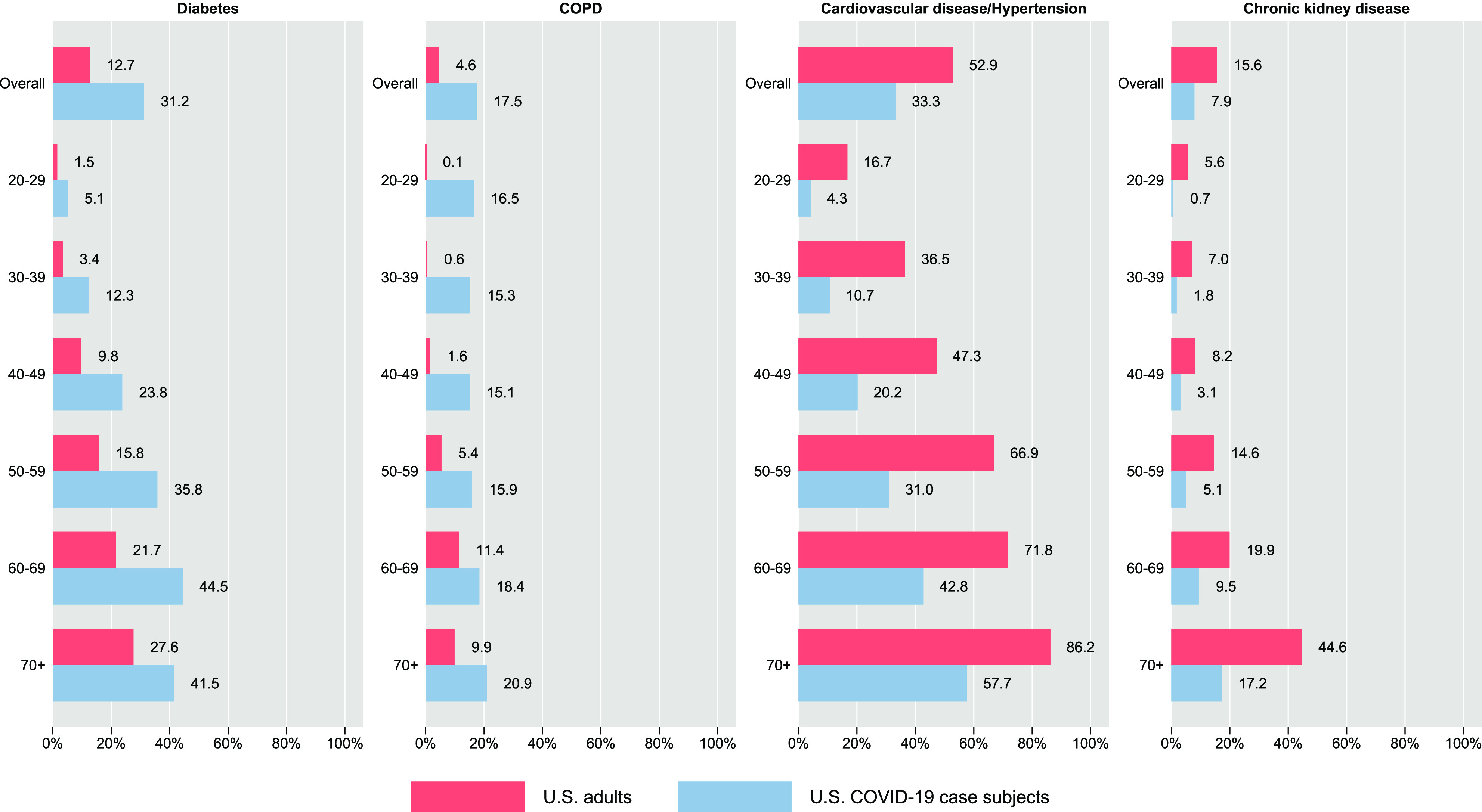
Prevalence of underlying conditions among U.S. adults with and without COVID-19, overall and by age. Estimates for U.S. adults came from the 2017–2018 NHANES. Estimates for COVID-19 case subjects were calculated from CDC’s notifiable disease surveillance COVID-19 case reporting, as reported in Stokes et al. (4). Diabetes was defined as prior diagnosis or calibrated HbA1c ≥6.5% in the NHANES and as diabetes on the CDC’s COVID-19 case report form. COPD was defined as a prior diagnosis in the NHANES and as chronic lung disease on the CDC’s COVID-19 case report form. Cardiovascular disease was defined as self-reported history of coronary heart disease, heart failure, heart attack, stroke, or hypertension (mean blood pressure ≥130/≥80 mmHg or use of antihypertensive medication) in the NHANES and as hypertension or cardiovascular disease on the CDC’s COVID-19 case report form. Chronic kidney disease was defined as an estimated glomerular filtration rate <60 mL/min/1.73 m2 or an albumin-to-creatinine ratio ≥30 mg/g in the NHANES and as chronic renal disease on the CDC’s COVID-19 case report form.
Our findings are consistent with prior research suggesting that diabetes is more common among those with COVID-19 (1–3). The high prevalence of diabetes in laboratory-confirmed case subjects supports diabetes as a risk factor for infection and/or diagnosis of COVID-19 (5). However, it is unknown whether diabetes contributes to risk of infection or whether individuals with diabetes are simply more likely to be diagnosed. Our data are also consistent with research linking respiratory illnesses with COVID-19 (1–3). We found that COPD may be an especially important risk factor for COVID-19 in younger adults. The CDC report found that having any underlying condition was associated with higher risk of hospitalization and death, but age differences were not accounted for and outcomes for diabetes or the other individual health conditions were not presented separately.
Prior reports have implicated cardiovascular disease, hypertension, and chronic kidney disease as risk factors for acute respiratory distress and mortality in persons hospitalized with COVID-19 (1–3). In contrast, we found that the prevalence of cardiovascular disease/hypertension and chronic kidney disease was lower in laboratory-confirmed COVID-19 case subjects compared with the general population. This suggests that these conditions may be risk factors for poor prognosis in COVID-19 but not risk factors for COVID-19 infection.
Several issues are important in the interpretation of these data. Approximately 78% of patients in the CDC report had missing information on underlying comorbidities, potentially leading to underreporting of chronic conditions among COVID-19 case subjects. Individuals who were infected but not diagnosed and those with confirmed diagnoses but not reported to CDC are also missing from the report. Diagnostic bias is another concern. Symptomatic individuals and those with certain underlying conditions may be more likely to be tested for SARS-CoV-2. Our definitions of health conditions may also have differed from the CDC report.
In conclusion, we found that diabetes and COPD were more common in patients with laboratory-confirmed COVID-19 than in the general population in 2017–2018. It remains unclear whether diabetes and/or COPD are causal risk factors for infection with SARS-CoV-2 or whether these associations are confounded by underlying factors such as socioeconomic status or the likelihood of testing (5). Reliable data on comorbidities in COVID-19 are lacking, especially in nonhospitalized patients. Systematic surveys with rigorous data collection are needed to improve our understanding of the role of diabetes and other comorbidities as independent risk factors for COVID-19 and its prognosis.
Article Information
Funding. M.F. was supported by National Institutes of Health (NIH) National Heart, Lung, and Blood Institute grant T32 HL007024. O.T. was supported by NIH National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) grant F30 DK120160. E.S. was supported by NIH NIDDK grant K24 HL152440.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. M.F., O.T., and E.S. designed the study. D.W. conducted the statistical analysis. M.F., O.T., and E.S guided the statistical analysis and drafted the manuscript. O.T. and E.S. provided critical revisions to the manuscript. All authors approved the final manuscript. M.F. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
This article is part of a special article collection available at https://care.diabetesjournals.org/collection/diabetes-and-COVID19.
References
- 1.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus–infected pneumonia in Wuhan, China. JAMA 2020;323:1061–1069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guan WJ, Ni ZY, Hu Y, et al.; China Medical Treatment Expert Group for Covid-19 . Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020;382:1708–1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Evidence used to update the list of underlying medical conditions that increase a person’s risk of severe illness from COVID-19, 2020. Accessed 26 June 2020. Available from https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/evidence-table.html [PubMed]
- 4.Stokes EK, Zambrano LD, Anderson KN, et al. Coronavirus disease 2019 case surveillance - United States, January 22-May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69:759–765 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Selvin E, Juraschek SP. Diabetes epidemiology in the COVID-19 pandemic. Diabetes Care 2020;43:1690–1694 [DOI] [PMC free article] [PubMed] [Google Scholar]


