Abstract
OBJECTIVE
In patients with type 2 diabetes uncontrolled with metformin, exenatide once weekly (QW) plus dapagliflozin produced greater reductions in glycemic parameters (glycated hemoglobin [HbA1c], fasting plasma glucose [FPG], and 2-h postprandial glucose [2-h PPG]), weight, and systolic blood pressure (SBP) than exenatide QW or dapagliflozin alone after 28 weeks of treatment in DURATION-8. Following a 24-week extension period, improvements were sustained at 52 weeks. In this study, we investigated efficacy and safety at 104 weeks after randomization.
RESEARCH DESIGN AND METHODS
DURATION-8 was a 104-week, multicenter, double-blind, randomized, active-controlled, phase 3 trial. In total, 695 adults (aged ≥18 years) with type 2 diabetes and inadequate glycemic control (HbA1c 8.0–12.0% [64–108 mmol/mol]) despite stable metformin monotherapy (≥1,500 mg/day) were randomly assigned (1:1:1) to receive exenatide 2 mg QW plus once-daily dapagliflozin 10 mg, exenatide QW plus placebo, or dapagliflozin plus placebo. All 104-week evaluations were exploratory.
RESULTS
At week 104, 431 (62.0%) patients completed treatment. The adjusted least squares mean change (SE) from baseline to week 104 in HbA1c was greater with exenatide QW plus dapagliflozin (−1.70% [0.11]) versus exenatide QW plus placebo (−1.29% [0.12]; P = 0.007) and dapagliflozin plus placebo (−1.06% [0.12]; P < 0.001). Clinically relevant changes in FPG, 2-h PPG, weight, and SBP were also observed with exenatide QW plus dapagliflozin. There were no unexpected safety findings, and exenatide QW plus dapagliflozin was well tolerated, with no episodes of major hypoglycemia.
CONCLUSIONS
In this exploratory analysis, among those individuals who completed the trial without rescue therapy, there was clinically relevant efficacy over 2 years with exenatide QW plus dapagliflozin, with no unexpected safety findings.
Introduction
Most patients with type 2 diabetes require multiple glucose-lowering agents over time, with initial combination therapy recommended for patients with newly diagnosed type 2 diabetes who have glycated hemoglobin (HbA1c) ≥1.5% (12.5 mmol/mol) above their glycemic target (1). Two of the most recent classes of diabetes drugs are the glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium–glucose cotransporter-2 (SGLT2) inhibitors (1,2). Both have beneficial effects on glycemic control and traditional cardiovascular (CV) risk factors (e.g., body weight, systolic blood pressure [SBP], and lipid profile), improving CV and renal outcomes with low rates of hypoglycemia in patients with type 2 diabetes (2–4). GLP-1RAs and SGLT2 inhibitors impact glucose metabolism differently: GLP-1 receptor stimulation increases insulin secretion and decreases glucagon secretion, which slows gastric emptying and increases satiety (2); SGLT2 inhibition increases urinary glucose excretion (2). To produce sustained weight loss, GLP-1RAs decrease food intake through a reduction in appetite, and SGLT2 inhibitors increase calorie excretion (2).
DURATION-8, a multicenter, double-blind, randomized, active-controlled, phase 3 trial, was the first to analyze the efficacy of GLP-1RA (exenatide once weekly [QW]) plus an SGLT2 inhibitor (dapagliflozin administered orally once daily) simultaneously added to stable metformin monotherapy in 695 patients with type 2 diabetes and poor glycemic control (5). At 28 weeks, treatment with exenatide QW plus dapagliflozin, versus each drug alone, achieved significant improvements in glycemic control (HbA1c, fasting plasma glucose [FPG], and 2-h postprandial glucose [2-h PPG]), body weight, and SBP, with no unexpected safety findings (5). A 24-week, double-blind extension period confirmed sustained efficacy and safety at 52 weeks (6).
As the insulin secretory capacity of patients with type 2 diabetes diminishes over time, it is important that treatment effects are durable (1,7). The long-term efficacy and safety of exenatide QW and dapagliflozin has been demonstrated in patients with type 2 diabetes over 7 and 4 years, respectively (7–9). However, whether the improvements seen in DURATION-8 with exenatide QW plus dapagliflozin combination therapy at 28 and 52 weeks are maintained over a longer treatment period remains unknown (5,6). In this study, we report the results of a 52-week, second extension period of DURATION-8, designed to evaluate the long-term efficacy and safety of exenatide QW plus dapagliflozin over 104 weeks of randomized treatment in patients with type 2 diabetes.
Research Design and Methods
Study Design and Participants
The design and procedures of DURATION-8 have been published in detail previously (5,6). In brief, the study enrolled adults aged ≥18 years with type 2 diabetes and poor glycemic control (HbA1c 8.0–12.0% [64–108 mmol/mol]) despite stable metformin monotherapy at ≥1,500 mg/day for at least 2 months prior to screening. Patients were excluded if they had received any glucose-lowering drugs other than metformin for >14 days in the 12 weeks prior to enrollment and had a creatinine clearance of <60 mL/min or serum creatinine of ≥133 μmol/L (≥1.5 mg/dL) for men and ≥124 μmol/L (≥1.4 mg/dL) for women. A complete list of inclusion and exclusion criteria has been previously described (5).
Eligible patients were randomized (1:1:1) to receive exenatide 2 mg QW by subcutaneous injection plus dapagliflozin 10 mg oral tablets daily, exenatide 2 mg QW plus dapagliflozin-matched oral placebo daily, or dapagliflozin 10 mg daily plus exenatide QW–matched placebo injections. After the 24-week first extension period (6), participants continued to the 52-week second extension period in which randomized treatment was continued to week 104, followed by a 10-week follow-up period (Supplementary Fig. 1). The second extension phase was added as a protocol amendment while the study was ongoing. Patients with inadequate glycemic control remained in the study and received open-label rescue therapy with basal insulin based on progressively stricter FPG criteria from weeks 8 to 36 and on progressively stricter HbA1c criteria after week 36 (Supplementary Table 1). The study protocol was approved by the institutional review board and ethics committee at each site, and the study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines. All patients provided written informed consent prior to any study procedure.
Outcomes
The primary end point was change in HbA1c from baseline to week 28, which has been previously reported (5). All analyses at week 104 were exploratory, and end points included the change from baseline to week 104 in glycemic parameters (HbA1c, proportion of patients achieving HbA1c <7.0% [<53 mmol/mol], FPG, 2-h PPG following a standardized liquid meal test, and the six-point self-monitored blood glucose [SMBG] profile). The proportion of patients rescued or discontinued due to lack of glycemic control over 104 weeks was recorded. The change from baseline to week 104 in selected CV risk factors was also assessed, including body weight (plus proportion of patients with weight loss ≥5%), SBP, diastolic blood pressure (DBP), waist circumference, and fasting lipids (total cholesterol, LDL cholesterol, HDL cholesterol, non-HDL cholesterol, and triglycerides). As previously described (5,6), safety was assessed by adverse events (AEs), laboratory tests (anti-exenatide antibodies, urinalysis, hematocrit, and estimated glomerular filtration rate [eGFR]), and vital signs (e.g., heart rate [HR]) (5,6). Potential CV and hepatic AEs were adjudicated. Hypoglycemic events were classified as major, minor, or “other” (i.e., events not meeting the major or minor hypoglycemia criteria) (Supplementary Table 2).
Statistical Analysis
All efficacy variables were assessed in the intention-to-treat (ITT) population, defined as all randomly assigned patients who received at least one dose of the study drug with at least one postbaseline HbA1c assessment. All end points at week 104 were exploratory and not adjusted for multiple comparisons; therefore, all P values were nominal. Changes in continuous variables (HbA1c, FPG, body weight, SBP, and DBP) were analyzed with a mixed-effects model for repeated measures; an ANCOVA model was used to analyze changes in 2-h PPG, SMBG, waist circumference, and fasting lipids. Categorical variables were analyzed using stratified Cochran-Mantel-Haenszel tests, with missing 104-week data for the categorical variables imputed by the last observation carried forward method. All safety variables were analyzed in the safety analysis set, defined as all randomly assigned patients who received at least one dose of the study drug, and were summarized descriptively. Data collected after the initiation of glycemic rescue therapy or at the posttreatment follow-up visits after premature treatment discontinuation were excluded from the efficacy analyses, except for SBP, which included data after rescue and excluded data after treatment discontinuation. All analyses were conducted using SAS version 9.2 or higher (SAS Institute Inc., Cary, NC). This trial is registered with ClinicalTrials.gov as NCT02229396.
Data and Resource Availability
Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data-sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure.
Results
Of the 695 patients randomized, 694 (99.9%) received treatment, and 431 (62.0%) completed the 104-week treatment period; 263 (37.8%) patients discontinued treatment, the most common reason being patient withdrawal (Supplementary Fig. 2). A majority of patient withdrawals were due to a protocol amendment to lengthen the study by 1 year after the end of the first 52 weeks of treatment, which required patients to resign their consent forms. Adherence to treatment was high, with a mean 94–100% of dispensed medication used. Baseline demographics and clinical characteristics were balanced between treatment groups (Table 1).
Table 1.
Baseline demographics and clinical characteristics (ITT population)
| Exenatide QW plus dapagliflozin (n = 228) | Exenatide QW plus placebo (n = 227) | Dapagliflozin plus placebo (n = 230) | |
|---|---|---|---|
| Age, mean (SD), years | 53.8 (9.82) | 54.2 (9.62) | 54.5 (9.16) |
| Male, n (%) | 102 (44.7) | 116 (51.1) | 110 (47.8) |
| Race, n (%) | |||
| White | 190 (83.3) | 194 (85.5) | 189 (82.2) |
| Black | 34 (14.9) | 27 (11.9) | 33 (14.3) |
| Asian | 3 (1.3) | 1 (0.4) | 1 (0.4) |
| Other | 1 (0.4) | 5 (2.2) | 7 (3.0) |
| Hispanic or Latino ethnicity, n (%) | 95 (41.7) | 91 (40.1) | 85 (37.0) |
| Weight, mean (SD), kg | 91.8 (22.2) | 89.8 (20.2) | 91.1 (19.7) |
| BMI, mean (SD), kg/m2 | 33.2 (6.8) | 32.0 (5.9) | 33.0 (6.1) |
| BMI group, n (%), kg/m2 | |||
| <25 | 17 (7.5) | 17 (7.5) | 15 (6.5) |
| ≥25 to <30 | 71 (31.1) | 78 (34.4) | 57 (24.8) |
| ≥30 | 140 (61.4) | 132 (58.1) | 158 (68.7) |
| HbA1c, mean (SD), % | 9.3 (1.1) | 9.30 (1.1) | 9.3 (1.0) |
| HbA1c, mean (SD), mmol/mol | 79 (11.7) | 78 (11.6) | 78 (11.3) |
| HbA1c group, n (%) | |||
| <8.0% (<64 mmol/mol) | 14 (6.1) | 13 (5.7) | 14 (6.1) |
| ≥8.0% to <9.0% (≥64 to <75 mmol/mol) | 84 (36.8) | 84 (37.0) | 88 (38.3) |
| ≥9.0% (≥75 mmol/mol) | 130 (57.0) | 130 (57.3) | 128 (55.7) |
| Duration of type 2 diabetes, mean (SD), years | 7.6 (6.0) | 7.4 (5.5) | 7.1 (5.5) |
| FPG, mean (SD), mmol/L | 11.0 (3.0) | 10.7 (2.8) | 10.6 (2.6) |
| SBP, mean (SD), mmHg | 130.1 (12.7) | 129.1 (13.1) | 130.0 (12.9) |
| eGFR-MDRD, mean (SD), mL/min/1.73 m2 | 97.7 (23.7) | 99.4 (26.8) | 97.5 (24.0) |
| eGFR-MDRD group, n (%) | |||
| ≥30 to <60 mL/min/1.73 m2 | 6 (2.6) | 7 (3.1) | 12 (5.2) |
| ≥60 mL/min/1.73 m2 | 222 (97.4) | 220 (96.9) | 218 (94.8) |
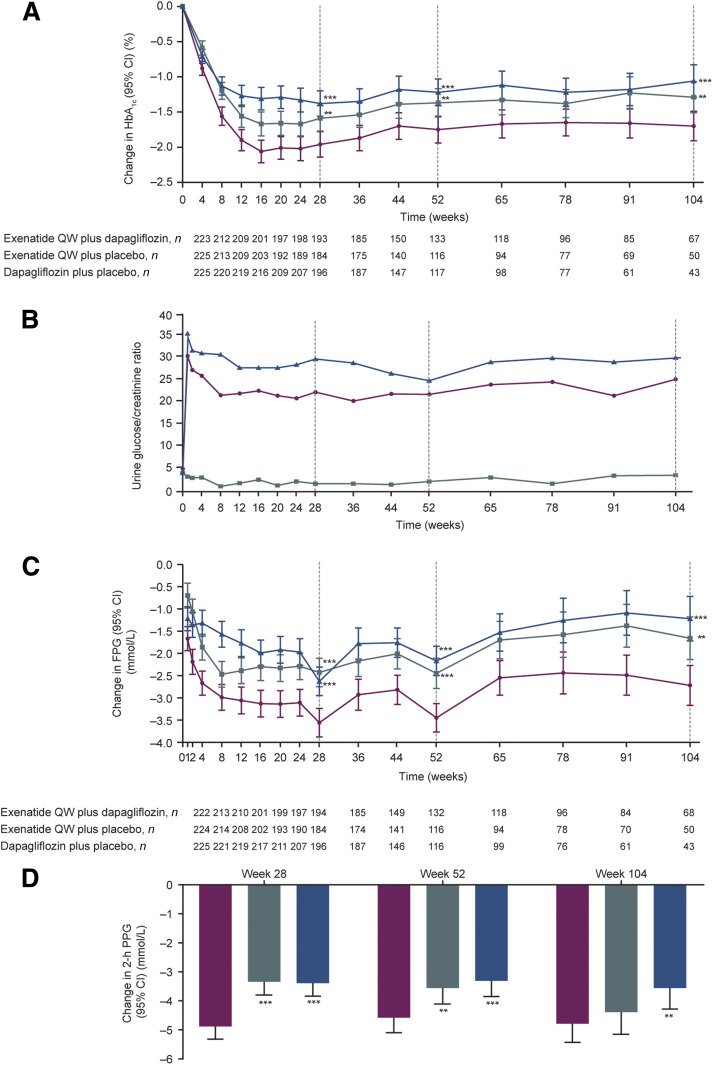
At week 28, the combination of exenatide QW plus dapagliflozin was superior to exenatide QW plus placebo or dapagliflozin plus placebo in reducing HbA1c (Fig. 1A). The differences between treatment groups were maintained at week 52 (Fig. 1A) and week 104 (Table 2 and Fig. 1A). At week 104, a numerically greater proportion of patients achieved HbA1c <7% (<53 mmol/mol) with exenatide QW plus dapagliflozin versus exenatide QW plus placebo or dapagliflozin plus placebo (Supplementary Fig. 3). The urinary glucose excretion, evaluated by the urinary glucose-to-creatinine ratio, observed at week 28 in the exenatide QW plus dapagliflozin and dapagliflozin plus placebo groups was maintained through week 104 (Fig. 1B). At week 28, exenatide QW plus dapagliflozin was superior to exenatide QW plus placebo or dapagliflozin plus placebo in reducing FPG (Fig. 1C); the differences between treatment groups were maintained at week 52 (Fig. 1C) and week 104 (Table 2 and Fig. 1C). At week 28, exenatide QW plus dapagliflozin was superior to exenatide QW plus placebo or dapagliflozin plus placebo in reducing 2-h PPG, and the differences between treatment groups were maintained at week 52 (Fig. 1D). At week 104, the difference in 2-h PPG between exenatide QW plus dapagliflozin and dapagliflozin plus placebo was maintained, and the difference in 2-h PPG between exenatide QW plus dapagliflozin and exenatide QW plus placebo was attenuated (Fig. 1D and Table 2). Reductions in mean daily SMBG were numerically greater with exenatide QW plus dapagliflozin versus exenatide QW plus placebo and dapagliflozin plus placebo (Supplementary Table 3).
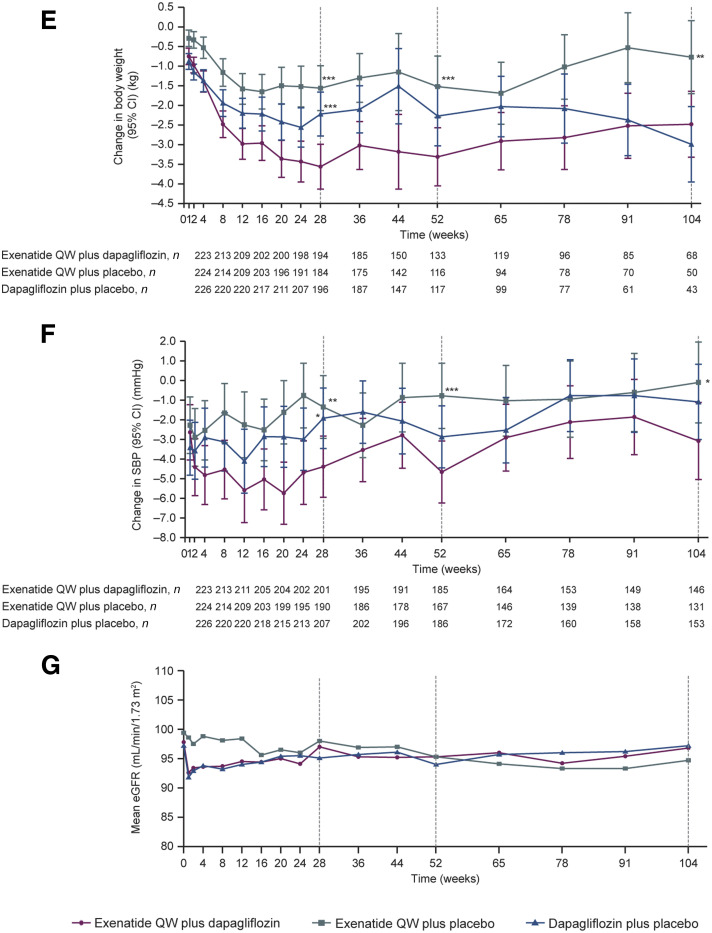
Figure 1.
Adjusted least squares mean (LSM) change in HbA1c (A), mean urine glucose/creatinine ratio (B), adjusted LSM change in FPG (C), adjusted LSM change in 2-h PPG (D), adjusted LSM change in body weight (E), adjusted LSM change in SBP (F), and mean eGFR (G) over 104 weeks of treatment. Error bars show 95% CIs. *P < 0.05, **P < 0.01, ***P < 0.001 vs. exenatide QW plus dapagliflozin (P values at weeks 52 and 104 are nominal).
Table 2.
Efficacy end points
| Between-group difference (95% CI) | |||||
|---|---|---|---|---|---|
| Exenatide QW plus dapagliflozin (n = 228) | Exenatide QW plus placebo (n = 227) | Dapagliflozin plus placebo (n = 230) | Exenatide QW plus dapagliflozin vs. exenatide QW plus placebo | Exenatide QW plus dapagliflozin vs. dapagliflozin plus placebo | |
| Glycemic outcomes | |||||
| HbA1c, % | |||||
| Baseline | 8.92 (0.98) | 8.97 (1.04) | 8.76 (0.91) | ||
| Week 104 | 6.55 (0.52) | 6.68 (0.65) | 7.07 (1.04) | ||
| Change at week 104 | −1.70 (0.11) | −1.29 (0.12) | −1.06 (0.12) | −0.42 (−0.72 to −0.12); P = 0.007 | −0.64 (−0.94 to −0.34); P < 0.001 |
| FPG, mmol/L | |||||
| Baseline | 9.95 (2.20) | 9.47 (2.20) | 9.65 (2.30) | ||
| Week 104 | 6.61 (1.43) | 7.01 (1.58) | 7.75 (1.79) | ||
| Change at week 104 | −2.72 (0.23) | −1.66 (0.25) | −1.22 (0.26) | −1.07 (−1.71 to −0.42); P = 0.001 | −1.50 (−2.16 to −0.85); P < 0.001 |
| 2-h PPG, mmol/L | |||||
| Baseline | 14.45 (3.45) | 13.91 (3.65) | 13.87 (3.50) | ||
| Week 104 | 9.94 (2.59) | 10.46 (3.03) | 11.06 (3.29) | ||
| Change at week 104 | −4.79 (0.33) | −4.39 (0.39) | −3.56 (0.37) | −0.40 (−1.26 to 0.46); P = 0.360 | −1.23 (−2.10 to −0.36); P = 0.006 |
| CV risk factors | |||||
| Body weight, kg | |||||
| Baseline | 94.97 (22.18) | 90.20 (17.77) | 92.09 (14.96) | ||
| Week 104 | 91.15 (20.74) | 88.35 (16.90) | 87.82 (13.15) | ||
| Change at week 104 | −2.48 (0.43) | −0.77 (0.47) | −2.99 (0.49) | −1.71 (−2.95 to −0.47); P = 0.007 | 0.50 (−0.77 to 1.77); P = 0.436 |
| SBP, mmHg | |||||
| Baseline | 131.2 (12.64) | 130.6 (12.04) | 130.3 (12.83) | ||
| Week 104 | 128.5 (12.90) | 131.5 (13.60) | 130.0 (13.37) | ||
| Change at week 104 | −3.1 (1.00) | −0.1 (1.05) | −1.1 (0.98) | −3.0 (−5.7 to −0.2); P = 0.034 | −2.0 (−4.6 to 0.7); P = 0.142 |
Baseline and week 104 data are mean (SD) and reported for patients with observed baseline and week 104 values. Change at week 104 data are adjusted least squares mean (SE), and between-group difference data are least squares mean (95% CI) in the ITT population. Analysis excluded measurements post–rescue therapy and post–premature discontinuation of the study medication, apart from SBP, which included measurements after rescue and excluded measurements post–premature discontinuation of the study medication.
Rescue rates increased at weeks 36, 65, and 91 due to the changes in rescue criteria (Supplementary Fig. 4), which became stricter with study progression. Between baseline and week 28, low numbers of patients received rescue therapy, with similar rescue rates across the treatment groups through week 24 (Supplementary Fig. 4). After week 24, a greater proportion of patients in the dapagliflozin plus placebo group received rescue therapy versus the exenatide QW plus dapagliflozin and exenatide QW plus placebo groups (Supplementary Fig. 4). After week 52, a greater proportion of patients in the exenatide QW plus placebo group received rescue therapy versus the exenatide QW plus dapagliflozin group (Supplementary Fig. 4).
At week 28, exenatide QW plus dapagliflozin was superior to exenatide QW plus placebo and dapagliflozin plus placebo in reducing body weight, and the differences between treatment groups were maintained at week 52 (Fig. 1E). The difference between exenatide QW plus dapagliflozin and exenatide QW plus placebo, but not dapagliflozin plus placebo, was maintained at week 104 (Table 2 and Fig. 1E). A similar trend was observed for the percentage of patients with weight loss ≥5% (Supplementary Fig. 3). Between weeks 91 and 104, there was an additional decrease in body weight in the dapagliflozin plus placebo group, resulting in a numerically greater weight loss at week 104 with dapagliflozin plus placebo versus exenatide QW plus dapagliflozin (Table 2 and Fig. 1E).
At week 28, exenatide QW plus dapagliflozin was superior to exenatide QW plus placebo or dapagliflozin plus placebo in reducing SBP (Fig. 1F). The differences between treatment groups were maintained at 52 weeks (Fig. 1F) and 104 weeks (Table 2 and Fig. 1F). Similar to weeks 28 and 52 (5,6), no clinically relevant differences between treatment groups were observed at week 104 for changes in DBP (Supplementary Table 3) and waist circumference (data not shown). Total cholesterol, LDL cholesterol, and non-HDL cholesterol increased in the exenatide QW plus dapagliflozin and dapagliflozin plus placebo groups to a greater extent at week 104 than at weeks 28 and 52 (5,6) (Supplementary Table 3). In the exenatide QW plus placebo group, non-HDL cholesterol slightly decreased at week 104, and there were no relevant changes in total cholesterol or LDL cholesterol (Supplementary Table 3). There were no relevant changes in HDL cholesterol in any treatment group (Supplementary Table 3). Whereas at week 28, there was a decrease in mean triglycerides in all three treatment groups (5), at week 104, there was no change in the mean triglycerides in the exenatide QW plus dapagliflozin group, a decrease in the exenatide QW plus placebo group, and an increase in the dapagliflozin plus placebo group (Supplementary Table 3).
Exenatide QW plus dapagliflozin was well tolerated over 104 weeks, with similar proportions of AEs and serious AEs across all treatment groups (Table 3). Six (0.9%) patients died during the 104-week treatment period (Table 3). Five of these deaths occurred during the initial 28-week treatment period and have been previously described (5). One death (hyperglycemia) occurred in the dapagliflozin plus placebo group after week 52, which was not associated with ketoacidosis and judged as unrelated to the study drugs. The most commonly reported AEs (frequency ≥5.0%) by preferred term during the 104-week treatment period were upper respiratory tract infections, urinary tract infections, nausea, injection-site nodules, diarrhea, headaches, nasopharyngitis, and vomiting (Table 3). Gastrointestinal AEs were more frequent in the exenatide-treated groups, whereas genital infections were more frequent in the dapagliflozin plus placebo treatment group (Table 3). At week 104, four (1.7%) patients in each treatment group had experienced an adjudicated CV event; two events (hemorrhagic stroke and ischemic stroke) occurred during the second extension period and were considered unrelated to the study drugs. There were two adjudicated hepatic events reported (one patient each in the exenatide QW plus placebo and dapagliflozin plus placebo groups, respectively [Table 3]). Both hepatic events occurred during the initial 28-week treatment period, have been previously described (5), and were adjudicated as unlikely to be causally related to the study drugs. Marked abnormalities of hematocrit were rare (Table 3). The mean eGFR initially decreased in the dapagliflozin-treated groups, recovering to baseline levels by week 104 (Fig. 1G). One (<1%) patient in the exenatide QW plus placebo group, but no patients in the other treatment groups, had diabetic ketoacidosis (5). There was a slight increase in HR at week 104 in the exenatide QW plus dapagliflozin group (0.6 beats per minute [bpm]) and the exenatide QW plus placebo group (1.4 bpm). The change in HR in the dapagliflozin plus placebo group was 0.1 bpm.
Table 3.
Number of patients with AEs in the safety analysis set
| Exenatide QW plus dapagliflozin (n = 231) | Exenatide QW plus placebo (n = 230) | Dapagliflozin plus placebo (n = 233) | |
|---|---|---|---|
| Any AE | 165 (71.4) | 161 (70.0) | 156 (67.0) |
| Any SAE | 17 (7.4) | 18 (7.8) | 18 (7.7) |
| Any AE with outcome of death | 3 (1.3) | 1 (0.4) | 2 (0.9) |
| AEs leading to discontinuation of study treatment | 16 (6.9) | 14 (6.1) | 12 (5.2) |
| AEs leading to study withdrawal | 15 (6.5) | 10 (4.3) | 8 (3.4) |
| AEs occurring in ≥5% of patients | |||
| Upper respiratory tract infection | 15 (6.5) | 17 (7.4) | 22 (9.4) |
| Urinary tract infection | 19 (8.2) | 15 (6.5) | 16 (6.9) |
| Nausea | 13 (5.6) | 26 (11.3) | 10 (4.3) |
| Injection-site nodule | 20 (8.7) | 14 (6.1) | 13 (5.6) |
| Diarrhea | 13 (5.6) | 17 (7.4) | 11 (4.7) |
| Headache | 16 (6.9) | 12 (5.2) | 12 (5.2) |
| Nasopharyngitis | 15 (6.5) | 8 (3.5) | 12 (5.2) |
| Vomiting | 8 (3.5) | 12 (5.2) | 7 (3.0) |
| Genital infection AEs | |||
| Any genital infection | 12 (5.2) | 5 (2.2) | 18 (7.7) |
| AEs of special interest | |||
| Gastrointestinal AEs | 48 (20.8) | 55 (23.9) | 38 (16.3) |
| Volume depletion–related AEs | 3 (1.3) | 1 (0.4) | 5 (2.1) |
| Hematocrit >55% | 5 (2.2) | 2 (0.9) | 5 (2.1) |
| Pancreatitis-related AEs | 3 (1.3) | 1 (0.4) | 0 |
| Pancreatic carcinoma–related AEs | 1 (0.4) | 0 | 0 |
| Acute renal failure–related AEs | 0 | 2 (0.9) | 3 (1.3) |
| Adjudicated CV AEs | 4 (1.7) | 4 (1.7) | 4 (1.7) |
| Adjudicated hepatic AEs | 0 | 1 (0.4) | 1 (0.4) |
| Injection-site–related AEs | 32 (13.9) | 27 (11.7) | 18 (7.7) |
| Thyroid neoplasm–related AEs | 0 | 0 | 0 |
| Hypoglycemia | 16 (6.9) | 8 (3.5) | 9 (3.9) |
| Major | 0 | 0 | 0 |
| Minor | 4 (1.7) | 0 | 1 (0.4) |
| Other | 16 (6.9) | 8 (3.5) | 8 (3.4) |
| Anti-exenatide antibodies | |||
| Week 104 | 43 (29.5) | 34 (26.0) | — |
| Injection-site–related AEs by anti-exenatide antibody levels | |||
| Negative | 3 (1.3) | 3 (1.3) | — |
| High positive (≥625) | 18 (7.8) | 10 (4.3) | — |
| Low positive (<625) | 11 (4.8) | 14 (6.1) | — |
| Any positive | 29 (12.6) | 24 (10.4) | — |
Data are n (%). AEs occurring in ≥5% of patients are listed by Medical Dictionary for Regulatory Activities–preferred (MedDRA version 20.1) term; preferred terms for remaining AE categories are not listed. SAE, serious AE.
In both exenatide QW treatment groups, the mean percentage of patients positive for anti-exenatide antibodies peaked at week 12 (70.4% in both groups) and declined over 104 weeks; 43 (29.5%) and 34 (26.0%) patients in the exenatide QW plus dapagliflozin and exenatide QW plus placebo groups, respectively, developed anti-exenatide antibodies at week 104 (Table 3). Anti-exenatide antibody status was not observed to have a consistent impact on HbA1c. At weeks 28 and 52, injection-site–related AEs were more common among patients with any positive anti-exenatide antibodies (5,6), and this was also observed at week 104 (Table 3).
No episodes of major hypoglycemia were reported. Episodes of minor hypoglycemia occurred in four (1.7%) patients in the exenatide QW plus dapagliflozin group and one (0.4%) patient in the dapagliflozin plus placebo group; no minor hypoglycemia events occurred in the exenatide QW plus placebo group (Table 3). At week 104, more patients in the exenatide QW plus dapagliflozin group had episodes of other hypoglycemia (16 [6.9%] patients) versus the exenatide QW plus placebo and dapagliflozin plus placebo groups (8 [3.5%] and 8 [3.4%] patients, respectively) (Table 3).
Conclusions
The ultimate goals of type 2 diabetes treatment are to prevent the development or progression of acute and chronic complications and to maintain patients’ quality of life (1,10). GLP-1RA plus SGLT2 inhibitor combination therapy is of clinical interest due to their complementary mechanisms of action and positive clinical outcomes (2–6,11). For patients with type 2 diabetes with established atherosclerotic CV disease who do not achieve target HbA1c with metformin plus lifestyle intervention, current treatment guidelines recommend the addition of a GLP-1RA or an SGLT2 inhibitor with proven CV benefit (1). If HbA1c remains above target after ∼3 months of dual therapy, intensification to triple therapy with the combination of a GLP-1RA, an SGLT2 inhibitor, and metformin is recommended (1).
In this study, we report—subject to the limitations mentioned above—that the exenatide QW plus dapagliflozin combination maintained clinically relevant efficacy and safety after 2 years of treatment in DURATION-8. At week 28, combination therapy with exenatide QW plus dapagliflozin resulted in greater HbA1c reductions than each drug alone (5), and these differences were maintained at week 104. Secondary end points, including mean change in FPG, 2-h PPG, body weight, and SBP, showed persistent clinically relevant efficacy over 104 weeks in the exenatide QW plus dapagliflozin group. Treatment differences observed at week 28 were maintained for some but not all secondary glycemic end points, partly due to the decrease in power resulting from increased premature discontinuation and rescue rates over time.
There were no unexpected safety findings over the 2 years of treatment, and the safety and tolerability profile of exenatide QW plus dapagliflozin was not different than expected based on the established safety profiles of the individual drugs (12,13). There were no episodes of major hypoglycemia over 104 weeks of treatment, and there were few events of minor and “other” hypoglycemia in the study; greater numbers of patients in the exenatide plus dapagliflozin group experienced an event of minor or “other” hypoglycemia compared with the exenatide plus placebo and dapagliflozin plus placebo groups.
The current long-term results of DURATION-8 add to the growing body of evidence that demonstrates the efficacy and safety of GLP-1RA plus SGLT2 inhibitor combination therapy and the durable effect of this combination (5,6,14–17). For instance, in obese patients without diabetes, exenatide QW plus dapagliflozin therapy reduced body weight, frequency of prediabetes, and SBP over 52 weeks (14). Although the 24-week study length was considerably shorter than the 2-year study reported in this article and had a different study design, the AWARD-10 study recently reported that dulaglutide plus SGLT2 inhibitor combination therapy resulted in significant and clinically relevant improvements in glycemic control, with acceptable safety in patients with type 2 diabetes (15). Similar results were recently reported by the 30-week SUSTAIN 9 study, showing the efficacy and safety of semaglutide add-on to previous SGLT2 inhibitor treatment (16). Additionally, a 52-week, open-label, phase 4 study in Japanese patients with type 2 diabetes and inadequate glycemic control demonstrated that the addition of canagliflozin to GLP-1RA therapy significantly reduced HbA1c, FPG, body weight, SBP, and HDL cholesterol (17).
Reduction in SBP with GLP-1RA plus SGLT2 inhibitor treatment has been attributed to the complementary mechanisms of action of both drug classes (2,11). In the current study, a durable treatment effect for the reduction of SBP was observed with the exenatide QW plus dapagliflozin combination over 104 weeks of treatment. However, the variability in SBP observed in all treatment groups over the 104 weeks of treatment should be considered and the results interpreted with caution. How SGLT2 inhibitors and GLP-1RAs work together from a volume and renal perspective requires further investigation and is being examined in a dedicated trial (DECADE; NTR6839), which aims to determine the albuminuria-lowering effect of exenatide QW plus dapagliflozin in patients with type 2 diabetes and microalbuminuria or macroalbuminuria.
A numerically greater body weight loss was observed in the dapagliflozin plus placebo group versus the exenatide QW plus dapagliflozin group from weeks 52 to 104, which could be attributed to increased variability arising from fewer patients remaining in the study after week 52; the low number of patients limits the interpretability of these data.
Strengths of the study include the double-blind, placebo-controlled design over a 2-year extended treatment period. Limitations include a relatively high rate of patient withdrawal observed after week 52, largely due to lengthening of the study by an additional year, which required reconsenting of patients; this loss of patients does decrease the robustness of the 2-year data. Patients who declined to resign the consent form extending study participation by 1 year were captured as “other” or “withdrawal by subject” in the electronic case report form. These were the two most common reasons for patient discontinuation. The reasons that some patients chose to not continue in the study are unclear. Though unwillingness to continue another year was not specifically captured in the electronic case report form, we had indications from the sites that many withdrew for this reason; the fact that the discontinuations occurred at the time of reconsenting also supports this point. Another limitation is that clinical relevance may be patient specific, and in that regard, individualized treatment may or may not involve combination therapy and could also be modified based on target and/or baseline HbA1c. Our claims of clinical efficacy should be interpreted in light of these factors. Additionally, analyses at 104 weeks were exploratory, with nominal P values calculated. DURATION-8 was designed to evaluate the simultaneous initiation of exenatide QW and dapagliflozin, but did not explore sequential intensification (i.e., the impact of adding exenatide to ongoing dapagliflozin plus metformin treatment or vice versa) as suggested by current treatment guidelines (1). Nevertheless, it may be that the dual add-on regimen has explored the worst-case scenario regarding the potential for AEs in the patient population.
In conclusion, in patients with type 2 diabetes who completed the trial without rescue therapy, clinically relevant efficacy was maintained over 2 years with the exenatide QW plus dapagliflozin combination, with no unexpected safety findings. Further studies are needed to investigate whether the combination treatment effects observed in DURATION-8 could potentially extend to a reduced incidence of CV and renal events in patients with type 2 diabetes.
Article Information
Acknowledgments. The authors thank Peter Öhman (AstraZeneca, Stockholm, Sweden) for the contributions to the study. The authors also thank the DURATION-8 trial team and the patients who participated in the study. Medical writing support, which was in accordance with Good Publication Practice guidelines (GPP3), was provided by Dr. Liam Gillies, Cactus Life Sciences (part of Cactus Communications, London, U.K.) and was funded by AstraZeneca.
Duality of Interest. This study was funded by AstraZeneca. AstraZeneca was involved in the study design and protocol development, provided logistical support, and obtained the data, which were evaluated jointly by the authors and the sponsor. E.H. and C.D.S. are employees and shareholders of AstraZeneca. C.G. has participated in scientific advisory boards and received consulting/lecturing fees from AstraZeneca, Boehringer Ingelheim, Egis Pharmaceuticals PLC, Eli Lilly and Company, Merck Sharp & Dohme, Novo Nordisk, and Sanofi. J.P.F. has received research support from AbbVie Inc., Allergan, AstraZeneca, Boehringer Ingelheim, Bristol-Myers Squibb, Cirius Therapeutics, CymaBay Therapeutics, Eli Lilly and Company, Genentech, Intercept Pharmaceuticals, Janssen, Johnson & Johnson, Lexicon Pharmaceuticals, Inc., Ligand Pharmaceuticals Incorporated, Madrigal Pharmaceuticals, Merck, Mylan, Novartis, Novo Nordisk, Pfizer, Sanofi, and Theracos, Inc.; and has received honoraria for consultancy and participation in advisory boards from AstraZeneca, Boehringer Ingelheim, Genentech, Gilead Sciences, Inc., Johnson & Johnson, Eli Lilly and Company, Merck, Novo Nordisk, and Sanofi. S.A.J. has received honoraria for consultancy from AstraZeneca, Eli Lilly and Company, and Janssen. A.A. has received research grants from AbbVie Inc., AstraZeneca, Kowa Pharmaceuticals America, Inc., Novo Nordisk, and Sanofi. J.C. was previously employed by AstraZeneca. No other potential conflicts of interest relevant to this article were reported.
Author Contributions. All authors contributed to the study and data interpretation, provided critical review, and edited and approved the manuscript for publication. All authors had full access to all of the data in the study and had the final responsibility of the decision to submit the manuscript for publication. S.A.J. is the guarantor of this work and, as such, had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Prior Presentation. Parts of this study were presented at the 78th Scientific Sessions of the American Diabetes Association, Orlando, FL, 22–26 June 2018, and at the 54th Annual Meeting of the European Association for the Study of Diabetes, Berlin, Germany, 1–5 October 2018.
Footnotes
Clinical trial reg. no. NCT02229396, clinicaltrials.gov
This article contains supplementary material online at https://doi.org/10.2337/figshare.12692078.
This article is featured in a podcast available at https://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.Davies MJ, D’Alessio DA, Fradkin J, et al. . Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2018;41:2669–2701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Busch RS, Kane MP. Combination SGLT2 inhibitor and GLP-1 receptor agonist therapy: a complementary approach to the treatment of type 2 diabetes. Postgrad Med 2017;129:686–697 [DOI] [PubMed] [Google Scholar]
- 3.Zelniker TA, Wiviott SD, Raz I, et al. . SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 2019;393:31–39 [DOI] [PubMed] [Google Scholar]
- 4.Kristensen SL, Rørth R, Jhund PS, et al. . Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials [published correction appears in Lancet Diabetes Endocrinol 2020;8:e2]. Lancet Diabetes Endocrinol 2019;7:776–785 [DOI] [PubMed] [Google Scholar]
- 5.Frías JP, Guja C, Hardy E, et al. . Exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy (DURATION-8): a 28 week, multicentre, double-blind, phase 3, randomised controlled trial. Lancet Diabetes Endocrinol 2016;4:1004–1016 [DOI] [PubMed] [Google Scholar]
- 6.Jabbour SA, Frías JP, Hardy E, et al. . Safety and efficacy of exenatide once weekly plus dapagliflozin once daily versus exenatide or dapagliflozin alone in patients with type 2 diabetes inadequately controlled with metformin monotherapy: 52-week results of the DURATION-8 randomized controlled trial. Diabetes Care 2018;41:2136–2146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jabbour S. Durability of response to dapagliflozin: a review of long-term efficacy and safety. Curr Med Res Opin 2017;33:1685–1696 [DOI] [PubMed] [Google Scholar]
- 8.Del Prato S, Nauck M, Durán-Garcia S, et al. . Long-term glycaemic response and tolerability of dapagliflozin versus a sulphonylurea as add-on therapy to metformin in patients with type 2 diabetes: 4-year data. Diabetes Obes Metab 2015;17:581–590 [DOI] [PubMed] [Google Scholar]
- 9.Philis-Tsimikas A, Wysham CH, Hardy E, Han J, Iqbal N. Efficacy and tolerability of exenatide once weekly over 7 years in patients with type 2 diabetes: an open-label extension of the DURATION-1 study. J Diabetes Complications 2019;33:223–230 [DOI] [PubMed] [Google Scholar]
- 10.Gæde P, Oellgaard J, Carstensen B, et al. . Years of life gained by multifactorial intervention in patients with type 2 diabetes mellitus and microalbuminuria: 21 years follow-up on the Steno-2 randomised trial. Diabetologia 2016;59:2298–2307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Block C. SGLT2 inhibitors and GLP-1 receptor agonists: a sound combination. Lancet Diabetes Endocrinol 2018;6:349–352 [DOI] [PubMed] [Google Scholar]
- 12.Genovese S, Mannucci E, Ceriello A. A review of the long-term efficacy, tolerability, and safety of exenatide once weekly for type 2 diabetes. Adv Ther 2017;34:1791–1814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jabbour S, Seufert J, Scheen A, Bailey CJ, Karup C, Langkilde AM. Dapagliflozin in patients with type 2 diabetes mellitus: a pooled analysis of safety data from phase IIb/III clinical trials. Diabetes Obes Metab 2018;20:620–628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lundkvist P, Pereira MJ, Katsogiannos P, Sjöström CD, Johnsson E, Eriksson JW. Dapagliflozin once daily plus exenatide once weekly in obese adults without diabetes: sustained reductions in body weight, glycaemia and blood pressure over 1 year. Diabetes Obes Metab 2017;19:1276–1288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ludvik B, Frías JP, Tinahones FJ, et al. . Dulaglutide as add-on therapy to SGLT2 inhibitors in patients with inadequately controlled type 2 diabetes (AWARD-10): a 24-week, randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 2018;6:370–381 [DOI] [PubMed] [Google Scholar]
- 16.Zinman B, Bhosekar V, Busch R, et al. . Semaglutide once weekly as add-on to SGLT-2 inhibitor therapy in type 2 diabetes (SUSTAIN 9): a randomised, placebo-controlled trial. Lancet Diabetes Endocrinol 2019;7:356–367 [DOI] [PubMed] [Google Scholar]
- 17.Harashima SI, Inagaki N, Kondo K, et al. . Efficacy and safety of canagliflozin as add-on therapy to a glucagon-like peptide-1 receptor agonist in Japanese patients with type 2 diabetes mellitus: a 52-week, open-label, phase IV study. Diabetes Obes Metab 2018;20:1770–1775 [DOI] [PMC free article] [PubMed] [Google Scholar]