Abstract
Objectives
There are limited public health data on urban American Indian/Alaska Native (AI/AN) populations, particularly adolescents. The current study attempted to address gaps by providing descriptive information on experiences of urban AI/AN adolescents across northern, central, and southern California.
Design
We describe demographics and several behavioral health and cultural domains, including: alcohol and other drug (AOD) use, risky sexual behavior, mental and physical health, discrimination experiences, involvement in traditional practices, and cultural pride and belonging. We recruited 185 urban AI/AN adolescents across northern, central, and southern California from 2014 to 2017 who completed a baseline survey as part of a randomized controlled intervention trial.
Results
Average age was 15.6 years; 51% female; 59% of adolescents that indicated AI/AN descent also endorsed another race or ethnicity. Rates of AOD use in this urban AI/AN sample were similar to rates for Monitoring the Future. About one-third of adolescents reported ever having sexual intercourse, with 15% reporting using alcohol or drugs before sex. Most reported good mental and physical health. Most urban AI/AN adolescents participated in traditional practices, such as attending Pow Wows and learning their tribal history. Adolescents also reported discrimination experiences, including being a victim of racial slurs and discrimination by law enforcement.
Conclusions
This study describes a select sample of California urban AI/AN adolescents across several behavioral health and cultural domains. Although these adolescents reported numerous discrimination experiences and other stressors, findings suggest that this sample of urban AI/AN teens may be particularly resilient with regard to behavioral health.
Keywords: Native American adolescents, American Indian/Alaska Native adolescents, urban, alcohol and drug use, sexual behavior, culture, discrimination
Introduction
It is well known that the American Indian/Alaska Native (AI/AN) population suffered tremendously from European contact and colonization, resulting in chronic trauma and unresolved grief across numerous generations (Brave Heart and DeBruyn 1998). In their seminal paper, Brave Heart and DeBruyn (1998) describe the many factors that contributed to this historical trauma among AI/ANs, including the boarding school era and the numerous federal policies focused on assimilation and destruction of Indigenous culture. The considerable urban population of AI/AN is due in large part to one of these federal policies, the Indian Relocation Act of 1956, which encouraged AI/AN families residing on reservations to move to urban centers (James 1992). According to the 2010 U.S. Census, approximately 70% of AI/ANs now reside within an urban setting (Norris, Vines, and Hoeffel 2012). Deleterious effects of this legislation have lasted for generations, and have been postulated to contribute to significant health disparities reflected in high rates of homelessness, unemployment, poverty, poor mental health (Duran and Duran 1995; Jernigan et al. 2015), and alcohol and drug use (Dickerson, Fisher, et al. 2012; Whitbeck et al. 2004), in addition to disconnection from culture and community (DeNavas-Walt and Proctor 2014; Dickerson, Johnson, et al. 2012).
Despite the large numbers of AI/ANs in urban settings, there is limited descriptive research on this population, particularly adolescents (West et al. 2012). We define adolescents in this paper as those who are aged 12–18. Most work in this area has examined clinical samples of AI/AN youth from early adolescence to young adulthood (Dickerson and Johnson 2012) versus a general urban population, or focused on one particular issue, such as identity, health disparities, or participation in cultural activities. The current paper adds to the literature on the health and well-being of urban AI/AN adolescents by describing a population of 185 urban adolescents, aged 14–18, living in northern, central, and southern California across a variety of behavioral health as well as social and cultural domains to better understand issues that may affect their overall health and well-being.
To date, several studies have focused on understanding cultural identity among urban AI/AN adolescents. For example, Kulis et al. (2013, 2011) conducted several cross-sectional studies examining ethnic identity with a sample of urban AI/AN adolescents in five middle schools (sample sizes range from 142 to 208). They found that urban AI/AN adolescents who were more connected to their AI/AN background also reported more involvement in traditional cultural practices (Kulis et al. 2013). They also found that following AI/AN traditional spiritual beliefs was associated with anti-drug attitudes, norms, and expectancies (Kulis et al. 2011).
Stumblingbear-Riddle and Romans (2012) conducted a cross-sectional study with 213 urban AI/AN adolescents and found that stronger enculturation and more social support from friends were both associated with higher resilience among these teens. Resilience is typically defined as being able to adapt positively in response to adversity (Waller and Okamoto 2003), and has been shown to be associated with decreased alcohol or other drug (AOD) use (Hodder et al. 2017). One study of 945 urban AI/AN adolescents and AI/AN adolescents residing on reservations examined participation in cultural activities and its association with ethnic identity (Schweigman et al. 2011). The association between cultural activities and ethnic identity was only significant among urban adolescents and not among reservation adolescents, highlighting the importance of participation in cultural events for urban adolescents to help maintain a strong connection with their AI/AN heritage (Schweigman et al. 2011).
Recent work has shown, however, that urban AI/AN adolescents often have limited opportunities to connect with their culture (Dickerson et al. 2015). Specifically, focus group work with two large urban communities in California emphasized the complex and traumatic history of AI/ANs, and the numerous challenges AI/AN adolescents face with cultural identity in the urban landscape, including struggles with mixed racial-ethnic identity and exposure to discrimination (Brown, Dickerson, and D’Amico 2016). These recent data from California support findings from an earlier qualitative study in 2012 of 107 AI families in Chicago describing the mental health and positive development needs of urban AI youth under the age of 25 in this area (West et al. 2012). Participants reported dispersion of the AI population across Chicago, and noted that gentrification had forced the AI community to live across many areas. This contributed to both mixed heritage and decreased knowledge of language and participation in cultural traditions. The authors also noted the importance of protective factors, such as having a supportive community focused on the healthy development of youth (West et al. 2012).
In terms of health disparities, few studies specifically address outcomes for urban AI/AN adolescents. Castor et al. (2006) used US Census data from 1990 to 2000 to compare health disparities between the general population in several urban counties and AI/ANs served by 34 federally funded urban Indian health organizations, which only included those over 18. They found disparities across socioeconomic, maternal and child health, and mortality. They also found that the AI/AN population was approximately twice as likely as the general population to be poor, unemployed, and to not have a college degree. They did not examine rates of AOD use.
Overall, research assessing differences in AOD use between urban AI/AN adolescents and urban adolescents from other races/ethnicities is scarce (Banks et al. 2017), and existing evidence is mixed. A 2008 study (Rutman et al. 2008) examining rates of AOD use from 1997 to 2003 from the Youth Risk Behavior Survey (YRBS) found that AI/ANs in grades 9–12 in urban areas were more likely to report lifetime marijuana (56.9%), cocaine (15.3%) and injection drug use (5.1%) compared with urban white adolescents (44.5% marijuana, 9.1% cocaine, 1.9% injection drug use). However, more recently, Cunningham and colleagues (Cunningham, Solomon, and Muramoto 2016) examined data from the National Survey on Drug Use and Health (NSDUH) for ages 12–65 from 2009 to 2013 and found that AI/ANs had lower or comparable rates across all alcohol use measures. Of note, no comparisons were made by age categories (e.g. 12–18) within each race/ethnicity or by geographical setting (e.g. reservation versus urban settings). Data from 2015 from the NSDUH on substance use prevalence (SAMHSA 2016) show that AI/AN adolescents aged 12–17 report lower rates of lifetime use of illicit drugs (20.7%) compared to whites (24.4%), blacks (28.4%), and Hispanics (26.6%); lifetime rates of cigarette use for AI/ANs (14%) were similar to whites (15%), and slightly higher compared to blacks (10.2%) and Hispanics (11.4%); and lifetime alcohol use for AI/AN adolescents (24.9%) was similar to blacks (24.8%), and lower than whites (30.2%) and Hispanics (28.6%). This report did not have a breakdown of marijuana use by race/ethnic categories for 12–17, nor did it assess adolescents across different geographic settings (e.g. urban versus rural). Overall, these more recent data suggest that AI/AN adolescents are reporting AOD use at equivalent or lower levels than other racial-ethnic categories.
In terms of sexual behavior, data from the YRBS (CDC 2016) indicate that, overall, 41% of high school teens report having engaged in sexual intercourse in their lifetime. Typically, the YRBS compares statistics by white, black, and Hispanic race/ethnic categories, and includes AI/AN adolescents in the ‘other’ category. A 2014 study that analyzed data from the YRBS from 2007 and 2009 separated out students in the AI/AN category by examining teens who reported that they were non-Hispanic and selected AI/AN as their only race (N = 436) or who selected AI/AN plus another race or Hispanic ethnicity (N = 1128), for a total of 1564 respondents (de Ravello et al. 2014). They found that AI/AN adolescents were less likely to report ever having had sexual intercourse in their lifetime (48.9%) than black (65.9%) adolescents. Rates of reported lifetime sexual intercourse among AI/AN adolescents were similar to Hispanic teens (50.3%), and more AI/AN adolescents reported having sex in their lifetime than white teens (42.8%). The percentage of currently sexually active AI/AN adolescents (32.8%) was similar to whites (32.4%) and Hispanics (36%) and lower than black adolescents (46.8); and rates of using a condom during last sexual intercourse did not differ by race-ethnicity (AI/AN: 57.3%, white: 61.6%, black: 63.8%, Hispanic: 58.1%).
Overall, these existing descriptive studies provide an important foundation by highlighting some of the issues that AI/AN adolescents may face. However, these studies typically focus on only one domain, such as substance use, sexual behavior, or cultural identity, many have small AI/AN samples, and most do not assess AI/AN adolescents that live in urban areas. The current study attempts to address some of these gaps by providing descriptive data on a population of 185 urban AI/AN adolescents living in northern, central, and southern California across a variety of behavioral health and cultural domains.
This work is an important first step in providing a more comprehensive understanding of the issues that California urban AI/AN adolescents may face. We utilize quantitative data, and focus on several behavioral health and cultural domains, including AOD use, risky sexual behavior, mental and physical health, discrimination experiences, involvement in traditional practices, and cultural pride and belonging. Given previous work with the AI/AN population, we expected that this sample of urban AI/AN adolescents would report high rates of AOD use and risky sexual behavior, poor mental and physical health, high rates of discrimination experiences, and low rates of involvement in traditional practices and cultural pride. This work provides a snapshot of the challenges and resiliency of this vulnerable population, which can help inform future prevention and intervention efforts.
Materials and methods
Procedure
We recruited AI/AN adolescents in northern, central, and southern California in urban areas from 2014 to 2017 as part of an intervention trial testing MICUNAY (Motivational Interviewing and Culture for Urban Native American Youth), a new substance use prevention program integrating motivational interviewing with AI/AN traditional practices (Dickerson et al. 2015). Data are from the baseline survey, for which adolescents were paid $25. All procedures were approved by the institution’s internal review board and by the communities with whom we collaborated on the project. We maintained a community advisory board and a teen advisory board over the course of the study, and we worked closely with several AI/AN community organizations in each city to determine the best ways to engage the community in our project and help us recruit AI/AN families and adolescents. For example, we created recruitment flyers using background images relevant to that community (e.g. in one community, we used a picture of a known landmark that community members recognized in a park where culturally-related events were often held), and we worked with leaders to provide events in each community tailored to the needs of that particular community (Jernigan, D’Amico, and Keawe‘aimoku Kaholokula 2018). We held community information events, attended Pow Wows and other community events, posted information on AI/AN email lists and on Facebook, and hired AI/AN recruiters in each community to discuss the project with AI/AN families. Interested parents and adolescents could call our toll-free project number or provide contact information to one of our recruiters at these events and be called by our staff. To be eligible for the project, adolescents had to be 14–18 years old (inclusive), and either verbally self-identify as AI/AN or be identified as AI/AN by a parent/guardian or community elder. Eligible adolescents were scheduled to complete a baseline survey at a time and place that was convenient to them. Our collaborator, Sacred Path Indigenous Wellness Center (SPIWC), our community advisory board, and the AI/AN organizations all worked closely with our team to ensure that our recruitment and engagement with these communities were conducted in a culturally-appropriate manner. Our Community-Based Participatory Research approach (CBPR) is reflective of an approach routinely used in National Institutes of Health (NIH)-funded studies of new health interventions (e.g. Dickerson et al. 2018; Minkler and Wallerstein 2011).
Measures
Race/Ethnicity
Adolescents either verbally self-identified as AI/AN or were identified as AI/AN by a parent/guardian or community elder to be part of the project. In a subsequent self-report survey using categories established by NIH, participants checked ‘all that apply’ for the following categories: AI/AN, Hispanic, Asian, Native Hawaiian or Pacific Islander, black or African American, white, and other.
AOD use
We assessed substance use with the well-established Monitoring the Future items (Miech et al. 2016). Adolescents reported lifetime, past year, and past 3-month use for a variety of substances, including cigarettes, e-cigarettes, alcohol, marijuana, inhalants, over-the-counter drugs and prescription drugs to get high, and stimulants. We report the percentage of adolescents who indicated any substance use at each time point.
Consequences of alcohol and marijuana use
Adolescents reported the consequences they had experienced from use in past three months. Consequences were based on the Diagnostic and Statistical Manual (DSM) criteria with seven items for alcohol (e.g. missed school or work) and 5 for marijuana (e.g. had difficulty concentrating) (D’Amico et al. 2016). Both scales have been used extensively with adolescents and were reliable with teens in this study (α = .75 for marijuana and α = .94 for alcohol).
Sexual behavior
items were taken from the YRBS (CDC 2014). Adolescents first reported whether they ever had sexual intercourse. Those that reported that they had sexual intercourse were asked to report: 1) age at first intercourse (from 11 or younger to 17 or older), 2) number of partners in their lifetime (from 1 to 6 or more), 3) whether they used AOD before the last time they had sex (yes/no), 4) and whether they used a condom the last time that they had sex (yes/no).
Family and peer items come from published research on adolescents (D’Amico et al. 2008). Items assessed whether an older sibling, or the adult most important to the adolescent, had ever used AOD. Three items assessed how often they spend time around teens who drink, use marijuana, or smoke cigarettes (1 = never to 4 = often).
Discrimination was measured using the short form of the Microaggressions Distress Scale (Walters 2009). Items asked about verbal, behavioral, and environmental encounters in the past year that implicitly or explicitly diminish racial heritage, identity, or culture (e.g. asked if participant is a ‘real Indian’). Response options were ‘yes,’‘I’m not sure, but I think so,’ and ‘no.’
Mental health status (e.g. felt downhearted and blue; been very nervous; α = .74) was measured with the well-validated Mental Health Inventory-5 (Stewart et al. 1992). Adolescents were asked to report on their mental health status in the last month using a 6-point Likert scale from 1 (‘all of the time’)to6(‘none of the time’). Relevant items are reversed so that a higher total score (transformed to range from 0 to 100) indicates better mental health. We used a cut point of 60 (Kelly et al. 2008), with a score of 60 or higher considered to be ‘good’ mental health for adolescents (Meredith et al. 2018).
General health status was measured with an item assessing perceptions of general health on a 5-point scale (1 = poor to 5 = excellent) from the Short Form Health Survey (SF-12) (Ware, Kosinski, and Keller 1996).
Traditional practices
Adolescents reported lifetime participation in more than 20 different traditional practices (e.g. going to Pow Wows, prayer, playing Native hand or stick games). Items were based upon extensive research conducted with AI/AN adolescents, parents, and community partners (Kaufman et al. 2014).
Cultural pride and belonging
We assessed adolescents’ sense of AI/AN cultural pride and sense of belonging with the Multigroup Ethnic Identity Measure (MEIM), which has twelve items (α = .94). Respondents are asked the degree to which they agree with statements such as, ‘I have a clear sense of my ethnic background and what it means to me’ on a scale from 1 = ‘strongly disagree’ to 5 = ‘strongly agree’ (Phinney and Ong 2007; Ponterotto et al. 2003). Given that our focus group work (Brown, Dickerson, and D’Amico 2016) indicated that many adolescents were of mixed ethnicity and our focus was on AI/AN identity, we modified items to focus on AI/AN heritage (e.g. ‘I have clear sense of my AI/AN identity and what it means to me’).
Cultural characteristics
Cultural characteristics were assessed with questions taken from various measures that have been utilized extensively with AI/ANs (Gossage et al. 2003; Moran et al. 1999). Adolescents were asked whether their family used their tribal language (does not speak, a few words, carries entire conversation), their tribal language proficiency (from 1 — does not speak to 4 — speaks very well), whether they lived on a reservation in the last 12 months (yes/no), whether they or a parent or grandparent ever attended an Indian boarding school (yes/no/don’t know), whether spirituality influenced different behaviors (yes/no) (e.g. diet, physical activity), whether they personally followed the tribal way of life (from 1 — not at all to 4 — a lot), whether it was important to keep their tribal identity, values, and practices (from 1 — not at all to 4 — a lot), and how different they felt their tribal culture was from ‘mainstream culture’ (no differences, small differences, big differences).
Results
Of the 185 adolescents who completed the baseline survey, 51% were female, and the average age was 15.6 years (Table 1). Approximately half of the sample reported living with two parents (45%). Among adolescents who knew their parents’ education, 80% reported that their mother had graduated high school, and 73% reported that their father had graduated high school. Fifty-nine percent of adolescents that self-identified on the survey as AI/AN also endorsed another race or ethnicity. Almost half of the sample (45%) marked that they were of Hispanic origin, and roughly one-fifth (17%) self-identified as white. Although adolescents had to self-identify verbally or be identified as AI/AN by a family member or elder as AI/AN to participate in the project, 35 adolescents (19%) did not mark AI/AN on the survey. Over 60 tribes were represented; however, to protect the confidentiality of participants and tribes, we do not report individual tribe information (Norton and Manson 1996).
Table 1.
MICUNAY sample demographics (N = 185).
| N | Percent | |
|---|---|---|
| Age | ||
| 14 years old | 51 | 28 |
| 15 years old | 38 | 21 |
| 16 years old | 44 | 24 |
| 17 years old | 31 | 17 |
| 18 years old | 19 | 10 |
| Sex | ||
| Male | 90 | 49 |
| Female | 95 | 51 |
| Race/Ethnicitya | ||
| Hispanic/Latino(a) | 83 | 45 |
| AI/AN | 150 | 81 |
| Asian/Asian American/Pacific Islander | 8 | 4 |
| Black/African American | 21 | 11 |
| White/Caucasian | 32 | 17 |
| Other | 8 | 4 |
| High school degree | ||
| Mother | 120 | 80 |
| Father | 94 | 73 |
Note that all youth had to verbally self-identify as AI/AN or be identified as AI/AN by a parent/guardian or community elder to be part of the project. They then completed a survey asking them to label their race/ethnicity. These numbers and percentages reflect what youth reported on the survey and can overlap if they identified more than one race/ethnicity. Thirty-five youth did not check AI/AN on the survey, although they self-identified verbally or were identified verbally by a parent/guardian or community elder as Native American to be in the study.
For substance use, marijuana was the most frequently reported drug across all time periods followed by alcohol and e-cigarette use (Table 2). About 1 in 4 teens reported heavy drinking (e.g. drinking 5 or more drinks in one sitting) in the past year, and about 1 in 8 adolescents reported heavy drinking in the past three months. Very few adolescents reported lifetime use of prescription drugs (n = 17) or stimulants (n = 11). Half of the adolescents that reported alcohol or marijuana use also reported experiencing two or more consequences in the past three months from this use.
Table 2.
Alcohol and other drug use (N = 185).
| Lifetime N (%) | Past year N (%) | Past 3 months N (%) | |
|---|---|---|---|
| Cigarettes | 35 (19%) | 27 (15%) | 19 (10%) |
| E-cigarettes | 48 (26%) | 29 (16%) | 18 (10%) |
| Alcohol | 71 (39%) | 63 (35%) | 43 (23%) |
| Heavy drinking | – | 43 (23%) | 24 (13%) |
| Marijuana | 78 (43%) | 66 (36%) | 52 (28%) |
| Inhalants | 18 (10%) | 10 (5%) | 2 (1%) |
| Over-the-counter drugs | 22 (12%) | 16 (9%) | 8 (4%) |
| Prescription drugs | 17 (9%) | 14 (8%) | 6 (3%) |
| Stimulants | 11 (6%) | 9 (5%) | 6 (3%) |
| Other drugs | 18 (10%) | 14 (8%) | 10 (5%) |
| Consequencesa | |||
| Alcohol: Experienced 2 or more consequences | – | – | 21 (49%) |
| Marijuana: Experienced 2 or more consequences | – | – | 25 (48%) |
Rates for experiencing alcohol and marijuana consequences are among those who consumed alcohol or marijuana, respectively, in the past three months.
After adjusting for age distribution, rates of AOD use in our urban AI/AN adolescent sample are similar to adolescent AOD use rates in Monitoring the Future (Miech et al. 2016) for most substances, except for marijuana, which is higher in our sample. However, age adjusted rates of use for all substances, including marijuana, are similar to a recent study with a racially/ethnically diverse sample of 1573 adolescents (51% Hispanic, 27% black) seen from 2013–2015 for general appointments at four different primary care clinics in Los Angeles and Pittsburgh (D’Amico et al. 2016).
Approximately one-third of the sample (n = 62) reported that they had ever had sexual intercourse (Table 3). Most of these adolescents reported that they had intercourse for the first time at the age of 14 or 15 (54%), and only had one sexual partner (44%) in their lifetime and in the past three months (51%). Almost half reported that they did not use a condom the last time they had sex (44%). Few reported using AOD before the last time they had sex (15%). Data from the YRBS (CDC 2016) are similar for condom use, with 43% of high school teens reporting that they did not use a condom the last time they had sex. More high school teens on the YRBS reported having engaged in sexual intercourse in their lifetime (41%) and using AOD before the last time they had sex (21%) than teens in our sample.
Table 3.
Sexual behavior among youth reporting ever having had intercourse (N = 62).
| N | Percent | |
|---|---|---|
| Age when had sex for 1st time | ||
| 11 or younger | 2 | 3 |
| 12 | 5 | 8 |
| 13 | 6 | 10 |
| 14 | 12 | 20 |
| 15 | 21 | 34 |
| 16 | 12 | 20 |
| 17 or older | 3 | 5 |
| Number of sexual partners (lifetime) | ||
| 1 | 27 | 44 |
| 2 | 8 | 13 |
| 3 | 10 | 16 |
| 4 | 6 | 10 |
| 5 | 2 | 3 |
| 6 or more | 8 | 13 |
| Number of sexual partners (past 3 months) | ||
| None in past 3 months | 22 | 36 |
| 1 | 31 | 51 |
| 2 | 5 | 8 |
| 3 | 2 | 3 |
| 4 | 0 | 0 |
| 5 | 0 | 0 |
| 6 or more | 1 | 2 |
| Used alcohol or drugs before last time had sex | 9 | 15 |
| Did not use condom last time had sex | 27 | 44 |
Note: Of N = 185 participants, 62 (34%) responded yes to the question, ‘Have you EVER had sexual intercourse?’ N = 119 participants (64%) reported no history of sexual intercourse, and 4 (2%) did not respond to the question.
Teens in our study also reported alcohol, marijuana, and commercialized tobacco use for the ‘most important adult’ in their life (Table 4). Cigarette use was highest at 25%, followed by marijuana (13%). Only a small percentage of adolescents (5%) reported that the most important adult in their life drank 4 or more days a week. Among participants who had older siblings, use was highest for alcohol (36%) followed by marijuana (28%) and cigarettes (15%). Regarding peer influence, almost half of the sample (48%) reported that they were often or sometimes around peers that used marijuana (versus never or hardly ever), about one-third said that they were very often or sometimes around peers that drank (32%), and one in five said they were very often or sometimes around friends that smoked cigarettes (20%).
Table 4.
Family and peer substance use, discrimination experiences, and physical and mental health (N = 185).
| N | Percent | |
|---|---|---|
| Family use | ||
| Most important adult ever smokes cigarettes | 45 | 25 |
| Most important adult drinks 4 or more days/week | 9 | 5 |
| Most important adult ever smokes marijuana | 24 | 13 |
| Older sibling: Cigarettesa | 21 | 15 |
| Older sibling: Alcohola | 49 | 36 |
| Older sibling: Marijuanaa | 39 | 28 |
| Peer influenceb | ||
| Time spent around peers who smoke cigarettes | 36 | 20 |
| Time spent around peers who drink | 58 | 32 |
| Time spent around peers who use marijuana | 89 | 48 |
| Experienced discrimination in past yearc | ||
| Discrimination by law enforcement | 30 | 16 |
| Victim of racial slurs | 52 | 29 |
| Trailed or followed | 17 | 9 |
| Mistaken for race other than Native | 100 | 55 |
| Past-life slur by non-Native | 66 | 36 |
| Told of spiritual connection to AI/AN from non-Native | 73 | 40 |
| Told ‘lucky to be AI/AN’ by non-Native | 112 | 62 |
| Asked if ‘real Indian’ by non-Native | 113 | 62 |
| Asked to prove authenticity by non-Native | 74 | 41 |
| Physically attacked | 11 | 6 |
| Self-reported health | ||
| Excellent | 38 | 21 |
| Very good | 67 | 36 |
| Good | 63 | 34 |
| Fair | 16 | 9 |
| Poor | 0 | 0 |
| Good mental health (60+ score on MHI-5) | 127 | 69 |
Rates for substance use by older siblings are among participants with older siblings.
‘Sometimes’ or ‘often’ (vs. ‘never’ or ‘hardly ever’)
‘Percent includes: ‘Yes’ or ‘I’m not sure but I think so.’
For discrimination experiences, we report the percentage of adolescents that indicated ‘yes’ or ‘I’m not sure, but I think so.’ Overall, many urban AI/AN adolescents in our sample reported discrimination experiences, with many teens reporting that they were asked if they were a ‘real Indian’ (62%), told they were ‘lucky to be American Indian/Native’ by a non-Native (62%), or asked to prove authenticity by a non-Native (41%). Almost 1 in 3 adolescents reported being a victim of racial slurs (29%), and 16% reported discrimination by law enforcement.
Most adolescents reported good mental and physical health. Specifically, 57% of the sample reported very good or excellent physical health, and more than two-thirds of the sample indicated good mental health (69%).
For the cultural characteristics (Table 5), almost two-thirds of adolescents reported that they did not speak their tribal language (63%), but one-third said that they used certain tribal words and phrases. More than half (55%) of the sample said that they followed the tribal way of life. Some adolescents reported that spirituality, religion, or beliefs influenced different aspects of their lives, such as diet (17%), physical activity (18%), or use of alcohol (12%). Few adolescents lived on a reservation in the past year (7%). Almost 1 in 5 reported that their grandparent attended an Indian boarding school (18%), and 8% said that their parents attended an Indian boarding school. Few adolescents had attended an Indian boarding school themselves (3%). Most adolescents indicated that their tribal culture was different from mainstream culture, with 40% saying it differed in big ways and 43% reporting small differences.
Table 5.
Cultural characteristics (N = 185).
| N | Percent | |
|---|---|---|
| Family use of tribal language | ||
| Does not speak | 113 | 63 |
| A few words or phrases | 59 | 33 |
| Carries entire conversations | 8 | 4 |
| Tribal language proficiency | ||
| Does not speak | 129 | 71 |
| Speaks a little, but not very well | 46 | 25 |
| Speaks moderately well | 5 | 3 |
| Speaks very well | 1 | 1 |
| Lived on a reservation past 12 months | 13 | 7 |
| Ever attended Indian boarding school | 6 | 3 |
| Any parents ever attend an Indian boarding school | ||
| Yes | 15 | 8 |
| No | 137 | 75 |
| Don’t know | 30 | 16 |
| Any grandparents go to boarding or residential school | ||
| Yes | 33 | 18 |
| No | 69 | 38 |
| Don’t know | 78 | 43 |
| Spirituality, religion, or beliefs have influence on …a | ||
| Diet or food | 31 | 17 |
| Drinking alcohol | 22 | 12 |
| Use of recreational drugs | 17 | 9 |
| Smoking | 16 | 9 |
| Physical activity | 34 | 18 |
| None of the above | 114 | 62 |
| Personally follow tribal way of life | ||
| Not at all | 82 | 45 |
| A little | 54 | 30 |
| Somewhat | 38 | 21 |
| A lot | 7 | 4 |
| Important to keep your tribal identity, values, and practices | ||
| Not at all | 28 | 16 |
| A little | 46 | 26 |
| Somewhat | 41 | 23 |
| A lot | 65 | 36 |
| How different is youth’s tribal culture from mainstream | ||
| No differences | 30 | 17 |
| Only small differences | 74 | 43 |
| Big differences | 70 | 40 |
Respondents were instructed to mark all that apply and categories are not mutually exclusive except for ‘none of the above.’
For cultural pride and belonging (Table 6), responses varied by the different items in the MEIM measure. About two-thirds of adolescents (68%) indicated that they felt good about their cultural background, that they were happy that they were a member of the AI/AN tribal group that they belonged to (64%), or had a lot of pride in their AI/AN identity (60%). About one-third reported that they spent time trying to find out more about their identity (36%) or that they thought a lot about how their life would be affected by their AI/AN identity (39%).
Table 6.
Cultural pride and belonging (MEIM)a (N = 185).
| N | Percent | |
|---|---|---|
| I have spent time trying to find out more about my AI/AN identity | 65 | 36 |
| I am active in groups that include mostly members of my AI/AN group | 50 | 28 |
| I have a clear sense of my AI/AN identity and what it means for me | 62 | 35 |
| I think a lot about how my life will be affected by my AI/AN identity | 69 | 39 |
| I am happy that I am a member of the AI/AN tribal group I belong to | 113 | 64 |
| I have a strong sense of belonging to my AI/AN tribal group | 73 | 41 |
| I understand pretty well what my AI/AN identity means to me | 76 | 42 |
| In order to learn more about my AI/AN identity, I have often talked to other people | 74 | 41 |
| I have a lot of pride in my AI/AN identity | 107 | 60 |
| I participate in cultural practices of my own AI/AN tribal group | 64 | 36 |
| I feel a strong attachment towards my AI/AN tribal group | 73 | 41 |
| I feel good about my cultural background | 121 | 68 |
Response of ‘agree’ or ‘strongly agree’ (versus ‘strongly disagree,’ ‘disagree,’ or ‘in the middle’).
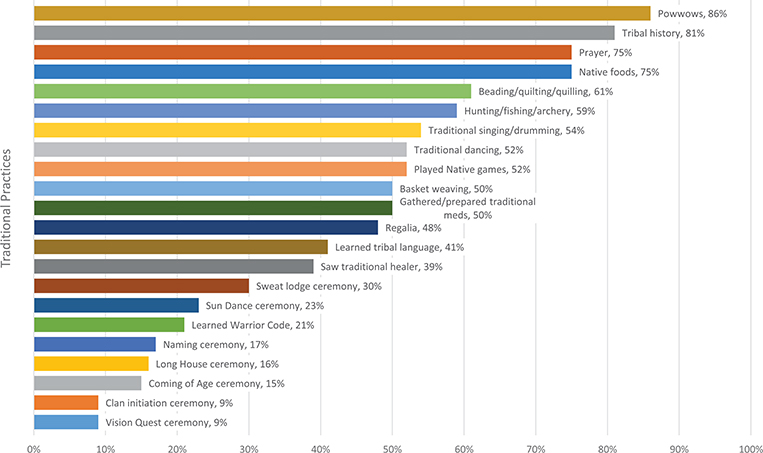
Finally, the majority of our urban sample reported participation in traditional practices (see Figure 1). The most frequently reported traditional practices were attending Pow Wows (86%), learning tribal history (81%), eating Native foods (75%), and engaging in prayer (75%). More than half of the adolescents also reported beading or quilting, hunting or fishing, participating in traditional singing, drumming, or dancing, and playing Native games. It’s also notable that at least 1 in 3 adolescents reported participating in traditional practices that might be more difficult to access given the urban setting, such as learning their tribal language (41%), seeing a traditional healer (39%), and participating in a sweat lodge ceremony (30%).
Figure 1.
Percent of youth reporting ever participating in traditional practices.
Discussion
This paper adds to the literature on urban AI/AN adolescents by describing a population that is typically left out of research and experiences social marginalization and discrimination. We provide descriptive data on urban AI/AN adolescents living in northern, central, and southern California across several domains, including AOD use, sexual behavior, mental and physical health, discrimination experiences, participation in traditional practices, and cultural pride and belonging.
Overall, the 185 adolescents in this study were from diverse racial and ethnic backgrounds and represented over 60 tribes. Contrary to our expectations, AOD use in this sample was similar to use rates seen in national surveys (Miech et al. 2016), although marijuana use was slightly higher in this California sample. This is also contrary to research indicating that AI/AN adolescents use substances at much higher rates than other races/ethnicities (Rutman et al. 2008), but is similar to the 2015 NSDUH data that found that AI/AN adolescents aged 12–17 reported lower rates of lifetime use of illicit drugs and alcohol, and similar lifetime rates of cigarettes use compared to whites (SAMHSA 2016). Also contrary to our expectations, rates of risky sexual behavior were comparable to national data. For example, 44% of our sample reported that they did not use a condom the last time that they had sex, and 43% of teens from the YRBS reported that they did not use a condom the last time they had sex (CDC 2016).
One reason that we may have found lower AOD use may be related to recent trends showing decreased AOD use across the U.S. for all adolescent populations (Johnston et al. 2018). Another reason that we may have found lower AOD use, in addition to lower risky sexual behavior, among our select sample of urban AI/AN adolescents compared with other urban AI/AN adolescents is because our recruitment captured teens with greater than average cultural knowledge and participation in traditional practices, which is known to be protective (Schweigman et al. 2011). Specifically, our measures of cultural belonging and pride emphasize that many teens in our sample felt good about their cultural background and took pride in their AI/AN identity. This may be due, in part, to our recruitment approach. For example, by hiring AI/AN recruiters from the community who knew the AI/AN community well, recruiting at community events, such as Pow Wows, and working with AI/AN organizations to recruit teens, our sample may have had a stronger cultural connection to their community than other population based urban AI/AN adolescent samples. The close connection with their AI/AN culture and community may have contributed to this urban sample being more resilient, and perhaps supported them in making healthier choices. Furthermore, rates of parental high school graduation were slightly higher in our sample compared to Census data from 2000 (Castor et al. 2006), which may also have been protective. Larger, nationally representative epidemiological studies focused on urban AI/AN adolescent risk behaviors are needed to better understand trends over time for this population. Furthermore, longitudinal work is also needed to determine how increased involvement in traditional practices and cultural pride may relate to engagement in these risk behaviors.
For family and peer influences, more adolescents reported being around friends that used marijuana compared to alcohol and cigarettes, which may be due, in part, to the changing legal landscape of this drug across the United States, and recent efforts to legalize recreational marijuana in California (D’Amico et al. 2017). During our previous focus groups conducted with these communities to understand the challenges that teens face, there was much discussion around norms for AOD use in the AI/AN community (Brown, Dickerson, and D’Amico 2016), and the importance of addressing these norms in prevention programing (Dickerson et al. 2015). Because peers are often linked with subsequent AOD use, this is an important area for prevention and intervention programs targeting urban AI/AN adolescents.
Compared to other work in this area, this study also offers a broad look at the types of traditional practices that urban AI/AN adolescents participated in over their lifetime. Participation rates were high, particularly for traditional practices that are easier to access, such as Pow Wows. Even for many ceremonies that may be more specific to certain tribes (e.g. the Sun Dance Ceremony), 1 in 10 of the adolescents indicated that they had participated in such activities, and 1 in 3 indicated that they had been to a sweat lodge ceremony. Given that many urban AI/AN teens may not feel connected to their heritage (Brown, Dickerson, and D’Amico 2016), findings are encouraging and suggest that this sample of California urban AI/AN adolescents was able to access cultural resources in their communities, which may have contributed to greater resilience. This is important, as other work in this area has shown that involvement in traditional practices is protective for behavioral health (Schweigman et al. 2011). Opportunities for engaging in traditional practices can be challenging within the urban setting (Brown, Dickerson, and D’Amico 2016); however, providing these opportunities for urban AI/AN teens may help to prevent risk behaviors within this population.
All adolescents in the study verbally self-identified as AI/AN or were identified as AI/AN by a family member or elder; however, 35 adolescents did not self-identify as AI/AN on the survey. Self-identification as AI/AN is an important construct that may help improve understanding of the role that race/ethnicity may play on various health outcomes for urban AI/AN adolescents. This survey self-identification corroborates focus group research conducted with urban AI/AN adolescents, who discussed the difficulties in identifying one’s race/ethnicity, particularly if teens were of mixed race/ethnicity (Brown, Dickerson, and D’Amico 2016). It is also consistent with other work from the longitudinal ADD Health data set examining how adolescents label their race/ethnicity (Nishina et al. 2010). These investigators found that over time, AI/AN adolescents had the highest rate of switching their ethnic identity, with almost half of these adolescents who reported white/Native American consolidating and just reporting white. In addition, many AI/ANs are of mixed race. For example, in the current study, many AI/AN adolescents marked other races/ethnicities, with 45% reporting being of Hispanic descent in addition to reporting AI/AN descent. This is likely due to the sample being from California, where 39% of the state reports being of Hispanic descent (US Census Bureau 2017). It is important to note that research has shown the difficulty that people have in identifying themselves into ethnic and racial categories (Gonzalez-Barrera and Lopez 2015; Zaslavsky, Ayanian, and Zaborski 2012), as identity is often fluid (Liebler et al. 2017; Quintana 2007), particularly during the developmental period of adolescence (Nishina et al. 2010). Finally, one must also consider the tribal specific identities that teens noted on their surveys. Research with this AI/AN urban population found that tribal specific identities were seen as compatible and interconnected with pan-tribal identity (Brown, Dickerson, and D’Amico 2016). In sum, research is needed to better understand the association between racial/ethnic identity and health and cultural outcomes among urban AI/AN adolescents. Future research must continue to consider the disadvantaged status of AI/ANs and the multiple categories of racial identification.
Many urban AI/AN adolescents in our sample reported discrimination experiences. More adolescents reported experiencing subtle forms of discrimination (e.g. told of spiritual connection to AI/AN by non-Native); however, almost 1 in 3 said that they were a victim of racial slurs, and 1 in 6 teens reported that they were discriminated against by law enforcement. Thus, urban AI/AN adolescents in California continue to struggle with discrimination in their day to day lives. This fits with focus group data from these communities where participants discussed both overt and more subtle forms of discrimination, as well as occasional conflict between the AI/AN belief system or cultural practices and behaviors or beliefs expressed in schools or other institutions (Brown, Dickerson, and D’Amico 2016). For example, teens said that they were often misidentified because of the low percentage of Native Americans in the population, so they might only be seen as Black or Hispanic rather than Native American. They also discussed that it was often difficult negotiating their own feelings surrounding having mixed heritage and how to identify with their mixed racial/ethnic heritage (Brown, Dickerson, and D’Amico 2016). Despite their high level of exposure to discrimination, the urban AI/AN adolescents in our study may be benefitting from their close connections with their AI/AN community, which could contribute to resilience. Further research on the impact of perceived discrimination on risky health behaviors among urban AI/ANs is warranted.
Overall, these urban AI/AN adolescents reported good physical and mental health, which contrasts with other health disparity research in this area (Castor et al. 2006); however, existing disparities work has not focused on teens, but rather on the adult AI/AN population. Research on self-rated health among teens is scant, and indicates that chronic health conditions generally do not contribute to adolescents’ assessments of self-rated health, which are more affected by momentary fluctuations in mood or aches and pains (sore throat, headache, etc.) (Boardman 2006). The lower stability of adolescent self-rated health over time is likely related to the fact that serious, chronic health conditions generally do not emerge until adulthood.
As noted earlier, there are limitations to the study. One of the main limitations is generalizability of findings as this was a select sample of urban AI/AN adolescents in California. In addition, we recruited at community based events, such as Pow Wows, and these adolescents volunteered to be part of this research project and may have therefore had more connection to their AI/AN communities than other AI/AN adolescents residing in these urban areas. Thus, our findings may not generalize to all urban AI/AN adolescent populations in the U.S. Finally, this was a self-report survey addressing a variety of risk behaviors, such as AOD use. However, the limitations of self-report are often exaggerated (Chan 2008), and recent work with young adults 18–21 has shown that self-reported alcohol use is corroborated by a biochemical measure, transdermal alcohol assessment (Simons et al. 2015).
Despite limitations, this study adds to the scant literature in this area by describing a sample of urban AI/AN adolescents in California across several behavioral health and cultural domains. This work provides important insight into the experiences of urban AI/AN teens, which can increase understanding of how to better allocate resources so that these adolescents go on to lead healthy, productive lives.
Implications and contribution.
This paper focused on describing urban AI/AN adolescents’ experiences. There are limited public health data on urban AI/AN adolescent populations, and findings suggest that although these teens experience numerous discrimination experiences and a variety of other stressors, the adolescents in this California sample may be particularly resilient. Thus, despite dealing with adverse experiences, these teens showed relatively healthy outcomes. This may be due, in part, to their high levels of participation in traditional activities, indicating that they have access to numerous cultural and traditional resources within their communities, which may help them connect to their heritage. It is critical to conduct epidemiological work with this population to better understand the needs of urban AI/AN adolescents across different geographic regions by measuring a variety of constructs. This information will help parents, providers, and communities determine the best ways to engage with and provide services for this underserved population.
Acknowledgement
Work on this article was supported by a grant from the National Institute of Alcohol Abuse and Alcoholism R01AA022066 to Drs. D’Amico and Dickerson, with co-funding from the National Institute on Drug Abuse. We would also to thank our Elder and youth advisory boards and the communities and organizations that helped us recruit adolescents for this study.
Funding
Work on this article was supported by a grant from the National Institute of Alcohol Abuse and Alcoholism R01AA022066 to Drs. D’Amico and Dickerson, with co-funding from the National Institute on Drug Abuse.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Banks, Devin E, Rowe Alia T., Mpofu Philani, and Tamika C B Zapolski 2017. “Trends in Typologies of Concurrent Alcohol, Marijuana, and Cigarette use among US Adolescents: An Ecological Examination by Sex and Race/Ethnicity.” Drug and Alcohol Dependence 179 (1):71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boardman, Jason D 2006. “Self-Rated Health Among U.S. Adolescents.” Journal of Adolescent Health 38 (4): 401–408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brave Heart M. Y. H., and DeBruyn Lemyra M. 1998. “The American Indian Holocaust: Healing Historical Unresolved Grief.” American Indian Alaska Native Mental Health Research 8(2): 56–78. [PubMed] [Google Scholar]
- Brown RA, Dickerson DL, and D’Amico EJ. 2016. “Cultural Identity Among Urban American Indian/Alaska Native Youth: Implications for Intervention Design.” Prevention Science 17 (7): 852–861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castor L. Mei, Smyser Michael S., Taualii Maile M, Park Alice N., Lawson Shelley A., and Forquera Ralph A.. 2006. “Nationwide Population-Based Study Identifying Health Disparities Between American Indians/Alaska Natives and the General Populations Living in Select Urban Counties.” American Journal of Public Health 96 (8): 1478–1484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. 2014. “Youth Risk Behavior Surveillance Survey.” https://www.cdc.gov/healthyyouth/data/yrbs/index.htm?s_cid=tw-zaza-1016.
- CDC. 2016. “Youth Risk Behavior Surveillance—United States, 2015.” MMWR Surveillence Summaries 65: 1–180. [DOI] [PubMed] [Google Scholar]
- Chan D 2008. “So Why Ask Me? Are Self-Report Data Really That Bad?” In Statistical and Methodological Myths and Urban Legends: Doctrine, Verity and Fable in the Organizational and Social Sciences, edited by Lance CE, and Vandenberg RJ, 309–336. New York: Psychology Press. [Google Scholar]
- Cunningham James K., Solomon Teshia A., and Muramoto Myra L.. 2016. “Alcohol use Among Native Americans Compared to Whites: Examining the Veracity of the ‘Native American Elevated Alcohol Consumption’ Belief.” Drug and Alcohol Dependence 160: 65–75. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Miles JNV, Stern SA, and Meredith LS. 2008. “Brief Motivational Interviewing for Teens at Risk of Substance Use Consequences: A Randomized Pilot Study in a Primary Care Clinic.” Journal of Substance Abuse Treatment 35: 53–61. [DOI] [PubMed] [Google Scholar]
- D’Amico EJ, Parast L, Meredith LS, Ewing BA, Shadel WG, and Stein BS. 2016. “Screening in Primary Care: What is the Best Way to Identify at-Risk Youth for Substance Use?” Pediatrics 138: 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Pedersen ER, and Shih RA. 2017. “Understanding Rates of Marijuana Use and Consequences Among Adolescents in a Changing Legal Landscape.” Current Addiction Reports 4 (4): 343–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeNavas-Walt C, and Proctor BD. 2014. U.S. Census Bureau, Current Population Reports: Income, Poverty, and Health Insurance Coverage in the United States: 2013. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- de Ravello L, Jones S. Everett, Tulloch S, Taylor M, and Doshi S. 2014. “Substance Use and Sexual Risk Behaviors Among American Indian and Alaska Native High School Students.” Journal of School Health 84 (1): 25–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Baldwin J, Belcourt A, Belone L, Gittelsohn J, Kaholokula K, Lowe J, Patten C, and Wallerstein N. 2018. “Encompassing Cultural Contexts Within Scientific Research Methodologies in the Development of Health Promotion Interventions.” Prevention Science, doi:10.1007/s11121–018-0926–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Brown RA, Johnson CL, Schweigman K, and D’Amico EJ. 2015. “Integrating Motivational Interviewing and Traditional Practices to Address Alcohol and Drug use Among Urban American Indian/Alaska Native Youth.” Psychology of Addictive Behaviors 65: 26–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Fisher DG, Reynolds GL, Baig S, Napper LE, and Anglin MD. 2012. “Substance use Patterns Among High-Risk American Indians/Alaska Natives in Los Angeles County.” American Journal on Addictions 21 (5): 445–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, and Johnson CL. 2012. “Mental Health and Substance Abuse Characteristics Among a Clinical Sample of Urban American Indian/Alaska Native Youths in a Large California Metropolitan Area: A Descriptive Study.” Community Mental Health Journal 48 (1): 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dickerson DL, Johnson CL, Castro C, Naswood E, and Leon JMP. 2012. “CommUNITY Voices: Integrating Traditional Healing Services for Urban American Indians/Alaska Natives in Los Angeles County.” In Learning Collaborative Summary Report,1–42. Los Angeles, Calif.: Los Angeles County Department of Mental Health. [Google Scholar]
- Duran E, and Duran B. 1995. Native American Post-Colonial Psychology. New York, NY: Suny Press. [Google Scholar]
- Gonzalez-Barrera A, and Lopez MH. 2015. “Is being Hispanic a matter of race, ethnicity or both?.” http://pewrsr.ch/1egbvPL.
- Gossage JP, Barton L, Foster L, Etsitty L, LoneTree C, Leonard C, and May PA. 2003. “Sweat Lodge Ceremonies for Jail-Based Treatment.” Journal of Psychoactive Drugs 35 (1): 33–42. [DOI] [PubMed] [Google Scholar]
- Hodder RK, Freund M, Wolfenden L, Bowman J, Nepal S, Dray J, Kingsland M, Yoong SL, and Wiggers J. 2017. “Systematic Review of Universal School-Based ‘Resilience’ Interventions Targeting Adolescent Tobacco, Alcohol or Illicit Substance Use: A Meta-Analysis.” Preventive Medicine 100: 248–268. [DOI] [PubMed] [Google Scholar]
- James MA 1992. The State of Native America: Genocide, Colonization, and Resistance Cambridge, MA: South End Press. [Google Scholar]
- Jernigan VB, D’Amico EJ, and Kaholokula J. Keawe‘aimoku. 2018. “Prevention Research with Indigenous Communities to Expedite Dissemination and Implementation Efforts.” Prevention Science. [DOI] [PMC free article] [PubMed]
- Jernigan VB, Peercy M, Dannielle Branam, Saunkeah B, Wharton D, Winkleby M, Lowe J, et al. 2015. “Beyond Health Equity: Achieving Wellness Within American Indian and Alaska Native Communities.” American Journal of Public Health Suppl 3: S376–S379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston LD, Miech RA, O’Malley PM, Bachman JG, Schulenberg JE, and Patrick ME. 2018. Monitoring the Future National Survey Results on Drug Use: 1975–2017: Overview, key Findings on Adolescent Drug Use Ann Arbor, MI: Institute for Social Research, The University of Michigan. [Google Scholar]
- Kaufman CE, Black K, Keane EM, Big Crow CK, Shangreau C, Arthur-Asmah R, Keith C, Morse B, Schaffer G, and Tuitt N. 2014. “Planning for a Group-Randomized Trial with American Indian Youth.” Journal of Adolescent Health Care 54 (3): S59–S63. [DOI] [PubMed] [Google Scholar]
- Kelly MJ, Dunstan FD, Lloyd K, and Fone DL. 2008. “Evaluating Cutpoints for the MHI-5 and MCS Using the GHQ-12: A Comparison of Five Different Methods.” BMC Psychiatry 8 (10), doi:10.1186/471–244x-8–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis S, Hodge D, Ayers SL, Brown EF, and Marsiglia FF. 2011. “Spirituality and Religion: Intertwined Protective Factors for Substance use among Urban American Indian Youth.” The American Journal of Drug and Alcohol Abuse 38 (5): 444–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulis S, Wagaman MA, Tso C, and Brown EF. 2013. “Exploring Indigenous Identities of Urban American Indian Youth of the Southwest.” Journal of Adolescent Research 28 (3): 271–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liebler CA, Porter SA, Fernandez LA, Noon JM, and Ennis SR. 2017. “America’s Churning Races: Race and Ethnicity Response Changes Between Census 2000 and the 2010 Census.” Demography 54: 259–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meredith LS, Ewing BA, Stein BS, Shadel WG, Holliday S. Brooks, Parast L, and D’Amico EJ. 2018. “Influence of Mental Health and Alcohol or Other Drug Use Risk on Adolescent Reported Care Received in Primary Care Settings.” BMC Family Practice 19 (1): 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miech RA, Johnston LD, O’Malley PM, Bachman JG, and Schulenberg JE. 2016. Monitoring the Future National Survey Results on Drug Use, 1975–2015: Volume I, Secondary School Students. Ann Arbor: Institute for Social Research, The University of Michigan. [Google Scholar]
- Minkler M, and Wallerstein N. 2011. Community-Based Participatory Research for Health: From Process to Outcomes. Hoboken, New Jersey: John Wiley & Sons. [Google Scholar]
- Moran R. James, Fleming Candace M., Somervell Philip, and Manson Spero M.. 1999. “Measuring Bicultural Ethnic Identity Among American Indian Adolescents: A Factor Analytic Study.” Journal of Adolescent Research 14 (4): 405–426. [Google Scholar]
- Nishina A, Bellmore A, Witkow MR, and Nylund-Gibson K. 2010. “Longitudinal Consistency of Adolescent Ethnic Identification Across Varying School Ethnic Contexts.” Developmental Psychology 46 (6): 1389–1401. [DOI] [PubMed] [Google Scholar]
- Norris T, Vines PL, and Hoeffel EM. 2012. “The American Indian and Alaska Native population: 2010 census briefs.” http://www.census.gov/prod/cen2010/briefs/c2010br-10.pdf.
- Norton IM, and Manson SM. 1996. “Research in American Indian and Alaska Native Communities: Navigating the Cultural Universe of Values and Process.” Journal of Consulting and Clinical Psychology 64: 856–860. [DOI] [PubMed] [Google Scholar]
- Phinney JS, and Ong AD. 2007. “Conceptualization and Measurement of Ethnic Identity: Current Status and Future Directions.” Journal of Counseling Psychology 54 (3): 271–281. [Google Scholar]
- Ponterotto JG, Gretchen D, Utsey SO, Stracuzzi T, and Saya R. 2003. “The Multigroup Ethnic Identity Measure (MEIM): Psychometric Review and Further Validity Testing.” Educational and Psychological Measurement 63 (3): 502–515. doi:10.1177/0013164403063003010. [Google Scholar]
- Quintana SM 2007. “Racial and Ethnic Identity: Developmental Perspectives and Research.” Journal of Counseling Psychology 54 (3): 259–270. [Google Scholar]
- Rutman, Shira, Park Alice, Castor Mei, Taualii Maile, and Forquera Ralph. 2008. “Urban American Indian and Alaska Native Youth: Youth Risk Behavior Survey 1997–2003.” Maternal and Child Health 12: S76–S81. [DOI] [PubMed] [Google Scholar]
- SAMHSA. 2016. Results From the 2015 National Survey on Drug Use and Health: Detailed Tables. Rockville, MD: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. https://www.samhsa.gov/data/sites/default/files/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015/NSDUH-DetTabs-2015.pdf. [Google Scholar]
- Schweigman K, Soto C, Wright S, and Unger J. 2011. “The Relevance of Cultural Activities in Ethnic Identity Among California Native American Youth.” Journal of Psychoactive Drugs 43 (4): 343–348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Wills TA, Emery NN, and Marks RM. 2015. “Quantifying Alcohol Consumption: Self-Report, Transdermal Assessment, and Prediction of Dependence Symptoms.” Addictive Behaviors 50: 205–212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart AL, Ware JE, Sherbourne CD, and Wells KB. 1992. “Psychological Distress/Well-Being and Cognitive Functioning Measures.” In Measuring Functioning and Well-Being: The Medical Outcomes Study Approach, edited by Stewart A, and Ware JE, 102–142. Durham, NC: Duke University Press. [Google Scholar]
- Stumblingbear-Riddle G, and Romans JSC. 2012. “Resilience Among Urban American Indian Adolescents: Exploration Into the Role of Culture, Self-Esteem, Subjective Well-Being, and Social Support.” American Indian Alaska Native Mental Health Research 19 (2): 1–19. [DOI] [PubMed] [Google Scholar]
- US Census Bureau. 2017. “Quick Facts: California” https://www.census.gov/quickfacts/CA.
- Waller MA, and Okamoto SK. 2003. “Resiliency Factors Related to Substance use/Resistance: Perceptions of Native Adolescents of the Southwest.” The Journal of Sociology & Social Welfare 30 (4): 79–94. [Google Scholar]
- Walters, Karina. 2009. “Lessons from the Field: Race, Culture and Children’s Mental Health.” In Center for Excellence in Children’s Mental Health. University of Minnesota. [Google Scholar]
- Ware JE, Kosinski M, and Keller SD. 1996. “A 12-Item Short Form Health Survey: Construction of Scales and Preliminary Tests.” Medical Care 34: 220–233. [DOI] [PubMed] [Google Scholar]
- West AE, Williams E, Suzukovich E, Strangeman K, and Novins D. 2012. “A Mental Health Needs Assessment of Urban American Indian Youth and Families.” American Journal of Community Psychology 49: 441–453. [DOI] [PubMed] [Google Scholar]
- Whitbeck BL, Chen X, Hoyt DR, and Adams GW. 2004. “Discrimination, Historical Loss and Enculturation: Culturally Specific Risk and Resiliency Factors for Alcohol Abuse Among American Indians.” Journal of Studies on Alcohol & Drugs 65: 409–418. [DOI] [PubMed] [Google Scholar]
- Zaslavsky, Alan M, Ayanian John Z., and Zaborski Lawrence B.. 2012. “The Validity of Race and Ethnicity in Enrollment Data for Medicare Beneficiaries.” Health Services Research 47 (3): 1300–1321. [DOI] [PMC free article] [PubMed] [Google Scholar]