Abstract
Background:
Diabetes is considered a risk factor for myocardial infarction. However, we have previously found that diabetes was not a short-term risk factor for myocardial infarction in the absence of obstructive coronary artery disease.
Methods:
We conducted a cohort study of patients undergoing coronary angiography from 2003 to 2012 and followed them by cross-linking Danish health registries. Patients were stratified according to coronary artery disease and diabetes. Endpoints included myocardial infarction, cardiac death, all-cause death and coronary revascularization.
Results:
86,202 patients were included in total (diabetes: n = 12,652). Median follow-up was 8.8 years. Using patients with neither coronary artery disease nor diabetes as reference (cumulative myocardial infarction incidence 2.6%), the risk of myocardial infarction was low and not substantially increased for patients with diabetes alone (3.2%; hazard ratio 1.202, 95% confidence interval 0.996−1.451), was increased for patients with coronary artery disease alone (9.3%; hazard ratio 2.75, 95% confidence interval 2.52−3.01) and was highest for patients with both coronary artery disease and diabetes (12.3%; hazard ratio 3.79, 95% confidence interval 3.43−4.20). Similar associations were observed for cardiac death and coronary revascularization.
Conclusion:
Diabetes patients without coronary artery disease by coronary angiography have a low risk of myocardial infarction, not substantially increased compared to patients with neither coronary artery disease nor diabetes. In the presence of coronary artery disease, however, diabetes increases the risk of myocardial infarction.
Keywords: Epidemiology, diabetes mellitus, coronary angiography, coronary disease, death
Introduction
Coronary artery disease (CAD) is a major cause of morbidity and mortality in patients with diabetes.1 Guidelines therefore recommend management of cardiovascular risk factors, including lifestyle interventions and treatment with statins, anti-hypertensive agents, specific glucose-lowering medications and consideration of antiplatelet therapy in high- and very high-risk diabetic patients.1,2
Haffner et al.3 reported that diabetes patients without prior myocardial infarction (MI) had a risk of MI similar to non-diabetes patients with previous MI. Subsequent studies, however, demonstrated that the impact of diabetes on a future MI was probably overestimated in the study by Haffner et al,3 but remained higher than observed in non-diabetes comparison groups.4,5 We have recently reported that diabetes patients had the same risk of MI as non-diabetes patients in the absence of obstructive CAD ascertained by either coronary angiography (CAG) or coronary computed tomography angiography (CCTA).6,7 However, these studies were limited by moderate follow-up periods (median of 4.1 years in the CAG study), lack of knowledge concerning diabetes type, diabetes duration and potential impact of coronary revascularization. In this updated cohort, we have included these data and have extended follow-up to 11 years. Our main objective was to examine whether the risk of MI remained similar in diabetes and non-diabetes patients in the absence of angiographically significant CAD.
Methods
Data sources
Each Danish resident is allocated a unique and permanent 10-digit personal identifier at birth or upon immigration. This identifier is used in every Danish health registry and facilitates accurate long-term follow-up data with minimal risk of loss to follow-up. The Western Denmark Heart Registry (WDHR) is a clinical database covering data on all patients referred for diagnostic, invasive and cardiac procedures in Western Denmark since 1999 (approximately 3.3 million inhabitants).8,9 The WDHR contains information on patient and procedural characteristics, including >240,000 CAGs with detailed description of the presence and extent of CAD. Besides the WDHR, we used the following databases: the Danish Civil Registration System, which records data on all Danish residents’ vital status (dead, alive, or emigrated); the Danish National Patient Registry, which collects data on all inpatient and outpatient hospital diagnoses and procedure codes; the Danish Register of Causes of Death, which collects causes of death of all Danish residents; and the Danish National Prescription Registry, which provides data on all reimbursed prescriptions redeemed at Danish pharmacies since 1994.10–14
CAD
CAD status was ascertained from the WDHR. CAD was defined as obstructive CAD, that is, ⩾1 coronary artery with ⩾50% angiographic lumen narrowing or as diffuse CAD, that is, <50% stenosis in >1 coronary artery. No CAD was defined as no stenosis in all coronary arteries or mild angiographic lumen narrowing (<50%) in a single coronary artery.
Diabetes
Diabetes patients were identified as follows: insulin ± oral diabetes treatment, oral diabetes treatment, or non-pharmacological dietary treated diabetes at the time of CAG as registered in the WDHR; redemption of ⩾1 prescription(s) for diabetes medication within 6 months before and 1 month after CAG; and/or a diagnosis of diabetes registered in the Danish National Registry prior to CAG. Diabetes duration was classified according to date of first redemption of diabetes medication as recorded in the Danish National Prescription Registry (and thus per definition not available for non-pharmacological dietary treated diabetes). Since the Danish National Prescription Registry was established in 1994 and patients were included from 2003, we chose to classify diabetes duration in categories of <5, 5−10 and >10 years. Type 1 diabetes patients were defined as patients redeeming an insulin prescription within 6 months before and 1 month after CAG and no history of redemption of non-insulin diabetes prescription. Type 2 diabetes patients were defined as patients redeeming a non-insulin diabetes prescription ± insulin treatment within 6 months before and 1 month after CAG or as patients registered in the WDHR with non-pharmacological dietary treated diabetes. Anatomical Therapeutic Chemical (ATC) codes for diabetes medications are provided in the Supplemental Table S1.
Patient selection
All patients with a CAG registered in the WDHR between 1 January 2003 and 31 December 2012 were included in the study (Figure 1). For patients undergoing >1 CAG during the study period, the first CAG was used as the index procedure. Patients aged <18 years and patients with missing CAD status were excluded. To reduce the risk of CAD misclassification, we excluded all patients with a previous MI, percutaneous coronary intervention (PCI) and/or coronary artery bypass grafting. Patients with <30 days of follow-up also were excluded.
Figure 1.
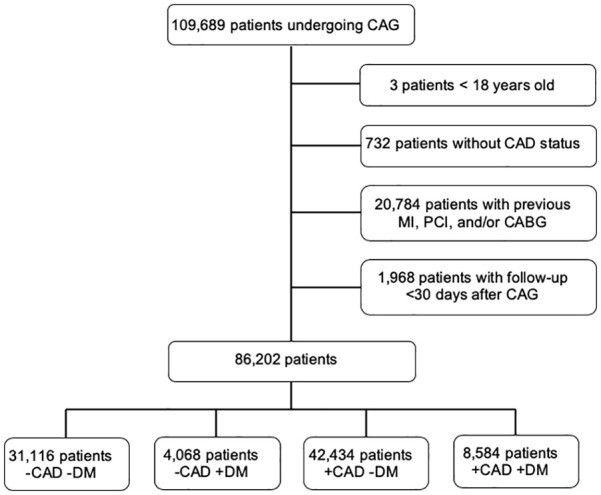
Flowchart of patients undergoing coronary angiography in Western Denmark between 1 January 2003 and 31 December 2012.
CABG: coronary artery bypass grafting; CAD: coronary artery disease; CAG: coronary angiography; DM: diabetes mellitus; MI: myocardial infarction; PCI: percutaneous coronary intervention.
Medication
Records of treatment with insulin, non-insulin diabetes medications, statins, β-blockers, angiotensin-converting enzyme (ACE) inhibitors, angiotensin II receptor blockers (ARB), calcium channel blockers, thiazide diuretics, aspirin, adenosine diphosphate (ADP) receptor inhibitors, vitamin K antagonists (VKA) and non-vitamin K oral anticoagulants (NOAC) were obtained from the Danish National Prescription Registry (Supplemental Table S1).14 Medical treatment was defined as reimbursement of a redeemed prescription between 6 months before and 1 month after the date of the index CAG.
MI
MI diagnoses were obtained from the Danish National Patient Registry using the diagnosis codes provided in Supplemental Table S2.11,12
Cardiac death
Cardiac death was defined as death caused by ischemic heart disease, cardiac arrest with unspecified cause, ventricular tachycardia or other specified cardiac arrhythmias, heart failure, sudden death with unspecified cause or unattended death with unspecified cause, as recorded on death certificates from the Danish Register of Causes of Death (Supplemental Table S3).13
All-cause death
Patients’ vital status (dead, alive or emigrated) was provided from the Danish Civil Registration System.10
Coronary revascularization
Coronary revascularization was ascertained from the Danish National Patient Registry and was defined as any PCI or coronary artery bypass grafting procedure >90 days after the index CAG. Follow-up began 90 days after the index CAG to exclude coronary revascularizations performed as a result of the CAG findings.
Comorbidity
Comorbidities were evaluated using a modified Charlson comorbidity index score (excluding ‘diabetes’ and ‘diabetes with end-organ damage’) based on International Classification of Diseases (ICD)-10 codes registered in the Danish National Patient Registry (Supplemental Table S2).15 We used a full look-back period of patient history before the date of the index CAG.
Statistical analyses Follow-up began 30 days after the index CAG except for patients undergoing coronary revascularization, for whom follow-up began 90 days after CAG, and continued until death, emigration or end of follow-up (31 December 2018), whichever occurred first. We estimated event rates for each endpoint per 100 person-years and constructed cumulative incidence proportion curves corresponding to the 75th percentile of follow-up. Cumulative incidence proportions of MI, cardiac death and coronary revascularization were estimated accounting for the competing risk of death.16 We used Cox proportional hazard regression to estimate unadjusted and adjusted hazard ratios (HRs) of MI, cardiac death, and all-cause death, using patients with neither CAD nor diabetes as reference. The assumption of proportional hazards (examined by log-log plot) was not met for coronary revascularization. Therefore, we used modified Poisson regression, with the event as the outcome and the natural log of person-years as the offset, to estimate unadjusted and adjusted incidence rate ratios (IRRs) of coronary revascularization.17 Each endpoint was adjusted for age, sex, hypertension, active smoking, previous ischemic stroke, previous peripheral artery disease (PAD), procedural priority (acute, subacute or elective CAG), year of index CAG, statin treatment, oral anticoagulant treatment (VKA and/or NOAC), and antiplatelet treatment (aspirin and/or ADP receptor inhibitor). For coronary revascularization, we further adjusted for coronary revascularization <90 days after CAG. When calculating HRs and IRRs, the maximum follow-up time was 11 years. We used multiple imputations with chained equations to impute missing values for smoking status generating 11 imputed data sets (11% missing values). We performed subgroup analyses limited to either patients with type 1 diabetes (n = 1259) or patients with type 2 diabetes (n = 11,393) provided in Supplemental Tables S4 and S5, respectively. We also performed subgroup analyses restricted to male patients (Supplemental Table S6) or female patients (Supplemental Table S7). We tested for interaction between sex and diabetes/CAD status. p < 0.05 was considered significant. Stata/MP software version 15.1 (StataCorp, College Station, Texas, USA) was used for all statistical analyses. The study was approved by the Danish Data Protection Agency (record no. 1-16-02-193-18).
Results
A total of 86,202 patients were included in the study (Figure 1). Of these, 31,116 (36.1%) patients had neither CAD nor diabetes, 4068 (4.7%) had diabetes alone, 42,434 (49.2%) had CAD alone, and 8584 (10.0%) had both CAD and diabetes. Median follow-up time was 8.8 years (Q1−Q3: 6.6−11.5). Two patients were lost during follow-up and 368 patients emigrated during follow-up and were censored from that date.
Baseline characteristics
Patients with CAD were older, more often male, and were characterized by higher proportions of active smoking, peripheral artery disease, and treatment with statins, β-blockers, aspirin and ADP inhibitors (Table 1). Furthermore, patients with CAD were more likely to undergo acute CAG.
Table 1.
Baseline patient characteristics.
| −CAD −DM (n = 31,116) | −CAD +DM (n = 4068) | +CAD −DM (n = 42,434) | +CAD +DM (n = 8584) | |
|---|---|---|---|---|
| Male (%) | 49.2 | 51.3 | 69.8 | 69.4 |
| Median age (years) (IQR) | 60 (51–68) | 61 (53–69) | 66 (58–74) | 67 (59–74) |
| Median follow-up (years) (IQR) | 9.4 (7.1–11.9) | 8.4 (6.4–11.0) | 8.7 (6.5–11.3) | 7.7 (5.3–10.3) |
| Active smoker (%)a | 22.7 | 20.3 | 32.5 | 25.8 |
| Median body mass index (kg/m2) (IQR) | 26 (23–29) | 30 (26–35) | 26 (24–29) | 29 (25–32) |
| Type 2 DM (%) | – | 90.9 | – | 89.7 |
| DM durationb | ||||
| 0–5 years (%) | – | 59.1 | – | 52.2 |
| 5–10 years (%) | – | 20.0 | – | 20.5 |
| >10 years (%) | – | 20.9 | – | 27.3 |
| Cardiovascular comorbidity | ||||
| Hypertension (%) | 47.4 | 76.6 | 53.9 | 79.0 |
| Previous heart failure (%) | 11.8 | 16.6 | 12.0 | 17.5 |
| Previous ischemic stroke (%) | 1.3 | 3.3 | 2.0 | 4.2 |
| Previous peripheral artery disease (%) | 2.2 | 3.6 | 5.1 | 10.5 |
| Medical treatment | ||||
| Insulin (%) | – | 29.5 | – | 33.0 |
| Non-insulin diabetes medication | – | 60.1 | – | 61.2 |
| Metformin (%) | – | 50.0 | – | 48.1 |
| Sulfonylurea (%) | – | 23.4 | – | 28.7 |
| GLP-1 analogue (%) | – | 2.5 | – | 1.9 |
| DPP-4 inhibitor (%) | – | 3.4 | – | 3.2 |
| Glitazone (%) | – | 1.0 | – | 1.3 |
| Statin (%) | 43.1 | 72.1 | 86.3 | 88.0 |
| β-blocker (%) | 51.4 | 56.3 | 76.3 | 73.7 |
| ACE inhibitor (%) | 28.2 | 47.1 | 37.1 | 54.3 |
| ARB (%) | 12.8 | 28.8 | 14.1 | 28.8 |
| Calcium channel blocker (%) | 24.5 | 35.2 | 28.6 | 40.6 |
| Thiazide diuretic (%) | 17.0 | 22.3 | 17.5 | 22.7 |
| Aspirin (%) | 54.9 | 67.2 | 86.1 | 85.7 |
| ADP receptor inhibitor (%) | 5.3 | 5.0 | 57.9 | 47.4 |
| VKA (%) | 13.7 | 15.5 | 9.1 | 11.5 |
| NOAC (%) | 0.3 | 0.4 | 0.3 | 0.3 |
| Modified Charlson comorbidity index score | ||||
| 0 (%) | 75.0 | 71.9 | 76.6 | 74.4 |
| 1 (%) | 15.6 | 19.0 | 13.3 | 16.7 |
| 2 (%) | 6.4 | 8.1 | 6.6 | 7.8 |
| ≥ 3 (%) | 3.1 | 1.0 | 3.5 | 1.1 |
| Procedural priority | ||||
| Elective/subacute (%) | 92.5 | 94.4 | 72.2 | 82.9 |
| Acute (%) | 7.5 | 5.6 | 27.8 | 17.1 |
| Procedural indication | ||||
| STEMI (%) | 4.3 | 3.0 | 25.7 | 15.0 |
| NSTEMI (%) | 8.1 | 7.1 | 18.4 | 18.0 |
| Unstable AP (%) | 2.1 | 2.0 | 1.9 | 2.1 |
| Stable AP (%) | 44.7 | 48.4 | 36.9 | 43.7 |
| Valvular disease (%) | 12.3 | 10.3 | 5.8 | 6.8 |
| Cardiomyopathy (%) | 8.5 | 9.4 | 3.1 | 5.5 |
| Other (%) | 20.0 | 19.8 | 8.2 | 8.9 |
ACE: angiotensin-converting enzyme; AP: angina pectoris; ARB: angiotensin-II receptor blocker; CAD: coronary artery disease; DM: diabetes mellitus; DPP-4 inhibitor: dipeptidyl peptidase-4 inhibitor; GLP-1 analogue: glucagon-like peptide-1 analogue; IQR: interquartile range; NOAC: non-vitamin K oral anticoagulant; NSTEMI: non-ST-elevation myocardial infarction; STEMI: ST-elevation myocardial infarction; VKA: vitamin K antagonist.
11% missing values for smoking.
11% missing values for DM duration.
Patients with diabetes more frequently had hypertension, heart failure, previous ischemic stroke, and were more often treated with ACE inhibitors, ARBs, calcium channel blockers, and thiazide diuretics. Diabetes medication use was similar in diabetes patients with and without CAD and metformin treatment was the most frequently used diabetes medication. Distribution of diabetes type was similar in diabetes patients with and without CAD, with approximately 90% of patients having type 2 diabetes. Diabetes duration was longer in patients with CAD.
Clinical endpoints
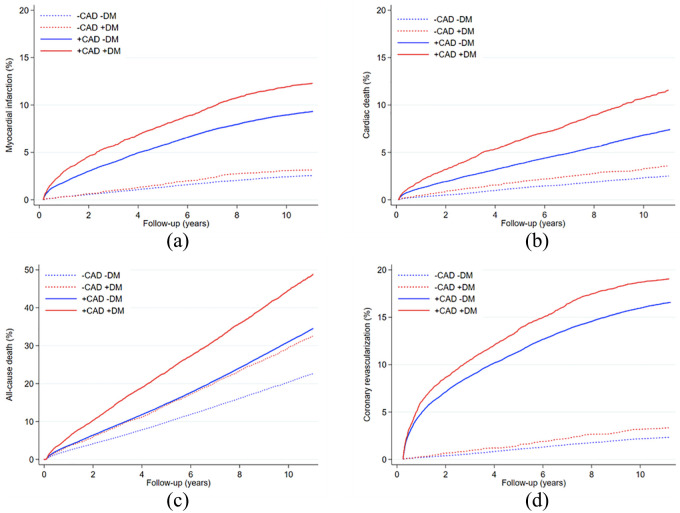
During the follow-up period, 5935 patients had a MI, 23,436 patients died (4455 from cardiac causes) and 9530 patients underwent coronary revascularization (Table 2). Cumulative incidence curves for each endpoint are shown in Figure 2(a)–(d).
Table 2.
Number of events and risk of myocardial infarction, cardiac death, all-cause death and coronary revascularization in patients with and without diabetes stratified by coronary artery disease.
| Events (n) | Rate per 100 person-years (95% CI) | CIP (95% CI) | Risk differencea (95% CI) | Unadjusted HR (95% CI) | Adjusted HRb (95% CI) | |
|---|---|---|---|---|---|---|
| Myocardial infarction | ||||||
| −CAD −DM (reference) | 795 | 0.24 (0.22–0.25) | 2.55% (2.39–2.74) | Reference | 1 | 1 |
| −CAD +DM | 128 | 0.29 (0.24–0.35) | 3.15% (2.64–3.72) | 0.60 (0.04–1.16) | 1.23 (1.02–1.49) | 1.202 (0.996–1.451) |
| +CAD −DM | 3957 | 0.90 (0.87–0.93) | 9.33% (9.03–9.59) | 6.77 (6.44–7.10) | 3.79 (3.51–4.09) | 2.75 (2.52–3.01) |
| +CAD +DM | 1055 | 1.21 (1.14–1.29) | 12.29% (11.64–13.03) | 9.74 (9.05–10.43) | 5.09 (4.64–5.58) | 3.79 (3.43–4.20) |
| Cardiac death | ||||||
| −CAD −DM (reference) | 689 | 0.26 (0.24–0.28) | 2.51% (2.32–2.70) | Reference | 1 | 1 |
| −CAD +DM | 126 | 0.39 (0.33–0.46) | 3.57% (3.00–4.25) | 1.06 (0.39–1.73) | 1.51 (1.25–1.82) | 1.65 (1.36–2.00) |
| +CAD −DM | 2768 | 0.81 (0.78–0.84) | 7.41% (7.14–7.69) | 4.90 (4.57–5.23) | 3.14 (2.88–3.41) | 2.36 (2.15–2.60) |
| +CAD +DM | 872 | 1.40 (1.31–1.50) | 11.58% (10.84–12.34) | 9.07 (8.33–9.81) | 5.42 (4.90–5.99) | 4.17 (3.73–4.67) |
| All-cause death | ||||||
| −CAD −DM (reference) | 6129 | 2.29 (2.23–2.35) | 22.80% (22.28–23.33) | Reference | 1 | 1 |
| −CAD +DM | 1117 | 3.45 (3.25–3.66) | 32.63% (30.96–34.36) | 9.83 (8.04–11.62) | 1.52 (1.43–1.62) | 1.67 (1.57–1.78) |
| +CAD −DM | 12,581 | 3.68 (3.61–3.74) | 34.77% (34.25–35.30) | 11.97 (11.22–12.72) | 1.62 (1.57–1.67) | 1.35 (1.30–1.40) |
| +CAD +DM | 3609 | 5.81 (5.63–6.01) | 49.14% (47.89–50.40) | 26.34 (25.09–27.59) | 2.58 (2.48–2.69) | 2.17 (2.08–2.28) |
| Unadjusted IRR (95% CI) | Adjusted IRRb (95% CI) | |||||
| Coronary revascularization >90 days after index coronary angiography | ||||||
| −CAD −DM (reference) | 730 | 0.22 (0.20–0.23) | 2.35% (2.18–2.52) | Reference | 1 | 1 |
| −CAD +DM | 136 | 0.31 (0.26–0.37) | 3.34% (2.82–3.93) | 0.99 (0.42–1.57) | 1.43 (1.19–1.72) | 1.32 (1.09–1.58) |
| +CAD −DM | 7029 | 1.70 (1.66–1.74) | 16.56% (16.21–16.92) | 14.21 (13.82–14.60) | 7.88 (7.30–8.51) | 6.62 (6.03–7.28) |
| +CAD +DM | 1635 | 2.01 (1.91–2.11) | 19.05% (18.22–19.88) | 16.70 (15.88–17.52) | 9.29 (8.51–10.15) | 7.72 (6.95–8.57) |
CAD: coronary artery disease; CIP: cumulated incidence proportion; DM: diabetes mellitus; IRR: incidence rate ratio; HR: hazard ratios; CI: confidence interval.
Maximum follow-up of 11 years.
Adjusted for age, sex, hypertension, active smoking, previous ischemic stroke, peripheral artery disease, procedural priority, year of index coronary angiography, statin treatment, oral anticoagulant treatment, and antiplatelet treatment, using patients with neither CAD nor DM as reference. IRR was further adjusted for coronary revascularization < 90 days after the index coronary angiography.
Figure 2.
Cumulative incidences of (a) myocardial infarction, (b) cardiac death, (c) all-cause death and (d) coronary revascularization in patients with diabetes mellitus (+DM) and without (−DM) diabetes stratified by the presence (+CAD) or absence (−CAD) of coronary artery disease.
Event rates for MI, cardiac death, all-cause death, and coronary revascularization were lowest in patients with neither CAD nor diabetes, followed by patients with diabetes alone, patients with CAD alone, and highest in patients with both CAD and diabetes (Table 2). Using patients with neither CAD nor diabetes as reference (cumulative MI incidence 2.6%), the risk of MI was low and not substantially increased in patients with diabetes alone (3.2%; HR 1.202, 95% CI 0.996−1.451), increased in patients with CAD alone (9.3%; HR 2.75, 95% CI 2.52−3.01) and further increased in patients with both CAD and diabetes (12.3%; HR 3.79, 95% CI 3.43−4.20). Similar associations were observed for cardiac death and coronary revascularization, although the risk was significantly increased in patients with diabetes alone compared to patients with neither CAD nor diabetes (Table 2). Still, the absolute risk of cardiac death and coronary revascularization remained low in patients without CAD regardless of diabetes status compared to patients with CAD alone and patients with both CAD and diabetes. For all-cause death, the risk was lowest in patients with neither CAD nor diabetes (reference), followed by patients with CAD alone (HR 1.35, 95% CI 1.30−1.40), patients with diabetes alone (HR 1.67, 95% CI 1.57−1.78), and highest in patients with both CAD and diabetes (HR 2.17, 95% CI 2.08−2.28).
The results were robust when stratified for type of diabetes (Tables S4 S5) or sex (Tables S6 S7). We did not see any interaction between sex and status of diabetes/CAD for MI (p = 0.71). There was no interaction with sex among diabetes patients without CAD either (p = 0.35).
Discussion
In this study, we extend our previous shorter term assessments demonstrating that diabetes patients without CAD by CAG or CCTA have a low risk of MI, not substantially increased compared to patients with neither CAD nor diabetes.6,7 In the current evaluation with prolonged follow-up, we found that diabetes patients, commonly believed to have an increased risk of MI due to accelerated atherosclerosis, remained at low risk of MI for at least an 11 year period if they had no or mild CAD at the baseline evaluation. Diabetes patients with CAD, however, continued to have a much higher risk than patients with CAD alone. Thus, a single imaging assessment of the coronary arteries provides risk stratification that extends out to 11-year follow-up, even in an assumed high-risk diabetes population.
Our previous CAG study, based on the same patient cohort, was limited to a maximum follow-up of 7 years and the database did not include data on diabetes type, diabetes duration, and coronary revascularization following CAG.6 In this updated cohort, we have included such data and have extended our follow-up to 11 years, corresponding to the 75th percentile of follow-up. Approximately 90% of diabetes patients had type 2 diabetes, irrespective of CAD status. When we restricted our analyses to patients with either type 1 or type 2 diabetes, the results did not change. However, we found that diabetes duration was longer in diabetes patients with CAD than without CAD, also reflecting older age among the former. The Framingham Heart Study also demonstrated that long diabetes duration was associated with increased risk of CAD and cardiac death, independently of other coexisting risk factors.18 Our data further revealed the important distinction that very few diabetes patients without CAD develop significant CAD, as determined by MI event or coronary revascularization, during an 11-year follow-up.
In this study, the risk of MI between patients with diabetes alone versus those with neither diabetes nor CAD was borderline significant, that is, the 95% CI varied from 0.4% lower relative risk to a potential 45% increased relative risk. However, the absolute risk difference between diabetes alone and the reference group was 0.60% during the 11-year follow-up. This corresponds to an absolute risk increase in 0.05% per year, which is not considered clinically relevant. In comparison, the absolute risk difference was 7% when compared to patients with CAD alone and 10% when compared to patients with both CAD and diabetes.
We observed an increased risk of all-cause death in patients with diabetes alone compared to patients with neither CAD nor diabetes, which is not explained by increased risk of cardiac death alone. Beyond cardiac disease, diabetes is associated with other macrovascular complications such as stroke and peripheral artery disease. Hence, we have previously reported that diabetes patients without CAD had increased risk of ischemic stroke compared to patients with neither CAD nor diabetes (adjusted IRR 1.74, 95% CI, 1.42–2.15), although the risk was lower risk than in patients with CAD and diabetes combined.19 In addition, diabetes also adversely affects the microvasculature in multiple organs leading to complications such as kidney failure and peripheral neuropathy.20 Thus, the absence of CAD by CAG ensures an 11-year low risk of MI for diabetes patients, but it only provides moderate protection against macrovascular complications, such as stroke19 and possibly PAD, which could explain the observed increased mortality in diabetes patients. Furthermore, microvascular complications, particularly kidney failure, are strongly associated with mortality.21,22
Our findings are consistent with previous studies based on coronary examinations by CAG or CCTA.7,23 Saely et al.23 followed 750 CAG patients and stratified them according to presence (≥ 50% stenosis) of CAD and diabetes. After a mean follow-up of 2.2 years, diabetes alone was not an independent predictor of vascular events, while the risk of vascular events was incrementally higher in patients with CAD alone and in patients with both diabetes and CAD.23 As in our study, diabetes patients with CAD had a longer duration of diabetes than diabetes patients without CAD.23 Recently, we used CCTA to examine CAD severity in patients with and without diabetes (n = 48,731) with a median follow-up of 3.6 years.7 In the absence of CAD, diabetes patients had the same low risk of MI as non-diabetes patients (adjusted IRR 1.40, 95% CI 0.71−2.78).7 Hence, the long-term results in this study confirm previous shorter term CAG and CCTA studies. The potential clinical consequence is that screening for CAD may be used to differentiate diabetes patients with and without increased risk of cardiovascular events and guide prophylactic strategies. However, this concept warrants validation in prospective randomized trials.
Systematic screening for CAD in asymptomatic diabetes patients is controversial and currently not recommended due to lack of evidence.2,24 Only a single randomized clinical trial, the FACTOR 64 trial,25 has examined screening for CAD in asymptomatic diabetes patients (n = 900) using CCTA. The trial did not find screening beneficial in preventing adverse cardiac events at 4-year follow-up. However, the trial was limited by a lower than anticipated incidence of adverse events. Moreover, as randomization was performed before CCTA, a potential treatment effect was diluted by the inclusion of many low-risk patients. Based on our results, one should consider using CCTA for risk stratification followed by randomization of high-risk patients with CAD in order to avoid dilution of treatment effects. Following the FACTOR 64 trial, several large randomized control trials have demonstrated reductions in cardiovascular morbidity and mortality among patients with type 2 diabetes when treated with sodium-glucose cotransporter 2 inhibitors26,27 and glucagon-like peptide-1 analogues28,29 in addition to standard care. The emergence of these cardioprotective glucose-lowering agents further suggests a need for new prospective randomized trials with optimized medical intervention.
The absence of significant CAD appears to be a valid predictor of low cardiovascular risk. Though CAG does not rule out coronary atherosclerosis, our results confirm the usefulness of CAG to predict a low risk of MI for at least an 11-year period. A factor that may have contributed to the low long-term risk of MI is the high use of prophylactic medications in patients with diabetes. The landmark paper by Haffner et al.3 led to an intensified focus on prevention and management of cardiovascular risk factors among diabetes patients, including hypertension, dyslipidemia and smoking.30 Moreover, improved diabetes detection may have caused lead time bias and consequently a reduced relative risk, when comparing patients with and without diabetes. Accordingly, long-term cohort studies have demonstrated declining rates of diabetes-related cardiovascular morbidity and mortality within the last two decades.31–33 In this study, statin use and anti-hypertensive treatment were frequent among diabetes patients with and without CAD. This high level of preventive therapy may have lowered the diabetes-related risk of MI in our study.
Limitations
First, we did not have access to HbA1c and fasting glucose levels to define diabetes or to islet autoantibodies and C-peptide levels to classify diabetes type. However, we used various registries to minimize the risk of misclassification. Second, classification of CAD was based on visual angiographic assessment by the treating physician, which might have introduced some degree of inter-observer variation. Using the same classification, we have previously been able to identify patients at low-, intermediate- and high-cardiovascular risk.34 Another limitation to CAG is that the procedure does not describe plaque vulnerability and lesion morphology in the vessel wall. Third, asymptomatic myocardial ischaemia is more frequent in diabetes patients and silent MI’s may have lowered the observed MI rate in patients with diabetes.35
Conclusion
In conclusion, diabetes patients without CAD by CAG have a low risk of MI, not substantially increased compared to patients with neither CAD nor diabetes. In the presence of CAD, however, diabetes increases the risk of MI.
Supplemental Material
Supplemental material, Supplemental_Material for Diabetes is not a risk factor for myocardial infarction in patients without coronary artery disease: A study from the Western Denmark Heart Registry by Christine Gyldenkerne, Kevin KW Olesen, Pernille G Thrane, Morten Madsen, Troels Thim, Morten Würtz, Lisette O Jensen, Bent Raungaard, Per L Poulsen, Hans E Bøtker and Michael Maeng in Diabetes & Vascular Disease Research
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Christine Gyldenkerne  https://orcid.org/0000-0001-5904-7063
https://orcid.org/0000-0001-5904-7063
Data availability: The data sets generated during and/or analysed during this study are not publicly available due to Danish law on personal data.
Supplemental material: Supplemental material for this article is available online.
References
- 1. American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2019. Diabetes Care 2019; 42: S103–S123. [DOI] [PubMed] [Google Scholar]
- 2. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 2019; 41: 255–323. [DOI] [PubMed] [Google Scholar]
- 3. Haffner SM, Lehto S, Ronnemaa T, et al. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998; 339: 229–234. [DOI] [PubMed] [Google Scholar]
- 4. Evans JM, Wang J, Morris AD. Comparison of cardiovascular risk between patients with type 2 diabetes and those who had had a myocardial infarction: cross sectional and cohort studies. BMJ 2002; 324: 939–942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lee CD, Folsom AR, Pankow JS, et al. Cardiovascular events in diabetic and nondiabetic adults with or without history of myocardial infarction. Circulation 2004; 109: 855–860. [DOI] [PubMed] [Google Scholar]
- 6. Olesen KKW, Madsen M, Egholm G, et al. Patients with diabetes without significant angiographic coronary artery disease have the same risk of myocardial infarction as patients without diabetes in a real-world population receiving appropriate prophylactic treatment. Diabetes Care 2017; 40: 1103–1110. [DOI] [PubMed] [Google Scholar]
- 7. Olesen KKW, Riis AH, Nielsen LH, et al. Risk stratification by assessment of coronary artery disease using coronary computed tomography angiography in diabetes and non-diabetes patients: a study from the Western Denmark cardiac computed tomography registry. Eur Heart J Cardiovasc Imaging 2019; 20: 1271–1278. [DOI] [PubMed] [Google Scholar]
- 8. Schmidt M, Maeng M, Madsen M, et al. The Western Denmark Heart Registry: its influence on cardiovascular patient care. J Am Coll Cardiol 2018; 71: 1259–1272. [DOI] [PubMed] [Google Scholar]
- 9. Schmidt M, Maeng M, Jakobsen CJ, et al. Existing data sources for clinical epidemiology: The Western Denmark Heart Registry. Clin Epidemiol 2010; 2: 137–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Schmidt M, Pedersen L, Sorensen HT. The Danish civil registration system as a tool in epidemiology. Eur J Epidemiol 2014; 29: 541–549. [DOI] [PubMed] [Google Scholar]
- 11. Schmidt M, Schmidt SA, Sandegaard JL, et al. The Danish national patient registry: a review of content, data quality, and research potential. Clin Epidemiol 2015; 7: 449–490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health 2011; 39: 30–33. [DOI] [PubMed] [Google Scholar]
- 13. Juel K, Helweg-Larsen K. The Danish registers of causes of death. Dan Med Bull 1999; 46: 354–357. [PubMed] [Google Scholar]
- 14. Pottegard A, Schmidt SAJ, Wallach-Kildemoes H, et al. Data resource profile: the Danish national prescription registry. Int J Epidemiol 2017; 46: 798–798f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40: 373–383. [DOI] [PubMed] [Google Scholar]
- 16. Lambert PC. The estimation and modelling of cause-specific cumulative incidence functions using time-dependent weights. Stata J 2017; 17: 181–207. [PMC free article] [PubMed] [Google Scholar]
- 17. Zou G. A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004; 159: 702–706. [DOI] [PubMed] [Google Scholar]
- 18. Fox CS, Sullivan L, D’Agostino RB, et al. The significant effect of diabetes duration on coronary heart disease mortality: the Framingham heart study. Diabetes Care 2004; 27: 704–708. [DOI] [PubMed] [Google Scholar]
- 19. Olesen KKW, Madsen M, Gyldenkerne C, et al. Diabetes mellitus is associated with increased risk of ischemic stroke in patients with and without coronary artery disease. Stroke 2019; 50: 3347–3354. [DOI] [PubMed] [Google Scholar]
- 20. American Diabetes Association. 11. Microvascular complications and foot care: standards of medical care in diabetes-2019. Diabetes Care 2019; 42: S124–S138. [DOI] [PubMed] [Google Scholar]
- 21. Edfors R, Szummer K, Evans M, et al. Renal function is associated with long-term outcomes independent of degree of atherosclerosis: 6-year data from the Swedish coronary angiography and angioplasty registry. Eur Heart J Qual Care Clin Outcomes 2016; 2: 91–98. [DOI] [PubMed] [Google Scholar]
- 22. Fox CS, Matsushita K, Woodward M, et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: a meta-analysis. Lancet 2012; 380: 1662–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Saely CH, Aczel S, Marte T, et al. Cardiovascular complications in type 2 diabetes mellitus depend on the coronary angiographic state rather than on the diabetic state. Diabetologia 2004; 47: 145–146. [DOI] [PubMed] [Google Scholar]
- 24. American Diabetes Association. Standards of medical care in diabetes-2018 abridged for primary care providers. Clin Diabetes 2018; 36: 14–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Muhlestein JB, Lappe DL, Lima JA, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. Jama 2014; 312: 2234–2243. [DOI] [PubMed] [Google Scholar]
- 26. Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med 2015; 373: 2117–2128. [DOI] [PubMed] [Google Scholar]
- 27. Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2019; 380: 347–357. [DOI] [PubMed] [Google Scholar]
- 28. Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016; 375: 311–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016; 375: 1834–1844. [DOI] [PubMed] [Google Scholar]
- 30. Fox CS, Golden SH, Anderson C, et al. Update on prevention of cardiovascular disease in adults with type 2 diabetes mellitus in light of recent evidence: a scientific statement from the American heart association and the American diabetes association. Diabetes Care 2015; 38: 1777–1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Gregg EW, Li Y, Wang J, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med 2014; 370: 1514–1523. [DOI] [PubMed] [Google Scholar]
- 32. Gregg EW, Cheng YJ, Srinivasan M, et al. Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: an epidemiological analysis of linked national survey and vital statistics data. Lancet 2018; 391: 2430–2440. [DOI] [PubMed] [Google Scholar]
- 33. Rawshani A, Rawshani A, Franzen S, et al. Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med 2017; 376: 1407–1418. [DOI] [PubMed] [Google Scholar]
- 34. Gyldenkerne C, Olesen KKW, Madsen M, et al. Extent of coronary artery disease is associated with myocardial infarction and mortality in patients with diabetes mellitus. Clin Epidemiol 2019; 11: 419–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Koistinen MJ. Prevalence of asymptomatic myocardial ischaemia in diabetic subjects. BMJ 1990; 301: 92–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Supplemental_Material for Diabetes is not a risk factor for myocardial infarction in patients without coronary artery disease: A study from the Western Denmark Heart Registry by Christine Gyldenkerne, Kevin KW Olesen, Pernille G Thrane, Morten Madsen, Troels Thim, Morten Würtz, Lisette O Jensen, Bent Raungaard, Per L Poulsen, Hans E Bøtker and Michael Maeng in Diabetes & Vascular Disease Research