Abstract
South Asian (SA) countries have been fighting with the pandemic novel coronavirus disease 2019 (COVID-19) since January 2020. Earlier, the country-specific descriptive study has been done. Nevertheless, as transboundary infection, the border sharing, shared cultural and behavioral practice, effects on the temporal and spatial distribution of COVID-19 in SA is still unveiled. Therefore, this study has been revealed the spatial hotspot along with descriptive output on different parameters of COVID-19 infection. We extracted data from the WHO and the worldometer database from the onset of the outbreak up to 15 May, 2020. Europe has the highest case fatality rate (CFR, 9.22%), whereas Oceania has the highest (91.15%) recovery rate from COVID-19. Among SA countries, India has the highest number of cases (85,790), followed by Pakistan (38,799) and Bangladesh (20,065). However, the number of tests conducted was minimum in this region in comparison with other areas. The highest CFR was recorded in India (3.21%) among SA countries, whereas Nepal and Bhutan had no death record due to COVID-19 so far. The recovery rate varies from 4.75% in the Maldives to 51.02% in Sri Lanka. In Bangladesh, community transmission has been recorded, and the highest number of cases were detected in Dhaka, followed by Narayanganj and Chattogram. We detected Dhaka and its surrounding six districts, namely Gazipur, Narsingdi, Narayanganj, Munshiganj, Manikganj, and Shariatpur, as the 99% confidence-based hotspot where Faridpur and Madaripur district as the 95% confidence-based spatial hotspots of COVID-19 in Bangladesh. However, we did not find any cold spots in Bangladesh. We identified three hotspots and three cold spots at different confidence levels in India. Findings from this study suggested the “Test, Trace, and Isolation” approach for earlier detection of infection to prevent further community transmission of COVID-19.
Keywords: Case fatality rate, Dhaka, South Asia, Risk, Community transmission, Bangladesh
Highlights.
Scientific question
Whether temporal pattern and spatial hotspot might be crucial or not to dig out the key players for community transmission of the pandemic COVID-19 in South Asia?
Evidence before this study
Circulation of COVID-19 is evident among South Asian countries since February, 2020. The spatial and temporal patterns and trends of community transmission of the Pandemic COVID-19 in South Asia is still unveiled. Therefore, this study has been revealed the hotspot along with descriptive output on different parameters of COVID-19 infection.
New findings
This study identified the probable hotspots of COVID-19 in India and Bangladesh along with the variation in trends of transmission in different SA countries from specified clusters to intense community transmission.
Significance of the study
Findings from this study suggested “test, trace and isolation” approach for earlier detection of infection to prevent further community transmission of COVID-19. We should establish a potential early-warning system that could be used under non-outbreak condition to identify potential pandemic like disease X that has occurred and could resurface in the future.
Alt-text: Unlabelled Box
1. Introduction
The novel coronavirus disease 2019 (COVID-19) is an emerging infectious disease that has been declared a pandemic by the World Health Organization on March 11, 2020 [1]. This pandemic has spread over the world more than 210 countries globally [2] and infected almost 5.5 million people and about 0.35 million deaths worldwide as of 15 May 2020 [3]. The COVID-19 was caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), which was initially reported as a novel pneumonia of unknown etiology [4,5]. The massive movement of people from and between the Asian region and other parts of the world increased the geographical spreading of contagion during the outbreak [6]. However, in the beginning, the infection of COVID-19 was epidemic; the spread is becoming overwhelming and has all the required epidemiological principles for a pandemic [7]. Experience from China, Italy, and the United States demonstrates that COVID-19 can be devastative for the healthcare capacities of well-equipped nations as well [8].
Circulation of COVID-19 is evident among South Asian (SA) countries since February 2020. A large portion (24%) of the global population live in SA [9], and due to the low per capita income and the scope of the jobs, people from this region migrate to Europe, Middle East countries, China, and the USA [10]. Before banning international travel in SA countries, expatriates return to their homelands from abroad. This movement of peoples from their workplace to home countries and mingling with their families and communities initiated the outbreak in SA countries. The high population density in the SA region [11] increases the chance of fast community transmission in this area. Traditional culture and customs might be the core factor for community transmission in SA countries as people of different religions mostly celebrated their cultural activities (with big gathering), including wedding ceremony as well [12]. COVID-19 can be rapidly transmitted from person-to-person that makes this pandemic quite challenging to control. Rigorous testing and case-based interventions have so far formed the crucial piece of control efforts in some countries, such as Singapore and China [13]. However, due to scarce resources, trained personnel, and COVID-19 testing facilities in SA countries, it is difficult to control and prevent infection efficiently. Earlier, the country-specific descriptive study on COVID-19 has been reported. But, as transboundary infection, the border sharing, shared cultural and behaviour practice, effects on the temporal and spatial distribution of SARS-CoV-2 in SA is still unveiled.
Bangladesh has a total population of 164,649,824, where 1,265 people live per km2 area. This high population density predisposes the frequent transmission of the SARS-CoV-2 virus in this country [14]. Moreover, the country has not only a shortage of testing kits and trained personnel but also has inadequate healthcare facilities. To shape the government and stakeholders' decisions, we compiled and compared the epidemiological characteristics of COVID-19 from the different geographical regions, including SA countries, along with the test rate in those regions. We investigated the spatial pattern of COVID-19 and the trend of community transmission in SA countries, especially Bangladesh, by identifying the hotspot in Bangladesh and its closest neighbor, India.
2. Materials and methods
2.1. Data extraction
We extracted population data (total population of the affected countries in 2020) from the world population review database (https://www.worldometers.info/population). The database has been designed and updated by the global community recently. We extracted the number of new cases, the number of total cases, the total number of death, the total number of recovery, and the total tested population from the WHO database [15] and worldometer coronavirus databases (https://www.worldometers.info/coronavirus). WHO and worldometer coronavirus databases were designed and updated every day (real-time) for every parameter. Furthermore, the data about Bangladesh has been cross-checked with the government source. We included data from the beginning of the outbreak to 15 May 2020, for our analysis.
2.2. Data analysis
We inserted the data in MS-Excel 2013 (Microsoft Corporation, Redmond, WA 98052–6399 USA) for analysis. We produced epidemic curves, calculated case fatality rate (CFR = number of death by COVID-19/number of total positive cases×100%), and recovery rate (number of recovered/number of overall positive cases×100%) according to different regions. Moreover, we showed the number of tests conducted per million people for other geographical areas in the world, in a graph. In all the cases, we produced maps showing spatial distribution using ArcGIS software. We also calculated the infection rate and mortality rate of COVID-19 among different age and gender groups in Bangladesh. The linear and log-linear diagram of COVID-19 cases in different SA countries were presented graphically. Getis-Ord general G was performed for hotspot detection of COVID-19 in Bangladesh and India. The methods have been implemented for calculation, as described by Peeters, Zude [16].
3. Results
3.1. Epidemiological characteristics and test rate of COVID-19 in the world
Europe witnessed the highest CFR (9.22%) due to COVID-19 than other regions of the world. In contrast, the lowest CFR (1.38%) was recorded in the Oceania region. On the other hand, the recovery rate from COVID-19 was highest (91.15%) in the Oceania continent and lowest in the North American region (24.91%). In SA, just over 30% of COVID-19 patients recovered from this disease (case) (Fig. 1 ).
Fig. 1.
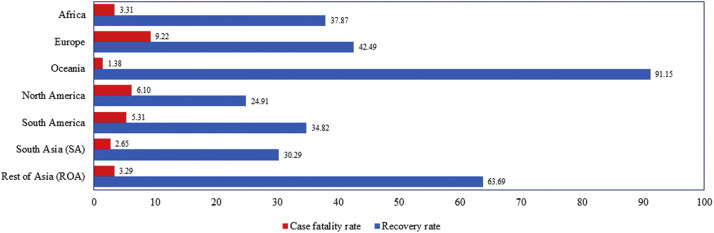
Case fatality rate and recovery rate of COVID-19 patients in different regions of the globe.
Europe did the highest number of tests per million population, followed by Oceania and North America. Africa and the South Asian region did the lowest quantity of tests per million people than others to confirm the COVID-19 infection (Fig. 2 ).
Fig. 2.
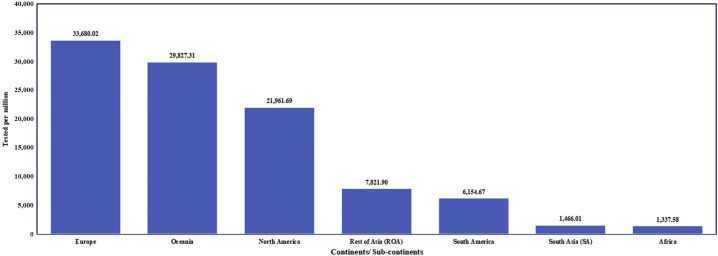
Tested population per 1 million for COVID-19 in different region across the globe.
3.2. Distribution and epidemiological characteristics of COVID-19 cases in SA countries (day basis)
A total of 150,514 people has been infected in SA countries, including Bangladesh, India, Pakistan, Sri Lanka, Afghanistan, Nepal, Bhutan, and the Maldives as of May 15, 2020. India has the highest number of cases (n = 85,784) followed by Pakistan (n = 37,218), Bangladesh (n = 20,065) and Afghanistan (n = 5,155). Other countries of SA have not crossed 1,000 cases yet. Very few cases were found in Nepal (n = 267) and Bhutan (n = 21) (Fig. 3, Fig. 4 ). Linear and log-linear distribution of COVID-19 cases among larger SA countries, including India, Pakistan, Afghanistan, and Bangladesh, the highest trend has been observed in India, followed by Pakistan, Bangladesh, and Afghanistan (Fig. 3). Contrarily, among the smaller countries of SA, the highest trend of COVID-19 cases has been reported in Sri Lanka, followed by Maldives, Nepal, and Bhutan.
Fig. 3.
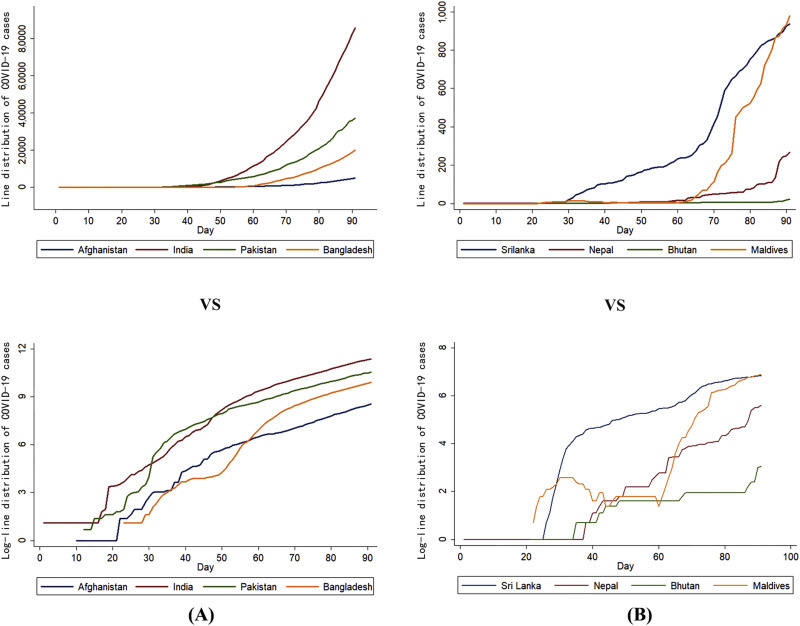
Linear (at the top) versus log-linear (at the bottom) distribution of COVID-19 cases from 15 February to 15 May (total = 91 days) in different SA countries. (A) Left pole: Afghanistan, India, Pakistan, and Bangladesh (scale in thousand); (B) Right pole: Sri Lanka, Nepal, Bhutan, and Maldives (scale in hundred).
Fig. 4.
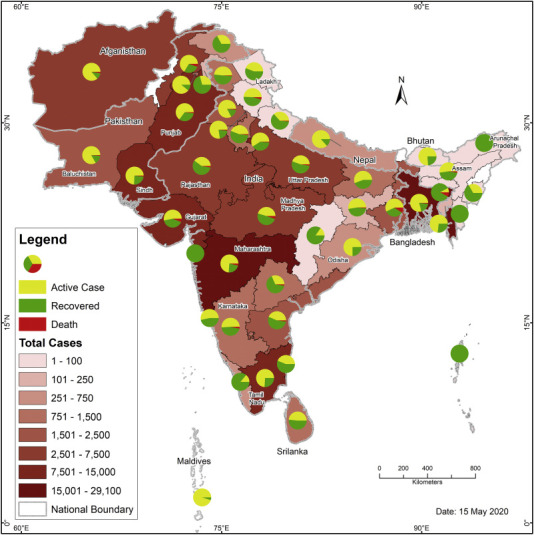
Geospatial distribution of Active, recovered, and death cases of COVID-19 in South Asian countries. The colour gradient of the base map is the illustration of a number of cases that have been reported yet as of 15 May, 2020). The pie chart of the map depicted the number of active cases (yellow coloured), recovered case (green coloured), and the death count (red coloured) in different areas.
The overall CFR among the SA countries have been calculated as highest in India (3.21%), followed by Afghanistan (2.53%) and Pakistan (2.15%). Nepal and Bhutan have no death due to COVID-19 so far. The recovery rate varied from 4.75% in the Maldives to 51.02% in Bhutan (Fig. 5 ). There is a positive correlation between the number of tests and CFR in Bangladesh (r = 0.90) and Pakistan (r = 0.27), but in India, there is a negative correlation (r = −0.43) between those two variables.
Fig. 5.
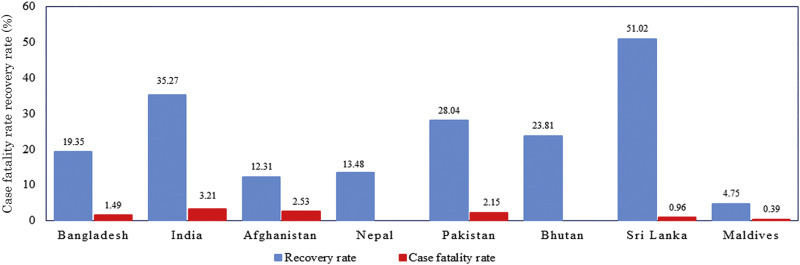
Case fatality rate and recovery rates in South Asian countries (the values are in percentage).
To combat pandemic COVID-19, Bangladesh, India, Pakistan, and Afghanistan had limited planning, whereas Nepal, Bhutan, and Sri Lanka were equipped with a well-planned attribute [[17], [18], [19], [20], [21]]. All the countries had measures to build up public awareness. Among SA countries, the first reported cases were identified in Nepal on 23 January, and within the last week of January, India and Sri Lanka have experienced their first cases. In February, Pakistan and Afghanistan have experienced the first case, whereas Bangladesh experienced at 2nd week of March. Travel and entry restriction, isolation and quarantine facility, training of health workers along with the availability of PPE were increased gradually among all the countries (Table 1 ).
Table 1.
Policies and action taken by different SA countries to combat with COVID-19.
| Measures taken | Bangladesh | India | Pakistan | Afghanistan | Nepal | Bhutan | Sri Lanka |
|---|---|---|---|---|---|---|---|
| Policy | |||||||
| Early stage planning | Limited | Limited | Limited | Limited | Well-planned | Well-planned | Well-planned |
| Support, incentive & stimulus package | √ | √ | √ | √ | √ | √ | √ |
| Public awareness | √ | √ | √ | √ | √ | √ | √ |
| Action | |||||||
| 1st reported case | 8 Mar. | 30 Jan. | 26 Feb. | 24 Feb. | 23 Jan. | 6 Mar. | 27 Jan. |
| Lockdown/ Movement restriction/Social Distancing | 23 Mar. - 30 May | 22 Mar. - 30 May | 1 Apr. - 9 May | Partially from 22 Mar., complete from 27 Mar. -21 May | From 24 Mar. | None | Complete from 19 Mar. - 11 May |
| Screening at port | Airport only; from 22 Jan. | Airports from 21 Jan. | Airports, from 30 Jan. | × | End of Feb. | Foreign tourist entry restricted from 7 Mar. | Initially airport, later all |
| Travel and entry restrictions | Complete restrictions from 14 Mar., except UK | From 13 Mar. 2020 | From 13 Mar. 2020 | × | 14 Mar. -30 Apr 2020 | From 23 Mar. 2020 | From 16 Mar. 2020 |
| Isolation and quarantine facilities | Increased gradually | Increased gradually | Increased gradually | Increased gradually | Early stage | Early stage | Early stage |
| Training of health workers | Increased gradually | Increased gradually | Increased gradually | Increased gradually | Early stage | Early stage | Early stage |
| PPE | Increased gradually | Increased gradually | Increased gradually | Increased gradually | Early stage | Early stage | Early stage |
| Testing strategy | Only symptomatic ones initially, later all. | Symptomatic ones initially (30) | Only symptomatic ones initially, later all. | Only symptomatic ones initially, later all. | All | Early stage | Only symptomatic ones. Now antibody test |
| Health bulletin | √ | √ | √ | √ | √ | None | √ |
| Fighting misinformation | √ | None | None | None | √ | None | None |
√-Step taken; × − Step not taken.
3.3. COVID-19 in Bangladesh
As of 15 May, 2020, a total of 20,065 patients of COVID-19 were confirmed in Bangladesh, among which 298 have died. Patients were identified from several districts with a higher percentage of in Dhaka (59.1%, n = 9,855) compared to any other districts of Bangladesh. Dhaka, the capital city, has almost 59.0% of the total confirmed cases. The second-highest concentration of COVID-19 cases (n = 1,463) was detected in Narayanganj, the district adjacent to Dhaka. Again, some densely populated communities, including Gazipur, Munshiganj, and Chattogram, have reported substantial COVID-19 cases, which varied between 701 and 1,500 (Fig. 6 ).
Fig. 6.
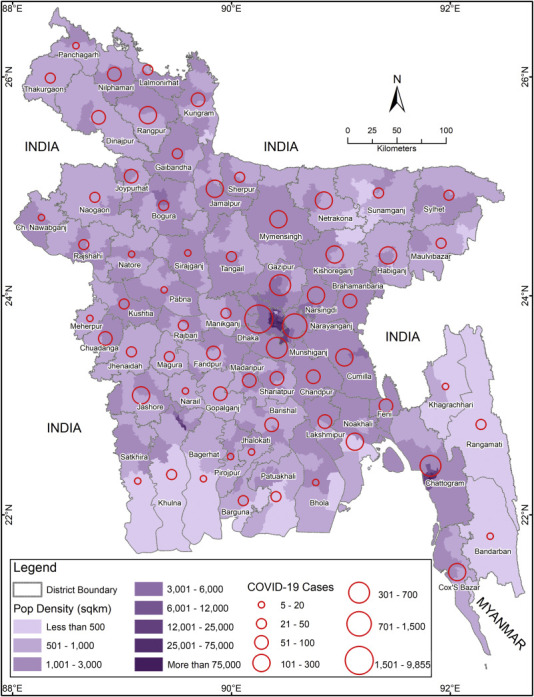
Spatial distribution of COVID-19 cases in different districts of Bangladesh. The graduated colour of the base map is the illustration of population density, where different sized red coloured circle depicted the case count in each district.
By 15 May, 2020, patients aged between 21 and 30 years had the highest infection (26%), whereas children (≤10 years) were documented as the lowest infected group (3%). The highest death (42%) was recorded among the senior citizens (>60 years), and the number of deaths has been found in the 11–20 years age group so far (Fig. 7 ). The infection was predominant among males (68%) than females (32%). Besides, the death rate was also higher in males (73%) than females (27%) (Fig. 7).
Fig. 7.
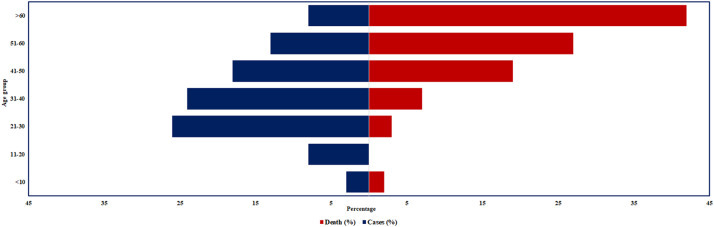
Confirmed COVID-19 cases and death among different age categories in Bangladesh as of May 15, 2020; blue bar denotes the percentage of cases, and the orange bar indicates the rate of death.
3.4. COVID-19 hotspot analysis for India and Bangladesh
Most areas do not show significant spatial and temporal trends. We have identified a wide hotspot (99% Cl: Confidence level) consisting of 5 different districts adjacent to Maharashtra and Gujrat province with around 50% district of both Maharashtra, Gujrat, and Karnataka province including Goa, India. Again, a 90% confidence-based hotspot has been identified in the Bharatpur and Bhilwara district of Rajsthan and Dhar district of Madhya Pradesh. We have also identified cold spot (90% Cl) regions located at Purnia district of Bihar, Dumka, and Pukur district of Jharkhand, Koriya, Korba, Surguja and Raj Nandgaon district of Chhattisgarh and Shivpuri and Sidhi district of Madhya Pradesh of India (Fig. 8 ).
Fig. 8.
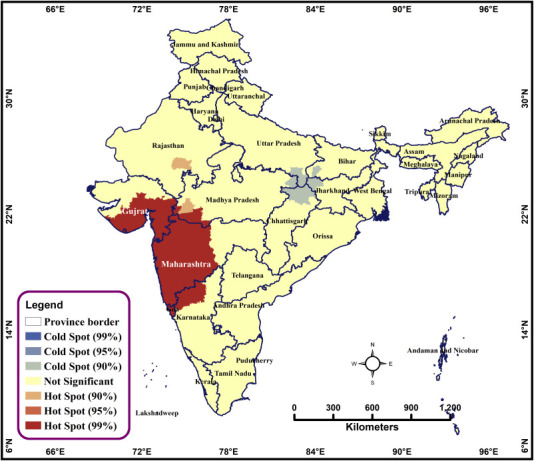
Spatial hotspots of COVID-19 in India as of May 15, 2020. The poinsettia red coloured area is indicating the Hot Spot region for COVID-19 at 99% confidence. The grey shaded area depicted the cold spot region at 90% confidence. The yucca yellow shaded area is an indication of a non-significant part.
Fig. 9 depicted a hotspot (99% Cl) in Bangladesh, located at the central portion and consisted of Dhaka, Gazipur, Narsingdi, Manikganj, Narayanganj, Munshiganj, and Shariatpur district. Again, a 95% confidence-based hotspot has been identified in the Faridpur and Madaripur district of Bangladesh. The infection has dispersed across the country designated as a non-significant area in the map. Unfortunately, there was not any cold spot region in Bangladesh.
Fig. 9.
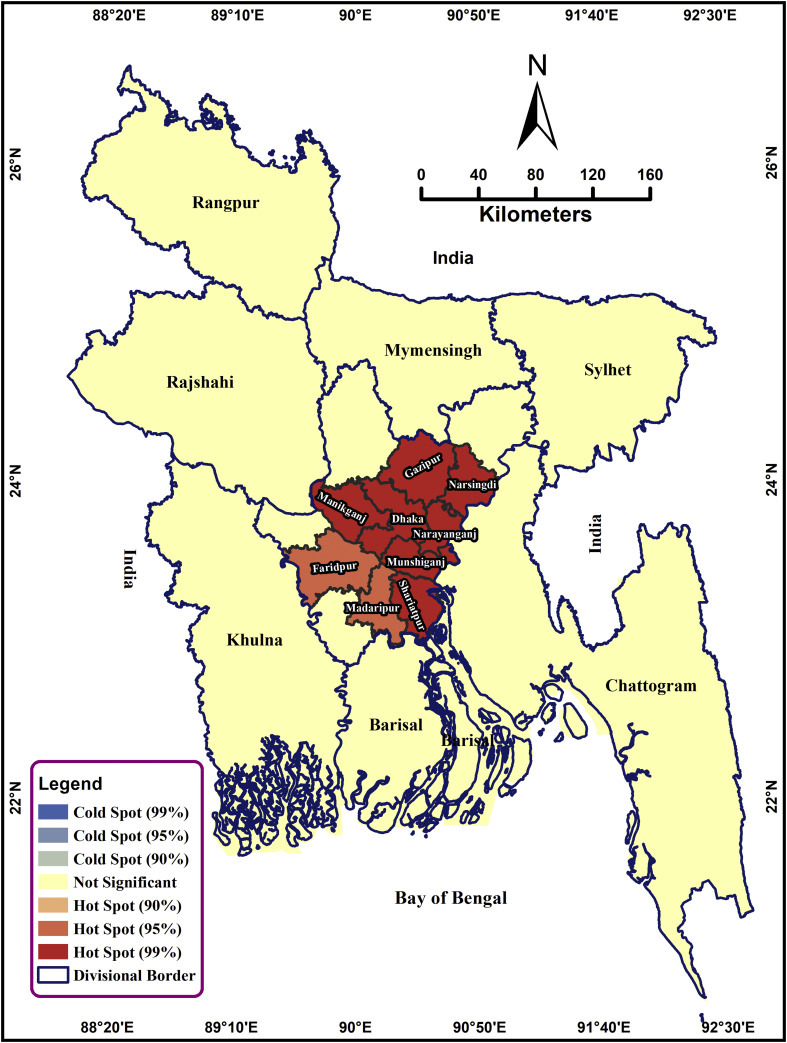
Spatial hotspots of COVID-19 in Bangladesh as of May 15, 2020. The poinsettia red coloured area is the indication of Hot Spot at 99% confidence. The cantaloupe coloured area is the illustration of the 90% confidence based Hot Spot area of Bangladesh. The yucca yellow coloured area is the indication of a non-significant region. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
4. Discussion
4.1. Epidemiological characteristics and test rate of COVID-19 in the world
We detected the highest CFR in Europe and the lowest CFR in the Oceania region. Keeping the CFR lower in Oceania can be attributed to their highest number of confirmatory tests per million people. If European countries and other areas follow the rule of “test, test, and test” by WHO, they could also reduce the CFR by COVID-19 [22]. Earlier, there was a belief that a high rate of CFR in Europe might result from lower environmental temperatures. Still, later on, this statement was negated as there is not any significant impact of ambient temperature on SARS-CoV-2 transmission [23]. Another reason for high CFR in Europe may be due to the higher percentage (19.2%) of the elderly (70 or above) people [24]. For example, Italy, a European country with 223,885 cases and 31,610 deaths due to COVID-19 as of May 15, 2020, has 39% of people aged 70 or above [25].
SA countries were not prepared at all for this global pandemic as this part of the world is most densely populated with a resource-limited healthcare system. As a result, they did the lowest number of confirmatory tests per million population. However, almost 30 per 100 people recovered from COVID-19 in SA, which is a smaller number considering the regions' limited test facilities and poor health system infrastructure [26]. Again, due to the heavy density of the population in contrast to European countries, it is challenging to maintain the social distancing where the crowding index is much higher. Many of the people of SA countries are migrant workers who came back to their native during the pandemic [27]. However, the family bonding in SA countries is responsible for spreading the virus at the community level due to the warm welcome of the migrant workers in the community without maintaining quarantine rules.
4.2. Distribution and epidemiological characteristics of COVID-19 cases in SA countries
COVID-19 has highly infected India and Pakistan in contrast to other SA countries. India has a population of 1,377 million, equivalent to 17.7% of the total world population (Worldometer). Similarly, Pakistan is another populous country with a density of around 287 people per km2 area (Worldometer). This high density of people per km2 in these two countries helped SARS-CoV-2 spread faster than any other country in the SA region. Both of the countries took lockdown and social distancing measures. But Pakistan removed their lockdown on 9 May, whereas India removed the lockdown on 1 June, 2020. After that, the number of cases is rising rapidly in both countries. We found a weak positive correlation between the number of tests and CFR in Pakistan, which might be due to scaling up testing for COVID-19, approached by the health care professionals [28]. However, a negative correlation is calculated between the number of tests and CFR in India, which might be due to lower Government Effectiveness score [29], along with insufficient hospital bed facility agreed with Liang, Tseng [28].
Similarly, Afghanistan is one of the most vulnerable countries globally, with 31.6 million people and 7.2 and 0.6 physicians (per 10,000 people) in urban and rural areas, respectively [30]. Moreover, 22.8 skilled health workers per 10,000 people are required to execute all essential health interventions [30]. So, Afghanistan faces a severe shortage of healthcare workers, facilities, and equipment in the treatment section. Other obstacles include inappropriate sampling, problems in the transfer of samples due to the absence of proper roads, and low social security in diagnosing this disease [19]. Besides, the lack of personal protective equipment has also affected many healthcare workers and even forced some of them to resign or stay home [31]. However, 71.5% of Afghanistan's population lives in rural areas [32] where cinemas, subways, apartment living, and even large public transports are not popular. So, contact among people is naturally less, which might slow down the transmission speed in this country [19].
Two SA countries, Nepal and Bhutan, have very few cases and zero CFR due to COVID-19. But the recovery rate is highest for Sri Lanka among the SA countries. Nepal has only a handful of cases of COVID-19, which indicate their well-organized planning during the earlier stage of the outbreak [17]. They formed monitoring teams and health desks at border checkpoints and cities, screened incoming persons at their only international airport, increased isolation and quarantine facilities, trained health workers, personal protective equipment, and testing facilities. The authority also disseminates information and communication materials through media. They closed schools, canceled events, shut down Mount Everest, and mostly restricted international travel [33]. These actions are courageous, considering the enormous economic costs. All these initiatives were paid back to the nation.
Similarly, Bhutan is also at the forefront of the battle against COVID-19. The Prime minister, foreign minister, and health minister of Bhutan are doctors and public health specialists. Due to their significant steps, Bhutan has a significantly low case [21] with zero fatalities. When other countries are struggling with the pandemic, Bhutan and Nepal are efficiently managing the crisis.
However, critical care capacity remains a problem in all SA countries [34]. Only a few hospitals have isolation capacity, which can provide intensive care with respiratory support. SA has an estimated 0.7–2.8 critical care beds per 100,000 population [34]. The number of beds is scarce compared to developed countries in the world. Nepal has fewer than 500 intensive care unit beds in the entire region for approximately 28 million people [34]. Still, their government has taken extraordinary and necessary measures to prevent the virus's entry through its borders. So, they have not faced any pressure on their health care system during the pandemic.
In Sri Lanka, the preparedness and preventive control measures of COVID-19 were unique compared with most other countries. They initiated steps to prevent the COVID-19 epidemic even before the first case was detected on 27 January, 2020. The health care system in Sri Lanka is relatively strong, with 3.9 hospital beds per 1,000 population [17]. The government of Sri Lanka acted swiftly to contain the transmission, with very stringent public health measures and social distancing: complete island-wide lockdown, contact tracing and isolation, and quarantine of all inbound passengers were all adopted almost simultaneously. The epidemic has not yet reached the stage of full-blown community transmission in Sri Lanka, and almost all cases still occur in clusters where the chain of transmission can be traced [33].
4.3. COVID-19 in Bangladesh
Dhaka, the capital of Bangladesh, is the center of most confirmed cases. It is also the center for business, industries, transportation, and airport. At the early stage of the pandemic, authorities did not ban international flights. So, many expatriates returned to the country from infected countries and brought the virus to spread among their families and relatives. Besides, a large number of mosques in Dhaka city predispose the Muslim community who prayers daily in mosques. All these leads to make Dhaka the epicenter of the infection.
On 25 March, 2020, the government announced a lockdown for ten days active from March 26th. All travel routes, including road, rail, water, and air, were stopped. Without pharmacies, groceries, and other unavoidable necessities, all educational institutions, inessential organizations, businesses were shut down. However, the estimated positive correlation between the number of tests and CFR indicates an increased early diagnosis facility of COVID-19 implemented by the government. Despite all measures, many people from cities started to leave for the village by various means, including overcrowded public transport services, with a high risk of contracting COVID-19 and in violation of the government instructions [[37], [38], [39]]. As a result, the infection spread quickly from one district to another.
The current data from Bangladesh suggest, spreading of COVID-19 in 64 districts as clusters where two or more patients have been identified within a close area. The distribution pattern of cases clearly shows, people who met the expatriates from abroad were infected mainly. Simultaneously massive scale community transmission has already been started to happen due to not maintaining proper lockdown approaches. Community transmission of novel coronavirus is evidenced by the inability to relate confirmed cases through chains of transmission.
The highly contagious virus, which is wreaking havoc on several countries, including the USA, Italy, and Spain, might have spread at the community level on a larger scale in Bangladesh. Nevertheless, the rapid growth and community transmission of this pandemic in Bangladesh are of grave concern, given that many of the affected countries are characterized by weak health systems and a high prevalence of malnutrition and other comorbidities. These factors can increase the burden of COVID-19 and pose an additional strain on the health care system.
Among the confirmed COVID-19 patient in Bangladesh, 68% were male. Similar gender trends were seen in patients from China as well [[38], [39], [40]]. One explanation may be the return of male expatriates from abroad after the outbreak started [41]. Moreover, some male individuals were visiting their workstation and getting in contact with co-workers. On the other hand, females more often tend to ignore their health and try to hide the illness until they can tolerate it [42,43]. The number of confirmed cases among the 21–30 years age group was highest due to active participation in different types of works and constant movement. Among different age groups, 298 persons have died due to comorbidity and other health conditions, and most of them are aged.
4.4. COVID-19 hotspot analysis for India and Bangladesh
We identified a wide hotspot zone and three small cold spots in India. On the other hand, two hotspots were detected in Bangladesh without any cold spot in the country. Bangladesh and India took lockdown and social distancing measures initially. These measures lessen interpersonal contact and slow the rate of COVID-19 infections [35]. It is assumed that social distancing measures and total lockdown help to flat the epidemic curves [36]. It is at least a 100 years old strategy, and history showed that social distancing works very well in the containment of epidemic [37]. The death rates of the Flu Pandemic of 1918 were about 50% lower in cities that implemented preventive measures, like social distancing and lockdown, early on compared to those who performed them later or not at all [36]. The most vibrant cities simultaneously closed schools, churches, theatres, and banned public gatherings, which slowed the spread of disease and allowed time for vaccine development, and lessened the stress on the hospitals [37]. Strict quarantine measures not only protect from COVID-19 but also exert a positive impact on the environment [38].
But both of these countries open the economy from the 1st of June without flattening the epidemic curve, which resulted in a surge of COVID-19 cases in Bangladesh. So, before restarting the economy, both countries should have a plan for reducing the number of cases. According to WHO, the novel coronavirus is ten times deadlier than swine flu, which caused a global pandemic in 2009. A vaccine would be necessary to halt transmission entirely. But antivirals and vaccines may need months to years to develop and test, going non-pharmaceutical interventions as the only immediate means of controlling SARS-CoV-2 transmission. So, the government of Bangladesh must continue to encourage strict adherence to establish public health measures such as social distancing, personal hygiene practices, and cough etiquette. But, without extensive testing and tracing, these measures will not be successful in the long run. Besides, the government should establish potential surveillance and early-warning system that could be used to identify potential pandemic like disease X having the possibility to emerge or resurface in the future.
4.5. Limitations of the study
A low test rate impacts the number of cases, thus affecting the death rate and recovery rate in SA. However, sometimes there is a lack of resources available for specific countries like Afghanistan, which is a crump to make a promising interpretation. Further statistical analysis with accumulated data or other available data resources is necessary to verify this study's findings.
5. Conclusion
Though the case count was lower initially in the SA countries due to a limited number of tests, as time elapses and the test facility is enhanced, the number of cases is increasing exponentially and transmitted to the community. We found that the spatial and temporal pattern of the COVID-19 varies across the region, which recommends customized country-specific prioritized policies identifying the real hotspot of infection and applying strict restriction of movement within hotspot areas. Strict lockdown is crucial for containing the spread of COVID-19, which is the best measure to maintain extreme social distancing, controlling the infection, and saving lives. We also recommend extensive testing, robust contract tracing, and strict quarantine, which are the leading imperative steps to lift the lockdown. Reopening too quickly or too boldly without a goal-oriented approach can cause a second wave of infection as fierce or even worse as the first. Health care in the region is already weak, marked by low funding levels and access to services. Besides, we should establish a potential early-warning system that could be used under the non-outbreak condition to identify possible pandemic like disease X that has occurred and could resurface in the future.
Acknowledgements
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. USAID's Emerging Pandemic Threats PREDICT program (Cooperative Agreement No.AID-OAA-A-14-00102) supported Ariful Islam and Jinnat Ferdous through EcoHealth Alliance. We acknowledge the Department of Health Services of each country in South Asia for publicly sharing COVID-19 outbreak data. We thank the Institute of Epidemiology Disease Control and Research (IEDCR), Chattogram Veterinary and Animal Sciences University (CVASU), and EcoHealth Alliance for continuous support to our research team.
Conflict of interest statement
The authors declare that there are no conflicts of interest.
Author contributions
Ariful Islam: Conceptualization, Methodology, Formal analysis, Supervision, Validation, Visualization, Writing- original draft. Md. Abu Sayeed: Methodology, Formal analysis, Visualization, Writing- review & editing. Md. Kaisar Rahman: Data curation, Writing- review & editing. Jinnat Ferdous: Writing- review & editing. Shahanaj Shano: Writing- review & editing. Shusmita Dutta Choudhury: Writing- review & editing. Mohammad Mahmudul Hassan: Supervision, Writing- review & editing.
References
- 1.World Health Organization . 2020. Virtual Press Conference on COVID-19. https://www.who.int/docs/default- source/coronaviruse/transcripts/who- audio- emergencies- coronavirus- press- conference- full- and- final- 11mar2020. pdf, 2020 (accessed 18 August 2020) [Google Scholar]
- 2.World Health Organization . 2020. Coronavirus disease 2019 (COVID-19): Situation report, 72. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200401-sitrep-72-covid-19.pdf?sfvrsn=3dd8971b_2, 2020 (accessed 17 August 2020) [Google Scholar]
- 3.World Health Organization Coronavirus disease (COVID-19) situation report – 116. 2020. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200515-covid-19-sitrep-116.pdf?sfvrsn=8dd60956_2 (accessed 17 August 2020)
- 4.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., Zhao X., Huang B., Shi W., Lu R., Niu P., Zhan F., Ma X., Wang D., Xu W., Wu G., Gao G.F., Tan W. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020;382(8):727–733. doi: 10.1056/nejmoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liu W., Zhang Q., Chen J., Xiang R., Song H., Shu S., Chen L., Liang L., Zhou J., You L., Wu P., Zhang B., Lu Y., Xia L., Huang L., Yang Y., Liu F., Semple M.G., Cowling B.J., Lan K., Sun Z., Yu H., Liu Y. Detection of Covid-19 in children in early January 2020 in Wuhan, China. N. Engl. J. Med. 2020;382(14):1370–1371. doi: 10.1056/NEJMc2003717. (accessed 17 August 2020) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang X., Liu C., Mao W., Hu Z., Gu L. Tracing the largest seasonal migration on earth, arXiv. 2014. https://arxiv.org/ftp/arxiv/papers/1411/1411.0983.pdf
- 7.Callaway E. Time to use the p-word? Coronavirus enter dangerous new phase. Nature. 2020;579(12):10–1038. doi: 10.1038/d41586-020-00551-1. [DOI] [PubMed] [Google Scholar]
- 8.Li R., Rivers C., Tan Q., Murray M.B., Toner E., Lipsitch M. The demand for inpatient and ICU beds for COVID-19 in the US: lessons from Chinese cities. medRxiv. 2020 doi: 10.1101/2020.03.09.20033241. [DOI] [Google Scholar]
- 9.Véron J., Horko K., Kneipp R., Rogers G. The demography of South Asia from the 1950s to the 2000s. Population. 2008;63(1):9–89. doi: 10.3917/popu.801.0009. [DOI] [Google Scholar]
- 10.ILO . 2015. The Contribution of the Labour Mobility to Economic Growth. http://www.ilo.org/ global/about-the-ilo/how-the-ilo-works/multilateral-system/g20/reports/WCMS_398078/lang-- en/index.htm, (accessed 15 June 2020) [Google Scholar]
- 11.Streatfield P.K., Karar Z.A. Population challenges for Bangladesh in the coming decades. J. Health Popul. Nutr. 2008;26(3):261–272. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2740702 [PMC free article] [PubMed] [Google Scholar]
- 12.Sultana R., Fuad N., Ferdous J. 2020. Containment Strategy during COVID-19 Outbreak -Analysis of Hospitals Hotspots in Dhaka to Prevent Community Transmission, SSRN Electronic Journal. [DOI] [Google Scholar]
- 13.Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.SEDAC, Socioeconomic Data and Applications Center 2020. https://sedac.ciesin.columbia.edu/data/collection/gpw-v4/sets/browse
- 15.World Health Organization Coronavirus Source Data. 2020. https://ourworldindata.org/coronavirus-source-data (accessed 3 May 2020)
- 16.Peeters A., Zude M., Käthner J., Ünlü M., Kanber R., Hetzroni A., Gebbers R., Ben-Gal A. Getis–Ord’s hot-and cold-spot statistics as a basis for multivariate spatial clustering of orchard tree data. Comput. Electron. Agric. 2015;111:140–150. doi: 10.1016/j.compag.2014.12.011. [DOI] [Google Scholar]
- 17.Shrestha R., Shrestha S., Khanal P., KC B. Nepal’s First Case of COVID-19 and public health response. J. Travel Med. 2020;27(3):taaa024. doi: 10.1093/jtm/taaa024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Khan H.R., Howlader T., Islam M.M. 2020. Battling the COVID-19 Pandemic: Is Bangladesh Prepared? medRxiv. [DOI] [Google Scholar]
- 19.Shah J., Karimzadeh S., Al-Ahdal T.M.A., Mousavi S.H., Zahid S.U., Huy N.T. COVID-19: the current situation in Afghanistan. Lancet Glob. Health. 2020;8(6):e771–e772. doi: 10.1016/S2214-109X(20)30124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lancet T. India under COVID-19 lockdown. Lancet. 2020;395(10233):1315. doi: 10.1016/S0140-6736(20)30938-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nafees M., Khan F. Pakistan’s response to COVID-19 pandemic and efficacy of quarantine and partial lockdown: a review. Electron. J. Gen. Med. 2020;17(6):em240. doi: 10.29333/ejgm/7951. [DOI] [Google Scholar]
- 22.Kishore R., Jha P.K., Das S., Agarwal D., Maloo T., Pegu H., Sahoo D., Singhal A., Sahu K.K. A kinetic model for qualitative understanding and analysis of the effect of complete lockdown imposed by India for controlling the COVID-19 disease spread by the SARS-CoV-2 virus. arXiv. 2020:1–22. https://arxiv.org/abs/2004.05684 [Google Scholar]
- 23.Yao Y., Pan J. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur. Respir. J. 2020;55(5):2000517. doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Davies R. 2020. Older People in Europe: EU Policies and Programmes. https://www.europarl.europa.eu/RegData/bibliotheque/briefing/2014/140811/LDM_BRI(2014)140811_REV1_EN.pdf, (accessed 18 May 2020) [Google Scholar]
- 25.Halb W., Raimond Y., Hausenblas M. 2020. Building Linked Data For Both Humans and Machines. http://ra.ethz.ch/CDstore/ www2008/, events. linkeddata.org/ldow2008/papers/06-halb-raimond-building-linked-data.pdf, 2020 (accessed 12 February 2020) [Google Scholar]
- 26.Akhtar S. Malnutrition in South Asia—a critical reappraisal. Crit. Rev. Food Sci. Nutr. 2016;56(14):2320–2330. doi: 10.1080/10408398.2013.832143. [DOI] [PubMed] [Google Scholar]
- 27.Pulla P. Covid-19: India imposes lockdown for 21 days and cases rise. BMJ. 2020;368:m1251. doi: 10.1136/bmj.m1251. [DOI] [PubMed] [Google Scholar]
- 28.Liang L.-L., Tseng C.-H., Ho H.J., Wu C.-Y. Covid-19 mortality is negatively associated with test number and government effectiveness. Sci. Rep. 2020;10(1):1–7. doi: 10.1038/s41598-020-68862-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bank T.W. 2020. Worldwide Governance Indicators. https://info.worldbank.org/ governance/wgi/Home/Reports. (accessed 6 August 2020) [Google Scholar]
- 30.Campbell J., Dussault G., Buchan J., Pozo-Martin F., Guerra Arias C., Leone A., Siyam A., Cometto G. Global Health Workforce Alliance and WHO; Geneva: 2013. A Universal Truth: No Health without a Workforce, Forum Report.https://www.almendron.com/tribuna/wp-content/uploads/2016/09/GHWA-a_universal_truth_report.pdf 2016 (accessed 15 March 2020) [Google Scholar]
- 31.Mousavi S.H., Abdi M., Zahid S.U., Wardak K. Coronavirus disease 2019 (COVID-19) outbreak in Afghanistan; measures and challenges. Infect. Control Hosp. Epidemiol. 2020:1–2. doi: 10.1017/ice.2020.240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Islamic Republic of Afghanistan National Statistics and Information Authority Afghanistan Statistical Yearbook 2018–19. 2019. https://www.nsia.gov.af:8080/wp-content/uploads/2019/11/Afghanistan-Statistical-Yearbook-2018-19_compressed.pdf (accessed 13 March 2020)
- 33.Bastola A., Sah R., Rodriguez-Morales A.J., Lal B.K., Jha R., Ojha H.C., Shrestha B., Chu D.K., Poon L.L., Costello A. The first 2019 novel coronavirus case in Nepal. Lancet Infect. Dis. 2020;20(3):279–280. doi: 10.1016/S1473-3099(20)30067-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bhutta Z.A., Basnyat B., Saha S., Laxminarayan R. Covid-19 risks and response in South Asia. BMJ. 2020;368:m1190. doi: 10.1136/bmj.m1190. [DOI] [PubMed] [Google Scholar]
- 35.Al Amin M.M. 2010. Factors Behind Internal Migration and Migrant’s Livelihood Aspects: Dhaka City, Bangladesh. http://lup.lub.lu.se/luur/download? func=download File&recordOId=1614168&fileOId=1614174, (accessed 5 May 2020) [Google Scholar]
- 36.Iftikhar-ul-Awwal A., Alamgir M. 2003. Dhaka, the capital of Islamic culture, Observer Magazine (Bangladesh). pp. 7–9.https://ssrn.com/abstract=2590171 [Google Scholar]
- 37.Anwar S., Nasrullah M., Hosen M.J. COVID-19 and Bangladesh: challenges and how to address them. Front. Public Health. 2020;8:154. doi: 10.3389/fpubh.2020.00154. 10.3389%2Ffpubh.2020.00154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang J., Zheng Y., Gou X., Pu K., Chen Z., Guo Q., Ji R., Wang H., Wang Y., Zhou Y. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int. J. Infect. Dis. 2020;94:91–95. doi: 10.1016/j.ijid.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Epidemiology Working Group for NCIP Epidemic Response, Chinese Center for Disease Control and Prevention The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Chin. J. Epidemiol. 2020;41(2):145. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003. [DOI] [Google Scholar]
- 40.Ruan Q., Yang K., Wang W., Jiang L., Song J. Correction to: clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Inten. Care Medi. 2020;46(5):846–848. doi: 10.1007/s00134-020-06028-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Expats stream in, raising corona concerns The Business Standard. 2020. https://tbsnews.net/bangladesh/expats-stream-raising-corona-concerns-56413 (accessed May 2020)
- 42.Kabir H., Saha N.C., Wirtz A.L., Gazi R. Treatment-seeking for selected reproductive health problems: behaviours of unmarried female adolescents in two low-performing areas of Bangladesh. Reprod. Health. 2014;11(1):1–7. doi: 10.1186/1742-4755-11-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ahmed S.M., Adams A.M., Chowdhury M., Bhuiya A. Gender, socioeconomic development and health-seeking behaviour in Bangladesh. Soc. Sci. Med. 2000;51(3):361–371. doi: 10.1016/S0277-9536(99)00461-X. [DOI] [PubMed] [Google Scholar]


