Abstract
The current pandemic of coronavirus disease (COVID-19) caused by SARS-CoV-2 is a significant global health challenge. A recent study by Carvelli and colleagues now demonstrates the involvement of complement C5a and its receptor C5aR1 in disease progression and suggests that blockade of the C5a-C5aR1 axis may represent a potential therapeutic strategy against COVID-19.
Keywords: COVID-19, SARS-CoV-2, GPCRs, cellular signaling, drug discovery, complement system
Infection with the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) leads to the highly infectious coronavirus disease 2019 (COVID-19), which constitutes a serious health challenge worldwide. A major complication of SARS-CoV-2 infection is the development of significant lung inflammation, which can cause severe pneumonia and acute respiratory distress syndrome (ARDS). While much is to be learnt regarding the underlying mechanisms of lung pathology in COVID-19, it is clear that the immune system contributes to the inflammatory response and cytokine ‘storm’ that occurs in the lungs of a significant number of patients. Thus, a greater understanding of the drivers of lung inflammation in COVID-19 could lead to targeted therapeutic approaches to reduce morbidity and mortality.
In a recent study in Nature, Carvelli and colleagues [1] examined immune alterations in healthy individuals and COVID-19 patients presenting with increasing disease severity, from paucisymptomatic individuals to those with pneumonia or ARDS. Plasma proinflammatory mediators, including interleukin (IL)-6, CCL2, CCL4, and CXCL9, were positively associated with COVID-19 severity (Figure 1A), as were increases in circulating neutrophils, supporting findings from prior reports [2]. As an acute phase reactant that plays a key role in severe infections, including pneumonia and sepsis, the complement cascade has been proposed as a possible driver of lung inflammation and the cytokine storm in COVID-19 [3,4]. Indeed, SARS-CoV-2 proteins have been shown to activate distinct complement pathways [3,5]. Complement is a key innate immune pathway that rapidly responds to pathogens and cellular injury and amplifies a range of innate and adaptive immune processes. One of the key drivers of complement-mediated inflammation is the C5 cleavage product, C5a, which acts through two different seven-transmembrane receptors, namely C5aR1 and C5aR2 [6]. The former is a member of the large superfamily of plasma membrane receptors, known as G protein-coupled receptors (GPCRs), which are involved in nearly every physiological process in mammals, including immune responses.
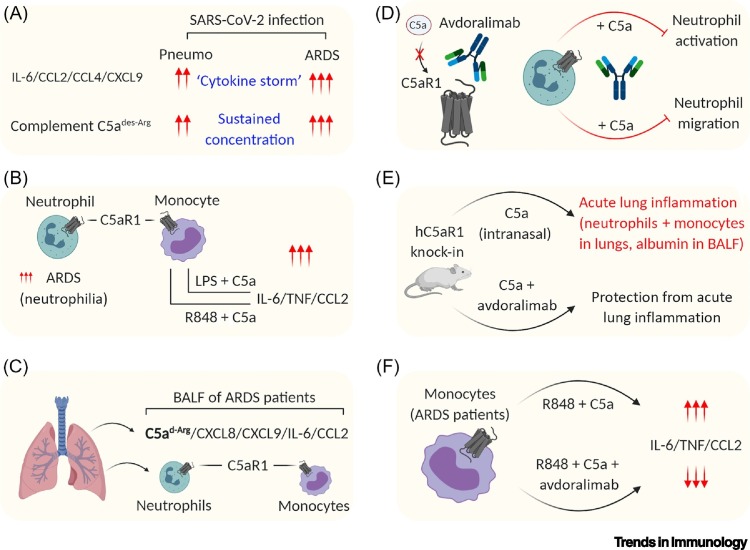
Figure 1.
C5aR1 Signaling Is Crucial in Modulating Coronavirus Disease 2019 (COVID-19) and May Represent a Potential Therapeutic Strategy.
(A) The concentrations of multiple cytokines and C5a are upregulated in the plasma of severe-COVID-19 patients [1]. (B) COVID-19 acute respiratory distress syndrome (ARDS) patients exhibit an increased number of circulating neutrophils (neutrophilia), which robustly express C5aR1, compared with healthy individuals [1]. Peripheral blood monocytes in ARDS patients also display robust C5aR1 expression, and C5a stimulation, in combination with either lipopolysaccharide (LPS) or R848 [as a mimic of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)-induced Toll-like receptor (TLR)7/TLR8 signaling]; this results in increased amounts of inflammatory cytokines relative to stimulation with LPS and R848 without C5a [1]. (C) The broncho-alveolar lavage fluid (BALF) derived from the lungs of COVID-19 ARDS patients contains a significant amount of C5a and other inflammatory cytokines, as well as a large number of neutrophils and monocytes expressing C5aR1 [1]. (D) Avdoralimab, a monoclonal antibody that blocks the binding of C5a to C5aR1, effectively inhibits C5a-induced activation and migration of neutrophils [1]. (E) Intranasal delivery of C5a in humanized C5aR1 knock-in mice leads to typical features of acute lung inflammation, which is effectively blocked by avdoralimab [1]. (F) The release of inflammatory cytokines upon C5a and R848 in vitro stimulation of monocytes derived from COVID-19 ARDS patients is blocked by pretreatment with avdoralimab [1]. This figure was created using Biorender. Abbreviations: IL, interleukin; Pneumo, pneumonia.
In line with increased plasma cytokine concentrations, Carvelli and coworkers reported that plasma C5a was elevated in COVID-19 patients and correlated with disease severity, with median C5a concentrations in ARDS patients reaching >250% those of healthy controls (Figure 1A) [1]. C5aR1 is highly expressed on myeloid cells in the healthy state and, indeed, no major alteration in neutrophil or monocyte receptor expression was observed in COVID-19 subjects. However, human monocytes co-stimulated with C5a and a Toll-like receptor (TLR) pathway activator, R848, drove the in vitro production of some of the same cytokines as those observed from COVID-19 patients (Figure 1B). In the lung, C5a and proinflammatory cytokines were detected in the broncho-alveolar lavage fluid (BALF) of COVID-19 patients, along with large numbers of neutrophils and monocytes (Figure 1C) [1], thus supporting a role for C5a in chemoattracting these C5aR1-expressing cells into the injured lung [7]. Indeed, immunohistochemistry staining and single-cell RNAseq transcriptomic data supported high expression of C5aR1 across myeloid cells and pulmonary macrophages in COVID-19 lungs [1].
There are currently multiple therapeutic candidates that target complement proteins at various stages of clinical development, with many of these drugs now undergoing clinical trials for COVID-19. These approaches include blocking central complement factors C3 and C5 and their downstream activation cleavage products, complement pathway inhibitors (e.g., MASP-2 lectin pathway inhibitors), as well as specific complement effector molecules [3]. In the study by Carvelli and colleagues [1], a targeted approach to C5aR1 was chosen to limit potentially immunocompromising consequences of blocking broader complement effector pathways, which might increase infection risk. Specifically, a fully human Fc-silent monoclonal antibody (mAb), avdoralimab (IPH5401), selectively blocked the C5a-C5aR1 interaction and its downstream signaling in human myeloid cells (Figure 1D). This was confirmed by avdoralimab-mediated in vitro inhibition of C5a-mediated neutrophil chemotaxis and upregulation of adhesion molecule CD11b in neutrophils, suggesting that avdoralimab might be useful in preventing neutrophil recruitment in COVID-19 diseased lungs. As avdoralimab is specific to human C5aR1, it’s in vivo activity was tested in human C5aR1 knock-in (hC5aR1) C57BL/6J mice (Figure 1E): intranasal instillation of human C5a induced key markers of acute lung inflammation [1], consistent with those observed in samples from COVID-19 patients, namely, neutrophil and monocyte infiltration, vascular leakage, hemorrhage, and alveolar wall thickening [8]. These findings support the concept that C5a may constitute a key molecule that contributes to lung pathology in COVID-19 patients. Notably, avdoralimab treatment prior to C5a administration in this study led to marked reductions in leukocyte infiltration to the lung, attenuated lung edema, and reduced features of lung pathology relative to isotype-antibody control-treated animals, confirming a key role for myeloid cell-expressing C5aR1 in this mouse model (Figure 1E) [1]. Moreover, avdoralimab also blocked C5a-mediated cytokine release from blood monocytes isolated from COVID-19 patients [IL-6, tumor necrosis factor (TNF)-α, CCL2] (Figure 1F) [1]. Overall, the study by Carvelli et al. [1] provides promising evidence that blockade of a single, yet major GPCR in acute myeloid cell-mediated lung inflammation, might ameliorate the severity and mortality associated with COVID-19 ARDS. Evidently, this will require rigorous testing.
An open question remains as to whether other complement effectors such as C3a and the terminal membrane attack complex (C5b-9) contribute to COVID-19. Furthermore, blocking C5aR1 with compounds such as avdoralimab leaves open the possibility that enhanced C5a activity occurs at its other receptor ligand C5aR2, which may have an impact on COVID-19. Although not coupled to G proteins, C5aR2 has been shown in mouse models of sepsis to worsen mortality, linked to C5a-C5aR2-mediated production of HMGB1 [9]. However, recent evidence indicates that C5aR2 signaling might play protective anti-inflammatory roles, as selective C5aR2 activation in human macrophages in vitro has inhibited cytokine secretion in response to a wide variety of immune cell activators [10]. Considering that C5aR2 robustly recruits and may signal through β-arrestins [5], this pathway should be carefully considered when targeting the C5a-C5aR1 axis to simultaneously engage both pathways and potentially yield more favorable outcomes. Another important caveat of the in vivo murine study performed by Carvelli and colleagues [1] is that avdoralimab was administered prophylactically in mice to reduce C5a-mediated lung injury, which might not correlate with an actual clinical setting, assuming that avdoralimab, in theory, would be administered to already-infected individuals. Thus, the timing of putative anti-C5aR1 treatments would be an important consideration when treating COVID-19 individuals, ensuring that the blockade of C5aR1-signaling occurs at a time where there is active C5aR1-mediated recruitment of myeloid cells to the lung. Finally, SARS-CoV-2 infection has also been associated with thrombogenic coagulopathy, an additional key driver of severe COVID-19 [11]. As C5a can induce the production of prothrombotic and coagulation-inducing factors such as tissue-factor from human platelets, immune cells, and the endothelium, this, together with inflammation, might drive endothelial dysfunction and thrombogenic coagulopathy in COVID-19 patients [3]. Indeed, in the study performed by Carvelli and colleagues [1], accumulation of C5aR1-expressing macrophages around the arteries and in the thrombus were observed in endoarteritis lesions. Whether blockade of complement C5aR1 signaling might also impact on endothelialitis-associated microthrombosis in COVID-19 remains to be determined.
In conclusion, the study by the Vivier and Explore COVID-19 Marseille Immunopole groups [1] potentially opens the door for a new direction in COVID-19 research that focuses on targeting the C5a-C5aR1 signaling axis for therapeutic benefit. Considering the ongoing efforts in multiple laboratories to identify novel modulators of C5aR1, together with pre-existing small molecule antagonists and monoclonal antibodies, this might emerge as a powerful candidate therapeutic avenue in the near future.
Acknowledgments
Acknowledgments
The work on the C5a-C5aR system in Dr Shukla’s laboratory is supported by the DBT/Wellcome Trust India Alliance (IA/I/14/1/501285), the Department of Biotechnology (BT/PR29041/BRB/10/1697/2018 and BT/HRD/NBA/39/06/2018-19) and the LADY TATA Memorial Trust. Prof Woodruff’s work on C5aR1 is supported by grants from the National Health and Medical Research Council (APP1082271 and APP1118881). The authors thank Martin Lo for constructive feedback.
Disclaimer Statement
Prof Woodruff has previously consulted for pharmaceutical companies that are commercially developing complement inhibitors. Dr Shukla declares no conflict of interest.
References
- 1.Carvelli J. Association of COVID-19 inflammation with activation of the C5a-C5aR1 axis. Nature. 2020 doi: 10.1038/s41586-020-2600-6. Published online July 29, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang C. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lo M.W. COVID-19: complement, coagulation, and collateral damage. J. Immunol. 2020;205:1488–1495. doi: 10.4049/jimmunol.2000644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Risitano A.M. Complement as a target in COVID-19? Nat. Rev. Immunol. 2020;20:343–344. doi: 10.1038/s41577-020-0320-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yu J. Direct activation of the alternative complement pathway by SARS-CoV-2 spike proteins is blocked by factor D inhibition. Blood. 2020 doi: 10.1182/blood.2020008248. Published online September 2, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pandey S. Emerging insights into the structure and function of complement C5a receptors. Trends Biochem. Sci. 2020;45:693–705. doi: 10.1016/j.tibs.2020.04.004. [DOI] [PubMed] [Google Scholar]
- 7.Russkamp N.F. Experimental design of complement component 5a-induced acute lung injury (C5a-ALI): a role of CC-chemokine receptor type 5 during immune activation by anaphylatoxin. FASEB J. 2015;29:3762–3772. doi: 10.1096/fj.15-271635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Xu Z. Pathological findings of COVID-19 associated with acute respiratory distress syndrome. Lancet Respir. Med. 2020;8:420–422. doi: 10.1016/S2213-2600(20)30076-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rittirsch D. Functional roles for C5a receptors in sepsis. Nat. Med. 2008;14:551–557. doi: 10.1038/nm1753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li X.X. C5aR2 activation broadly modulates the signaling and function of primary human macrophages. J. Immunol. 2020;205:1102–1112. doi: 10.4049/jimmunol.2000407. [DOI] [PubMed] [Google Scholar]
- 11.Merrill J.T. Emerging evidence of a COVID-19 thrombotic syndrome has treatment implications. Nat. Rev. Rheumatol. 2020;16:581–589. doi: 10.1038/s41584-020-0474-5. [DOI] [PMC free article] [PubMed] [Google Scholar]