Abstract
Introduction
This study aimed to investigate the response of the radiology workforce to the impact of the coronavirus disease 2019 (COVID-19) pandemic on professional practice in India and eight other Middle Eastern and North African countries. It further investigated the levels of fear and anxiety among this workforce during the pandemic.
Methods
A quantitative cross-sectional study was conducted using an online survey from 22 May-2 June 2020 among radiology workers employed during the COVID-19 pandemic. The survey collected information related to the following themes: (1) demographic characteristics, (2) the impact of COVID-19 on radiology practice, and (3) fear and (4) anxiety emanating from the global pandemic.
Results
We received 903 responses. Fifty-eight percent had completed training on infection control required for handling COVID-19 patients. A large proportion (79.5%) of the respondents strongly agreed or agreed that personal protective equipment (PPE) was adequately available at work during the pandemic. The respondents reported experiences of work-related stress (42.9%), high COVID-19 fear score (83.3%) and anxiety (10%) during the study period.
Conclusion
There was a perceived workload increase in general x-ray and Computed Tomography imaging procedures because they were the key modalities for the initial and follow-up investigations of COVID-19. However, there was adequate availability of PPE during the study period. Most radiology workers were afraid of being infected with the virus. Fear was predominant among workers younger than 30 years of age and also in temporary staff. Anxiety occurred completely independent of gender, age, experience, country, place of work, and work status.
Implications for practice
It is important to provide training and regular mental health support and evaluations for healthcare professionals, including radiology workers, during similar future pandemics.
Keywords: Radiology, COVID-19, Radiographer, Fear, Anxiety
Introduction
The World Health Organisation officially announced the coronavirus disease 2019 (COVID-19) outbreak as a pandemic in March 20201 after the virus was initially detected in the Chinese city of Wuhan in December 2019.2 , 3 Radiological investigations, such as chest radiography and Computed Tomography (CT), play a major support role in the diagnosis of respiratory manifestations in COVID-194, 5, 6, 7 along with the patient's clinical history and blood biomarkers.8 , 9 Thus, radiology departments are essential in the management of highly infectious patients, and the radiology workforce (RWF) is a part of the multidisciplinary healthcare team on the front lines of combating the COVID-19.
Most of the RWF comes into physical contact with patients while positioning them for radiological examinations. Therefore, it is essential for the imaging team to strictly adhere to appropriate rules of conduct to protect themselves from the risk of exposure and contracting coronavirus, especially as a nosocomial infection.10, 11, 12 However, the pandemic has brought a risk of infection and a high mortality rate as well as psychological and mental trauma to the public and medical personnel.13 , 14
In response to the pandemic, Health Care Professionals (HCPs) have dedicated themselves to the service of others despite the impact on their emotional and physical wellbeing due to uncertainties, varying work requirements and extended work schedules.15, 16, 17 Moreover, significant amounts of variance in work may indirectly impose a considerable amount of anxiety and stress among HCPs,18 , 19 as has been revealed in other outbreaks, such as Severe Acute Respiratory Syndrome and Ebola.20 , 21 , 17 Anxiety can be either stimulus-related or general in nature,22 and these experiences can lead to negative impacts and long term adverse mental health consequences among HCPs.23 , 24 Thus, HCPs face incredible challenges while having to deliver radiological services to patients during this unprecedented time.23
Stress is an emotional experience that increases when events are uncontrollable and unpredictable.25 Stress can produce biophysical reactions, such as headache, abdominal pain, chest pain, eating and sleep disturbances and heart palpitation, as well as; psychological–emotional reactions, such as anxiety, depression, tension, anger, nervousness and frustration.26 Stress and anxiety are linked to fear.27 Fear is a present response when facing a real or supposed threat, while anxiety is a future response that indicates an impending danger.25 Anxiety and fear are likely distinct emotional states but often overlap due to underlying behavioural mechanisms.28
Furthermore, in an attempt to maintain adequate number of healthcare workers to cope with COVID-19 cases, it is likely that work-related anxiety may affect all members of the healthcare team. This impact can lead to variation in the team's psychosocial variables along with burnout and emotional exhaustion.29 , 30 Additionally, these experiences may weaken the team's morale and confidence and can affect the healthcare delivery system and its associated reassurance to the public.30
Prevention and intervention are requirements that focus on the individual along with the working conditions to reduce high levels of emotional tension and to positively impact work-related behaviour.31 To improve the current situation and plan for future similar incidents, periodic evaluations of HCPs’ experiences and identification of underlying reasons may aid in building appropriate coping strategies.32 Hence, it is important to conduct significant research among HCPs during pandemics to establish clear directives, initiate precautionary measures and provide health-informed interventions in preparation for current and future outbreaks.33
The Middle East, North Africa and India (MENAIN) constitute a major fraction of the world's population.34 , 35 Moreover, due to the unique cultural factors and the nature of daily interpersonal relations in Middle Eastern countries, there are relatively more close contacts and interpersonal social activities in this area than in the rest of the world.36 , 37 Considering the aforementioned factors and the current pandemic, it is important to investigate the perceptions of the impact of the current pandemic, including the mental and physical health of HCPs serving in this region, to inform planning for similar future pandemics. The current study aimed to assess the response of the RWF on the impact of the COVID-19 pandemic, including the level of fear and anxiety among professionals across the MENAIN region.
Methods
This work was a part of an international study, COVID-19 Response in Radiology, aimed at assessing the global impact of the COVID-19 pandemic on the RWF and radiology practice. Data were collected from 22 May to 2 June 2020 from nine countries across the MENAIN region during the COVID-19 pandemic.
This was an exploratory, quantitative, cross-sectional study that investigated the impact of COVID-19 and related anxiety and fear among the RWF across the MENAIN region. The study was needed to capture the impact of the current urgent situation of the COVID-19 outbreak. The current study design was generally quick, easy, and cheap to perform and was particularly suitable for estimating the impact of COVID-19 on the population.38 , 39
Participants
Participants included the RWF working at hospitals during the pandemic, such as radiologists, radiographers, advanced practitioners, and radiology nurses. The population size was unidentified, as there have been no previous studies in this region to the best of our knowledge. Therefore, we used the formula of cross-sectional studies to calculate the sample size with a 95% confidence level, the margin of error was set at 5%, and the population size was infinite. The calculation proposed a minimum of 385 participants. The study used convenience sampling as it is an easy method to access participants in different geographical proximity.
Instruments
The survey consisted of four sections: (1) demographic characteristics, (2) radiology professional practice survey, (3) the Coronavirus Anxiety Scale (CAS), and (4) the Fear of COVID-19 Scale (FC–19S).
The demographic characteristics included general participant information, such as gender, age and years of experience. The radiology professional practice survey contained questions related to the impact of the pandemic on professional practice, infection control and COVID-19 related stress. This instrument was developed by a team of academic radiographers from the United Kingdom (UK). The team comprised of representatives from UK nations (England, Wales, Scotland and Northern Ireland) who outlined and piloted the questions required for the survey.40 The CAS was used to measure anxiety41 , 42 with a 5-point frequency scale (0 = ‘not at all’ to 4 = ‘nearly every day over the last two weeks’). The scale measures the physiological and psychological symptoms of fear or anxiety that respondents experienced when exposed to COVID-19 related thoughts or information. The total score was calculated by adding up each item's score (ranging from 0 to 20). Based on a CAS cut-off score of ≥9, current users of the CAS may consider lowering the cut-off score to ≥5 when assessing the general population but retaining a cut-off score of ≥9 when screening at risk or anxious groups.35 The FC-19S was used to assess fears caused by COVID-19.43 The participants indicated their level of agreement with the statements using a five-item Likert-type scale ranging from (5 = ‘strongly disagree’, 4 = ‘disagree’, 3 = ‘neither agree nor disagree’, 2 = ‘agree’, and 1 = ‘strongly agree’. The total score was calculated by adding up each item's score (ranging from 7 to 35). The higher the score, the greater the fear of COVID-19.43
The professional practice questionnaire was adopted from a previous study carried out in the UK.40 A pilot study was conducted, and minimal language edits were performed based on the feedback received from participants. Participants of the pilot study were not included in the current study. The CAS is a highly reliable (α = 0.92) and factorially valid measure that meets conventional standards for model fit.41 , 42 The FC-19S is also a highly reliable measure with acceptable internal consistency (α = 0.82).43 Moreover, the CAS and FC-19S have been validated and used in previous studies for HCPs and the general public.44, 45, 46, 47, 48, 49
The link to the online survey was shared amongst the radiology health board leads across multiple countries via email and was advertised on social media platforms. Participants were given an electronic informed consent form to indicate their willingness to participate in the study, and a completed form was mandatory before filling in the survey.
Ethical approval for the study was obtained from the Research Ethics Committees of three institutions (ID: 31,818, ID:20-05-18-01 and ID: 45/2020).
Analysis
The data were collected, categorized and processed using the Statistical Package for Social Sciences (SPSS), version 24®. The quantitative variables were expressed as percentages, and comparisons were made using independent sample t-tests and Pearson Chi-square tests. P-value of <0.05 were considered statistically significant. All graphs were created using Microsoft Office Excel 2013®.
Cut-off point ≥9 was used to assess the level of anxiety among participants, and the score of ≥9 was considered dysfunctionally anxious. The mean CAS score was calculated based on the total score of all items scores. There was no defined cut-off point for the FC-19S; therefore, the authors suggested a score of >19 as a high fear score, while scores from 9 to 19 as medium fear, and <8 were regarded as low fear.
Results
Demographics
Nine hundred and three responses were received from radiology workers. Of these, 49.1% percent (n = 443) were female and 50.9% (n = 460) were male. The largest age group with 49.7% of the participants (n = 449) was the group from 18 to 29 years, while 38.1% (n = 344) of the sample had less than five years of experience. The majority of the sample included radiographers (92.5%, n = 835) and 78% (n = 705) were permanent staff. The temporary staff members who were only working during the COVID-19 pandemic made up the remaining 22% (n = 198) and were comprised of students (13%, n = 117) and retired staff (9%, n = 81). Participants were from nine countries: United Arab Emirates, Oman, Kingdom of Saudi Arabia, Turkey, Sudan, Bahrain, India, Kuwait and Jordan (Table 1 ).
Table 1.
Demographic information.
| Count | Column N % | |
|---|---|---|
| Gender | ||
| Female | 443 | 49.1% |
| Male | 460 | 50.9% |
| Age | ||
| 18–29 Years | 449 | 49.7% |
| 30–39 years | 252 | 27.9% |
| 40–49 years | 161 | 17.8% |
| 50–59 years | 38 | 4.2% |
| 60 years or above | 3 | 0.3% |
| Experience | ||
| Less than 5 years | 344 | 38.1% |
| 6–10 years | 222 | 24.6% |
| 11–15 years | 126 | 14.0% |
| 16–20 years | 99 | 11.0% |
| more than 20 years | 112 | 12.4% |
| Title | ||
| Radiographer | 835 | 92.5% |
| Advanced practitioner | 13 | 1.4% |
| Radiologists | 21 | 2.3% |
| Radiology Assistants | 8 | 0.9% |
| Radiology residents | 9 | 1.0% |
| Nurse | 8 | 0.9% |
| Others | 9 | 1.0% |
| Workplace | ||
| Academic institute | 103 | 11.4% |
| Government Hospital | 489 | 54.2% |
| Government Clinic | 51 | 5.6% |
| Private Hospital | 206 | 22.8% |
| Private clinic | 34 | 3.8% |
| Research centre | 14 | 1.6% |
| Regularity body | 2 | 0.2% |
| Consultancy | 4 | 0.4% |
| Country | ||
| United Arab Emirates | 144 | 15.9% |
| Oman | 59 | 6.5% |
| Kingdom of Saudi Arabia | 84 | 9.3% |
| Turkey | 237 | 26.2% |
| Sudan | 129 | 14.3% |
| Bahrain | 62 | 6.9% |
| India | 124 | 13.7% |
| Kuwait | 40 | 4.4% |
| Jordan | 24 | 2.7% |
| Work Status | ||
| Temporary staff (student) | 117 | 13.0% |
| Temporary staff (retired) | 81 | 9.0% |
| Permanent staff | 705 | 78.0% |
Infection control
Of participants, 57.9% had received training on infection control and handling infected patients. Fig. 1 shows that 93.6% strongly agreed and agreed that they understood the methods of COVID-19 transmission, and 88.9% strongly agreed and agreed that their current understanding of infection prevention principles and control was adequate to protect themselves and their patients during the COVID-19 pandemic. Finally, 79.5% of the respondents strongly agreed and agreed that PPE was adequately available at the workplace (Fig. 1).
Figure 1.
Infection control of COVID-19.
Workload
The main diagnostic tools used for both the initial and follow-up investigations of COVID-19 patients were general x-ray and CT; these modalities were used by 610 and 552 of the respondents, respectively. Therefore, 48.1% (n = 434) and 36.7% (n = 331) of respondents reported an increased workload for general x-ray and CT, respectively, during the study period. The overall workload in the radiology department increased during the study period for 38.5% of the participants, while 23.6% reported an irregular pattern (Fig. 2 ).
Figure 2.
Workload during COVID-19 pandemic.
Stress
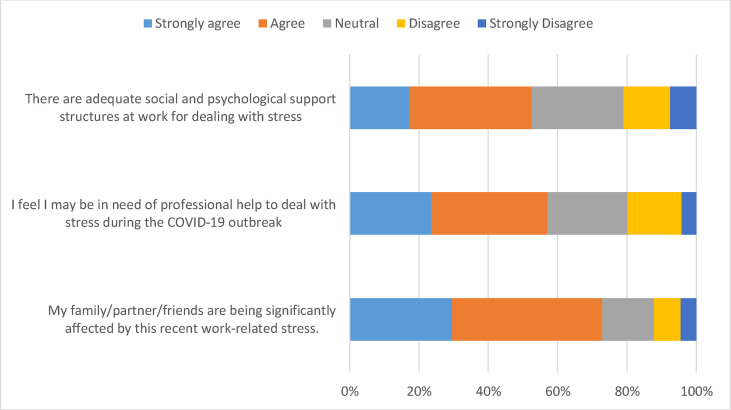
The results indicated that 42.9% of the respondents began to experience work-related stress during the COVID-19 pandemic, and 40.9% experienced stress sometimes. The analysis revealed that 72.9% strongly agreed and agreed that their family, partners and friends were significantly affected by their recent work-related stress.
While 52.5% strongly agreed and agreed that they had adequate social and psychological support structures at work for dealing with stress, 57.1% of the participants felt that they might need professional help to cope with their stress during the COVID-19 outbreak (Fig. 3 ). Fear of becoming infected with COVID-19 was a major (56.9% n = 514) stressor at work since the COVID-19 pandemic (Fig. 4 ).
Figure 3.
Stress related to COVID-19.
Figure 4.
Stressor at work.
Anxiety
The mean of the total score of the CAS was 3.2 ± 3.7 out of 20 points. The analysis of the CAS revealed that only 10% (n = 90) of respondents were anxious, and 90% (n = 813) were not anxious. The percentage of anxiety was 25%, 22.2% and 19.2% for nurses, radiology residents and radiographers, respectively (Fig. 5 ). Almost seventy percent of respondents did not feel nauseous or had no gastrointestinal problems at all when they thought about or were exposed to information about the COVID-19. Similarly, 53.3% did not have trouble falling or staying asleep because they were thinking about the COVID-19 (Table 2 ).
Figure 5.
Level of Coronavirus Anxiety among workers.
Table 2.
Coronavirus anxiety scale (CAS).
| Not at all |
Rare |
Several days |
>7 days |
Every day |
M | SD | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |||
| I felt dizzy, lightheaded, or faint when I read or listened to news about the coronavirus. | 526 | 58.3% | 253 | 28.0% | 89 | 9.9% | 18 | 2.0% | 17 | 1.9% | 0.61 | 0.9 |
| I had trouble falling and staying asleep because I was thinking about coronavirus. | 481 | 53.3% | 193 | 21.4% | 174 | 19.3% | 42 | 4.7% | 13 | 1.4% | 0.80 | 1.0 |
| I felt paralysed/frozen when I thought about or was exposed to information about the coronavirus. | 583 | 64.6% | 179 | 19.8% | 105 | 11.6% | 21 | 2.3% | 15 | 1.7% | 0.57 | 0.9 |
| I lost interest in eating when I thought about or was exposed to information about the coronavirus. | 569 | 63.0% | 130 | 14.4% | 162 | 17.9% | 24 | 2.7% | 18 | 2.0% | 0.66 | 1.0 |
| I felt nauseous or had stomach problems when I thought about or was exposed to information about the coronavirus. | 630 | 69.8% | 101 | 11.2% | 121 | 13.4% | 39 | 4.3% | 12 | 1.3% | 0.56 | 1.0 |
Fear
The mean of the total score of fear for COVID-19 among participants was 24.7 ± 6.4 out of 35 possible points. The FC-19S analysis revealed that 83.3% (n = 752) had a high fear score, 15.9% (n = 144) had a medium fear score, and only 0.8% (n = 7) had a low score of fear for COVID-19. The group of workers that experienced the greatest fear about COVID-19 were advanced practitioners (100%) and radiologists (95.2%) (Fig. 6 ).
Figure 6.
Level of Fear of COVID-19 among workers.
We found that 35.4% of the participants strongly agreed and agreed that they felt uncomfortable when thinking about COVID-19. Similarly, 28.6% reported being afraid of COVID-19 (Table 3 ).
Table 3.
Fear of COVID-19 (FC–19S).
| Strongly Agree |
Agree |
Neutral |
Disagree |
Strongly Disagree |
M | SD | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | N | % | |||
| I am most afraid of coronavirus-19. | 73 | 8.1% | 185 | 20.5% | 250 | 27.7% | 219 | 24.3% | 176 | 19.5% | 3.3 | 1.2 |
| It makes me uncomfortable to think about coronavirus-19. | 65 | 7.2% | 255 | 28.2% | 198 | 21.9% | 208 | 23.0% | 177 | 19.6% | 3.2 | 1.2 |
| My hands become clammy when I think about coronavirus-19. | 18 | 2.0% | 80 | 8.9% | 236 | 26.1% | 344 | 38.1% | 225 | 24.9% | 3.8 | 1.0 |
| I am afraid of losing my life because of coronavirus-19. | 82 | 9.1% | 122 | 13.5% | 224 | 24.8% | 253 | 28.0% | 222 | 24.6% | 3.5 | 1.2 |
| When watching news and stories about coronavirus-19 on social media, I become nervous or anxious | 44 | 4.9% | 187 | 20.7% | 213 | 23.6% | 247 | 27.4% | 212 | 23.5% | 3.4 | 1.2 |
| I cannot sleep because I'm worrying about getting coronavirus-19. | 29 | 3.2% | 88 | 9.7% | 173 | 19.2% | 342 | 37.9% | 271 | 30.0% | 3.8 | 1.1 |
| My heart races or palpitates when I think about getting coronavirus-19. | 23 | 2.5% | 96 | 10.6% | 179 | 19.8% | 322 | 35.7% | 283 | 31.3% | 3.8 | 1.1 |
The Pearson Chi-square correlation showed no significant association between anxiety level and gender, age, length of experience, country, working place, or work status.
Similarly, Pearson Chi-square correlation results revealed no significant association between fear of COVID-19 and either gender, length of experience, or country. Nevertheless, there were statistically significant correlations with age (Χ2 (8)> = 54.3, p = 0.01), working place (Χ2 (14)> = 49.1, p = 0.001), and work status (Χ2 (13)> = 13.3, p = 0.03). The post hoc test showed that the fear of COVID-19 was most frequently associated with participants aged 18–29 years, workers in private hospitals, and students working as temporary staff during the COVID-19 pandemic.
An independent samples t-test was conducted to compare the CAS with training and the results showed insignificant differences (p = 0.54). Moreover, an independent samples t-test was also carried out to compare the scores for fear of COVID-19 among radiology workers who had previous COVID-19 training and others who had not received training. The results showed a significant difference in the mean fear level of the COVID-19 between workers who attended the training (M = 25.78, SD = 5.8) and others who did not (M = 23.33, SD = 7.01) at p < 0.001). These results suggest that training does influence fear, and workers who attended training had a lower fear score.
Discussion
Radiology examinations are key clinical decision tools used in the management of patients presenting with respiratory distress and possible COVID-19 symptoms.50 Radiographers are usually in close proximity to the patient during image acquisition.10 , 12 Therefore, it is important for RWF to demonstrate a comprehensive understanding and application of infection control knowledge during practice.11 , 12 However, the current study found that only 58% of RWF had received training on infection control for handling COVID-19 patients, 93.6% understood the mode of coronavirus transmission and 88.9% confirmed an adequate level of infection control knowledge. This finding is broadly consistent with the results of other studies51 , 52 that similarly reported a high understanding of infection control, prevention and compliance among HCPs. The high level of understanding of infection control measures perceived by the RWF in the current study could be attributed to the wide and active dissemination of COVID-19 information by public health agencies via media outlets, including social media platforms, at the onset of the pandemic.53 It could also be attributed to the robust training on infection control included within the radiology/radiography curriculum or the maintenance of an active continuous professional development portfolio by radiology practitioners.
The workload in the radiology department was perceived to have increased during the study period by 38.5% of the participants, while 24% noticed a decrease in workload. These contradicting responses can be due to the nature and size of individual radiology departments and also the type of patients they typically serve. For example, an increase in the workload can be justified in a large hospital where new incoming COVID-19 patients do not hamper routine work but add to it along with the extra time required taken for the associated infection control measures. However, a small department may stop receiving routine patients in order to exclusively serve COVID-19 patients due to limited capacity. Increased pressure on general x-ray and CT services were perceived as expected because these modalities were the key recommended initial and follow-up investigation tools in use during the current pandemic.4, 5, 6, 7 Baseline chest x-ray showed a sensitivity of 69% in COVID-19 infection and imaging follow-up54; chest CT has a limited but important role in the clinical management of COVID-19 patients.50 The perceived reduction of patient numbers may also have been potentially due to adherence to national and international guidance to minimize non-urgent work in the radiology department,55 , 56 as well as due to infection control issues related to transporting COVID-19 patients to CT scanners and availability of CT modality in the departments.57 While the study did not investigate the occupational radiation dose, it is worth emphasising the importance of radiation safety for all RWF members58; corrective actions are needed to comply with radiation safety and protection during radiology examinations.59 Moreover, proper radiation protection for patients should be implemented60 to ensure radiation safety practice in both routine and crisis situations.
It was apparent that the number of patients needing care in the imaging modalities was increased; as a result, hospitals recruited temporary staff to work during the COVID-19 pandemic.61 The result of the current study showed that the temporary staff recruited during the pandemic constituted 22% of the total workers to augment service delivery.
Previous studies have shown that epidemics can lead to the development of new or worsening psychiatric symptoms or ailments, such as fear, depression, anxiety, panic attacks, somatic symptoms, psychosis and even suicide.62, 63, 64 Another recent study reported similar findings during the COVID-19 pandemic, with a heightened risk for mental health problems among HCP who in direct contact with confirmed or suspected COVID-19 cases.14 Even though 79.5% reported adequate availability of PPE, 56.9% were afraid that they would be infected with COVID-19. A higher percentage of fear was reported in China; 85% of HCPs were afraid of becoming infected at work.65 Although some HCPs might need psychosocial support, they rarely seek help.66 Similarly, the current results showed that 57% of the participants suggested a need for professional support to deal with stress during the COVID-19 pandemic. HCPs involved in the care of COVID-19 patients should undergo regular evaluations of stress, depression, and anxiety levels to support their wellbeing.14 , 66 Our findings also acknowledge the requirement of creating awareness of the need for professional support amongst the RWF in dealing with stress, anxiety and other psychological disorders that might arise during the COVID-19 pandemic and similar crises.
Stress can produce biophysical reactions, such as headache, abdominal pain, chest pain, eating and sleep disturbances and heart palpitation, as well as; psychological–emotional reactions, such as anxiety, depression, tension, anger, nervousness and frustration.26 The current study showed that 18% of respondents had eating problems, such as nausea and stomach problems, and 19% reported trouble falling or staying asleep after the pandemic began. Eating problems are often associated with anxiety67 and anxious people find it difficult to fall asleep and may wake up frequently during the night.68 The COVID-19 pandemic has become a significant stressor and studies in China found that medical professionals reported elevated levels of depression, stress, anxiety and insomnia.66 , 69 Stress and anxiety are linked to fear.27 Fear is a present response when facing a real or supposed threat, while anxiety is a future response that indicates an impending danger.25 Anxiety and fear are likely distinct emotional states but often overlap due to underlying behavioural mechanisms.28
The result of the current study found no significant association between anxiety level and gender, age, experience, country, workplace, or work status was demonstrated in the present study, even though the countries varied in their readiness and strategies for tackling the new pressures. The lack of association with age or gender may indicate that the interaction and support level between different workers was so high and effective during stressful times that it helped to lift people and homogenize their responses. Likewise, no significant association was found between the fear of COVID-19 and gender, experience, or country. Nevertheless, in the current study, fear of COVID-19 was strongly associated with participants from 18 to 29 years of age and also with respondents'work status. A recent study documented that the safety of medical staff during the pandemic and lack of treatment for COVID-19 were the main factors that induced stress in all medical staff, with no significant differences between the study groups.70
Furthermore, a different review study found that increasing evidence suggests that COVID-19 can be an independent risk factor for stress among HCPs.71 In the current study, temporary staff showed a higher level of fear, which might be due to the relatively lower practical experience of students or the experience of retired workers of being away from work. Therefore, it is suggested that temporary staff be engaged in expeditious training to update their skills and knowledge. Our findings accordingly suggest that training in infection control does influence fear, and workers who attended this type of training had a lower fear score than those who did not. Moreover, training in stress management helped to prevent and reduce COVID-19 fear, stress and anxiety.49 , 72
Strengths and limitations
The main strengths of this study were the robust actions taken to document the radiology response in multiple countries and providing insight into the RWF's health and wellbeing. Moreover, our ability to assess the impact of the COVID-19 pandemic on radiology practices and associated factors, such as fear and anxiety, among the RWF provided more insight into the psychological needs of medical workers to continue providing quality service.
The study was limited by our inability to capture the underlying reasons for participants’ responses as well as their expectations and ideas for service improvement during future pandemics. We also acknowledge the existence of differences in social and cultural stress factors across the countries studied, which likely influenced our findings.
Conclusions
It is extremely important to investigate the mental and physical health of HCPs serving in the MENAIN region to handle the current pandemic and also prepare for potential future pandemic situations. The results of the current study revealed the status of the RWF in terms of workforce, fear, stress and anxiety. It was demonstrated that the workload changed in a bipolar way; it increased by 38% due to pressure on general x-ray and CT scanning as they were the initial and follow-up investigations for COVID-19 patients, and also decreased by 23% due to adherence to national and international guidance to minimize non-urgent work. There was adequate availability of PPE; however, radiology workers still worried about becoming infected with COVID-19. We found that 42.9% of the respondents began to experience work-related stress after the COVID-19 pandemic began and 57.1% felt that they might need professional help to deal with stress during the COVID-19 pandemic.
Fear was associated with workers younger than 30 years of age and also with temporary staff. Nevertheless, anxiety occurred completely independently of gender, age, experience, country, working environment and work status. Therefore, professional support is needed to reduce or prevent fear, stress, and anxiety among HCPs. It is imperative to establish clear directives, initiate precautionary measures, provide informed health interventions, obtain support from family and increase the productivity of the RWF in preparation for both current and future outbreaks.
Funding
None
Declarations of interest
None
Acknowledgement
The authors would like to thank all participants in the study for taking time off their busy schedules in such unprecedented times to complete the survey. We also appreciate the support received from the Society of Radiographers & Radiological Technologists and colleagues and alumni of the department of Medical Imaging Technology, Manipal University, India. Also, would like to thank Dr Saravanan Coumaravelou for his advice.
References
- 1.World Health Organization WHO Director-General's opening remarks at the media briefing on COVID-19. 11 March 2020. https://www.who.int/dg/speeches/detail/who-director-general-s-openingremarks-at-the-media-briefing-on-covid-19---11-march-2020 Available from: Retrieved from.
- 2.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joob B., Wiwanitkit V. Radiology management and COVID-19 in resource limited setting. Acad Radiol. 2020;27(5):750. doi: 10.1016/j.acra.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D., Hu B., Hu C., Zhu F., Liu X., Zhang J. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in wuhan, China. J Am Med Assoc. 2020;323(11) doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xu X., Yu C., Zhang Z., Jiang R., Ding Y., Lin L. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imag. 2020;47(5):1275–1280. doi: 10.1007/s00259-020-04735-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yu J., Ding N., Chen H., Liu X.-J., He W.-J., Dai W.-C. Infection control against COVID-19 in departments of radiology. Acad Radiol. 2020;27(5):614–617. doi: 10.1016/j.acra.2020.03.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhang J., Xie Y., Li Y., Shen C., Xia Y. COVID-19 screening on chest X-ray images using deep learning based anomaly detection. arXivorg. 2020 https://arxiv.org/abs/2003.12338 Retrieved from. [Google Scholar]
- 8.Xiong Y., Sun D., Liu Y., Fan Y., Zhao L., Li X. Clinical and high-resolution CT features of the COVID-19 infection: comparison of the initial and follow-up changes. Invest Radiol. 2020;55(6):332–339. doi: 10.1097/RLI.0000000000000674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tan C., Huang Y., Shi F., Tan k., Ma Q., Chen Y. C-reactive protein correlates with computed tomographic findings and predicts severe COVID-19 early. J Med Virol. 2020;92(7) doi: 10.1002/jmv.25871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cao Y., Liu X., Xiong L., Cai K. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2: a systematic review and meta-analysis. J Med Virol. 2020;92(9) doi: 10.1002/jmv.25822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kotian R., Faujdar D., Kotian S., D'souza B. Knowledge and understanding among medical imaging professionals in India during the rapid rise of the COVID-19 pandemic. Nature Public Health Emergency Collection. 2020:1–6. doi: 10.1007/s12553-020-00437-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cieszanowski A., Czekajska E., Giżycka B., Gruszczyńska K., Podgórska J., Oronowicz-Jaśkowiak A. Management of patients with COVID-19 in radiology departments, and indications regarding imaging studies - recommendations of the Polish Medical Society of Radiology. Pol J Radiol. 2020;85 doi: 10.5114/pjr.2020.95022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xiao C. A novel approach of consultation on 2019 novel coronavirus (COVID-19)-related psychological and mental problems: structured letter therapy. Psychiatry investigation. 2020:175. doi: 10.30773/pi.2020.0047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rana W., Mukhtar S., Mukhtar S. Mental health of medical workers in Pakistan during the pandemic COVID-19 outbreak. Asian journal of psychiatry. 2020;51:102080. doi: 10.1016/j.ajp.2020.102080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen K.-Y., Yang C.-M., Lien C.-H., Chiou H.-Y., Lin M.-R., Chang H.-R. Burnout, job satisfaction, and medical malpractice among physicians. Int J Med Sci. 2013;10(11):1471. doi: 10.7150/ijms.6743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Adams J.G., Walls R.M. Supporting the health care workforce during the COVID-19 global epidemic. J Am Med Assoc. 2020;323(15) doi: 10.1001/jama.2020.3972. [DOI] [PubMed] [Google Scholar]
- 17.Maunder G.R., Lancee J.W., Rourke J.S., Hunter S.L.J., Goldbloom S.L.D., Balderson S.L.K. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in toronto. Psychosom Med. 2004;66(6):938–942. doi: 10.1097/01.psy.0000145673.84698.18. [DOI] [PubMed] [Google Scholar]
- 18.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Publ Health. 2020;17(5) doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Qian Hui C.W., Chiah Ker, Vasoo S., Chua H.C., Sim K. Narrative synthesis of psychological and coping responses towards emerging infectious disease outbreaks in the general population: practical considerations for the COVID -19 pandemic. Singap Med J. 2020:1–31. doi: 10.11622/smedj.2020046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McAlonan G.M., Lee A.M., Cheung V., Cheung C., Tsang K.W., Sham P.C. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatr. 2007;52(4):241–247. doi: 10.1177/070674370705200406. [DOI] [PubMed] [Google Scholar]
- 21.Lehmann M., Bruenahl C.A., Lowe B., Addo M.M., Schmiedel S., Lohse A.W. Ebola and psychological stress of health care professionals. Emerg. infect. Dis. 2015;21(5):913. doi: 10.3201/eid2105.141988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lazarus R.S. Oxford University Press; New York: New York: 1991. Emotion and adaptation.https://www.researchgate.net/profile/Craig_Smith11/publication/232438867_Emotion_and_Adaptation/links/00463536ae7d206717000000.pdf Retrieved from. [Google Scholar]
- 23.Liu X., Kakade M., Fuller C.J., Fan B., Fang Y., Kong J. Depression after exposure to stressful events: lessons learned from the severe acute respiratory syndrome epidemic. Compr Psychiatr. 2012;53(1):15–23. doi: 10.1016/j.comppsych.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wu P., Fang Y., Guan Z., Fan B., Kong J., Yao Z. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatr. 2009;54(5):302–311. doi: 10.1177/070674370905400504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bakioğlu F., Korkmaz O., Ercan H. Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int J Ment Health Addiction. 2020 May 31:1. doi: 10.1007/s11469-020-00331-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Saleh M.S., Eltahlawy E., Amer N. Job satisfaction and prevalence of stress signs. International Journal of Research in Environmental Sciences. 2016;2:28–35. [Google Scholar]
- 27.Fink G. InStress: concepts, cognition, emotion, and behavior. Academic Press; 2016 Jan 1. Stress, definitions, mechanisms, and effects outlined: lessons from anxiety; pp. 3–11. [Google Scholar]
- 28.Steimer T. The biology of fear-and anxiety-related behaviors. Dialogues Clin Neurosci. 2002 Sep;4(3):231. doi: 10.31887/DCNS.2002.4.3/tsteimer. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marjanovic Z., Greenglass E.R., Coffey S. The relevance of psychosocial variables and working conditions in predicting nurses' coping strategies during the SARS crisis: an online questionnaire survey. Int J Nurs Stud. 2007;44(6):991–998. doi: 10.1016/j.ijnurstu.2006.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shanafelt T., Ripp J., Trockel M. Understanding and addressing sources of anxiety among health care professionals during the COVID-19 pandemic. J Am Med Assoc. 2020;323 doi: 10.1001/jama.2020.5893. [DOI] [PubMed] [Google Scholar]
- 31.Schulz M., Damkröger A., Voltmer E., Löwe B., Driessen M., Ward M. Work-related behaviour and experience pattern in nurses: impact on physical and mental health. J Psychiatr Ment Health Nurs. 2011;18(5):411. doi: 10.1111/j.1365-2850.2011.01691.x. [DOI] [PubMed] [Google Scholar]
- 32.Maunder R., Lancee W.J., Balderson K.E., Bennett J.P., Borgundvaag B., Evans S. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. (RESEARCH) Emerg Infect Dis. 2006;12(12):1924. doi: 10.3201/eid1212.060584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Goulia P., Mantas C., Dimitroula D., Mantis D., Hyphantis T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect Dis. 2010;10:322. doi: 10.1186/1471-2334-10-322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kahia M., Jebli M.B., Belloumi M. Analysis of the impact of renewable energy consumption and economic growth on carbon dioxide emissions in 12 MENA countries. Clean Technol Environ Policy. 2019 May 15;21(4):871–885. doi: 10.1007/s10098-019-01676-2. [DOI] [Google Scholar]
- 35.Mauldin W.P. Population growth. Routledge; 2017 Jul 5. The population of India; pp. 191–205. [Google Scholar]
- 36.Wood J.T. Nelson Education; 2015. Interpersonal communication: everyday encounters. [Google Scholar]
- 37.Collins H. World Bank Publications; 2013. Atlas of global development: a visual guide to the world's greatest challenges; pp. 24–25.https://books.google.ae/books?hl=en&lr=&id=M6dQsbipkrEC&oi=fnd&pg=PR1&dq=Atlas+of+global+development:+a+visual+guide+to+the+world%27s+greatest+challenges&ots=g4WciPYmQr&sig=_KhBFoMkufMbSLaq63L6q4NeI6g&redir_esc=y#v=onepage&q=Atlas%20of%20global%20development%3A%20a%20visual%20guide%20to%20the%20world's%20greatest%20challenges&f=false Retrieved from: [Google Scholar]
- 38.Sedgwick P. Cross sectional studies: advantages and disadvantages. Bmj. 2014 Mar 26:348. doi: 10.1136/bmj.g2979. [DOI] [PubMed] [Google Scholar]
- 39.Elman C., Gerring J., Mahoney J. The Production of Knowledge: Enhancing Progress in Social Science. Cambridge University Press; 2020 Mar 19. [Google Scholar]
- 40.Akudjedu T.N., Lawal O., Sharma M., Elliott J., Stewart S., Gilleece T. Impact of the COVID-19 pandemic on radiography practice: findings from a UK radiography workforce survey. BJR| Open. 2020 Sep;2:20200023. doi: 10.1259/bjro.20200023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee S.A. Coronavirus Anxiety Scale: a brief mental health screener for COVID-19 related anxiety. Death Stud. 2020;44(7):393–401. doi: 10.1080/07481187.2020.1748481. [DOI] [PubMed] [Google Scholar]
- 42.Lee S.A. Replication analysis of the coronavirus anxiety scale. Düşünen Adam J Psychiatry Neurol Sci. 2020;33(2) doi: 10.14744/DAJPNS.2020.00079. [DOI] [Google Scholar]
- 43.Ahorsu D.K., Lin C.-Y., Imani V., Saffari M., Griffiths M.D., Pakpour A.H. The fear of COVID-19 scale: development and initial validation. Int J Ment Health Addiction. 2020:1–9. doi: 10.1007/s11469-020-00270-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Labrague L., De los Santos J.A. COVID-19 anxiety among frontline nurses: predictive role of organisational support, personal resilience and social support. medRxiv. 2020 doi: 10.1111/jonm.13121. Online ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Evren C., Evren B., Dalbudak E., Topcu M., Kutlu N. Measuring anxiety related to COVID-19: a Turkish validation study of the Coronavirus Anxiety Scale. Death Stud. 2020 Jun 2:1–7. doi: 10.1080/07481187.2020.1774969. [DOI] [PubMed] [Google Scholar]
- 46.Wang Y., Di Y., Ye J., Wei W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med. 2020 Mar 31 doi: 10.1080/13548506.2020.1746817. 1-0. [DOI] [PubMed] [Google Scholar]
- 47.Labrague LJ, De los Santos J. Fear of COVID-19, psychological distress, work satisfaction and turnover intention among front line nurses. [DOI] [PMC free article] [PubMed]
- 48.Satici B., Gocet-Tekin E., Deniz M.E., Satici S.A. Adaptation of the Fear of COVID-19 Scale: its association with psychological distress and life satisfaction in Turkey. Int J Ment Health Addiction. 2020 May 8:1. doi: 10.1007/s11469-020-00294-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Reznik A., Gritsenko V., Konstantinov V., Khamenka N., Isralowitz R. COVID-19 fear in eastern europe: validation of the fear of COVID-19 scale. Int J Ment Health Addiction. 2020 May 12:1. doi: 10.1007/s11469-020-00283-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Stogiannos N., Fotopoulos D., Woznitza N., Malamateniou C. Coronavirus disease 2019 (COVID-19) in the radiology department: what radiographers need to know. Radiography. 2020;26(3):254–263. doi: 10.1016/j.radi.2020.05.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Desta M A., Ayenew T., Sitotaw N., Tegegne N., Dires M., Getie M. Knowledge, practice and associated factors of infection prevention among healthcare workers in Debre Markos referral hospital, Northwest Ethiopia. BMC Health Serv Res. 2018;18(1):465. doi: 10.1186/s12913-018-3277-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stein A.D., Makarawo T.P., Ahmad M.F. A survey of doctors' and nurses' knowledge, attitudes and compliance with infection control guidelines in Birmingham teaching hospitals. J Hosp Infect. 2003;54(1):68–73. doi: 10.1016/S0195-6701(03)00074-4. [DOI] [PubMed] [Google Scholar]
- 53.Chan A.K.M., Nickson C.P., Rudolph J.W., Lee A., Joynt G.M. 2020. Social media for rapid knowledge dissemination: early experience from the COVID-19 pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wong H.Y.F., Lam H.Y.S., Fong A.H.-T., Leung S.T., Chin T.W.-Y., Lo C.S.Y. Frequency and distribution of chest radiographic findings in COVID-19 positive patients. Radiology. 2019:201160. doi: 10.1148/radiol.2020201160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.World Health Organization . 2020. COVID-19 technical guidance: infection prevention and control/WASH; p. 2020.https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technicalguidance/infection-prevention-and-control Retrieved from. [Google Scholar]
- 56.Department of Health . 2020. Temporary pause of routine screening programmes.https://www.health-ni.gov.uk/news/temporary-pause-routine-screeningprogrammes Retrieved from. [Google Scholar]
- 57.Jacobi A., Chung M., Bernheim A., Eber C. Portable chest X-ray in coronavirus disease-19 (COVID-19): a pictorial review. Clin Imag. 2020;64:35–42. doi: 10.1016/j.clinimag.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Elshami W., Abuzaid M., Piersson A.D., Mira O., AbdelHamid M., Zheng X. Occupational dose and radiation protection practice in uae: a retrospective cross-sectional cohort study (2002–2016) Radiat Protect Dosim. 2019 Dec 31;187(4):426–437. doi: 10.1093/rpd/ncz184. [DOI] [PubMed] [Google Scholar]
- 59.Abuzaid M.M., Elshami W., Noorajan Z., Khayal S., Sulieman A. Assessment of the professional practice knowledge of computed tomography preceptors. European Journal of Radiology Open. 2020 Jan 1;7:100216. doi: 10.1016/j.ejro.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elshami W., Abuzaid M.M., Tekin H.O. Effectiveness of breast and eye shielding during cervical spine radiography: an experimental study. Risk Manag Healthc Pol. 2020;13:697–704. doi: 10.2147/RMHP.S257185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Peiffer-Smadja N., Lucet J.C., Bendjelloul G., Bouadma L., Gerard S., Choquet C. Challenges and issues about organizing a hospital to respond to the COVID-19 outbreak: experience from a French reference centre. Clin Microbiol Infect. 2020:669. doi: 10.1016/j.cmi.2020.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sim K., Huak Chan Y., Chong P.N., Chua H.C., Wen Soon S. Psychosocial and coping responses within the community health care setting towards a national outbreak of an infectious disease. J Psychosom Res. 2010;68(2):195–202. doi: 10.1016/j.jpsychores.2009.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hall R.C.W., Hall R.C.W., Chapman M.J. The 1995 Kikwit Ebola outbreak: lessons hospitals and physicians can apply to future viral epidemics. Gen Hosp Psychiatr. 2008;30(5):446–452. doi: 10.1016/j.genhosppsych.2008.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Montemurro N. The emotional impact of COVID-19: from medical staff to common people. Brain Behav Immun. 2020;87 doi: 10.1016/j.bbi.2020.03.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhou M., Tang F., Wang Y., Nie H., Zhang L., You G. Knowledge, attitude and practice regarding COVID-19 among health care workers in Henan, China. J Hosp Infect. 2020 Apr 9;105(2) doi: 10.1016/j.jhin.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Xiang Y.T., Yang Y., Li W., Zhang L., Zhang Q., Cheung T. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. The Lancet Psychiatry. 2020:228–229. doi: 10.1016/S2215-0366(20)30046-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Swinbourne J., Hunt C., Abbott M., Russell J., St Clare T., Touyz S. The comorbidity between eating disorders and anxiety disorders: prevalence in an eating disorder sample and anxiety disorder sample. Aust N Z J Psychiatr. 2012 Feb;46(2):118–131. doi: 10.1177/0004867411432071. [DOI] [PubMed] [Google Scholar]
- 68.Xiao H., Zhang Y., Kong D., Li S., Yang N. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Mon Int Med J Exp Clin Res: international medical journal of experimental and clinical research. 2020;26 doi: 10.12659/MSM.923549. e923549-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R. Brain, behavior, and immunity; 2020 Mar 10. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cai H., Tu B., Ma J., Chen L., Fu L., Jiang Y. vol. 26. Med Sci Monit; 2020. Q Psychological impact and coping strategies of frontline medical staff in Hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID19) in Hubei. (China med sci monit). 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian J Psychiatr. 2020 Jun 1;51:102119. doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Ornell F., Schuch J.B., Sordi A.O., Kessler F.H. “Pandemic fear” and COVID-19: mental health burden and strategies. Brazilian Journal of Psychiatry. 2020 Jun;42(3):232–235. doi: 10.1590/1516-4446-2020-0008. [DOI] [PMC free article] [PubMed] [Google Scholar]