Abstract
Background
Cancer patients had been profoundly affected by the outbreak of COVID-19 especially after quarantine restrictions in China. We aimed to explore the treatment changes and delays of early breast cancer (EBC) during the first quarter of 2020.
Methods
We did this retrospective, multicentre, cohort study at 97 cancer centres in China. EBC patients who received treatment regardless of preoperative therapy, surgery or postoperative therapy during first quarter of 2020 were included.
Findings
8397 patients were eligible with a median age of 50 (IQR 43–56). 0·2% (15/8397) of EBC patients were confirmed as COVID-19 infection. Only 5·2% of breast cancer diagnosis occurred after quarantine in Hubei compared with 15·3% in other provinces (OR= 0·30, 95%CI 0·24–0·38). postoperative endocrine therapy were least affected compared with different regions after quarantine (OR=0·37 [95%CI 0·19–0·73]). The proportion of surgery decreased from 16·4% in December last year to 2·6% in February in Hubei. Compared with intervals from diagnosis to treatment before quarantine restrictions, the average time increased with significance from 3·5 to 7·7 days in Hubei and 5·7 to 7·7 days in other provinces (p< 0·001). There were also 18·5 and 7·2 days delay in Hubei and other provinces respectively when calculating interval from surgery to postoperative therapy.
Interpretation
EBC from high risk regions had a comparative rate of COVID-19 infection. After implementation of COVID-19 quarantine restrictions, fewer diagnosis and surgery with significant delays were seen when compared with treatment before.
Funding
Beijing Medical Award Foundation (YJ0120)
Key words: Early breast cancer, COVID-19, Quarantine restrictions, Treatment decline, Delay, Regional disparity
Research in context.
Evidence before this study
We searched PubMed on June 4, 2020, for reports published in English and describing the influence of cancer patients from COVID-19 with the search terms “COVID-19 or SARS-CoV-2 or 2019-nCoV or novel coronavirus” AND “tumour or carcinoma or cancer”. We found patients with cancer and COVID-19 who were admitted to hospital had a high case-fatality rate. They were more likely to deteriorate into severe illness than those without cancer. One comment discussed potential deleterious effect of delaying radiotherapy. Another comment found that fewer cancer diagnosed during COVID-19. However, we found no published articles with a large sample size from multicentre describing the distribution changes and delays of cancer treatment especially after COVID-19 quarantine restrictions in China.
Added value of this study
In this retrospective, multicentre, cohort study, we report treatment of breast cancer and its delays during the first quarter of 2020. 15 early breast cancer patients in Hubei were confirmed as COVID-19. Fewer cancer diagnosis and surgery were performed since January 23, a critical time point of response to COVID-19 in China. Significant decreases in diagnosis and surgery were found in both Hubei and other provinces especially in February in China. Patients received diagnosis or surgery had significant longer intervals to receive their following treatments since quarantine restrictions.
Implications of all the available evidence
Quarantine restrictions has a positive impact on COVID-19 transmission while a negative impact on regular cancer therapy. Low infection rates of COVID-19 while remarkable reductions and delays in treatment showed that more attentions should be paid to those uninfected patients as the widespread of COVID-19 has been under control in China. Too much emphasis on avoiding COVID-19 infection could delay cancer treatment, and could ultimately increase the potential risk of relapse.
Alt-text: Unlabelled box
1. Introduction
The outbreak of the Coronavirus disease 2019 (COVID-19) has had a profound impact on humanity [1,2]. As of June 5, the World Health Organization has reported over 6416,828 confirmed cases worldwide [3]. Experiences from the Severe Acute Respiratory Syndrome(SARS), Middle East Respiratory Syndrome (MERS) and other outbreaks has shown that we face an urgent need to expand public health activities to avoid the potential collapse from those novel viruses [4].
A series of actions have been taken to reduce the transmission of COVID-19. Patients with fever or suspicious respiratory symptoms are preferentially hospitalized, certain health-care institutions had to postpone non-urgent appointments due to the urgent requisition of medical resources [5,6]. China has initiated three levels of response to COVID-19 in different regions after the epidemic. As the epicentre of COVID −19, Hubei and its capital Wuhan, have suspended public transportation and taken the highest emergency response since January 23 [7],making COVID-19 a social concern. These measures are highly necessary to curb the epidemic from spreading [8].
However, those actions may also hamper the response to patients with other diseases [9], especially for those with cancer. It is important for cancer patients to maintain their effective therapies because delayed therapy may deteriorate their conditions and increase the risk of relapse [10]. Unfortunately, exactly how cancer patients receive their regular therapy without interference from COVID-19 has yet to be established [11,12].
We have addressed ten hot issues for breast cancer patients at the beginning of February this year to mitigate the potential negative impacts from quarantine restrictions [13]. From our own practise, preoperative therapy and manageable postoperative endocrine therapy were encouraged. While chemotherapy with high risk to febrile neutropenia or surgery like modified radical mastectomy are discouraged during the pandemic. These suggestions combine with experience from frontline oncologists [14] have contributed to better managements of cancer patients.
Nevertheless, there is still a lack of sufficient data to tell us how COVID-19 has affected regular cancer therapy during this period. Under these perquisites, we've conducted this national survey (CSCO BC NCP-01) to uncover how patients with early breast cancer get their regular treatments during the first quarter (Q1) of 2020 and to explore the real delays from different regions and different periods.
2. Methods
2.1. Study design and participants
This study is a Chinese Society of Clinical Oncology Breast Cancer committee-initiated survey on Novel Coronavirus Pneumonia (CSCO BC NCP-01) done at 97 specialist cancer centres across 19 provinces. All the directors of these cancer centres were from or had good cooperative relations with CSCO BC committee.
We invited all centres to contribute data for patients diagnosed as early breast cancer with clear pathological results and their treatment records and had received at least one therapy such as preoperative therapy, surgery or postoperative therapy during Q1 of 2020. All patients meeting those criteria should be included to avoid possible selection bias. All of them were first followed up on March 31, 2020.
This study was done in accordance with the principles of Good Clinical Practice, the Declaration of Helsinki, and Chinese regulations. The central ethics committee approved the study protocol. This study was registered with Chinese Clinical Trial Registry (ChiCTR2000033200).
2.2. Procedures
Demographic, clinical treatment and outcome data were extracted from electronic medical records through questionnaire. Data concerning diagnosis and treatments before Q1 of 2020 were also recorded as controls. The questionnaire was designed based on the Chinese Society of Clinical Oncology Breast Cancer Committee Database established in 2017. Details regarding COVID-19 were added to this questionnaire to fulfil this national survey.
From April 1 to May 15, local medical workers collected the data from electronic medical records according to inclusion criteria. Doctors from local hospitals were responsible for the initial check of these data. If data did not meet the inclusion criteria, a query would be sent to local centres to complete the survey. Each record would be checked again by centre medical workers.
2.3. Outcomes
The primary outcome was COVID-19 infection rate. Nucleic acid test was performed to clarify COVID-19 infections. Another primary outcome was time intervals of different therapies which can be divided into three indicators according to their therapies. i) diagnosis to treatment: time (in days) from diagnosis to therapy whether it is preoperative therapy or surgery; ii) preoperative therapy to surgery: time (in days) from preoperative to surgery; iii) surgery to postoperative therapy: time (in days) from surgery to postoperative therapy whether it is chemotherapy or other therapy. Secondary objective was treatment distribution which was defined as the proportion of patients receiving different treatment (newly diagnosis, preoperative therapy, surgery and postoperative therapy) in the same periods. Event free survival, calculated as the interval from randomisation to the earliest occurrence of disease progression resulting inoperability, recurrence, metastases or death from any cause, will not be reported in this article due to the limited follow-ups
2.4. Statistical analysis
For primary outcomes, we used a two-way analysis of variance (ANOVA) to test for significance of the differences in averages between different regions (Hubei province or not) and different time period (before restriction or after). Bonferroni test was used to correct for multiple comparisons. To compare treatment delays and distributions, previous treatments of these enroled patients were regard as control group. Dates are crucial to calculate the time intervals and to classify therapy distributions. However, missing dates were common, especially in the early years. Excluding all these data would produce a spuriously treatment distributions, which would have led us to underestimate the actual efficacy of COVID-19 on cancer patients. To avoid this bias, we excluded those data with missing days when calculating time intervals, while including them when exploring therapy distributions. Dates with missing year or month were excluded.
We used odds ratios, calculated with Mantel–Haenszel models, for possible differences in treatment between the different regions and periods. A two-sided α of less than 0·05 was considered statistically significant. Statistical analysis was done using SPSS software.
2.5. Role of funding source
Beijing Medical Award Foundation provided financial support to this trial, but had no roles in study design, data collection, data analysis, data interpretation, or the writing of this report. CSCO BC Database Collaborative Group provided support in data collection. Corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
3. Results
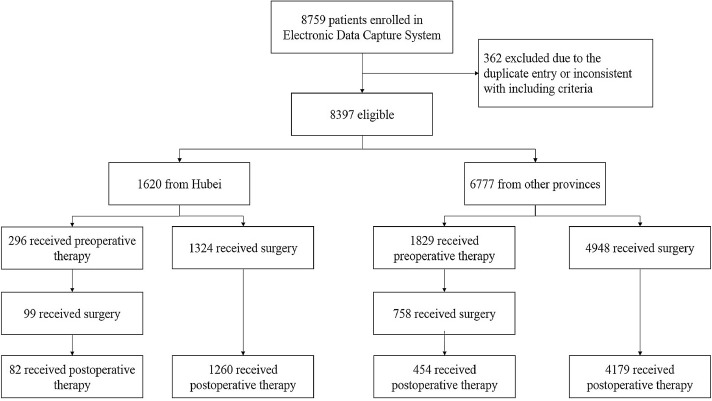
After excluding 362 patients due to the duplicate entry or inconsistent with including criteria, 8397 early breast cancer patients from 97 hospitals (Appendix 1) received cancer treatments during Q1 of this year (Fig. 1). 1620 patients of 43 hospitals were from Hubei province, 6777 patients of 54 hospitals were from other provinces. The median age of these patients were 50 (IQR 43–56) (Table 1). Their diagnosis time ranged from 2014 to 2020. Compared with patients in other provinces, patients in Hubei had a higher proportion in receiving surgery (87·8% vs.84·2%) and postoperative therapy (82·8% vs. 68·4%). (Table 1). All patients were followed up to March 31.
Fig. 1.
Trial profile.
Table 1.
Baseline characteristics of the population.
| Characteristics | Overall | Hubei | Other provinces | p |
|---|---|---|---|---|
| N = 8397(%) | n = 1620(%) | n = 6777(%) | ||
| Ages | ||||
| Median | 50 | 50 | 50 | 0.44 |
| IQR | 43, 56 | 44, 56 | 43, 57 | |
| Sex | ||||
| Male | 34(0.4) | 8(0.5) | 26(0.4) | |
| Female | 8363(99.6) | 1612(99.5) | 6751(99.6) | 0.53 |
| COVID-19 infection | ||||
| Yes | 15(0.2) | 15(0.9) | 0 | |
| No | 8382(99.8) | 1605(99.1) | 6777(100.0) | – |
| Clinical T stage | ||||
| T1–2 | 7108(84.6) | 1430(88.3) | 5678(83.8) | |
| T3–4 | 683(8.1) | 133(8.2) | 550(8.1) | 0.69 |
| Unknown | 606(7.2) | 57(3.5) | 549(8.1) | |
| Clinical N stage | ||||
| Negative | 4216(50.2) | 830(51.2) | 3386(50.0) | |
| Positive | 3694(44.0) | 712(44.0) | 2982(44.0) | 0.64 |
| Unknown | 487(5.8) | 78(4.8) | 409(6.0) | |
| Subtypes | <0.0001 | |||
| ER/PR +,HER2- | 3426(40.8) | 565(34.9) | 2861(42.2) | |
| ER/PR +,HER2+ | 1589(18.9) | 340(21.0) | 1249(18.4) | |
| ER/PR -,HER2+ | 1168(13.9) | 309(19.1) | 859(12.7) | |
| Triple negative | 1031(12.3) | 254(15.7) | 777(11.5) | |
| Unknown | 1183(14.2) | 152(9.4) | 1031(15.2) | |
| Histological grade | ||||
| Grade 1–2 | 3801(45.3) | 802(49.8) | 2999(44.3) | |
| Grade 3 | 1876(22.3) | 493(30.0) | 1383(20.4) | <0.0001 |
| unknown | 2720(32.4) | 325(20.2) | 2395(35.3) | |
| Neoadjuvant therapy | ||||
| Yes | 2125(25.3) | 296(18.3) | 1829(27.7) | |
| No | 6272(74.7) | 1324(81.7) | 4948(72.3) | <0.0001 |
| Surgery | ||||
| Yes | 7129(84.9) | 1423(87.8) | 5706(84.2) | |
| No | 1268(15.1) | 197(12.2) | 1071(15.8) | <0.0001 |
| Adjuvant therapy | ||||
| Yes | 5975(71.2) | 1342(82.8) | 4633(68.4) | |
| No | 2422(18.8) | 278(17.2) | 2144(31.6) | <0.0001 |
Data are median (range) or number (%), p value was calculated by excluded unknown data.
IQR= interquartile range, ER= oestrogen receptor, PR=progesterone receptor.
By the data cut-off date (March 31,2020), 0·9% (15/1620) of patients in Hubei province were COVID-19 positive. 14 breast cancer patients had positive nucleic acid result for SARS-CoV-2, the other one was confirmed by positive serum specific IgG antibody with negative result of nucleic acid. amongst all patients, 40·0% (6/15) were older than 60·2 patients received surgery prior to infection, 12 patients received chemotherapy and 1 received aromatase inhibitor. Two cases of death were found after infections. A newly operated 85-year old female receiving her postoperative aromatase inhibitor endocrine therapy and a 24-year old female receiving her first cycle of anthracycline and cyclophosphamide postoperative chemotherapy(Table 2).
Table 2.
Clinical characteristics of early breast cancer with COVID-19.
| Case1 | Case2 | Case3 | Case4 | Case5 | Case6 | Case7 | Case8 | Case9 | Case10 | Case11 | Case12 | Case13 | Case14 | Case15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 47 | 62 | 64 | 44 | 51 | 47 | 62 | 57 | 56 | 24 | 60 | 66 | 40 | 43 | 85 |
| T | 3 | 2 | 2 | 3 | 2 | 2 | 2 | 2 | 1 | 1 | 1 | 1 | UK | 2 | 2 |
| N | 3 | 0 | 0 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 3 | UK | 0 | 0 |
| ER/PR | – | UT | – | + | – | + | – | + | – | + | – | – | – | + | + |
| HER2 | + | UT | UK | + | + | – | – | – | + | – | + | – | + | + | – |
| NST | YES | NO | NO | YES | YES | NO | NO | NO | NO | NO | NO | NO | NO | NO | NO |
| Surgery | NO | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES | YES |
| AST | NO | YES | NO | YES | YES | YES | YES | YES | YES | YES | YES | YES | NO | YES | YES |
| Last therapy | DOC | DOC | Surgery | H | H | AC | DOC | AC | AC | AC | AC | AC | Surgery | DOC+H | AI |
| Time of last therapy | 1/27 | 1/20 | 1/15 | 1/15 | 2/12 | 1/27 | 1/10 | 1/22 | 1/23 | 1/18 | UK* | 1/22 | 1/4 | 1/15 | 1/23 |
| COVID-19 confirmed | 2/17 | 3/31 | 1/23 | 2/4 | 2/UNK | 2/21 | 3/17 | 1/31 | 2/3 | 1/23 | UK* | 2/8 | 3/12 | 2/5 | 2/1 |
| Event | Treating | Recovery | Recovery | Recovery | Recovery | Recovery | Recovery | Recovery | Recovery | Death | Recovery | Recovery | Treating | Recovery | Death |
| Time of event | 3/31 | 4/28 | 2/23 | 3/5 | 3/UNK | 3/10 | 4/10 | 2/13 | 3/1 | 2/6 | UK* | 3/13 | 3/31 | UK | 2/UK |
NST=Neoadjuvant systemic therapy, AST= adjuvant systemic therapy, DOC= Docetaxel, H= Trastuzumab, UT= Untested, UK= Unknown.AC= anthracyclines plus cyclophosphamide,.
Time of last therapy was defined as the last therapy concerning breast cancer. Event was defined as the outcome to COVID-19.
Case 11 was confirmed by positive serum specific IgG antibody with negative result of nucleic acid for SARS-CoV-2.
After the quarantine procedures took effect in China, there were significant differences in diagnosis and treatment from different regions. 13·3% of diagnosis occurred after quarantine restrictions. The proportion in Hubei province and other provinces was 5·2% and 15·3% respectively (OR=0·30,95%CI 0·24–0·38). Only 5·5% of surgeries were performed after restrictions in Hubei compared with 15·8% in other provinces. (OR=0·21,95%CI 0·17–0·27) (Table 3). Postoperative endocrine therapy were least affected when compared with different regions after quarantine restrictions(difference 5·4%, 95%CI 0·6–10·2). There was no statistical significance in radiotherapy (OR=0·71,95%CI 0·48–1·06) when compared with different regions.
Table 3.
Treatment after quarantine restrictions.
| Characteristics | Overall |
Hubei province |
Other provinces |
Difference (95% CI) | OR (95% CI) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | n | % | N | n | % | N | n | % | |||
| Diagnosis | 8322 | 1110 | 13.3 | 1620 | 84 | 5.2 | 6702 | 1026 | 15.3 | 10.1 (8.7–11.5) | 0.30 (0.24–0.38) |
| Neoadjuvant therapy | 2109 | 1304 | 61.8 | 295 | 157 | 53.2 | 1814 | 1147 | 63.2 | 10.0 (3.9–16.1) | 0.66 (0.52–0.85) |
| Surgery | 7075 | 1282 | 18.1 | 1423 | 78 | 5.5 | 5652 | 1204 | 21.3 | 15.8 (14.2–17.4) | 0.21 (0.17–0.27) |
| Adjuvant therapy | 5961 | 4692 | 78.7 | 1335 | 822 | 61.6 | 4626 | 3870 | 83.7 | 22.1 (19.3–24.9) | 0.31 (0.27–0.36) |
| Chemotherapy | 5123 | 3320 | 64.8 | 1267 | 627 | 49.5 | 3856 | 2693 | 69.8 | 20.3 (17.2–23.5) | 0.42 (0.37–0.48) |
| Anti-HER2 therapy | 1442 | 1016 | 70.5 | 341 | 190 | 55.7 | 1101 | 825 | 74.9 | 19.2 (13.4–25.1) | 0.42 (0.33–0.54) |
| Endocrine therapy | 1102 | 1055 | 95.7 | 145 | 132 | 91.0 | 957 | 923 | 96.4 | 5.4 (0.6–10.2) | 0.37 (0.19–0.73) |
| Radiotherapy | 771 | 418 | 54.2 | 117 | 55 | 47.0 | 654 | 363 | 55.5 | 8.5 (−1.3–18.3) | 0.71 (0.48–1.06) |
OR= odds ratio. N= total number. n= patients received treatment after quarantine restrictions.
Patients with unknown dates were excluded. Treatment in other provinces were treated as reference when calculating OR.
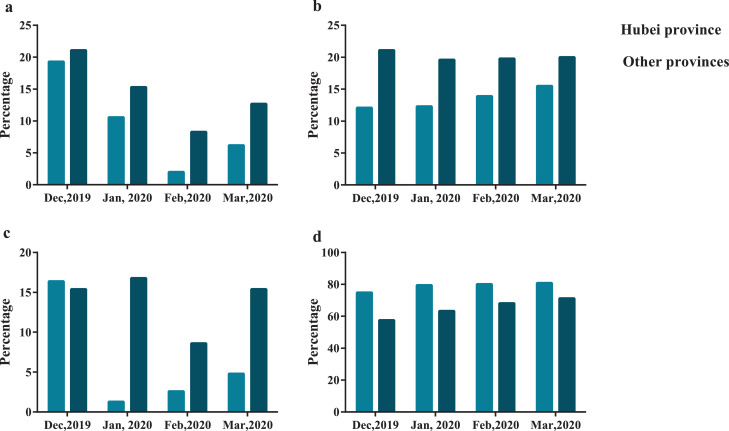
In comparison with treatments in 2019, a huge reduction of proportion was seen in diagnosis and surgery both in Hubei and other provinces (Fig. 2). In Hubei, over 15% of patients received surgery last year. This portion fell to 1·3%, 2·6% and 4·8% in January, February and March respectively (Fig. 2C). Only 2·0% of patients were newly diagnosed in February compared with 19·3% of patients in December last year in Hubei (Fig. 2a, Appendix 2). The reduction was also significant in other provinces especially in February (Fig. 2a and 2c). On the contrary, slight increases were seen in preoperative therapy in Hubei province and in postoperative setting in other provinces (Fig. 2b and 2d, Appendix 2).
Fig. 2.
Treatment distributions in different periods and regions
%=numbers of patients received relative treatment (diagnosis or preoperative therapy or surgery or postoperative therapy)in a month/total numbers of patients received diagnosis and treatment in that month
(a) diagnosis. (b)preoperative therapy. (c) surgery. (d) postoperative therapy.
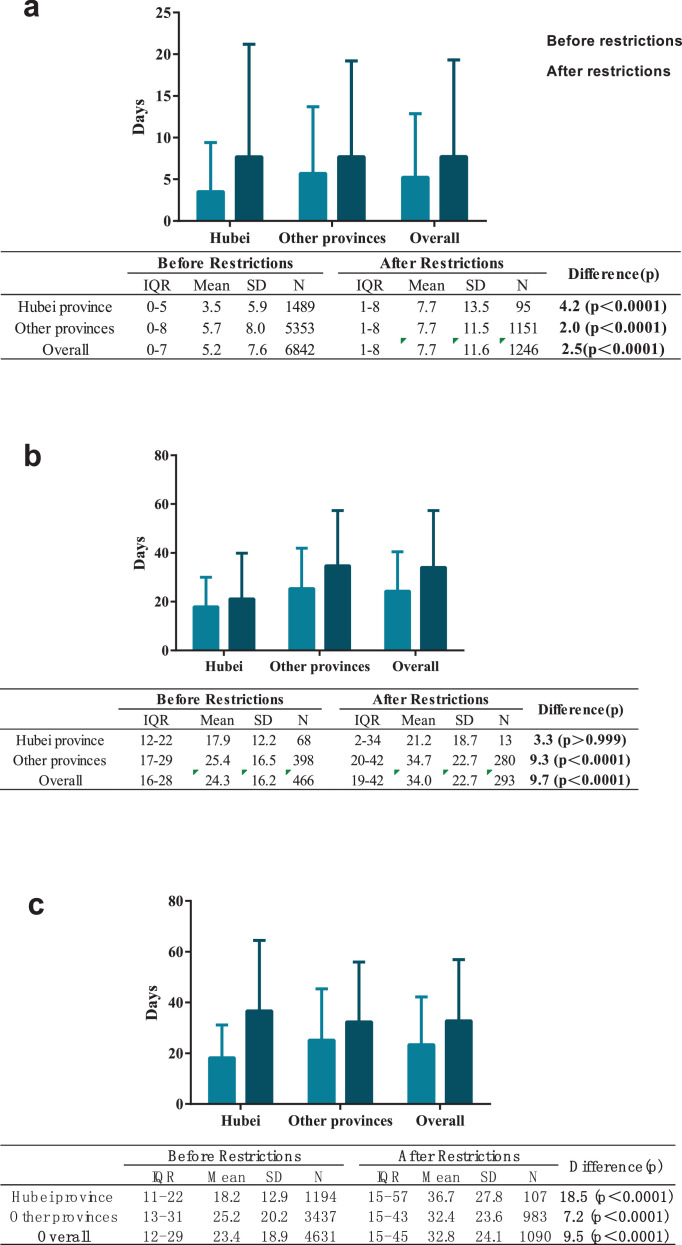
A total of 8088 cases were analysed in time from diagnosis to treatment. After quarantine restrictions, it took an average 7·7 day to receive treatment after diagnosis, 4·2 days delay than that before quarantine restrictions in Hubei compared with 2·0 days delay in other provinces (Fig. 3a). This delay was significant when the initiated treatment was surgery rather than preoperative therapy in Hubei province (Appendix 3–4). amongst the 2125 patients that had received preoperative therapy, 759 patients received surgery with clear dates. The average time from the end of preoperative therapy to surgery since restrictions was 34·7 days in other provinces, 9·3 days delay compared with the interval before. The average delay in Hubei province was not statistically significant perhaps due to the limited available data (17·9 days vs. 21·2 days, Fig. 3b).
Fig. 3.
Treatment delays for different therapy
(a) intervals from diagnosis to treatment, (b) interval from preoperative therapy to surgery and (c) intervals from surgery to postoperative therapy
Restrictions were performed since January 23 in China.
A total of 5721 cases were included in surgery to postoperative therapy analysis after excluding unknown dates for surgery or start of postoperative therapy. The average interval from surgery to postoperative therapy after quarantine restrictions was 36·7 days, 18·5 days delay compared with intervals before in Hubei province. The delay in other provinces was 7·2 days with significance in different periods (Fig. 3c). The delay was also significant in surgery to postoperative chemotherapy interval (17·3 days vs. 36·3 days in Hubei and 25·1 days vs. 31·8 days in other provinces, Appendix 3–4).
4. Discussion
In this national survey, only 0·2% of early breast cancer patients had a history of COVID-19 infection, all these confirmed cases were from Hubei province, two of them had passed away. We also found that quarantine restrictions for COVID-19 could have a negative impact on regular cancer therapy. Fewer patients were diagnosed and received surgical treatments since quarantine restrictions. A significant reduction was seen in February when compared with treatment distributions last year. Patients who were receiving preoperative or postoperative therapy were least affected. Additionally, our survey confirmed substantial delays of therapy for breast cancer patients after quarantine restrictions initiated in China.
Numerous articles have reported the clinical characteristics and the treatments for other patients combined with COVID-19 infection [15], [16], [17], providing valuable insights for us. From our study, although only 0·2% of EBC patients infected with COVID-19, all of them were from Hubei province. 0·9% of COVID-19 infection in Hubei province has shown the same percentage as other articles have reported. In China, less than 20% of COVID-19 infections occurred in other provinces, leading to the overall low infection rate in our study. Meanwhile, the widespread warning of infection, strict quarantine restrictions and the short time of follow-ups may also contribute to the low infection rates. Furthermore, most patients in our study received surgery and postoperative chemotherapy before infected. It is said that compromised immune systems are particularly vulnerable to infections [17]. Whether surgery or chemotherapy are determined risk factors of COVID-19 infection needs further examination. For two victims, dosage of chemotherapy or endocrine therapy were not exceed what the Chinese guideline [18] recommended, which means the death might be attributed to COVID-19 rather than breast cancer treatment. Considering the overall low infection rates compared with other studies [19], we can conclude that most cancer patients, especially in low infection risk regions, should receive their regular therapy without interference. Since the widespread of pandemic is more or less contained in China due to the effective quarantine restrictions, we should pay more attention to those uninfected patients.
It is said that quarantine restrictions could contribute to a notable reduction in diagnosis and treatment of breast cancer when compared with the period before [20,21]. Our results are highly consistent with this assume. In Hubei, the proportion of patients receiving treatment since restriction is much lower than that of other provinces. The decrease describes the substantial influence from the pandemic and quarantine restrictions especially on newly diagnosis and surgery. On the contrary, over 90% of patients received their endocrine therapy since quarantine restrictions in Hubei, showing minimum difference between Hubei and other regions. Indeed, the National Medical Security Bureau in China has launched a "long prescription" reimbursement policy, which will be conducive to promote endocrine therapy with low infection potential. This explains why patients receiving postoperative endocrine therapy are the least affected during this special time.
The mayhem caused by COVID-19 has brought about substantial changes in treatment distributions. In our analysis, a pronounced decrease can be seen in newly diagnosis and surgery when taking treatment distributions of each month into account. Last year, nearly 20% of patients were newly diagnosed and over 15% of patients received surgery every month. The percentage declined significantly in January and February in Hubei province. The same reductions were also seen in other provinces. There are two theories that might explain these reductions. First, individuals with potential symptoms of cancer may had little access to receive diagnosis during this period. Second, anxiety on acquiring COVID-19 infection in hospital and insufficient capacity for cancer patients treatment without infections may also hamper the implementation of diagnosis and surgery which required multidisciplinary experts participation more than preoperative and postoperative therapy did. For patients receiving preoperative or postoperative therapy, they were less affected as long as they followed their original plans. Meanwhile, endocrine therapy, target therapy or even a switch to low toxicity chemotherapy is desirable if patients can no longer continue their original regimen. However, whether the decline of diagnosis and surgery may contribute to a late stage with early relapse of breast cancer needs further follow-ups.
The primal focus of this study was to investigate delays of different cancer therapies. It has been reported that delayed therapy would compromise both local control and survival [22,23]. There is no doubt that over precautious measurements on avoiding COVID-19 infection could delay the precious time of cancer treatment [24]. However, no articles have reported the specific delays of cancer therapy during pandemic. NCP-01 study has reported the delays of breast cancer patients for the first time in different strategies. When comparing delays over different time periods, all the three indicators in Hubei or other provinces were significant except intervals from preoperative to surgery in Hubei province due to the limited data. Compared with the period free from COVID-19, the time from diagnosis to treatment was extended by 4·4 days on average in Hubei province and 2·1 days in other provinces. The striking delays were seen in intervals from surgery to postoperative therapy. It took 18·2 days for patients in Hubei to receive postoperative therapy after surgery compared with 25·2 days in other provinces. There is a common consensus that patients should receive postoperative within 3–4 weeks after surgery. However, due to existing restrictions, the average days were prolonged to 37·6 and 32·5 respectively, doubled in Hubei province. Several reasons might explain such delays. First, newly admitted patients need an approximate 7-day quarantine and nucleic acid test for COVID-19 in China. Patients with potential respiratory symptoms would be put under a longer quarantine to rule out COIVD-19 infections. Second, in some regions, cancer centres are temporarily halted due to strenuous demands on medical resources during this period. Third, formulating treatment plans based on evidence and expert experience is a severe test to all medical professionals. Multi-disciplinary cooperation amongst surgeons, internists, pathologists and radiologists are required to decide an appropriate regimen, which is also desperately needed during times like these. Last, the removal of the primary tumour could improve the outcome of breast cancer patients. A 2–4 week postpone of postoperative therapy is widely accepted to decrease the risk of infection with COVID-1914. However, those delays might have little effect on the overall survival due to long term courses of postoperative therapy. A loading dose after the epidemic could ensure the overall dose intensity of therapy. Whether those measures will reduce the risk of recurrence needs further investigation.
As the nationwide survey to investigate the impact of COVID-19 and the restrictions on early breast cancer, there were also some limitations, such as short-term follow-ups and selection bias. Several considerations should be taken into account when interpreting our findings. First, time interval like surgery to postoperative therapy can only be calculated after receiving postoperative therapy. This means a large number of cut-off data are excluded. Second, whether those delays are directly attributed to the COVID-19 pandemic needs discussion. Third, the differences in patients from other provinces are not fully evaluated. Further investigations and follow-ups will be performed to resolve the aforementioned issue and to determine the literal implications of the ongoing pandemic.
COVID-19 and the restrictions it inflicted had significantly affected early breast cancer treatment, with fewer diagnosis and surgery being performed. Significant delays were seen especially for those to receive treatment after diagnosis or surgery. Considerations should be given to balance the risk of infection and the increased risks of relapse derived from delayed therapy.
Contributors
ZJ had the idea of this study. GW and SS were principal investigators in Hubei province. ZJ and JL designed the questionnaire to collect data. HW,CG, ZL, JL, YL, JN, GS, QO, XW, XL, YC, YL, QC, PF, FY, JC, HZ, YY, JZ, FJ, JC, XK, JC, HZ, SP, GW, YL were involved in acquisition of the data. JL wrote the first draft of the article. All authors reviewed the results, interpreted the data, contributed substantially to development of the Article, and reviewed and approved the final version for submission
Data sharing
Data collected for the study were available to others with publication after approval of a proposal
Declaration of Competing Interest
We declare no conflict of interests
Acknowledgments
Acknowledgments
We thank Beijing Medical Award Foundation for financial support. We thank all patients involved in the study. We acknowledge all health-care workers involved in collecting data in this study. We also thank Prof. Jielai Xia from Air Force Medical University and Yi Wen and his fellows from Medbanks for statistics support.
Funding
Beijing Medical Award Foundation provided financial support to this trial
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.eclinm.2020.100503.
Contributor Information
Jianbin Li, Email: docli1018@sina.com.
Shengrong Sun, Email: sun137@sina.com.
Zefei Jiang, Email: jiangzefei@csco.org.cn.
Appendix. Supplementary materials
Reference
- 1.Wang C., Horby P.W., Hayden F.G., Gao G.F. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhu N., Zhang D., Wang W. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382(8):727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . 2020. Coronavirus (COVID-19) pandemic.https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed June 5) [Google Scholar]
- 4.Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of COVID-19 — studies needed. N Engl J Med. 2020;382(13):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- 5.Rubin E.J., Harrington D.P., Hogan J.W., Gatsonis C., Baden L.R., Hamel M.B. The urgency of care during the COVID-19 pandemic - learning as we go. N Engl J Med. 2020 doi: 10.1056/NEJMe2015903. published online May 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Burki T.K. Cancer care in the time of COVID-19. The Lancet Oncol. 2020;21(5):628. doi: 10.1016/S1470-2045(20)30201-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang Z., Wang J., He J. Active and effective measures for the care of patients with cancer during the covid-19 spread in China. JAMA oncol. 2020 doi: 10.1001/jamaoncol.2020.1198. published online Apr 1. [DOI] [PubMed] [Google Scholar]
- 8.Tian H., Liu Y., Li Y., Wu C., Chen B. e. An investigation of transmission control measures during the first 50 days of the COVID-19 epidemic in China. Science. 2020;368(6491):638–642. doi: 10.1126/science.abb6105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devi S. Travel restrictions hampering COVID-19 response. Lancet. 2020;395(10233):1331–1332. doi: 10.1016/S0140-6736(20)30967-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tian J., Yuan X., Xiao J. Clinical characteristics and risk factors associated with COVID-19 disease severity in patients with cancer in Wuhan, China: a multicentre, retrospective, cohort study. The Lancet Oncol. 2020 doi: 10.1016/S1470-2045(20)30309-0. published online May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The Lancet O. COVID-19: global consequences for oncology. The Lancet Oncol. 2020;21(4):467. doi: 10.1016/S1470-2045(20)30175-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Lancet O. Safeguarding cancer care in a post-COVID-19 world. The Lancet Oncol. 2020;21(5):603. doi: 10.1016/S1470-2045(20)30243-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zefei J., Jianbin L. Ten hot issues of breast cancer under the novel coronavirus pneumonia. Natl Med J China. 2020;100(10):721–723. doi: 10.3760/cma.j.cn112137-20200207-00218. [DOI] [PubMed] [Google Scholar]
- 14.Mei H., Dong X., Wang Y., Tang L., Hu Y. Managing patients with cancer during the COVID-19 pandemic: frontline experience from Wuhan. The Lancet Oncol. 2020;21(5):634–636. doi: 10.1016/S1470-2045(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen H., Guo J., Wang C. Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. Lancet. 2020;395(10226):809–815. doi: 10.1016/S0140-6736(20)30360-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang L., Zhu F., Xie L. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.03.296. published online Mar 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yang K., Sheng Y., Huang C. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. The Lancet Oncol. 2020 doi: 10.1016/S1470-2045(20)30310-7. published online May 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.CSCO BC . People’s Medical Publishing house; 2019. Guidelines of Chinese Society of Clinical Onclogy Breast Cancer. [Google Scholar]
- 19.Yu J., Ouyang W., Chua M.L.K., Xie C. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA oncol. 2020 doi: 10.1001/jamaoncol.2020.0980. published online Mar 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miyashita H., Mikami T., Chopra N. Do patients with cancer have a poorer prognosis of COVID-19? an experience in New York City. Ann Oncol. 2020 doi: 10.1016/j.annonc.2020.04.006. published online Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dinmohamed A.G., Visser O., Verhoeven R.H.A. Fewer cancer diagnoses during the COVID-19 epidemic in the Netherlands. The Lancet Oncol. 2020;21(6):750‐751. doi: 10.1016/S1470-2045(20)30265-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bleicher R.J., Ruth K., Sigurdson E.R. Preoperative delays in the US Medicare population with breast cancer. J clin oncol. 2012;30(36):4485–4492. doi: 10.1200/JCO.2012.41.7972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bleicher R.J., Ruth K., Sigurdson E.R. Time to surgery and breast cancer survival in the United States. JAMA oncol. 2016;2(3):330–339. doi: 10.1001/jamaoncol.2015.4508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nagar H., Formenti S.C. Cancer and COVID-19 - potentially deleterious effects of delaying radiotherapy. Nat Rev Clini oncol. 2020;17(6):332‐334. doi: 10.1038/s41571-020-0375-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.