Abstract
Acetaminophen, an analgesic and antipyretic available over-the-counter and used in over 600 medicines, is one of the most consumed drugs in the USA. Recent research has suggested that acetaminophen’s effects extend to the blunting of negative as well as positive affect. Because affect is a determinant of risk perception and risk taking, we tested the hypothesis that acute acetaminophen consumption (1000 mg) could influence these important judgments and decisions. In three double-blind, placebo-controlled studies, healthy young adults completed a laboratory measure of risk taking (Balloon Analog Risk Task) and in Studies 1 and 2 completed self-report measures of risk perception. Across all studies (total n = 545), acetaminophen increased risk-taking behavior. On the more affectively stimulating risk perception measure used in Study 2, acetaminophen reduced self-reported perceived risk and this reduction statistically mediated increased risk-taking behavior. These results indicate that acetaminophen can increase risk taking, which may be due to reductions in risk perceptions, particularly those that are highly affect laden.
Keywords: NSAID, decision-making, risk perception, anti-inflammatory
Acetaminophen, the active ingredient in Tylenol® and nearly 600 other medicines, is taken each week by an estimated 23% of the US adult population (Kaufman et al., 2002). Recent research has demonstrated that acetaminophen’s effects on pain and fever reduction extend to psychological processes. For example, acetaminophen reduces hurt feelings (Dewall et al., 2010), meaning threats (Randles et al., 2013), distress over another’s suffering (Mischkowski et al., 2016), loss aversion (DeWall et al., 2014) and affective reactivity to negatively valenced images (Durso et al., 2015). In this latter study, acetaminophen also blunted affective reactivity to positively valenced images, suggesting that it may reduce affective reactivity more generally, rather than solely influencing negative experiences. Because risk judgments and decisions rely on both positive and negative affect (Loewenstein et al., 2001; Slovic et al., 2004), it is reasonable to hypothesize that acetaminophen may influence them.
Affect and decision-making
Work on the ‘affect-heuristic’ and ‘risk-as-feelings’ hypothesis have demonstrated a key role for affect in risk judgments and decisions (Loewenstein et al., 2001; Slovic et al., 2004). In particular, when faced with a complex decision, people often use their feelings about an option as information, substituting it for the more difficult probabilities and outcomes that accurately describe risks. This affect then serves as a simple cue, allowing people to avoid hazards quickly and efficiently. As a result, affect manipulations, perhaps including acetaminophen, should influence decisions about risks.
Affect heuristic and risk taking
The affect heuristic predicts that individuals will use affect as information to guide decisions, especially in risky tasks that are affectively stimulating and experientially engaging (Figner and Weber, 2011). The Balloon Analog Risk Task (BART; (Lejuez et al., 2002)), for example, is such an experiential task; performance on it predicts drug and alcohol use, delinquent behavior and risky sexual behavior (e.g. (Lejuez et al., 2004,2007; Aklin et al., 2005)). The BART is a computerized task in which participants inflate balloons to earn money, but each pump risks them losing all of their prior earnings. The task is probabilistic although it does not provide explicit information about the probability of loss events. It is also visual and experiential, making it a strong candidate for a task in which participants are likely to use the affect heuristic.
Indeed, experimentally induced increases to participant’s negative affect have reduced risk taking on the BART (Yuen and Lee, 2003; Heilman et al., 2010; Parkinson et al., 2012). This research suggests that negative affect experienced during the BART signals one to engage in less risk taking. Because the BART negative loss events are more visually and auditorily salient than its win events and because manipulations of negative affect had significant influences on task performance, it seems likely that negative affect toward potential or experienced losses exerts a stronger influence on BART decisions than does positive affect toward potential or experienced gains. Therefore, acetaminophen’s blunting of negative affect may lead to a reduction in this negative affect signal and an increase in risk taking. These considerations led to our first hypothesis: Acetaminophen will increase risk taking on the BART (Hypothesis 1).
Affect heuristic and risk and benefit judgments
Affect-heuristic use also has also been explored in the context of risk and benefit judgments (Slovic and Peters, 2006). Individuals appear to rely on affect to infer the risks and benefits offered by activities and hazards. Objects that elicit positive affect, say alcoholic beverages, tend to be judged as having high benefits and low risks. Conversely, objects that elicit negative affect, say nuclear power, tend to be judged as low in benefit and high in risk. Because acetaminophen appears to reduce the extremity of affective reactions to stimuli, it may reduce perceived risk and perceived benefit of a behavior or policy. Therefore, our second hypothesis is: acetaminophen will reduce the negative affect elicited when considering potential risk, leading to reduced risk perception (Hypothesis 2A). The corollary of this hypothesis is that acetaminophen will reduce the positive affect elicited when considering potential benefits, leading to reduced benefit perception (Hypothesis 2B).
To test these hypotheses, we used an acute, double-blind, placebo-controlled, parallel-arm design with acute administration of the standard extra-strength dosage (1000 mg) of acetaminophen.
Study 1
Method
Participants.
Participants were 142 undergraduate volunteers (76 men, 64 women, 2 nonresponses) with a mean age of 19.36 years (s.d. = 1.68). Sample size was determined a priori based on the expectation of a similar effect size as that found in previous acetaminophen and affect research (Durso et al., 2015) and acetaminophen and decision-making research (DeWall et al., 2014). All research reported herein was approved by the Ohio State University Institutional Review Board.
Acetaminophen.
A double-blind, placebo-controlled design was used. Participants were randomly assigned to drug condition using a random number generator (n = 69 placebo, n = 73 acetaminophen). Participants were given a placebo or 1000 mg of acetaminophen, the recommended extra strength dosage for a headache and the dosage commonly used in studies of acetaminophen’s psychological effects (Durso et al., 2015). Acetaminophen and placebo solutions were prepared by Pharmacy Specialists Compounding Pharmacy (Altamonte Springs, Florida; http://www.makerx.com/). The drug solution consisted of acetaminophen (100 mg/ml) suspended in Ora-Plus suspension liquid and flavored with Fagron Simple Syrup. The placebo solution consisted of Avicel Microcrystalline powder (100 mg/ml) dissolved in Ora-Plus suspension liquid and flavored with Ora-Sweet Syrup. After consuming the assigned solution, participants were given a small cup of water to wash it down. At the conclusion of the experiment, participants were asked to guess which drug condition they were in (acetaminophen, placebo, or ‘no idea’); thus, participants could opt out of guessing their condition, or guess between drug and placebo conditions, a 50% chance of guessing correctly. In the acetaminophen condition, 46.6% of participants correctly guessed which condition they were in (i.e. choosing ‘acetaminophen’ and not ‘placebo’ or ‘no idea’). A one-sample t-test for proportions reveals that this was not significantly different from chance, t = −0.58, P = 0.56. In the placebo condition, 34.8% of participants correctly guessed which condition they were in (i.e. selecting ‘placebo’ and not ‘acetaminophen’ or ‘no idea’), a proportion that was significantly worse than chance, t = −2.64, P = 0.01, suggesting that participants did not accurately predict their experimental condition (the most common response in this group was ‘no idea’, 41%).
Risk taking.
To measure risk taking, the BART was used (Lejuez et al., 2002). In this task, participants complete 30 trials, each of which includes 1–128 participant responses. A trial begins with a small, uninflated balloon on a computer screen. Participants can inflate the balloon, with each pump earning $0.05. Though they played this game for imaginary money, they were told their goal was to earn as much money as possible in the task. Participants can collect their total trial earnings and move them to a permanent bank at any point by pressing a button saying ‘Collect $$$’. However, participants also are told that the balloon can burst as early as the first trial and as late as when the balloon fills the entire computer screen. Bursts are accompanied by a bursting sound and popping animation. If the balloon bursts prior to the participants pressing the ‘Collect $$$’ button, they lose any money earned thus far on that trial, and must move on to the next trial having added no money to their permanent bank.
Participants are not told about the maximum number of pumps, the likelihood of bursts, nor that, for each balloon, the first pump has a 1/128 probability of bursting, the second pump 1/127, and so on until on the 128th pump there is a 1/1 probability of bursting.
Risk and benefit perception.
To assess acetaminophen’s impact on use of the affect heuristic in risk judgments, participants completed the risk and benefit perceptions questionnaire used by Finucane et al. (2000). Participants were asked to make risk and benefit judgments of various activities and technologies for US society as a whole. They made these judgments on a 7-point scale ranging from not at all risky (beneficial) to very risky (beneficial). To enhance affect-heuristic use, participants were put under time pressure with a countdown clock on the screen while making judgments, with 5.2 s for each item (as in Finucane et al., 2000). The scale consisted of 23 items (e.g. ‘Pesticides’, ‘Nuclear Power Plants’), presented one at a time on the screen. Items were presented in randomized order. After completing ratings of all 23 items on the first scale (either risk or benefit), participants then received instructions for completing the second scale (benefit or risk), with all items presented again in a different random order. Order of the benefit and risk perception tasks was counter-balanced.
Procedure.
After signing up for the experiment, participants received an email informing them that ‘Half of the participants will receive a liquid dose of acetaminophen (i.e. Tylenol) and half of the participants will receive a liquid dose of placebo (i.e. a sugar pill or inactive liquid). Therefore, there is a 50% chance you will be in the group that receives acetaminophen’. The email informed them about the risk factors associated with acetaminophen (e.g. currently taking a drug containing acetaminophen, a history of liver disorder, an allergic reaction to acetaminophen, currently taking an anticoagulant, or a history of alcohol abuse) and asked them to refrain from participation if they met any of these risk factors. To facilitate drug absorption, we also asked participants to refrain from consuming food for three hours before the experiment. Upon arrival at the laboratory and after providing informed consent (which repeated the information in the email described above), participants consumed either the drug or placebo, based on random assignment. To allow for sufficient drug uptake into the brain (Singla et al., 2012), we waited 45 min to begin the main tasks of the study. During drug uptake, participants completed a number of background personality and health measures. At 45 min, participants began completing decision-making tasks. At approximately 50 min after the drug consumption, participants completed the risk and benefit perception task using the online survey program Qualtrics (Qualtrics, Provo, UT). Immediately following and approximately 60 min after the drug consumption, participants completed the BART task, implemented using the Psychology Experiment Building Language (PEBL) package and prepackaged BART script (Mueller and Piper, 2014; http://pebl.sourceforge.net/). Following the BART, participants answered a short survey, which included demographic information, then were debriefed and thanked.
Results
Risk-taking main effect.
To analyze the BART data, we computed participants’ adjusted average number of pumps across the 30 trials, according to methods in prior work (Lejuez et al., 2002). Specifically, trials on which a balloon burst occurred were excluded, as the number of pumps completed on this trial reflected balloon bursts rather than the participant’s desired amount of risk taking had a burst not occurred. After those trials were excluded, averages across the remaining trials were computed.
Consistent with our first hypothesis that acetaminophen would increase BART risk taking, a t-test revealed a significant difference in risk taking between those on acetaminophen and those on placebo, t(140) = −2.29, P = 0.023, 95% CI [−10.94, − 0.81], Cohen’s d = 0.38 (Figure 1A, left panel). As hypothesized, those in the placebo condition engaged in significantly less risk taking as indexed by adjusted average number of pumps (M = 33.10, s.d. = 15.75) than those on acetaminophen (M = 38.98, s.d. = 14.80). Hierarchical linear modeling techniques demonstrated similar results, but did not identify further psychological mechanisms driving these effects (see supplementary material). There was also a significant difference (t(140) = − 2.02, P = 0.045, 95% CI [−2.95, −0.033]) in the number of balloons that burst as a function of drug condition with more balloons bursting in the acetaminophen condition (M = 10.07, s.d. = 4.13) than the placebo condition (M = 8.58, s.d. = 4.64).
Fig. 1.
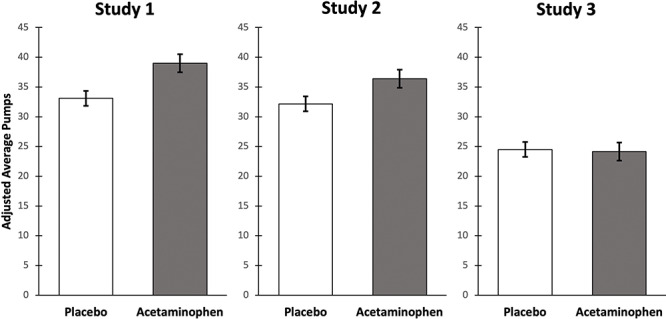
Graphs of the adjusted average number of pumps for each study (error bars denote standard error of the mean). In Studies 1, 2 and the combined analysis of all three studies, the acetaminophen group had significantly more adjusted average pumps.
Risk and benefit perception.
To assess risk perception, average ratings were computed across the 23 items. The same process was used for benefit perception. Our second hypothesis that acetaminophen would decrease risk and benefit perceptions was not supported. A t-test for average risk perception revealed no significant difference between drug conditions, t(140) = 1.48, P = 0.14, 95% CI [−0.05, 0.34]. Descriptively, those on placebo perceived more risk (M = 3.93, s.d. = 0.62) than those on acetaminophen (M = 3.78, s.d. = 0.56). A t-test for average benefit perception also revealed no significant difference between drug conditions, t(140) = 0.74, P = 0.46, 95% CI [−0.13, 0.28]. Descriptively, those on placebo perceived more benefit (M = 4.58, s.d. = 0.61) than those on acetaminophen (M = 4.50, s.d. = 0.62). We also examined acetaminophen’s impact on the correlation between risk and benefit judgments; these analyses are described in the supplementary online material.
Study 1 discussion
Study 1 provided initial support for our first hypothesis; those on acetaminophen, relative to placebo, engaged in significantly more risk taking on the BART. Little evidence emerged, however, for our second hypothesis that acetaminophen would reduce risk and benefit perceptions. We speculated that our participants perceived these items to be less affectively stimulating than those in the original Finucane et al. (2000) affect-heuristic study. Indeed, in our placebo group, negative correlations between risk and benefit perceptions were obtained (r = −0.23), but were much weaker than those in the same time-pressure condition of the original study (r = −0.80). If participants had weaker negative affect to these risks in our study, acetaminophen may not have exerted much effect on judgments because acetaminophen has weaker effects on stimuli that are less affective compared to more affective (Durso et al., 2015).
Study 2
In Study 2, we attempted a direct replication with the BART task and used a risk-perception scale with items that may be more affectively stimulating than those of Study 1 to re-test our second hypothesis.
Method
Participants.
One-hundred eighty-nine undergraduates volunteered (109 men, 79 women, 1 nonresponse) and had a mean age of 19.49 years (s.d. = 2.89). We aimed for 200 participants based on a power analysis of Study 1 (Cohen’s d = 0.38); data collection ended at the end of the semester.
Acetaminophen.
As in Study 1, we used a double-blind, placebo-controlled design with random assignment to 1000 mg of acetaminophen or placebo (n = 95 and 94, respectively). Participants were asked to guess which drug condition they were in (acetaminophen or placebo). A total of 54.7% of participants in the acetaminophen condition correctly guessed which condition they were in, a proportion that was not significantly different from chance, t = 0.92, P = 0.36. A total of 52.1% of participants in the placebo condition correctly guessed which condition they were in, a proportion that was not significantly different than chance, t = 0.41, P = 0.68.
BART.
The same behavioral measure of risk taking, the BART, was used in Study 2. Participants completed 30 trials. Following this, participants answered self-report questions about their experience and perception of balloon bursts during the task (see supplementary material for full materials and analysis).
Risk and benefit perceptions.
To examine acetaminophen’s effect on risk and benefit perceptions, we used the revised Domain Specific Risk-Taking Scale (DOSPERT; Blais and Weber, 2006). This 30-item scale provides behavioral scenarios (e.g. ‘Betting a day’s income on the outcome of a sporting event’) for which participants were then asked for their gut-level perception of the riskiness of each behavior as well as the expected benefits that would be obtained from enacting each behavior. Participants responded on a 7-point scale ranging from not at all risky (no benefits at all) to extremely risky (great benefits). Because these items are more experientially descriptive and participants are asked to judge risk and benefit personally rather than for society, we thought they would be more affectively stimulating than Study 1’s items. We found support for this hypothesis in an additional study described in the supplemental materials. In brief, the DOSPERT items were rated as significantly more emotional and negative than the Finucane items. Participants also reported feeling more worried when thinking about those items than the Finucane items.
The DOSPERT scale can be analyzed both for general risk and benefit perceptions as well as domain-specific perceptions in ethical (‘passing off somebody else’s work as your own’), financial (‘betting a day’s income at a high-stake poker game’), health (‘driving a car without a seatbelt’), recreational (‘Bungee jumping off a tall bridge B’) and social (‘moving to a city far away from your extended family’) domains. We analyzed the data for average risk/benefit overall and separately within each of the five domains.
Procedure.
Study 2’s procedure was nearly identical to Study 1 and used the same software. Participants gave informed consent, consumed drug or placebo, and waited 45 min while completing background measures. Approximately 50 min after drug administration, participants completed the DOSPERT. Following this and approximately 60 min after drug administration, participants completed the BART, followed by the self-report items concerning recalled affective experience during the BART task (see supplemental material).
Results
Risk-taking main effect.
As in Study 1, we computed participants’ adjusted average number of pumps across the 30 trials. A t-test revealed a significant difference in risk taking between those on placebo and those on acetaminophen, t(187) = − 2.14, P = 0.033, 95% CI [−8.11, −0.34], Cohen’s d = 0.31. Those on acetaminophen (M = 36.38, s.d. = 14.79) engaged in significantly more risk taking than those on placebo (M = 32.15, s.d. = 12.14) (Figure 1, middle panel), thus replicating Study 1’s effect. As in Study 1, more balloons burst in the acetaminophen condition (M = 9.54, s.d. = 4.29) than the placebo condition (M = 8.73, s.d. = 4.43). However, the difference was not statistically significant (t(187) = − 1.27, P = 0.21, 95% CI [−2.06, 0.45]).
Risk and benefit perception.
To test the second hypothesis that acetaminophen would decrease risk and benefit perceptions, we used t-tests to compare placebo and acetaminophen groups’ summed risk and summed benefit perception across all 30 DOSPERT items, as is typically done when analyzing the DOSPERT scale. A t-test revealed a significant difference in risk perception between conditions, t(187) = 2.72, P = 0.007, 95% CI [1.93, 12.19], Cohen’s d = 0.40. Those on acetaminophen (M = 133.89, s.d. = 18.03) perceived significantly less risk than those on placebo (M = 140.96, s.d. = 17.71). Thus, Hypothesis 2A was supported for risk perceptions. When analyzed separately by domain, this effect held for risk perception in the social (P = 0.005) and recreational (P = 0.025) domains was marginally significant in the financial (P = 0.069) domain and was nonsignificant but in the hypothesized direction in the health (P = 0.12) and ethical (P = 0.67) domains.
For benefit perception (Hypothesis 2B), a t-test revealed no significant difference in summed benefit perception between conditions, t(187) = 0.10, P = 0.92, 95% CI [−4.85, 5.35]; this null effect existed for each of the five domains when analyzed separately. Thus, Hypothesis 2B was not supported.
Risk-taking mediation.
The finding that acetaminophen significantly reduced perceived risk (measured with the DOSPERT) could account for the drug’s effect on BART risk taking. We explored whether acetaminophen’s effect on risk taking was mediated by the drug’s effect on DOSPERT risk perception by using PROCESS Model 4 (Hayes, 2012). This analysis revealed a significant indirect effect of acetaminophen on risk taking through risk perception (point estimate: 0.88, 95% bootstrap CI = 0.14 to 2.31); acetaminophen no longer had a direct effect on risk taking (direct effect = 3.34, P = 0.09, 95% CI = − 0.58 to 7.26). No evidence existed of an indirect effect through benefit perception (point estimate: − 0.03, 95% bootstrap CI = − 0.88 to 0.66).
Study 2 discussion
Study 2 replicated and extended Study 1’s risk-taking result: Again, acetaminophen increased risk taking, supporting our first hypothesis. Furthermore, there was also support for hypothesis 2A: acetaminophen reduced risk perceptions (but not benefit perceptions) on the DOSPERT. These effects of acetaminophen on risk perceptions in Study 2, but not Study 1, are likely due to the greater negative emotion elicited by the DOSPERT items than Finucane et al. (2000) items (see supplementary material for the aforementioned additional study demonstrating greater emotionality of the DOSPERT items).
In addition, the acetaminophen-caused reduction in risk perceptions mediated increased risk taking on the BART, suggesting that acetaminophen may reduce negative affect to options and thereby how risky they seem.
Study 3
The goal of Study 3 was to replicate and extend Study 2.
Method
Participants.
Two-hundred fifteen undergraduates volunteered (91 men, 122 women, 1 selected ‘prefer not to answer’) and had a mean age of 19.49 years (s.d. = 2.89). Like in Study 2, we aimed for 200 participants; data collection ended at the end of the semester. The sample was 69% white, 10% Asian, 8% Black or African American, and 14% Mixed race or some other origin.
Drug preparation.
As in the prior studies, we used a double-blind, placebo-controlled design with random assignment to 1000 mg of acetaminophen or placebo (n = 109 and 106, respectively). It should be noted that a different preparation procedure and vehicle were used for acetaminophen administration than in the prior studies. Drug suspension was prepared in the laboratory by adding 40g of acetaminophen powder with 0.6 g Vivasol® GF to 400 ml of Flavor Blend™ suspending vehicle from which 10 ml (1000 mg) aliquots were administered to participants. Placebo solutions were prepared in the same manner by adding 40 g of Avicel® PH-105 microcrystalline cellulose powder with 0.6 g Vivasol® GF to 400 ml of Flavor Blend™ suspending vehicle. All products were prepared and provided by Pharmacy Specialists Compounding Pharmacy (Altamonte Springs, Florida; http://www.makerx.com/).
Procedure.
The procedure was similar to prior studies. After consenting and consuming drug or placebo, participants completed background questionnaires. At least 45 min later, participants completed two tasks (Columbia Card Task (Figner et al., 2009) and the Iowa Gambling task (Bechara et al., 1994); these data have not been analyzed and will be reported separately) followed by the BART. A different software platform (Inquisit, www.millisecond.com) was used to implement the BART. An additional change in procedure was that after the first 15 balloons, participants completed the same self-report items as in Study 2, which were repeated after the final 15 balloons. Participants did not complete any self-reported risk perception items in this study.
Results and discussion
Unlike the prior studies, participants in the acetaminophen condition were better at guessing their condition; 61.2% correctly guessed their condition, a proportion significantly better than chance, t = 2.45, P = 0.02.
As measured by the average number of pumps on nonbursting trials, we did not find a significant difference in risk taking on the BART between the acetaminophen (M = 24.13, s.d. = 12.56) and placebo condition (M = 24.49, s.d. = 13.30), t(213) = 0.20, P = 0.84, 95% CI [−3.11, 3.83] in this study (Figure 1, right panel). Although we thought it plausible that guessed drug condition might have predicted performance, according to an ANOVA, no main effect existed of guessed drug condition (F(l,210) = 1.59, P = 0.21) nor was there an interaction effect of guessed drug condition (F(1,210) = 0.32, P = 0.57) with actual drug condition (one subject did not guess condition). There was a greater number of balloon bursts in the acetaminophen (M = 6.56, s.d. = 3.60) than the placebo condition (M = 6.17, s.d. = 3.47); however, the difference was not significant (t(213) = − .81, P = 0.42, 95% CI [−1.34, 0.56]).
It should be noted that the average number of pumps in this study (across both conditions), which used the Inquisit software (M = 24.31, s.d. = 12.90) was significantly less (F(2,543) = 39.88, P < 0.0001) than that from the prior two studies that used the PEBL software (Study 1, M = 36.12 s.d. = 15.50; Study 2 M = 34.28, s.d. = 13.66). Similarly, the number of bursts in this study (M = 6.37, s.d. = 3.53) was significantly lower (F(2,543) = 2185.73, P < 0.001) than those in the prior two studies (Study 1: M = 9.35, s.d. = 4.34; Study 2: M = 9.14, s.d. = 4.37). Consistent with these differences, significant differences existed in earnings (F(2,545) = 31.5, P < 0.001), with lower earnings in Study 3 (Study 1: M = $34.27, s.d. = 10.14 Study 2: M = $34.02, s.d. = 10.37; Study 3: M = $26.53, s.d. = 11.95).
Combined analysis of studies 1, 2 and 3
As compilation of results across studies can lead to improved interpretation of effects (Braver et al., 2014; Fabrigar and Wegener, 2016), we combined data from all three studies. In this compilation, there was a significant main effect of acetaminophen on BART risk taking (t(544) = − 2.26, P = 0.024, 95% CI [−5.35, −0.38], Cohen’s d = 0.19) with a greater average number of pumps on nonbursting balloons in the acetaminophen condition (M = 32.24, s.d. = 15.40) than the placebo condition (M = 29.37, s.d. = 14.11). Consistent with the acetaminophen group engaging in greater risk taking, there was a greater number of balloon bursts (t(544) = − 2.237, P = 0.026, 95% CI [−1.543, −0.100]) in the acetaminophen condition (M = 8.51, s.d. = 4.28) than the placebo condition (M = 7.68, s.d. = 4.30). This provides strong evidence that acetaminophen increases risk-taking on the BART.
General discussion
Across three separate studies, acetaminophen increased risk taking on the BART. In Study 2, acetaminophen also reduced perceived risk on the DOSPERT, and this experimentally induced reduction in perceived risk accounted for increased risk taking on the BART, suggesting acetaminophen may reduce negative affect and risk perception in turn and, thereby, increase risk taking.
Acetaminophen did not reduce risk perceptions using the Finucane items (Study 1) in contrast to the effects seen with the DOSPERT risk perception items (Study 2). Motivated by prior work showing that acetaminophen has greater effects on affective stimuli rated to be more extreme in negative or positive valence than less extreme stimuli (Durso et al., 2015), our additional online study (see supplementary material) provided evidence that Study 2’s items were more affectively stimulating (e.g. they were rated more emotional and negative) than Study 1’s items These findings provide initial evidence that acetaminophen can influence risk judgments, especially for more affectively stimulating stimuli.
Interestingly, although acetaminophen significantly reduced perceived risk in Study 2, it did not reduce perceived benefit. One potential explanation for the lack of effect on benefit items is that their phrasing may have elicited more cognitive evaluation, whereas the risk questions may have been more affectively stimulating. The risk questionnaire asked participants to rate ‘your gut level assessment of how risky each situation or behavior is’ whereas the benefit scale asks for ‘the benefits you would obtain from each situation’. An emphasis on gut level risk assessment may increase reliance on the affect heuristic. This difference may account for Study 2’s acetaminophen-caused reduced risk perceptions and its lack of effect on perceived benefits.
Although not all studies were independently significant, when treated in aggregate, a significant relation emerged between taking acetaminophen and choosing more risk. Multiple studies with effects in the same direction, even if not significant, reduce the probability that the population effect is zero (Braver et al., 2014; Fabrigar and Wegener, 2016), suggesting that this is a reliable effect. Potential factors contributing to the lack of an effect in Study 3 could be the different drug formulation that led to greater awareness of drug condition as well as the differences in software used to implement the BART. Each inflation of the balloon using the software in Study 3 was larger, leading to fewer pumps being necessary to fill the screen and thus less overall pumps and bursts. Such reduced range may have impaired the ability to detect a drug effect.
Another consideration is whether or not playing the BART with actual money would have changed the results. Although some controversy exists about the differential role of hypothetical relative to monetary reinforcers on decision-making tasks (Johnson and Bickel, 2002; Madden et al., 2003; Hinvest and Anderson, 2010), it appears that when real monetary reinforcers have differential effects they tend to amplify the differences between conditions (Bowman and Turnbull, 2003). For example, large monetary losses in a modified form of the BART led to greater neural reactivity and reductions in risk behavior than hypothetical losses (Xu et al., 2018). Thus, employing a BART with real money could potentially enhance the effects of acetaminophen.
Future directions
In addition to decreases in risk perception, other psychological processes are likely involved in acetaminophen’s effects on risk taking. One possible unexplored mechanism is anticipatory experienced anxiety. It may be that as the balloon increases in size, those on placebo feel increasing amounts of anxiety about a potential burst. When the anxiety becomes too much, they end the trial. Acetaminophen may reduce this anxiety, thus leading to greater risk taking. As indicated in the supplement, self-reported affective experiences to the BART did not differ between conditions, but these recalled emotions may not reflect affective responses experienced in the moment.
Additionally, there are many potentially interesting ways in which we might examine the impact of risk taking on tasks that involve stronger positive affect. It may be the case that risk-taking tasks that focus on the positive affect associated with gains may actually show reverse effects of acetaminophen due to acetaminophen’s affect-blunting effects. For instance, if we manipulated the BART to make gain events more salient (adding sounds and visuals) or more intense (larger payoffs), acetaminophen may decrease risk taking.
Alternatively, acetaminophen’s effects on risk taking may be driven less by affective influences on judgment than by effects on another psychological process such as learning during the task (Pearson et al., 2018) or error monitoring. Event-related potentials (ERPs) recorded during a Go/No-Go task, for example, showed that acetaminophen reduced the error positivity (Pe), which partially mediated acetaminophen-induced increases in omission errors (Randles et al., 2016). The Pe is a signal that appears to be associated with the emergence of conscious awareness of committing an error (Nieuwenhuis et al., 2001; Murphy et al., 2012) and highly correlated with activity in the anterior insula (Ullsperger et al., 2010). Of note, the association of greater anterior insula activation with anticipated risk is one of the most reliable findings in the neural decision-making literature (Knutson and Huettel, 2015). Because acetaminophen blunts activity in the anterior insula (Dewall et al., 2010) as well as the Pe, it may be influencing risk-related processing particularly at a conscious level. Dissecting such influences on the BART could provide insight into additional psychological mechanisms accounting for the drug-induced increase in risk taking.
Another question for future research will be identifying the biological mechanisms responsible for these effects of acetaminophen. Like more conventional nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and aspirin, acetaminophen inhibits the production of prostaglandins in the brain (Flower and Vane, 1972). The administration of such drugs might provide insight into whether the prostaglandins are involved in risk judgments as well as which enzymes producing prostaglandins (cyclooxygenase 1 and cyclooxygenase 2) are greater contributors to the effect. Alternatively, acetaminophen may exert its effects on risk taking through a different biological pathway than the prostaglandins, potentially through the vanilloid, cannabinoid or serotoninergic systems (Graham et al., 2013).
Potential implications
With nearly 25% of the population consuming acetaminophen each week (Kaufman et al., 2002), reduced risk perceptions and increased risk taking could have important societal effects. Many areas of daily life require making decisions that involve the processes examined here. For example, many patients in the hospital have acetaminophen in their systems when presented with risk information and asked to make potentially life-changing risk assessments such as whether or not to do an invasive surgery. Similarly, when driving, one is regularly presented with decisions that involve risk perception and assessment. Thus, it is imperative that we understand acetaminophen’s effects on choices made and risks taken. Risk perception and risk taking are judgments and decisions that can affect many aspects of our lives, and this common, over-the-counter drug may influence this process, unbeknownst to the millions taking the drug.
Supplementary Material
Acknowledgements
We would like to acknowledge the helpful assistance of Liv Bobb, Amanda Brown, Brittany Boltz, Michael Butrey, Japera Benson, Nicole Hadjisofocli, Catie Johnson, Elianna Miller, Cori O’Boyle, Maggie Walsh and Zachary Weisenseel.
Contributor Information
Alexis Keaveney, Department of Psychology, The Ohio State University, Columbus, OH 43210, USA.
Ellen Peters, School of Journalism and Communication, University of Oregon Eugene, OR 97403, USA.
Baldwin Way, Department of Psychology, The Ohio State University, Columbus, OH 43210, USA.
Supplementary data
Supplementary data are available at SCAN online.
Open practices
The consent form completed by participants in these studies stated, ‘Only the investigators and their research assistants will have access to the original research data’. As a consequence, we cannot share the original data publicly at this time. However, for anyone interested in accessing the data for verifying our analyses, please contact the authors. Study 1 (https://osf.io/p2e5c/) and the online study reported in the supplemental material (https://osf.io/496rc/) were preregistered with the Open Science Framework.
Funding
This research was generously supported by funds from the Ohio State University as well as the National Science Foundation (Award #1558230; Peters (PI), Way (Co-I)). The funders had no influence on the design, collection, analysis and interpretation of the data, writing of the report and decision to submit this article for publication.
Conflict of interest
The authors do not have any conflicts of interest.
References
- Aklin, W.M., Lejuez, C.W., Zvolensky, M.J., et al. (2005). Evaluation of behavioral measures of risk taking propensity with inner city adolescents. Behaviour Research and Therapy, 43, 215–28. [DOI] [PubMed] [Google Scholar]
- Bechara, A., Damasio, A.R., Damasio, H., et al. (1994). Insensitivity to future consequences following damage to human prefrontal cortex. Cognition, 50, 7–15. [DOI] [PubMed] [Google Scholar]
- Blais, A.-R., Weber, E.U. (2006). A domain-specific risk-taking (DOSPERT) scale for adult populations. Judgment and Decision Making, 1, 33–47. [Google Scholar]
- Bowman, C.H., Turnbull, O.H. (2003). Real versus facsimile reinforcers on the Iowa Gambling Task. Brain and Cognition, 53, 207–10. [DOI] [PubMed] [Google Scholar]
- Braver, S.L., Thoemmes, F.J., Rosenthal, R. (2014). Continuously cumulating meta-analysis and replicability. Perspectives on Psychological Science, 9, 333–42. [DOI] [PubMed] [Google Scholar]
- DeWall, C.N., Chester, D.S., White, D.S. (2014). Can acetaminophen reduce the pain of decision-making? Journal of Experimental Social Psychology. 56, 117–120. [Google Scholar]
- Dewall, C.N., Macdonald, G., Webster, G.D., et al. (2010). Acetaminophen reduces social pain: behavioral and neural evidence. Psychological Science, 21, 931–7. [DOI] [PubMed] [Google Scholar]
- Durso, G.R.O., Luttrell, A., Way, B.M. (2015). Over-the-counter relief from pains and pleasures alike: acetaminophen blunts evaluation sensitivity to both negative and positive stimuli. Psychological Science, 26, 750–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabrigar, L.R., Wegener, D.T. (2016). Conceptualizing and evaluating the replication of research results. Journal of Experimental Social Psychology, 66, 68–80. [Google Scholar]
- Figner, B., Mackinlay, R.J., Wilkening, F., et al. (2009). Affective and deliberative processes in risky choice: age differences in risk taking in the Columbia Card Task. Journal of Experimental Psychology. Learning, Memory, and Cognition, 35, 709. [DOI] [PubMed] [Google Scholar]
- Figner, B., Weber, E.U. (2011). Who takes risks when and why? Determinants of risk taking. Current Directions in Psychological Science, 20, 211–6. [Google Scholar]
- Finucane, M.L., Alhakami, A., Slovic, P., et al. (2000). The affect heuristic in judgments of risks and benefits. Journal of Behavioral Decision Making, 13, 1–17. [Google Scholar]
- Flower, R.J., Vane, J.R. (1972). Inhibition of prostaglandin synthetase in brain explains the anti-pyretic activity of paracetamol (4-acetamidophenol). Nature, 240, 410–1. [DOI] [PubMed] [Google Scholar]
- Graham, G.G., Davies, M.J., Day, R.O., et al. (2013). The modern pharmacology of paracetamol: therapeutic actions, mechanism of action, metabolism, toxicity and recent pharmacological findings. Inflammopharmacology, 21, 201–32. [DOI] [PubMed] [Google Scholar]
- Hayes, A.F. (2012). PROCESS: A Versatile Computational Tool for Observed Variable Mediation, Moderation, and Conditional Process Modeling. KS: University of Kansas. [Google Scholar]
- Heilman, R.M., Crişan, L.G., Houser, D., et al. (2010). Emotion regulation and decision making under risk and uncertainty. Emotion, 10, 257. [DOI] [PubMed] [Google Scholar]
- Hinvest, N.S., Anderson, I.M. (2010). The effects of real versus hypothetical reward on delay and probability discounting. The Quarterly Journal of Experimental Psychology, 63, 1072–84. [DOI] [PubMed] [Google Scholar]
- Johnson, M.W., Bickel, W.K. (2002). Within-subject comparison of real and hypothetical money rewards in delay discounting. Journal of the Experimental Analysis of Behavior, 77, 129–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaufman, D.W., Kelly, J.P., Rosenberg, L., et al. (2002). Recent patterns of medication use in the ambulatory adult population of the United States. JAMA: The Journal of the American Medical Association, 287, 337–44. [DOI] [PubMed] [Google Scholar]
- Knutson, B., Huettel, S.A. (2015). The risk matrix. Current Opinion in Behavioral Sciences, 5, 141–6. [Google Scholar]
- Lejuez, C.W., Aklin, W., Daughters, S., et al. (2007). Reliability and validity of the youth version of the balloon analogue risk task (BART–Y) in the assessment of risk-taking behavior among inner-city adolescents. Journal of Clinical Child and Adolescent Psychology, 36, 106–11. [DOI] [PubMed] [Google Scholar]
- Lejuez, C.W., Read, J.P., Kahler, C.W., et al. (2002). Evaluation of a behavioral measure of risk taking: the Balloon Analogue Risk Task (BART). Journal of Experimental Psychology Applied, 8, 75–84. [DOI] [PubMed] [Google Scholar]
- Lejuez, C.W., Simmons, B.L., Aklin, W.M., et al. (2004). Risk-taking propensity and risky sexual behavior of individuals in residential substance use treatment. Addictive Behaviors, 29, 1643–7. [DOI] [PubMed] [Google Scholar]
- Loewenstein, G.F., Weber, E.U., Hsee, C.K., et al. (2001). Risk as feelings. Psychological Bulletin, 127, 267–86. [DOI] [PubMed] [Google Scholar]
- Madden, G.J., Begotka, A.M., Raiff, B.R., et al. (2003). Delay discounting of real and hypothetical rewards. Experimental and Clinical Psychopharmacology, 11, 139–45. [DOI] [PubMed] [Google Scholar]
- Mischkowski, D., Crocker, J., Way, B.M. (2016). From painkiller to empathy killer: acetaminophen (paracetamol) reduces empathy for pain. Social Cognitive and Affective Neuroscience, 11, 1345–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mueller, S.T., Piper, B.J. (2014). The psychology experiment building language (PEBL) and PEBL test battery. Journal of Neuroscience Methods, 222, 250–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy, P.R., Robertson, I.H., Allen, D., et al. (2012). An electrophysiological signal that precisely tracks the emergence of error awareness. Frontiers in Human Neuroscience, 6, 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieuwenhuis, S., Ridderinkhof, K.R., Blom, J., et al. (2001). Error-related brain potentials are differentially related to awareness of response errors: evidence from an antisaccade task. Psychophysiology, 38, 752–60. [PubMed] [Google Scholar]
- Parkinson, B., Phiri, N., Simons, G. (2012). Bursting with anxiety: adult social referencing in an interpersonal Balloon Analogue Risk Task (BART). Emotion, 12, 817. [DOI] [PubMed] [Google Scholar]
- Pearson, R., Koslov, S., Hamilton, B., et al. (2018). Acetaminophen enhances the reflective learning process. Social Cognitive and Affective Neuroscience, 13, 1029–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randles, D., Heine, S.J., Santos, N. (2013). The common pain of surrealism and death: acetaminophen reduces compensatory affirmation following meaning threats. Psychological Science, 24, 966–73. [DOI] [PubMed] [Google Scholar]
- Randles, D., Kam, J.W., Heine, S.J., et al. (2016). Acetaminophen attenuates error evaluation in cortex. Social Cognitive and Affective Neuroscience, 11, 899–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singla, N.K., Parulan, C., Samson, R., et al. (2012). Plasma and cerebrospinal fluid pharmacokinetic parameters after single-dose administration of intravenous, oral, or rectal acetaminophen. Pain Practice, 12, 523–32. [DOI] [PubMed] [Google Scholar]
- Slovic, P., Finucane, M.L., Peters, E., et al. (2004). Risk as analysis and risk as feelings: some thoughts about affect, reason, risk, and rationality. Risk Analysis: An International Journal, 24, 311–22. [DOI] [PubMed] [Google Scholar]
- Slovic, P., Peters, E. (2006). Risk perception and affect. Current Directions in Psychological Science, 15, 322–5. [Google Scholar]
- Ullsperger, M., Harsay, H.A., Wessel, J.R., et al. (2010). Conscious perception of errors and its relation to the anterior insula. Brain Structure & Function, 214, 629–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu, S., Pan, Y., Qu, Z., et al. (2018). Differential effects of real versus hypothetical monetary reward magnitude on risk-taking behavior and brain activity. Scientific Reports, 8, 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen, K.S., Lee, T.M. (2003). Could mood state affect risk-taking decisions? Journal of Affective Disorders, 75, 11–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


