Abstract
Dyke–Davidoff–Masson syndrome (DDMS) (also referred to as cerebral hemiatrophy) is a rare condition characterized by seizures, facial asymmetry, contralateral spastic hemiplegia, or hemiparesis, with or without learning difficulties. It usually presents in the early childhood or late adolescence. The diagnosis is mainly associated with the presence of radiologic findings which include contralateral cerebral hemiatrophy with ipsilateral dilatation of the lateral ventricle and hypertrophy of the sinuses. Here, we report a case of a 49-year-old female patient who presented with chronic headache episodes for 10 years, and radiological findings revealed the DDMS.
Keywords: Cerebral hemiatrophy, Dyke–Davidoff–Masson syndrome, radiology, seizures, severe headache, United Arab Emirates
Introduction
Dyke–Davidoff–Masson syndrome (DDMS) is a rare disease and was first described by C.G. Dyke, L.M. Davidoff, and C.B. Masson in 1933.[1] The clinical characteristics of DDMS include cerebral hemiatrophy, facial asymmetry, contralateral hemiplegia or hemiparesis, seizures, speech and language disorders, mental retardation, and occasionally, behavioral changes and psychiatric manifestations.[2,3] It is caused by cerebral insult at any stage of the growing brain or trauma to the developing brain, resulting in a loss of neurons that compromise the growth and development of the brain, leading to facial asymmetry, contralateral hemiplegia or hemiparesis, seizures, speech and language disorders, and mental retardation. Here, we report a case of a 49-year-old female patient who presented with chronic headache episodes for 10 years, and radiological findings revealed the DDMS.
Case Report
This patient had an uneventful course during the perinatal period but sustained a traumatic head injury during the early childhood (the patient did not recall at which age) without a focal neurological residual deficit and had normal development as a child. At the age of 39 years, the patient started to have severe headache episodes, with frequent emergency department (ED) visits as a patient with classic migraine. On examination, there were no focal neurological deficits and normal bilateral deep tendon reflexes, and the patient had normal gait and speech. She did not report having abnormal involuntary movements. She has been followed in the neurology clinic regularly every 6 months without any improvement and continued to visit the ED. In 2014, the patient had ≥100 ED visits, 20 short admissions for pain control, and ≥10 head computed tomography (CT) scans, although she was on paracetamol–codeine and sometimes lorazepam. In 2018, she had approximately 150 ED visits, two short admissions for pain control, and two head CT scans. Moreover, in June 2018, she developed an episode of pseudoseizure which was attributed to an anger episode.
A review of her last head CT in August 2018 showed a hemiatrophy of the left cerebral hemisphere with volume loss and ex-vacuo dilatation of the body, frontal horn, temporal horn, and occipital horn of the left lateral ventricle [Figure 1a]. The cerebrospinal fluid spaces were also widened on the left side. There was also relative atrophy of the left cerebral peduncle. In addition, calvarial thickening on the left side, hyperaeration of the left frontal sinus, ethmoid air cells and the left sphenoid sinus, and a shallow anterior cranial fossa and left middle cranial fossa were observed [Figure 1b]. No mass effect or midline shift was noted. It is worth mentioning that these head changes were the same in her previous head CT scans in 2011 and 2014. She also had a few brain magnetic resonance imaging (MRI) scans that showed the left cerebral hemiatrophy with ipsilateral ventriculomegaly in T2-weighted and fluid-attenuated inversion recovery images [Figure 2a and b]. The patient had an electroencephalography evaluation in 2015, which revealed a mild amount of potentially epileptiform discharges that were seen over the right hemisphere. These waveforms may predispose the patient to develop epilepsy and may suggest structural lesions in that area.
Figure 1.
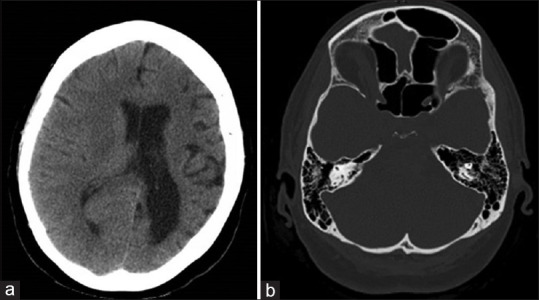
(a) Head computed tomography scan 2018 showing hemiatrophy of the left cerebral hemisphere with volume loss, ex-vacuo dilatation of the body, frontal horn, temporal horn, and occipital horn of the left lateral ventricle. (b) Head computed tomography showing sinus hyperaeration
Figure 2.
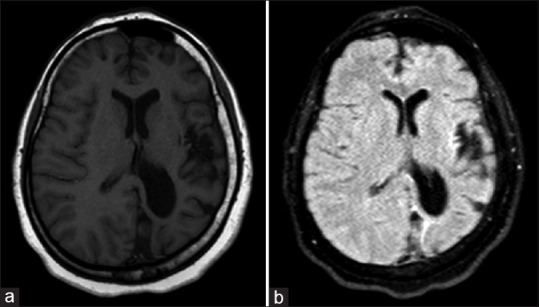
(a) Brain magnetic resonance imaging (T2 weighted) and (b) Brain magnetic resonance imaging (fluid-attenuated inversion recovery) showing the left cerebral hemiatrophy with ipsilateral ventriculomegaly
During follow-up, she reported that for the past 6 months, her condition deteriorated in the form of a recurrent headache occurring more than usual, as often as every 2 days. She underwent Botox injection in the forehead as part of the chronic headache treatment. She noticed after the injection that she was getting stiffness of the jaw, left arm, and leg together with the headache bout. Currently, she was responsive to diphenhydramine intravenous (IV) and paracetamol IV. She will be followed up in rehabilitation and neurology clinics. Written informed consent was obtained from the patient.
Discussion
In 1933, C.G. Dyke, L.M. Davidoff, and C.B. Masson reported a series of nine patients with DDMS and showed the following radiological findings: contralateral cerebral atrophy in the form of widening of the sulci and dilatation of the ipsilateral lateral ventricle, thickening of the adjacent calvarium, and hypertrophy of the frontal and ethmoid sinuses.[4] Most of these findings are seen in the authors' case. All these findings are best seen on CT or MRI, which considered the modality of choice for diagnosing DDMS.
The interesting finding, in this case, was the delay in presentation until a late age, with ≥100 ED visits with a severe headache and no permanent neurological sequelae. To the best of our knowledge, this is the first case of DDMS identified in a late adult-aged woman. In most cases, DDMS has been identified at a young age.[1,2,3,5] Therefore, it is possible that DDMS can occur even at a late adult age. In the present case, the patient has experienced only one episode of seizure, although seizures have been frequently reported in other cases.[6,7,8] The differential diagnoses are Sturge–Weber syndrome, basal ganglia germinoma, Fishman syndrome, Silver–Russell syndrome, linear nevus syndrome, and Rasmussen's encephalitis, which have unique clinical and radiological features.[9,10]
The treatment is usually symptomatic, in addition to domiciliary physiotherapy and occupational and speech therapy which have crucial roles.[11] In our case, she is receiving diphenhydramine 50 mg IV, paracetamol 1 g IV, paracetamol–codeine (500 mg/0 mg) 2 tablets q 8 h, and sometimes, lorazepam 1 mg orally.
Conclusion
This study reports a confirmed case of DDMS in the late adult age without permanent neurological sequelae. Therefore, the diagnosis of DDMS can be considered in patients who present with persistent chronic headaches in the late adult age.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Dyke C. Cerebral hemiatrophy with homolateral hypertrophy of the skull and sinuses. J Nerv Mental Dis. 1934;79:703. [Google Scholar]
- 2.Kumar S, Lakshmaiah V, Naidu KC. A rare cause for seizures and mental retardation– Dyke Davidoff Masson Syndrome. Int J Biolog Med Res. 2011;2:1186–8. [Google Scholar]
- 3.Jain D, Aggarwal HK, Goyal S, Mittal A. Dyke-Davidoff-Masson syndrome: A rare case report. Iran J Neurol. 2014;13:255–6. [PMC free article] [PubMed] [Google Scholar]
- 4.Ratnaparkhi C, Mitra K, Onkar P. Dyke-Davidoff-Masson syndrome: Cerebral hemiatrophy-five cases with review of literature. Southeast Asian J Case Rep Rev. 2015;4:1834–43. [Google Scholar]
- 5.Rashid AM, Noh MS. Dyke-Davidoff-Masson syndrome: A case report. BMC Neurol. 2018;18:76. doi: 10.1186/s12883-018-1079-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chetty S. A case report on a Dyke Davidoff Masson syndrome with right hemisphere involvement: Peer reviewed case report. South Afr Radiograh. 2016;54:12–4. [Google Scholar]
- 7.Kumar MD, Pinto DS. Adult presentation of Dyke Davidoff Masson syndrome with schizoaffective disorder – A case report. Kerala J Psych. 2017;30:84–7. [Google Scholar]
- 8.Diestro JD, Dorotan MK, Camacho AC, Perez-Gosiengfiao KT, Cabral-Lim LI. Clinical spectrum of Dyke-Davidoff-Masson syndrome in the adult: An atypical presentation and review of literature. BMJ Case Rep. 2018;2018:bcr. doi: 10.1136/bcr-2018-224170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Narra R, Kamaraju SK, Pasupaleti B, Jukuri NR. Dyke-Davidoff-Masson syndrome: A case report of cerebral hemiatrophy with crossed cerebellar diaschisis. Afr J Med Health Sci. 2015;14:150–2. [Google Scholar]
- 10.Thakkar PA, Dave RH. Dyke-Davidoff-Masson syndrome: A rare cause of cerebral hemiatrophy in children. J Pediatr Neurosci. 2016;11:252–4. doi: 10.4103/1817-1745.193365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arora R, Rani JY. Dyke-Davidoff-Masson syndrome: Imaging features with illustration of two cases. Quant Imaging Med Surg. 2015;5:469–71. doi: 10.3978/j.issn.2223-4292.2014.11.17. [DOI] [PMC free article] [PubMed] [Google Scholar]


