Abstract
Background:
Whether surgical or nonsurgical management is more appropriate for primary patellar dislocations (PPDs) in adolescents (younger than 18 years) remains controversial.
Purpose:
To compare the clinical outcomes of surgical versus nonsurgical treatment for adolescents and children with PPDs.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
There were 2 reviewers who independently searched the PubMed, Embase, Ovid, and Cochrane databases for English-language studies of randomized controlled trials (RCTs), quasi-RCTs, and observational studies comparing surgical with nonsurgical treatment for PPDs. The primary outcomes were redislocations, the Kujala score, and the Knee injury and Osteoarthritis Outcome Score (KOOS), and the secondary outcome was subsequent surgery.
Results:
A total of 6 studies were included in our systematic review and meta-analysis. Among patients younger than 18 years, surgery was associated with a lower redislocation rate compared with nonsurgical treatment within 5 years of treatment (risk ratio [RR], 0.58 [95% CI, 0.37-0.91]; P = .02; I 2 = 47%) but not beyond 5 years (RR, 0.80 [95% CI, 0.59-1.07]; P = .14; I 2 = 34%). However, surgery resulted in worse Kujala and KOOS scores compared with nonsurgical treatment. Yet, the treatment difference between the 2 groups tended to decrease over time.
Conclusion:
The available evidence suggests that for adolescents with PPDs, surgery was superior to nonsurgical treatment in the short term to reduce the redislocation rate but resulted in poorer outcomes of knee function based on the Kujala and KOOS scores. However, the superiority of either surgical or nonsurgical treatment in adolescents did not appear to persist in the long term.
Keywords: primary patellar dislocation, adolescents, surgery, nonsurgical treatment
A primary patellar dislocation (PPD) occurs when an undamaged patella is displaced from the natural trochlear groove outward toward the lateral side.6 Its incidence ranges from 5.8 to 77.8 per 100,000, and it is particularly prevalent among young people.8,24 Without effective treatment, PPDs can lead to subsequent redislocations, painful instability, and patellofemoral degeneration.18,20,28
Nonsurgical treatment has been regarded as the first-line option for PPDs, except in patients with osteochondral fractures or other severe joint disorders in the knee.5 However, such treatment is associated with a high redislocation rate and residual symptoms of instability in up to 44% of patients.5,17 Therefore, attention has shifted toward surgical treatment for addressing patellar instability.3,4,25 Several systematic reviews and meta-analyses focusing on the overall population have concluded that surgery yields fewer redislocations and better knee function than nonsurgical treatment among all patients at short-term follow-up but that outcomes are similar in the long term.27,29,34
However, how surgery compares with nonsurgical treatment in adolescents or children remains a controversy. Only 2 systematic reviews,7,22 with conflicting conclusions, have investigated this topic in adolescents or children. One concluded that surgery is associated with fewer redislocations and better knee function than nonsurgical treatment,22 while the other revealed similar findings regarding redislocations and knee function between the 2 treatment methods.7 Unfortunately, neither review included the 2018 high-quality randomized controlled trial (RCT) by Askenberger et al2 indicating that surgery may not lead to better outcomes than nonsurgical treatment in adolescents.
The current study aimed to compare outcomes after surgical versus nonsurgical treatment for the management of PPDs in adolescents and children through a systematic review and meta-analysis of available comparative studies. The primary outcome measures were redislocation rate and results on the 2 most frequently reported indicators for knee function, the Kujala score and the Knee injury and Osteoarthritis Outcome Score (KOOS), in both the short (within 5 years of treatment) and long term (beyond 5 years). The secondary outcome measure was rate of reoperations. We hypothesized that surgical treatment may not provide better results in preventing redislocations and improving functional outcomes in adolescents and children.
Methods
Search Strategy
The PubMed, Embase, Ovid, and Cochrane databases were searched using the following terms: (“patella* dislocation”) AND (primary OR acute OR first-time OR traumatic) AND (operat* OR surg*) AND (conservative OR non-operat* OR non-surg*) AND (adolescent* OR child* OR juvenile OR skeletally immature). Studies were first excluded on the basis of their titles and abstracts if they seemed clearly irrelevant. Remaining studies were read in full to determine whether they should be included. Reference lists from eligible studies, conference papers, and dissertations were also screened.
Selection Criteria
Studies were included in our review and meta-analysis if they were RCTs, quasi-RCTs, or other studies that compared surgical to nonsurgical treatment in skeletally immature patients with PPDs and that reported at least 1 of the primary outcomes (patellar redislocation, Kujala score, KOOS score) or the secondary outcome (subsequent surgery). The Kujala and KOOS scores are both calculated according to a 100-point system, with a higher score reflecting better knee function.
Studies were excluded if they were case reports, reviews, editorial letters, or expert opinions. Studies were also excluded if they involved patients older than 18 years or with recurrent patellar dislocations, previous severe knee injuries or surgical procedures, PPDs with concomitant injuries in the ligament and/or meniscus needing treatment, PPDs involving only osteochondral fractures treated with fixation, open injuries or surgical procedures, or patellar fractures.
In the included studies, PPDs were diagnosed on the basis of the appearance of an acute locked dislocation; typical clinical manifestations and signs, such as knee pain, hemarthrosis, palpation of the femoral epicondyle or medial peripatellar structures, and positive apprehension sign; imaging findings of effusion in the patellofemoral joint, medial retinacular injury, osteochondral lesions, and/or loose bodies; examination results of an easily displaced patella under anesthesia; and/or a medial retinacular injury under arthroscopic surgery.
Surgical techniques used in the included studies were arthroscopic and open medial patellofemoral ligament reconstruction or repair, lateral retinacular release, and distal realignment. Nonsurgical treatment included patient education, immobilization with bracing, splinting or taping techniques, manual or physical therapy, and exercise-based rehabilitation.
Data Extraction
Two reviewers (K.Z., H.J.) independently extracted and analyzed the following data from included studies into an Excel (Microsoft) database: first author, journal title, publication year, number of participants, mean age of participants, type of surgical and nonsurgical intervention, duration of posttreatment follow-up, and outcomes. A third reviewer (J.L.) resolved any disagreements regarding data extraction. If a study did not report means and standard deviations, we contacted the authors or estimated values according to the reported median, range, and sample size.10
Quality Assessment
The Cochrane Collaboration’s risk-of-bias tool for randomized trials9 and the Newcastle-Ottawa scale31 for non-RCTs and observational studies were used to assess the methodological quality of the included studies. The overall quality of evidence for each outcome was graded as high, moderate, low, or very low according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) guidelines.26 Again, the 2 reviewers independently performed the quality assessment.
Statistical Analysis
The meta-analysis was performed using Review Manager software (version 5.3; Cochrane Collaboration). Pooled results for dichotomous variables were expressed in terms of the risk ratio (RR) and 95% CI, while pooled results for continuous variables were expressed as the mean difference (MD) and 95% CI.
Heterogeneity was assessed in terms of I 2 and P values. According to the Cochrane Handbook,9 heterogeneity was deemed to be unimportant if the I 2 value was <50% and the P value was >.1 and considerable if the I 2 value was >50% and the P value was <.1. We used a fixed-effects model for the meta-analysis of data showing unimportant heterogeneity and a random-effects model for data showing considerable heterogeneity.
Meta-analyses were performed for all outcomes regardless of follow-up length or for outcomes measured within 5 years of treatment (short term) or beyond 5 years (long term).
Results
Included Studies
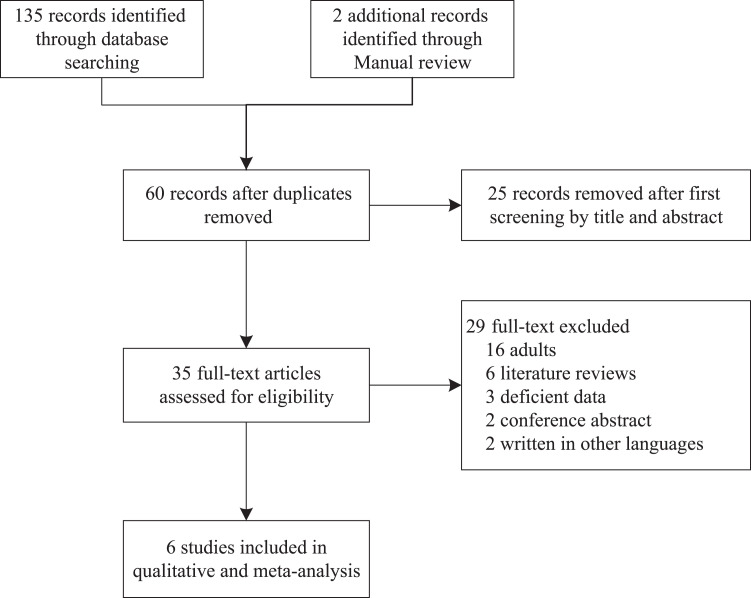
The literature search resulted in 137 potentially relevant studies (Figure 1). After the removal of duplicates and exclusion based on titles and abstracts, 3 RCTs,2,23,25 1 prospective study,1 and 2 retrospective cohort studies13,19 were included.
Figure 1.
Flowchart of literature search and study inclusion.
The included studies involved 339 patients who underwent nonsurgical treatment and 130 who underwent surgery (Table 1). The results of the risk-of-bias assessment for RCTs and for non-RCTs and retrospective cohort studies are shown in Tables 2 and 3. Clinical outcomes are summarized in Table 4.
TABLE 1.
Characteristics of Included Studiesa
| Author (Year) | Study Type | Age,b y | Initial No. of Patients (M/F) | Intervention | Follow-up,c y |
|---|---|---|---|---|---|
| Askenberger2 (2018) | RCT | 2 | |||
| Nonsurgical | 13.03 ± 1.14 | 37 (17/20) | 4 wk of brace and physical therapy | ||
| Surgical | 13.19 ± 1.08 | 37 (19/18) | MPFL repair | ||
| Regalado25 (2016) | RCT | 3 and 6 | |||
| Nonsurgical | 13.5 (8-16) | 20 (9/11) | 6 wk of brace and physical therapy | ||
| Surgical | 13.5 (8-16) | 16 (5/11) | Isolated LRR and modified RG procedure | ||
| Palmu23 (2008) | RCT | 7 and 14 (11-15) | |||
| Nonsurgical | 13 ± 2 | 28 (9/19) | Immobilization and thigh muscle exercises | ||
| Surgical | 13 ± 2 | 32 (5/27) | MPFL repair and LRR or isolated LRR | ||
| Apostolovic1 (2011) | Non-RCT | 6.1 (5-8) | |||
| Nonsurgical | 14.26 (12-16) | 23 (4/19) | 3 wk of immobilization quadriceps exercises | ||
| Surgical | 13.07 (12-16) | 14 (5/9) | MRR and capsular repair or LRR | ||
| Moström19 (2014) | RCS | ||||
| Nonsurgical | 13.5 ± 1.3 | 33 (17/16) | Physical therapy | 7.7 ± 1.5 | |
| Surgical | 12.6 ± 2.3 | 7 (4/3) | Proximal realignment and LRR with RG or RET procedure | 7.0 ± 1.4 | |
| Lewallen13 (2013) | RCS | 3.1 | |||
| Nonsurgical | 14.9 (9-18) | 198 (—) | Closed reduction and immobilization with physical therapy | ||
| Surgical | 14.9 (9-18) | 24 (—) | LRR, MPFL repair, and medial extensor mechanism imbrication |
aF, female; LRR, lateral retinacular release; M, male; MPFL, medial patellofemoral ligament; MRR, medial retinacular release; RCS, retrospective cohort study; RCT, randomized controlled trial; RET, Roux-Elmslie-Trillat; RG, Roux-Goldthwait.
bPresented as mean ± SD or median (range).
cPresented as mean, mean (range), or mean ± SD.
TABLE 2.
Risk of Bias for Randomized Controlled Trials (Cochrane Risk-of-Bias Tool9)
| Author (Year) | Random Sequence Generation | Allocation Concealment | Blinding of Participants and Personnel | Blinding of Outcome Assessment | Incomplete Outcome Data | Selective Reporting | Other Source of Bias |
|---|---|---|---|---|---|---|---|
| Askenberger2 (2018) | Low | Low | High | High | Low | Low | Low |
| Regalado25 (2016) | High | High | High | High | Low | Low | Low |
| Palmu23 (2008) | Unclear | Unclear | High | High | High | Unclear | High |
TABLE 3.
Risk of Bias for Non–Randomized Controlled Trials and Retrospective Cohort Studies (Newcastle-Ottawa Scale31)
| Author (Year) | Selection | Comparability | Outcome | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Representativeness of Exposed Cohort | Selection of Nonexposed Cohort | Ascertainment of Exposure | Demonstration That Outcome of Interest Was Not Present at Start of Study | Selection of Most Important Factor | Study Controls for Any Additional Factor | Assessment of Outcome | Selection of Adequate Follow-up Period for Outcome of Interest | Adequacy of Follow-up of Cohort | |
| Apostolovic1 (2011) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 |
| Moström19 (2014) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 1 |
| Lewallen13 (2013) | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 0 | 0 |
TABLE 4.
Clinical Outcomes Between Surgery and Nonsurgical Treatment for Primary Patellar Dislocationsa
| Author (Year) | No. of Redislocations | Kujala Score | No. of Reoperations | Subjective Satisfactionb | Tegner Score | Cincinnati Score | VAS Score | KOOS Subscore | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pain | Symptoms | ADL | Sports | QoL | ||||||||
| Askenberger2 (2018) | ||||||||||||
| Nonsurgical | 16 | 95.9 ± 7.2 | NR | NR | 5.0 ± 1.4 | NR | NR | 89.3 ± 11.7 | 89.3 ± 13.0 | 96.4 ± 7.0 | 84.4 ± 16.5 | 74.9 ± 16.8 |
| Surgical | 8 | 90.9 ± 13 | NR | NR | 4.5 ± 2.0 | NR | NR | 83.1 ± 16.8 | 82.1 ± 16.1 | 92.2 ± 11.4 | 70.4 ± 25.5 | 62.7 ± 22.5 |
| Regalado25 (2016)c | ||||||||||||
| Nonsurgical | 7 | NR | 4 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Surgical | 0 | NR | 0 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Regalado25 (2016)d | ||||||||||||
| Nonsurgical | 11 | NR | 5 | 11 | NR | NR | NR | NR | NR | NR | NR | NR |
| Surgical | 5 | NR | 0 | 13 | NR | NR | NR | NR | NR | NR | NR | NR |
| Palmu23 (2008)e | ||||||||||||
| Nonsurgical | 15 | 88.0 ± 8.0 | NR | 22 | 5.2 ± 2.1 | NR | 90 ± 9 | NR | NR | NR | NR | NR |
| Surgical | 18 | 81.0 ± 21.0 | NR | 21 | 4.7 ± 2.0 | NR | 83 ± 17 | NR | NR | NR | NR | NR |
| Palmu23 (2008)f | ||||||||||||
| Nonsurgical | 20 | 84.0 ± 13.0 | 11 | NR | 6.0 ± 1.9 | NR | 91 ± 10 | NR | NR | NR | NR | NR |
| Surgical | 24 | 83.0 ± 18.0 | 16 | NR | 4.4 ± 1.4 | NR | 84 ± 18 | NR | NR | NR | NR | NR |
| Apostolovic1 (2011) | ||||||||||||
| Nonsurgical | 1 | NR | 4 | NR | NR | 332.14 (210-420)g | NR | NR | NR | NR | NR | NR |
| Surgical | 2 | NR | 4 | NR | NR | 362.87 (170-420)g | NR | NR | NR | NR | NR | NR |
| Moström19 (2014) | ||||||||||||
| Nonsurgical | 22 | 84 ± 10 | NR | NR | NR | NR | NR | 90 ± 14 | 82 ± 14 | 94 ± 12 | 77 ± 24 | 69 ± 20 |
| Surgical | 3 | 84 ± 7 | NR | NR | NR | NR | NR | 92 ± 8 | 82 ± 11 | 97 ± 4 | 79 ± 15 | 76 ± 19 |
| Lewallen13 (2013) | ||||||||||||
| Nonsurgical | 76 | NR | 39 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
| Surgical | 8 | NR | 7 | NR | NR | NR | NR | NR | NR | NR | NR | NR |
aValues are shown as mean ± SD unless otherwise noted. ADL, Activities of Daily Living; KOOS, Knee injury and Osteoarthritis Outcome Score; NR, not reported; QoL, Quality of Life; VAS, visual analog scale.
bPresented as number of patients reporting excellent and good outcomes.
cAt 2 years after treatment.
dAt 6 years after treatment.
eAt 6 years after treatment.
fAt 14 years after treatment.
gPresented as median (interquartile range).
Redislocations
Redislocations were reported in all 6 studies (N = 469 knees). The overall rate of recurrence was 41.8% (196/469); specifically, 43.1% (146/339) of knees that underwent nonsurgical treatment and 38.4% (50/130) that underwent surgery experienced a redislocation. Several studies reporting outcomes at follow-up times shorter2,13,25 and longer than 5 years after the first treatment1,19,23,25 were considered separately in the analyses of short- and long-term outcomes.
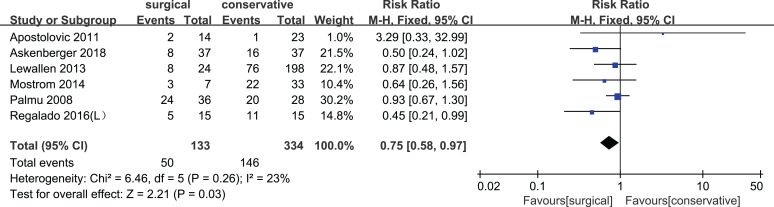
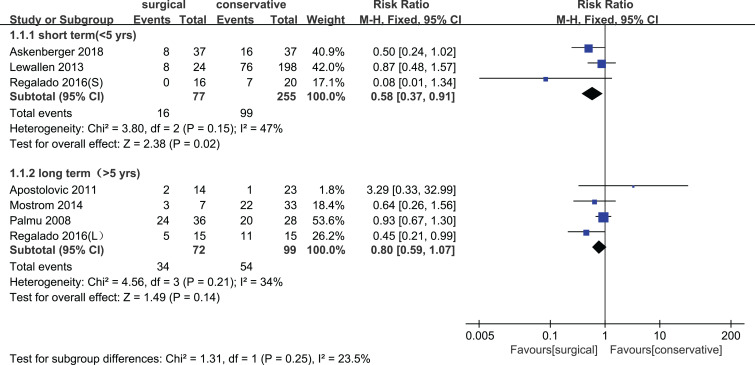
Using a fixed-effects model, the pooled meta-analysis across all studies showed that the surgery group had a significantly lower redislocation rate compared with the nonsurgical treatment group (RR, 0.75 [95% CI, 0.58-0.97]; P = .03; I 2 = 23%) (Figure 2). The subgroup meta-analysis using a fixed-effects model showed that surgical treatment was associated with a significantly lower redislocation rate than nonsurgical treatment within 5 years after treatment (RR, 0.58 [95% CI, 0.37-0.91]; P = .02; I 2 = 47%), but this result was not obtained beyond 5 years after treatment (RR, 0.80 [95% CI, 0.59-1.07]; P = .14; I 2 = 34%) (Figure 3).
Figure 2.
Forest plot of the meta-analysis comparing the incidence of overall redislocations between surgery and nonsurgical treatment, regardless of follow-up time (fixed-effects model; Mantel-Haenszel [M-H] method). L, long term.
Figure 3.
Forest plot of the meta-analysis comparing the incidence of redislocations between surgical and nonsurgical treatment, stratified by short- and long-term follow-up (fixed-effects model; Mantel-Haenszel [M-H] method). L, long term; S, short term.
Kujala Score
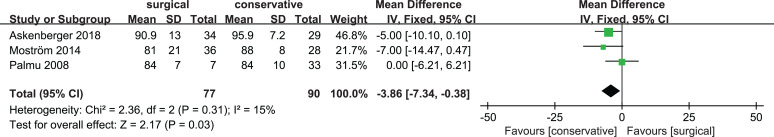
The Kujala score was reported in 3 studies,2,19,23 which included 174 patients (98 for nonsurgical treatment and 76 for surgery). One of these studies reported short- and long-term scores, and these were considered separately in the subgroup analysis.23
Surgery was associated with a significantly lower Kujala score in the RCTs by Askenberger et al2 (follow-up of <5 years) and Palmu et al23 (cohort with follow-up of 5-10 years). However, no significant difference in scores was seen in the Moström et al19 study or in the Palmu et al cohort with over 10-year follow-up.
A subsequent meta-analysis using a fixed-effects model showed that surgical treatment was associated with a significantly lower Kujala score compared with nonsurgical treatment within 10 years after treatment (MD, 3.86 [95% CI, 0.38-7.34]; P = .03; I 2 = 15.1%) (Figure 4).
Figure 4.
Forest plot of the meta-analysis comparing the Kujala score after surgical or nonsurgical treatment for all patients, regardless of follow-up time (fixed-effects models; inverse variance [IV] method).
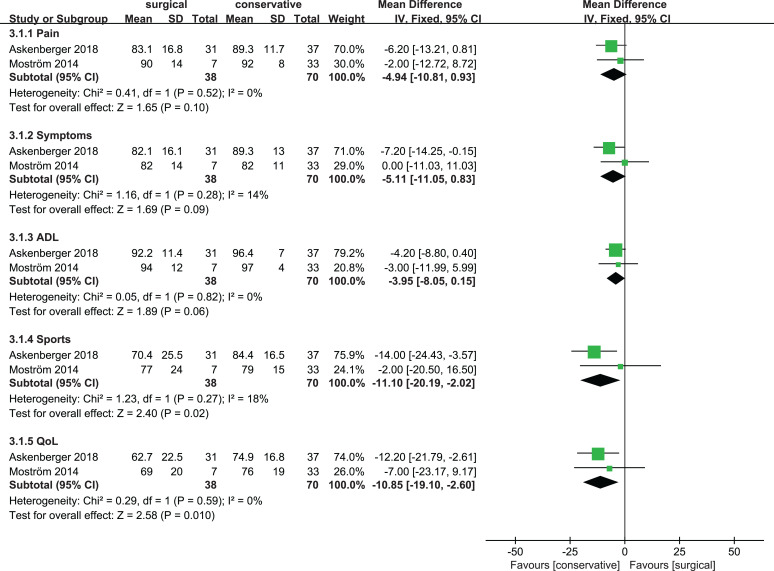
KOOS Score
Overall, 2 studies2,19 reported KOOS scores for 114 patients, including 70 for nonsurgical treatment and 44 for surgery. The RCT by Askenberger et al,2 reporting results within 5 years, showed that patients treated nonsurgically had a better knee function score on all 5 subscales of the KOOS compared with surgical treatment. In the Moström et al19 study, with a follow-up beyond 5 years, all 5 subscores were similar except that surgery was associated with a significantly higher score on quality of life.
The meta-analysis showed a significantly higher KOOS score with nonsurgical treatment on 2 of 5 subscales: sports (MD, 11.10 [95% CI, 2.02-20.19]; P = .02; I 2 = 18%) and quality of life (MD, 10.85 [95% CI, 2.60-19.10]; P = .01; I 2 = 0%). The relatively higher score on the other 3 subscales indicated a tendency for supporting nonsurgical treatment, although there was no statistically significant difference. These meta-analyses were carried out using a fixed-effects model (Figure 5).
Figure 5.
Forest plot of the meta-analysis comparing the Knee injury and Osteoarthritis Outcome Score (KOOS) score after surgical or nonsurgical treatment for all patients, regardless of follow-up time (fixed-effects models; inverse variance [IV] method).
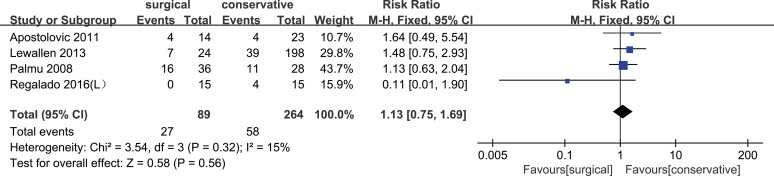
Reoperations
A total of 4 studies1,13,23,25 (n = 355 patients, including 269 for nonsurgical treatment and 86 for surgical treatment), reported on the occurrence of reoperations. The overall rate of reoperations was 23.9% (85/355); specifically, 58 of 269 (21.6%) knees undergoing nonsurgical treatment and 27 of 86 (31.4%) undergoing surgery experienced subsequent surgery. Quantitative analysis using a fixed-effects model showed that the occurrence was similar after surgical or nonsurgical treatment among all patients (RR, 1.13 [95% CI, 0.75, 1.69]; P = .56; I 2 = 15%) (Figure 6).
Figure 6.
Forest plot of the meta-analysis comparing the incidence of reoperations between surgical and nonsurgical treatment, regardless of follow-up time (fixed-effects model; Mantel-Haenszel [M-H] method).
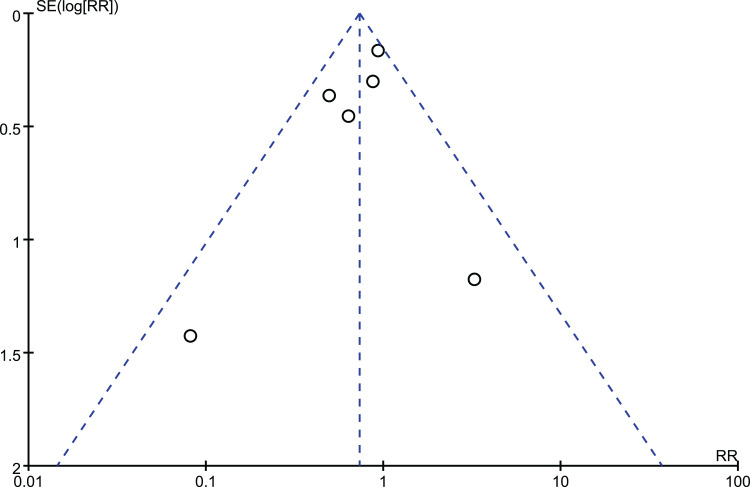
Risk of Bias and Quality of Evidence
All studies showed a relatively high risk of bias. In particular, blinding was lacking in all the studies for the nature of surgical trials, which might affect subjective outcomes such as the Kujala and KOOS scores. The high risk of bias also influenced the quality of evidence by the GRADE guidelines. Because of the lack of blinding for the Kujala and KOOS scores, the level of evidence was downgraded 2 points. The evidence for redislocation and reoperation rates was downgraded by just 1 point because lack of blinding had limited influence on objective outcomes. Regarding inconsistency, the heterogeneity of our study was relatively low except for the KOOS score, which entailed further downgrading for the KOOS score. No points were lost owing to the risk of publication bias (Figure 7). Thus, the level of evidence was moderate for redislocations and reoperations, low for the Kujala score, and very low for the KOOS score.
Figure 7.
Funnel plot to assess publication bias for the redislocation rate. RR, risk ratio.
Discussion
For adolescents with PPDs, surgery was superior to nonsurgical treatment in the short term with regard to the redislocation rate, whereas the outcome of knee function was favorable with nonsurgical treatment. However, the superiority of either surgery or nonsurgical treatment in adolescents did not appear to persist in the long term.
A few published systematic reviews and meta-analyses in the past 5 years have compared the efficacy of surgery versus nonsurgical treatment. There were 2 meta-analyses15,33 that indicated that, when patient age and follow-up duration are not taken into account, surgery is associated with a lower recurrent dislocation rate and similar Kujala scores as nonsurgical treatment. When only considering the follow-up duration, 3 meta-analyses27,29,34 further suggested a lower redislocation rate and better Kujala score with surgery than with nonsurgical treatment in the short term, but these benefits disappeared in the long term.
When separately analyzing skeletally immature patients, the present review also confirmed this tendency favoring surgery, although only in reducing the redislocation rate. To our surprise, none of our included studies reported a significant benefit of surgery over nonsurgical treatment on knee function in terms of the Kujala or KOOS score in either the short or long term, and some studies even observed worse Kujala and KOOS scores in the short term.2,23 This result is different from what was reported by Nwachukwu et al22 in their review of children and adolescents with acute patellar dislocation. They observed a lower redislocation rate, higher clinical scores, and better return-to-sport levels for patients who underwent surgery. However, their study included some uncontrolled studies and qualitatively analyzed them with other controlled studies. Moreover, they did not include the 2018 high-level RCT by Askenberger et al.2
Similar to our results, several original articles have also confirmed this conclusion.2,23 This result may reflect overtightening or insufficient tissue integrity and weaker muscle function in adolescents, which likely do not match their accelerated growth.2 The finding may also help explain why previous meta-analyses27,33,35 involving both adults and adolescents made the paradoxical observation that surgery was associated with a lower rate of redislocations but not better Kujala scores than nonsurgical treatment.
The results of our meta-analysis remind us that surgery does not always work for adolescents. Before offering a treatment suggestion, we should take patients’ comments into consideration, whether they are associated with worry about redislocation or poor knee function. According to our study, surgery may effectively help a patient with the former concern, while patients plagued by the latter should be informed of the risk of a poor prognosis in the short term and carefully weigh the pros and cons of surgery. Given the invasiveness and cost of surgery,21 this consideration can maximize the benefits and reduce the risks of surgery for adolescents with PPDs.12,14,32
Limitations
Despite various strengths, this study exhibited several limitations. First, the number of included studies in each subgroup was relatively small. Second, 2 retrospective studies were included in the study, which may have increased the risk of bias or confounding. Third, the follow-up duration on adolescents was from 2 to 14 years, which may have contributed to heterogeneity and confounded results. Fourth, patients across the studies varied in their baseline characteristics, including age, sex, and family history, all of which are regarded as risk factors for primary and recurrent patellar dislocations.8,11,13 Fifth, surgical methods differed across the studies, which could have affect outcomes.16,30
Conclusion
This study found that for adolescents with PPDs, surgery was superior to nonsurgical treatment in the short term to improve the redislocation rate but resulted in poorer outcomes of knee function based on the Kujala and KOOS scores. However, the superiority of either surgery or nonsurgical treatment in adolescents did not appear to persist in the long term. Our results should be confirmed through future large, high-quality RCTs.
Footnotes
Final revision submitted February 23, 2020; accepted March 26, 2020.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Apostolovic M, Vukomanovic B, Slavkovic N, et al. Acute patellar dislocation in adolescents: operative versus nonoperative treatment. Int Orthop. 2011;35(10):1483–1487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Askenberger M, Bengtsson ME, Ekström W, et al. Operative repair of medial patellofemoral ligament injury versus knee brace in children with an acute first-time traumatic patellar dislocation: a randomized controlled trial. Am J Sports Med. 2018;46(10):2328–2340. [DOI] [PubMed] [Google Scholar]
- 3. Bitar AC, D’Elia CO, Demange MK, Viegas AC, Camanho GL. Randomized prospective study on traumatic patellar dislocation: conservative treatment versus reconstruction of the medial patellofemoral ligament using the patellar tendon, with a minimum of two years of follow-up. Rev Bras Ortop. 2011;46(6):675–683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Camanho GL, Viegas AC, Bitar AC, Demange MK, Hernandez AJ. Conservative versus surgical treatment for repair of the medial patellofemoral ligament in acute dislocations of the patella. Arthroscopy. 2009;25(6):620–625. [DOI] [PubMed] [Google Scholar]
- 5. Cofield RH, Bryan RS. Acute dislocation of the patella: results of conservative treatment. J Trauma. 1977;17(7):526–531. [DOI] [PubMed] [Google Scholar]
- 6. Fithian DC, Paxton EW, Stone ML, et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32(5):1114–1121. [DOI] [PubMed] [Google Scholar]
- 7. Fuller J, Hammil H, Pronschinske K, Durall C. Operative vs. nonoperative treatment after acute patellar dislocation: which is more effective at reducing recurrence in adolescents. J Sport Rehabil. 2018;27(6):601–604. [DOI] [PubMed] [Google Scholar]
- 8. Gravesen KS, Kallemose T, Blønd L, Troelsen A, Barfod KW. High incidence of acute and recurrent patellar dislocations: a retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1204–1209. [DOI] [PubMed] [Google Scholar]
- 9. Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions: Version 5.1.0. 2011. www.handbook.cochrane.org. Accessed February 1, 2020.
- 10. Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jaquith BP, Parikh SN. Predictors of recurrent patellar instability in children and adolescents after first-time dislocation. J Pediatr Orthop. 2017;37(7):484–490. [DOI] [PubMed] [Google Scholar]
- 12. Kang HJ, Wang F, Chen BC, Zhang YZ, Ma L. Non-surgical treatment for acute patellar dislocation with special emphasis on the MPFL injury patterns. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):325–331. [DOI] [PubMed] [Google Scholar]
- 13. Lewallen LW, McIntosh AL, Dahm DL. Predictors of recurrent instability after acute patellofemoral dislocation in pediatric and adolescent patients. Am J Sports Med. 2013;41(3):575–581. [DOI] [PubMed] [Google Scholar]
- 14. Liu JN, Steinhaus ME, Kalbian IL, et al. Patellar instability management: a survey of the International Patellofemoral Study Group. Am J Sports Med. 2018;46(13):3299–3306. [DOI] [PubMed] [Google Scholar]
- 15. Longo UG, Ciuffreda M, Locher J, Berton A, Salvatore G, Denaro V. Treatment of primary acute patellar dislocation: systematic review and quantitative synthesis of the literature. Clin J Sport Med. 2017;27(6):511–523. [DOI] [PubMed] [Google Scholar]
- 16. Ma LF, Wang F, Chen BC, Wang CH, Zhou JW, Wang HY. Medial retinaculum plasty versus medial patellofemoral ligament reconstruction for recurrent patellar instability in adults: a randomized controlled trial. Arthroscopy. 2013;29(5):891–897. [DOI] [PubMed] [Google Scholar]
- 17. Maenpaa H, Huhtala H, Lehto MU. Recurrence after patellar dislocation: redislocation in 37/75 patients followed for 6-24 years. Acta Orthop Scand. 1997;68:424–426. [DOI] [PubMed] [Google Scholar]
- 18. Matic GT, Magnussen RA, Kolovich GP, Flanigan DC. Return to activity after medial patellofemoral ligament repair or reconstruction. Arthroscopy. 2014;30(8):1018–1025. [DOI] [PubMed] [Google Scholar]
- 19. Moström EB, Mikkelsen C, Weidenhielm L, Janarv PM. Long-term follow-up of nonoperatively and operatively treated acute primary patellar dislocation in skeletally immature patients. ScientificWorldJournal. 2014;2014:473281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nomura E, Inoue M. Second-look arthroscopy of cartilage changes of the patellofemoral joint, especially the patella, following acute and recurrent patellar dislocation. Osteoarthritis Cartilage. 2005;13(11):1029–1036. [DOI] [PubMed] [Google Scholar]
- 21. Nwachukwu BU, So C, Schairer WW, et al. Economic decision model for first-time traumatic patellar dislocations in adolescents. Am J Sports Med. 2017;45(10):2267–2275. [DOI] [PubMed] [Google Scholar]
- 22. Nwachukwu BU, So C, Schairer WW, Green DW, Dodwell ER. Surgical versus conservative management of acute patellar dislocation in children and adolescents: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24(3):760–767. [DOI] [PubMed] [Google Scholar]
- 23. Palmu S, Kallio PE, Donell ST, Helenius I, Nietosvaara Y. Acute patellar dislocation in children and adolescents: a randomized clinical trial. J Bone Joint Surg Am. 2008;90(3):463–470. [DOI] [PubMed] [Google Scholar]
- 24. Panni AS, Vasso M, Cerciello S. Acute patellar dislocation: what to do. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):275–278. [DOI] [PubMed] [Google Scholar]
- 25. Regalado G, Lintula H, Kokki H, Kröger H, Väätäinen U, Eskelinen M. Six-year outcome after non-surgical versus surgical treatment of acute primary patellar dislocation in adolescents: a prospective randomized trial. Knee Surg Sports Traumatol Arthrosc. 2016;24(1):6–11. [DOI] [PubMed] [Google Scholar]
- 26. Ryan R, Hill S. How to GRADE the Quality of the Evidence: Version 3.0. 2016. http://cccrg.cochrane.org/author-resources. Accessed February 1, 2020.
- 27. Saccomanno MF, Sircana G, Fodale M, Donati F, Milano G. Surgical versus conservative treatment of primary patellar dislocation: a systematic review and meta-analysis. Int Orthop. 2016;40(11):2277–2287. [DOI] [PubMed] [Google Scholar]
- 28. Sanders TL, Pareek A, Hewett TE, Stuart MJ, Dahm DL, Krych AJ. High rate of recurrent patellar dislocation in skeletally immature patients: a long-term population-based study. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1037–1043. [DOI] [PubMed] [Google Scholar]
- 29. Smith TO, Donell S, Song F, Hing CB. Surgical versus non-surgical interventions for treating patellar dislocation. Cochrane Database Syst Rev. 2015;2:CD008106. [DOI] [PubMed] [Google Scholar]
- 30. Song JG, Kang SB, Oh SH, et al. Medial soft-tissue realignment versus medial patellofemoral ligament reconstruction for recurrent patellar dislocation: systematic review. Arthroscopy. 2016;32(3):507–516. [DOI] [PubMed] [Google Scholar]
- 31. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010;25:603–605. [DOI] [PubMed] [Google Scholar]
- 32. Stefancin JJ, Parker RD. First-time traumatic patellar dislocation: a systematic review. Clin Orthop Relat Res. 2007;455:93–101. [DOI] [PubMed] [Google Scholar]
- 33. Wang SN, Qin CH, Jiang N, Wang BW, Wang L, Yu B. Is surgical treatment better than conservative treatment for primary patellar dislocations? A meta-analysis of randomized controlled trials. Arch Orthop Trauma Surg. 2016;136(3):371–379. [DOI] [PubMed] [Google Scholar]
- 34. Yao LW, Zhang C, Liu Y, et al. Comparison operative and conservative management for primary patellar dislocation: an up-to-date meta-analysis. Eur J Orthop Surg Traumatol. 2015;25(4):783–788. [DOI] [PubMed] [Google Scholar]
- 35. Zheng X, Kang K, Li T, Lu B, Dong J, Gao S. Surgical versus non-surgical management for primary patellar dislocations: an up-to-date meta-analysis. Eur J Orthop Surg Traumatol. 2014;24(8):1513–1523. [DOI] [PubMed] [Google Scholar]