Respiratory system is the main target in COVID-19 infection.1 Acute gastrointestinal (GI) manifestations of COVID-19 are rare.2–4 We describe a case of COVID-19 presenting with acute abdomen, diagnosed as haemorrhagic enteritis.
A 61-year-old man residing in a COVID-19 containment area presented in emergency room with severe abdominal pain and vomiting. There was no history of fever, cough, respiratory or any significant symptoms. Contrast enhanced computer topography axial precontrast and postcontrast venous phase showed long segment small bowel wall thickening with high-density areas in the bowel wall likely representing haemorrhage with mild ascites (figure 1A, B). Routine haemogram showed haemoglobin 8.5 gm/dL, total white cell count 6900/mm3 and platelet count 137000/mm3. Prothrombin time was 24.4 s (control value 12.05) and international normalised ratio 2.19. In view of his residential area, nasopharyngeal swab was collected for COVID-19 testing by RT-PCR. With due precautions, patient was operated on emergency basis. Explorative laparotomy with resection of bowel segment and ileostomy was done. After surgery, the report of COVID-19 was found to be positive. Postoperative period was uneventful. Resected specimen of small intestine measuring 70 cm in length was markedly congested, haemorrhagic with viable resection margins. Histopathology revealed extensive transmural haemorrhages with many congested and dilated blood vessels. Occasional fibrin thrombi are seen within capillaries (figure 1C). There was no evidence of viral, fungal infection, other infective or inflammatory pathology.
Figure 1.
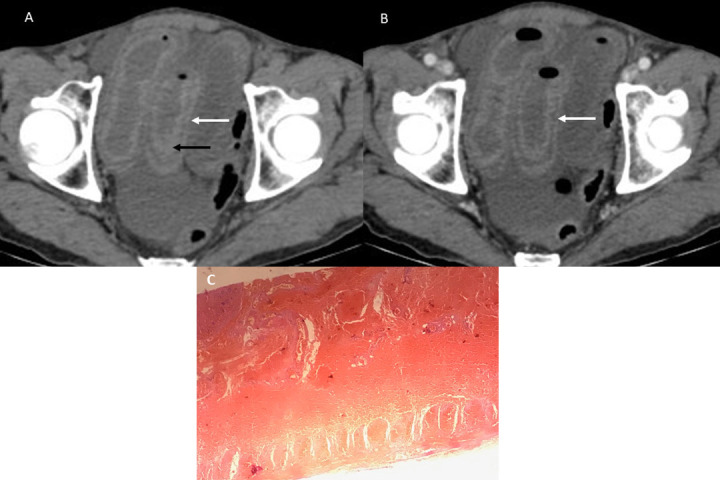
Axial (A) precontrast and (B) postcontrast venous phase showing long segment small bowel wall thickening (white arrows) with high-density areas in the bowel wall (black arrow in A) representing haemorrhage with mild ascites. (C) Histopathology showing extensive transmural haemorrhages (He 100×).
Extrapulmonary involvement of COVID-19 is in the form of coagulopathy, venous thromboembolism and GI involvement.2–5 Most of the patients with GI involvement present with diarrhoea, abdominal pain, vomiting or nausea. GI symptoms can exist independently of respiratory symptoms. Our case presented with acute abdomen and diagnosed as haemorrhagic enteritis without any predisposing conditions. Patient was COVID-19 positive on RT-PCR. Whether it was causal or coincidence, one should be aware of atypical life-threatening GI symptoms associated with COVID-19 infection. There should be high index of suspicion and encourage to test for COVID-19 in this pandemic situation.
Footnotes
Handling editor: Runjan Chetty.
Contributors: All authors contributed equally to the work. ADA, PV and NP: contributed to this article with literature review, data analysis and drafting the manuscript. PV and NP: data acquisition, analysis and interpretation. ADA: critical revision and editing for intellectual content; conception and design of the study; and final approval of the final version.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Next of kin consent obtained.
Provenance and peer review: Not commissioned; internally peer reviewed.
References
- 1. Huang C, Wang Y, Li X, et al. . Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497–506. 10.1016/S0140-6736(20)30183-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Wong SH, Lui RN, Sung JJ. Covid-19 and the digestive system. J Gastroenterol Hepatol 2020;35:744–8. 10.1111/jgh.15047 [DOI] [PubMed] [Google Scholar]
- 3. Wang D, Hu B, Hu C, et al. . Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061–9. 10.1001/jama.2020.1585 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pan L, Mu M, Yang P, et al. . Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol 2020;115:766–73. 10.14309/ajg.0000000000000620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tang N, Li D, Wang X, et al. . Abnormal coagulation parameters are associated with poor prognosis in patients with novel coronavirus pneumonia. J Thromb Haemost 2020;18:844–7. 10.1111/jth.14768 [DOI] [PMC free article] [PubMed] [Google Scholar]


