Abstract
Objective
To explore the role of psychological, social and contextual factors across the recovery stages (ie, acute, rehabilitation or return to sport (RTS)) following a traumatic time-loss sport-related knee injury.
Material and methods
This review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews and Arksey and O’Malley framework. Six databases were searched using predetermined search terms. Included studies consisted of original data written in English that identified or described a psychological, social or contextual factor related to recovery after a traumatic time-loss sport-related knee injury. Two authors independently conducted title–abstract and full-text reviews. Study quality was assessed using the Mixed Methods Appraisal Tool. Thematic analysis was undertaken.
Results
Of 7289 records, 77 studies representing 5540 participants (37% women, 84% anterior cruciate ligament tears, aged 14–60 years) were included. Psychological factors were investigated across all studies, while social and contextual factors were assessed in 39% and 21% of included studies, respectively. A cross-cutting concept of individualisation was present across four psychological (barriers to progress, active coping, independence and recovery expectations), two social (social support and engagement in care) and two contextual (environmental influences and sport culture) themes. Athletes report multiple barriers to recovery and valued their autonomy, having an active role in their recovery and diverse social support.
Conclusion
Diverse psychological, social and contextual factors are present and influence all stages of recovery following a traumatic sport-related knee injury. A better understanding of these factors at the time of injury and throughout rehabilitation could assist with optimising injury management, promoting RTS, and long-term health-related quality-of-life.
Keywords: knee injuries, recovery, rehabilitation, review, sporting injuries
Background
Up to 40% of reported time-loss sport injuries involve knee trauma.1 2 Despite best efforts, many athletes do not return to sport (RTS) following a traumatic knee injury3 4 and/or develop early-onset post-traumatic osteoarthritis (PTOA), irrespective of management approach.5–7 Traditionally, injury recovery predominantly focused on resolving physical impairments. However, improved physical outcomes are not always associated with return to physical activity,8 long-term satisfaction9 or favourable health-related quality-of-life (HRQoL),10 suggesting that additional ‘non-physical factors’ may mediate recovery. These non-physical factors likely encompass a broad range of psychological, social and contextual domains.11
Psychological factors that influence recovery from a traumatic, time-loss, sport-related knee injury include cognitive (eg, perceptions), behavioural (eg, adherence) and affective (eg, moods) responses associated with an individual’s experience of the injury, rehabilitation, surgery and RTS.11 12 For example, fear of re-injury and poor psychological readiness for RTS in individuals with an anterior cruciate ligament (ACL) tear negatively influence activity levels and RTS.13–15 Similarly, a recent systematic review highlighted the association between greater preoperative self-efficacy (ie, belief that one is capable of executing a behaviour in a specific context)16 and less future knee pain and favourable functional and RTS outcomes following an ACL reconstruction (ACLR).17 Social factors that influence recovery in this population include the social networks (eg, family, sport, therapy) and social exchanges (eg, relationships, support) that influence, and are influenced by an individual’s injury experience.18 19 Specifically, effective communication and a strong patient–therapist (therapeutic) alliance have been shown to be associated with improved rehabilitation outcomes following a musculoskeletal injury.20 21 Contextual factors that influence an individual’s injury experience include the structural and institutional systems that they are embedded in (eg, physical or sport environment, ethnicity, socioeconomic status).19 22 For instance, cultural perceptions shaped by one’s ethnicity or societal influences (eg, community views about disability) could impact beliefs, recovery expectations, rehabilitation satisfaction, and HRQoL in individuals with chronic low back pain.23 24
A holistic approach that considers physical, psychological, social and contextual factors was recommended to optimise recovery in a recent consensus statement on sport-related injuries.25 Yet, evidence about the psychological, social and contextual factors influencing recovery following a time-loss sport-related knee injury is lacking, making clinical application of these recommendations challenging. Although previous reviews13 15 have broadly summarised psychosocial factors related to sport injury outcomes, no review has looked at psychological and social factors as distinct domains or considered contextual factors after a time-loss traumatic knee injury. Unlike a systematic review, which aims to synthesise evidence from multiple studies to answer a specific research question,26 a scoping review aims to map the breadth and depth of the current evidence around a particular topic that is dispersed across disciplines and heterogeneous study designs.27–29 The aim of this scoping review is to consolidate and examine the evidence related to the role of psychological, social and contextual factors across the recovery stages (ie, acute, rehabilitation or RTS) following a traumatic time-loss sport-related knee injury to identify key themes and knowledge gaps.
Methods
This review was conducted and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews.30 We followed the methodological framework of Arksey and O’Malley (2005) with refinements proposed by Levac et al (2010) and the Johanna Briggs Institute (2015).27–29 At the initiation of this review, there was no database to register a priori scoping review strategies.
Study team
To facilitate robust and clinically relevant review findings,29 the study team included individuals with expertise in evidence synthesis, quantitative and qualitative research methodology, clinical epidemiology, sport and exercise psychology, clinical therapeutic relationships, and sport and knee injury rehabilitation.
Data sources and search
Relevant studies were identified by searching six online databases (ie, MEDLINE, PsycINFO, CINAHL, SportDiscus, SCOPUS and ProQuest) from inception to May 2018, selected based on their relevance to the research topic. Keywords and constructs (ie, MeSH, Boolean phrases) used to execute each search were developed a priori from a preliminary search, conceptual papers,11 12 18 22 31 search strategies from relevant systematic reviews,13 14 and in consultation with team members and a health sciences librarian scientist. A list of search terms is provided in table 1, and the full search strategies for all databases are found in online supplementary file 1. To ensure that the search strategy was capturing relevant records, an iterative process involving team meetings to refine search terms and resolve challenges was used.27 29 One specific challenge was operationalising ‘psychological’, ‘social’ and ‘contextual’. In the end, search terms were refined to include examples of each. All searches were limited to the English language, conducted by the lead author, and organised using the reference management software EndNote X8.1.
Table 1.
Search terms
| Construct | Keywords |
| Population: (sport participants with a lower body injury)* |
Athlet* injur* or sport* injur* or recreation* injur* lower extremit* or lower limb* or hip* or thigh* or leg* or knee* or ankle* or foot or feet or toe* or ((anterior or posterior) adj cruciate adj2 ligament*) or ((medial or lateral) adj collateral adj2 ligament*) or femoracetabular or femur or menisc* or patellofemoral |
| Injury type: (musculoskeletal) |
tear* or rupture* or ligament* or sprain* or strain* or dislocation* |
| Non-physical factor: (psychological, social, contextual) | psycholog* or psychosocial or psycholog* response or psycholog* readiness or social support or cognition* or affect or behav* or motiv* or emotion* or patient belief* or confiden* or attitude* or personalit* or self esteem or locus of control or self efficacy or autonomy or kinesiophob* or fear* of reinjur* or avoidance or anxiet* or frustrat* or coping or cope or stress* or optimism or quality of life or patient satisfaction or goal setting or goal* or expectation* or perception* or patient prefer* or athlet* identit* or well-being or mindfulness or resilienc* or catastrophi* or accept* or compassion* or hope or achiev* or education or knowledge or relationship* or interaction* or alliance* or feedback or encourag* or trust or communicat* or rapport or respect or caring or connection or socioeconomic status or cultural or ethnicity or urban rural |
*initial search strategy targeted all traumatic sport-related lower extremity injuries.
bjsports-2019-101206supp001.pdf (349.8KB, pdf)
Study screening
After accounting for duplication, the titles and corresponding abstracts of all returned records were independently reviewed by two raters, blinded to record author(s) and journal title. Prior to the title and abstract reviews, all raters independently screened a random sample of 120 titles and abstracts to assess the applicability of the exclusion criteria and inter-rater agreement and Cohen’s kappa (K) with the senior author. All reviewers reached acceptable agreement (95%–98%, K=0.75–0.90). Finally, two independent raters performed full-text screening to determine final study selection. Consensus was reached on disagreements, first between raters and if required with the senior author. A review of the reference list of included studies, relevant systematic or literature reviews, and clinical guidelines was used to identify additional relevant records.
Study selection
Studies were included if they identified, described or assessed a psychological, social or contextual factor during the acute, rehabilitation or RTS stages of recovery following a traumatic time-loss knee injury resulting from or interfering with sport participation. See table 2 for definitions and table 3 for inclusion and exclusion criteria.
Table 2.
Operationalised definitions
| Term | Definition |
| Psychological factor | Cognitive, behavioural or affective responses associated with an individual’s experience of injury, rehabilitation, surgery and RTS11 |
| Social factor | Social networks and social exchanges that shape an individual’s experience of injury, rehabilitation, surgery and RTS18 32 |
| Contextual factor | Structural and institutional systems in which an individual is embedded that influence their experience of injury, rehabilitation, surgery and RTS22 31 |
| Acute recovery stage | The time period immediately post-injury and/or pre-surgery or post-surgery |
| Rehabilitation recovery stage | The time period between the acute and RTS stage that is focused on restoring physical and psychological function |
| RTS recovery stage | The time period when an injured athlete is engaged in a graduated RTS programme or have returned to sport and/or physical activity |
| Traumatic time-loss knee injury | Any trauma to the knee (joint, ligament, muscles) caused by a transfer of energy that exceeded the body’s ability to maintain its structural and/or functional integrity and resulted in a player missing at least one training session (practice) or match play129 |
| Sport participation | Participation in any level (recreation, competitive or professional) of organised sport at time of injury130
|
RTS, return to sport.
Table 3.
Study exclusion and inclusion criteria
| Inclusion criteria | Exclusion criteria |
| English language | Not English language |
| Human participants | Animal models or cadavers |
| Primary study design with original data | Not primary or original data (eg, conference proceedings or abstracts, editorials, commentaries, opinion-based papers or reviews) |
| Traumatic time-loss knee injury | Do not involve a traumatic time-loss knee joint injury |
| Describes a psychological, social or contextual factor during recovery (acute, rehabilitation or RTS) | Does not describe a psychological, social, contextual factor during recovery (eg, injury prevention, epidemiology or surgical technique studies) |
RTS, return to sport.
Data extraction
Data extracted from each study included the following: study year, design, location and aim; sport and sport participation level; sample age and size; injury type (eg, ACL, ACLR, patella dislocation); instrument(s) or approach(s) used to assess psychological, social and/or contextual factor; recovery stage (ie, acute, rehabilitation or RTS); and study result (ie, identification or description of psychological, social and/or contextual factor during the acute, rehabilitation or RTS stages of recovery). For studies that asked participants to reflect on past experiences, the assigned recovery stage was categorised based on the period being assessed.
Data extraction was completed by the lead author using a customised form. Prior to data extraction, the performance of the form was assessed by comparing data extracted by two independent raters across a purposive sample of 12 studies of various designs to ensure accurate and relevant data were extracted across different study designs.
Data synthesis
Individual psychological, social and contextual factors were identified across studies. Factors were operationalised based on consultation with the study team and relevant sport injury or conceptual papers.11 12 18 22 32 An inductive thematic analysis33 was used to identify patterns, summarise consistent findings across studies and generate common themes. The Biopsychosocial Model11 and WHO HRQoL framework34 were used to categorise individual factors and themes into psychological, social and contextual domains. These conceptual models were used to facilitate translation of the findings to patients, healthcare providers and other stakeholders and assist in the identification of knowledge gaps. Regular study team meetings were held to discuss and agree on emerging themes and interpretations.
Quality assessment
The methodological quality of included studies was assessed by two independent raters using the Mixed Methods Appraisal Tool (MMAT) 2018 Version (online supplementary file 2).35 The MMAT assesses five different methodological categories, allowing the tool to be used across various study designs and is reliable, valid and efficient.35–37 The level of evidence represented by each record was determined with a modified version of the Oxford Centre of Evidence Based Medicine (OCEBM) 2009 model (online supplementary file 3). Discrepancies in the MMAT scoring or OCEBM categorisation were resolved by consensus between the raters and as needed with the senior author.
Rigor
The iterative nature of a scoping review allows for refinement of exclusion and inclusion criteria to ensure an adequate yet feasible scope of relevant evidence.27 29 The initial scope of this review included grey literature (ie, PhD theses) and all sport-related lower extremity injuries. Given the small number of records remaining after title/abstract screening that assessed non-knee injuries (n=5) or grey literature (n=18), a decision was made to focus on published peer-reviewed studies and knee injuries. Of the 16 grey literature records pertaining to the knee, the findings of three were included as peer-reviewed papers and the remaining were re-visited to ensure no theme or construct was missed.
Results
Identification of studies
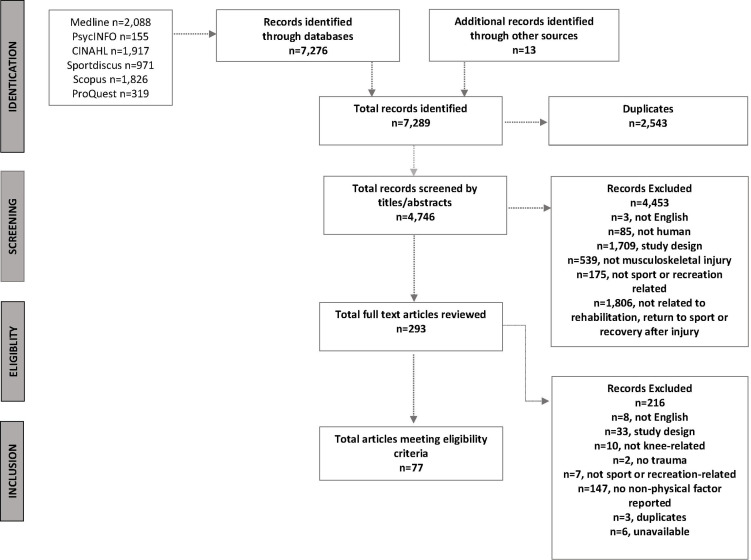
An overview of the study identification process is provided in figure 1. Of 7289 potential records, 4746 unique records underwent title/abstract screening, 293 were reviewed in full, and 77 studies were included.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Extension for Scoping Reviews flow chart.
Study characteristics
In all, 54 (70%) studies were quantitative (involving longitudinal (30%),38–63 cross-sectional (27%)64–84 or case series (5%)85–88 designs), three (4%) included an intervention,89–91 18 (23%) studies were qualitative92–109 (consisting of seven (39%) descriptive, five (28%) case or narrative, three (17%) grounded theory, and three (17%) phenomenology approaches) and five (6%) mixed methods designs.110–114 Full details of study characteristics are summarised in online supplementary file 4.
Studies represented data from 5540 participants (men=2986, women=2030) ranging in age from 14 to 60 years from 14 countries. Across studies, participants represented a variety of sport participation levels. Most studies investigated individuals 18 years of age or older (77%), with only two studies investigating adolescence. In all, 65 (84%) of studies involved individuals following ACL injury or ACLR, with the remaining investigating individuals with a patella dislocation, meniscectomy or other ligament injury.
Psychological, social and contextual factors and recovery stage
Table 4 provides the summary and definition of the psychological, social and contextual factors identified across studies. Psychological factors were reported in all studies, while only 39% and 21% of included studies reported on social and contextual factors, respectively. Most studies were performed during rehabilitation (47%) or RTS (37%) recovery stage, with only 15% of included studies addressing the acute stage.
Table 4.
Categorisation and definitions of identified psychological, social and contextual factors and themes
| Theme | Factor | Definition | No. of studies |
| Psychological domain | Psychological factor | 77 | |
| Barriers to progress | Fear/anxiety131 | Fear* is a biological mechanism associated with definite danger (eg, fear of re-injury), whereas anxiety is associated with anticipation or uncertainty from previous experience (eg, re-injury anxiety) | 29 |
| Other emotions32 | The way one feels after an event (eg, injury) and can consist of feelings and/or mood disturbances (eg, frustration, anger, depression) | 24 | |
| Psychological readiness32 | A state of mental preparedness. In the context of RTS, this includes an appraisal of one’s health status and risks (perceived or actual) associated with sport participation | 8 | |
| Sport-confidence132 | The belief or degree of certainty individuals possess about their ability to be successful in sport | 6 | |
| Active coping | Coping133 | Cognitive and behavioural efforts used to manage demands that are appraised as taxing or exceeding one’s resources | 19 |
| Identity134 | An internal, self -constructed, dynamic organisation of drives, abilities, beliefs, and individual history | 13 | |
| Catastrophising pain24 | A negative appraisal of pain that may represent ineffective or inappropriate pain coping strategy | 4 | |
| Resilience135 | The ability to use personal qualities to withstand pressure, ‘bounce back’, and persist during stressful or adverse encounters (eg, injury) | 2 | |
| Independence | Self-efficacy16 | A situation-specific form of confidence that involves self-assessment or judgement of one’s capability to execute behaviours to attain an outcome | 12 |
| Motivation115 | All aspects of activation and intention on behaviour, including energy, direction, persistence and equifinality | 10 | |
| Autonomy115 | An internal perceived locus of causality or degree to which individuals desire to control life events or behaviour | 4 | |
| Recovery expectations | Recovery expectation127 | A belief that some anticipated future outcome is likely | 12 |
| Perceptions136 | How one views or perceives their current situation or injury | 8 | |
| Beliefs136 | A dispositional mindset that may or may not manifest either in consciousness or behaviour | 5 | |
| Social domain | Social factor | 30 | |
| Social Support | Social support137 | An exchange of resources or social interactions between individuals comprising of emotional, informational and tangible support | 29 |
| Engagement in care | Therapeutic alliance138 | A working relationship between a healthcare provider and patient that involves agreement on treatment goals, tasks, and an affective bond (eg, trust) | 7 |
| Shared decision-making125 | A process whereby healthcare providers and patients work together to make healthcare choices based on best available evidence and patient’s values | 4 | |
| Contextual domain | Contextual factor | 16 | |
| Environmental influences | Environment139 | The atmosphere or setting of a situation which is created by a combination of external (eg, healthcare provider) factors and/or one’s individual context | 12 |
| Sport culture | Sport culture139 | The environment or ethos of a sport | 4 |
*Given that fear has been heavily investigated in this population, we chose to separate it from ‘other emotions.’ Fear and anxiety (fear of re-injury/re-injury anxiety) were grouped together as these two constructs were often used interchangeably across studies.
RTS, return to sport.
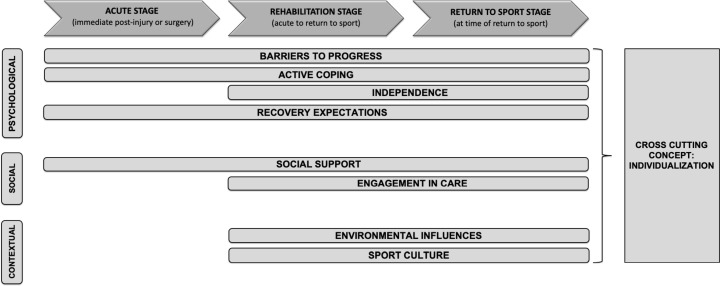
Data synthesis
Higher-level themes that represented consistent findings and patterns across studies are presented in figure 2. These themes were further categorised into psychological, social or contextual domains resulting in four psychological, two social and two contextual themes with one cross-cutting concept.
Figure 2.
Representation of psychological, social and contextual themes by recovery stage.
Psychological domain themes
Barriers to progress
Athletes experience a variety of barriers to progress during recovery from a knee injury. While fear was most commonly reported, other emotional barriers such as frustration and anxiety68 92–94 100 101 105 106 108 112 113 were evident throughout all recovery stages.41 57 68 83 93 96 100 110 Fear was most commonly seen as a major barrier during RTS.61 65 73 76 78 82 92 95 105 106 110 113 114 However, only 20%–45% of athletes stated fear as the main reason for not returning to sport73 76 78 113 with psychological readiness,48 64 84 85 knee and sport confidence,92 94 114 and motivation54 58 identified as other barriers for RTS. Beyond recovery, fear of re-injury was associated with ACL re-injury within 2–5 years53 88 and reduced activity levels 3–20 years following ACLR.47 95 113 Across studies, early recognition and acknowledgement of negative emotions were important for recovery.93 102 110
Active coping
Injured athletes value playing an active role in their recovery. Immediately after injury, athletes reported wanting strategies that help them understand their injury and diagnosis,94 103 110 manage emotions87 93 106 and deal with athletic identity loss.96–98 106 108 109 Approaches to managing recovery setbacks (eg, flare-ups or re-injuries)105 112 and problem-based coping tactics during RTS92 were also important. There was a continued need for active coping strategies beyond RTS to assist in accepting the long-term consequences of knee injury,94 95 improve knee confidence75 and transition to a life outside of sport.98 107 An absence of coping strategies was associated with being unprepared for the mental demands of recovery,97 depressed feelings,108 failed RTS102 and maladaptive behaviours such as substance abuse or catastrophising pain.40 In contrast, providing active coping strategies was associated with greater motivation,99 101 102 110 111 resilient behaviour,99 112 and adherence to rehabilitation.93 104
Independence
Across studies, injured athletes reported a desire to develop or preserve their independence and have control over their rehabilitation.42 56 60 67 69 70 93 97 99 101–103 112 Developing greater independence by promoting self-motivation,54 64 67 70 76 85 87 101 104–106 confidence,78 92 94 98 100 102 105 108 113 114 self-efficacy,60 81 99 and autonomy around decisions for RTS and future activity choices42 69 97 103 104 were reported to positively influence either rehabilitation or RTS outcomes. Furthermore, fostering psychological readiness for RTS promoted independence, self-awareness on readiness to RTS and greater confidence on RTS.39 48 64 84 85 92 100 102 103 109
Recovery expectations
Establishing realistic expectations for rehabilitation or RTS97 98 103 106 108 and long-term recovery66 109 was important to athletes recovering from knee injuries. However, several studies identified unrealistic expectations about the length of recovery by athletes requiring surgery.55 72 79 83 Not meeting recovery expectations was associated with negative emotions (eg, frustration) and a loss of confidence during rehabilitation.97 98 112 Interestingly, recovery expectations were influenced by interactions with healthcare providers,98 106 high-level role models, other players and coaches,98 105 prior perceptions,87 and/or beliefs.68 83
Social domain themes
Social support
The exchange of resources such as informational (ie, education) or emotional support positively influenced recovery expectations,98 101 106 negative emotions92 98 107 108 and risk appraisal on RTS.100 109 Social support was associated with greater adherence,52 67 93 104 106 resilience,94 99 confidence98 108 and self-motivation.106 108 Sources of social support changed throughout recovery with athletes reporting support from family, friends and teammates as important in early stages98 110 and a shift towards valuing support from coaches, physical therapists and other medical staff at later stages.50 92 110 Furthermore, an injury role model, a forum to discuss and share experiences, and establishing new social roles and networks were important for staying motivated and effectively coping during recovery from injury.94 96 99–101 103 106 108 111 112
Engagement in care
Injured athletes valued healthcare providers who engaged and involved them in their care through strategies such as goal setting.93 97 102 105 106 A strong therapeutic alliance, where individual goals and values of athletes were respected led to positive rehabilitation experiences and improved trust in healthcare providers.93 96 101 102 108 Open discussions with healthcare providers and coaches92 allowed for athletes to have autonomy over surgery and RTS decisions and favour successful RTS.98 103 106
Contextual domain themes
Environmental influences
An environment that promoted autonomy-supported behaviours were associated with greater levels of adherence to rehabilitation, independence and self-motivation.69 70 110 Considerations important for adherence to rehabilitation included addressing situational factors (eg, lack of time or equipment, personal activity preferences)104 and making rehabilitation enjoyable or challenging.93 97 104
Sport culture
A paucity of studies investigated the role of sport culture on recovery from a traumatic sport-related knee injury, but a few studies reported on the hyper-masculine culture of sport that validated enduring pain and downplaying injuries.92 107 Intense social pressure from peers106 and culture of risk-taking within sport92 109 contributed to athletes considering premature RTS.106 109
Cross-cutting concept of Individualisation
Psychological, social or contextual factors manifested differently across athletes, highlighting a concept of ‘individualisation’. For example, fear or anxiety may manifest as fear of re-injury/re-injury anxiety,65 71 73 74 76 78 82 94 95 105 106 113 114 fear/anxiety of poor performance,92 101 106 fear of failure,110 fear of the unknown or uncertainty of the situation (eg, contact sport, future long-term consequences)100 109 113 or fear of having to repeat rehabilitation.106 108 109 113 Similarly, individual coping strategies,83 101 111 desire for social support,50 112 preference to remain or avoid social roles96 102 105 106 and environmental factors that influence treatment adherence exist.44 104 Recovery expectations differed by gender and age, with men and younger athletes reporting greater expectations to RTS55 72 79 113 114 and different pressures to RTS (ie, peer pressure, performing through pain) compared with women or adults.106 107 109
Quality assessment
MMAT ratings of included studies are summarised in online supplementary file 4. Most quantitative studies were rated as poor to moderate quality with only six studies rated as high quality (scoring four or higher). Qualitative studies had higher MMAT scores with nine studies rated as high quality. The highest level of evidence demonstrated by quantitative studies using the OCEBM model was level 2b (low-quality RCTs), with the majority classified as level 4 (61%).
Discussion
This comprehensive synthesis highlights a broad spectrum of psychological, social and contextual factors that mediate recovery after a traumatic time-loss sport-related knee injury. Athletes who have suffered a sport-related knee injury experience fear/anxiety as well as other barriers to progress recovery, most predominately at RTS. Across all recovery stages, athletes valued having an active role in their recovery and engaging in decision-making, as well as having their autonomy respected. Working with healthcare providers to set realistic expectations and receiving educational resources and social support was essential to successfully recover from a sport-related knee injury. The psychological, social and contextual factors were dynamic over recovery stages, and must be assessed and managed on an individual level.
Psychological considerations for recovery from sport-related knee injury
We identified four themes within the psychological domain: barriers to progress, active coping, independence and recovery expectations. Consistent with previous research,13 14 fear is common in this population and consistently reported as a barrier for RTS.73 76 78 113 However, other barriers such as frustration, anxiety, lack of confidence,92 94 114 motivation54 58 or psychological readiness for RTS48 64 65 84 85 are also important. The desire for ‘active coping’ and ‘independence’ is consistent with the well-established self-determination theory115 that highlights satisfying individual needs for competence, relatedness and autonomy enhance recovery outcomes.116 Active coping strategies appear to be a common approach for athletes,117 which can promote motivation and resilience, particularly when facing a significant time-loss injury.59 99 101 102 110 111 Athletes should be active in the development of their rehabilitation plan to foster autonomy and enhance internal locus of control.115 Given the importance of RTS for this population, early discussions and setting realistic expectations are vital to minimise negative emotions in later stages of recovery.97 98 112
Social considerations for recovery from sport-related knee injury
Social support and engagement in care were the two themes identified in the social domain. As highlighted by others,20 118 needs for social support change over time and continued re-evaluation of these needs are required to ensure the amount and type of social support desired by the athletes recovering from a knee injury is provided. Social support in the form of education was desired throughout recovery. Knowledge is a cornerstone of patient empowerment119 and may be an important consideration for coping with a significant time-loss injury.
Patient and healthcare provider engagement in care is drawing considerable attention, given its positive association with self-care (eg, fostering autonomy) and overall health outcomes.120 Engagement is a necessary condition for a strong therapeutic relationship in physical therapy121 and a key component of a shared decision-making model.122 A strong therapeutic alliance was associated with improved rehabilitation outcomes in chronic musculoskeletal conditions123 and is likely relevant to recovery from a sport-related knee injury. Given the high risk of re-injury124 and future PTOA5 in this population, employing a shared decision-making approach early in the recovery process might enhance patient autonomy and the ability to make informed decisions regarding their current and future knee health. Although this model has been widely promoted as the ideal approach for RTS decisions,25 there appears to be a lack of understanding of shared decision-making in healthcare.125
Contextual considerations for recovery from sport-related knee injury
Contextual factors during recovery from a sport-related knee injury are rarely studied, but consistent themes of environmental influences and sport culture were present. Our findings align with prior research that highlight sport cultivates a culture of ‘no pain no gain’ and risk-taking, which can contribute to premature RTS and further injury.31 While it is not typical for healthcare providers to consider the systemic environmental factors that shape an athlete’s recovery from injury, it is essential to understand that this context may be a stronger determinant of recovery than the treatment provided as it determines access to resources and shapes behaviours.
Individual considerations for recovery from sport-related knee injury
The importance of tailoring recovery to the individual is essential if patient-centred care is the goal.126 Understanding personal goals, values and definitions of success are important as they influence recovery expectations.127 It is clear that individual characteristics such as gender, age and level of sport participation influence the presentation of psychological, social and contextual factors across recovery stages and can shape recovery outcomes, such as sport participation after an injury. For example, prior studies have reported that men are more likely to return to their pre-injury sport compared with women after ACLR.3 This might reflect gender-specific and sex-specific psychological, social and contextual factors. Specifically, men may embrace the hyper-masculine sport culture and indulge in risky behaviours92 107 than women who may be more risk adverse.109 Similarly, the social peer pressure to RTS may be more apparent during adolescence106 as sport participation is an important form of social connection during the developmental years.128 It is likely that cultural perceptions, religion, social gradient, and multiple other social and contextual factors also influence recovery and drive specific actions and behaviours in different populations. A better understanding of an individual’s context is essential to developing a holistic approach to optimise recovery.
Clinical implications
Table 5 provides the summary of the clinical implications of our findings.
Table 5.
Clinical implications
| Key findings from review | Clinical implications |
| 1. Acknowledge the importance of psychological, social and contextual factors | Psychological, social and contextual factors should be acknowledged and not be viewed as less important than physical factors. Given the wide range of psychological, social and contextual factors present, a holistic approach may more adequately determine the individual needs |
| 2. Psychological, social and contextual factors are dynamic and change over time | Psychological, social and contextual factors should be assessed early and monitored throughout recovery stages as they change from the acute to RTS stage of recovery |
| 3. Consider addressing social and contextual factors to optimise care | Strategies to develop a strong therapeutic alliance and engaging athletes in their care while considering how broader environmental and societal factors impact decision-making should be vital components of recovery |
| 4. Focus on the individual | Interpretation and experience of psychological, social and contextual factors during recovery is individual, and will facilitate the development of a recovery plan that best addresses individual needs and most likely to achieve success. |
Strengths and limitations
The broad research question and inclusion of diverse study designs that contained both quantitative and qualitative data resulted in a rich, in-depth mapping of the current evidence-base. Using two established frameworks required us to consider factors and themes in psychological, social and contextual domains, and provided more clarity about the types of factors and themes that are present in this population. We recognise that many identified factors share overlapping domains; however, this complexity and interrelatedness is critical to an accurate representation and understanding of psychological, social and contextual factors across recovery stages.
Scoping reviews rarely evaluate the methodological quality of included studies, but we chose to take this additional step to confidently develop our conclusions and identify the knowledge gaps.29 It is important to reiterate that most included studies were of poor to moderate methodological quality, indicating the need for higher-quality studies in this field. With that said, the consistent themes that emerged across studies provide us with confidence in our conclusions.
Despite a comprehensive search strategy, most included studies were limited to ACL injuries, pointing to a paucity of evidence related to other traumatic time-loss lower extremity injuries potentially limiting the generalisability of our findings. With that said, it is possible that our findings and their clinical implications may have broad applicability across recovery from other traumatic sport injuries. The studies contributing data to the RTS stage were heterogeneous in time since injury as many were retrospective in nature. While we followed a rigorous approach and engaged a research team with diverse expertise, formal consultation with other stakeholders (ie, persons with traumatic knee injuries), disciplines (ie, social scientists) and inclusion of grey literature may have provided further insight at all stages of the review.
Future directions
This review provides a foundation to understand the role and interactions between psychological, social and contextual factors as it relates to recovery following a traumatic time-loss sport-related knee injury. Although a great deal is known about interpersonal psychological factors, particularly fear, further research is needed to understand social and contextual factors, including the broader influence of systemic determinants on recovery from a traumatic time-loss sport-related knee injury. Overall, there is a paucity of knowledge about the status of psychological, social and contextual factors at the time of injury. Better understanding of these factors in the early stages of recovery will assist in the development of screening strategies for poor recovery and facilitate research aimed at understanding how these factors change and are influenced over time.
There is an opportunity to address inconsistencies in terminology used to define social and contextual factors within the sport and exercise medicine/rehabilitation field, and align with broader definitions from the social sciences. Furthermore, developing consensus on how individual psychological, social and contextual factors are defined and reported is essential for amalgamating data across studies and will promote uptake of these constructs in clinical practice.
Currently, there is a tendency in the sport and exercise medicine/rehabilitation field to lump psychological and social factors together and to focus care at the individual level. To date, few studies have considered the broader systemic aspects of social (societal) and contextual conditions (eg, social isolation or social gradient) in which athletes are injured and recover.19 A better understanding of how these broader social and contextual factors shape an athletes recovery is essential to optimising that process and improving overall well-being.
Conclusions
This scoping review highlighted the broad spectrum of psychological, social and contextual factors that can play a role during the acute, rehabilitation and RTS stages of recovery following a traumatic time-loss sport-related knee injury. The experience and interpretation of these factors are individual. While high-quality research is needed in this field, there appears to be consistent evidence of the impact of psychological and social factors on recovery. Individualised consideration of these factors should be an essential component of an evidence-based approach to managing sport-related knee injuries.
What are the new findings?
Psychological, social and contextual domains play an important role in recovery following a sport-related knee injury.
Athletes who suffer a sport-related time-loss knee injury experience many barriers to progress beyond fear across all stages of recovery.
Athletes value having an active role in their recovery, being engaged in decision-making, and having their autonomy respected.
Psychological, social and contextual factors change over time and should be assessed early and often throughout recovery stages.
Individual consideration of psychological, social and contextual factors is an essential component of an evidence-based approach to management of sport-related knee injuries.
How might it impact on clinical practice in the future?
Recovery from a traumatic time-loss knee injury does not always have a happy ending, with a significant proportion of individuals failing to return to pre-injury sport and reporting reduced health-related quality of life.
Despite many reports about the importance of considering psychological, social and contextual factors after a sport-related knee injury, management tends to prioritise physical impairments.
Assessment and monitoring of psychological, social and contextual factors should be conducted throughout recovery, and not just at the return to sport stage
Consider an individual and patient-centered focus when managing psychological, social and contextual factors to optimise recovery
Acknowledgments
The authors would like to acknowledge the assistance of Dr Linda Li who provided feedback on the first draft of the manuscript and Maria Tan, Health Science Librarian, who contributed to the development of the search strategy. LK Truong was supported by a First Year Recruitment Award provided by the Faculty of Rehabilitation Medicine, University of Alberta.
Footnotes
Twitter: @LKTphysio, @choltpt, @yegphysio, @twitter.com/MaxiMiciak, @jwhittak_physio
Collaborators: Linda C Li; Maria Tan.
Contributors: LKT and JLW were responsible for the conception of the study and along with Maria Tan developed the search strategy. LKT executed the search strategy. All authors independently reviewed records, assessed the methodological quality of included studies and extracted data. LKT was responsible for the first draft of the manuscript. All authors contributed to the interpretation of the findings, critical revision of the manuscript and reviewed the document prior to submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Emery CA, Meeuwisse WH, McAllister JR. Survey of sport participation and sport injury in Calgary and area high schools. Clin J Sport Med 2006;16:20–6. 10.1097/01.jsm.0000184638.72075.b7 [DOI] [PubMed] [Google Scholar]
- 2. Finch CF, Kemp JL, Clapperton AJ. The incidence and burden of hospital-treated sports-related injury in people aged 15+ years in Victoria, Australia, 2004-2010: a future epidemic of osteoarthritis? Osteoarthritis Cartilage 2015;23:1138–43. 10.1016/j.joca.2015.02.165 [DOI] [PubMed] [Google Scholar]
- 3. Ardern CL, Taylor NF, Feller JA, et al. . Fifty-five per cent return to competitive sport following anterior cruciate ligament reconstruction surgery: an updated systematic review and meta-analysis including aspects of physical functioning and contextual factors. Br J Sports Med 2014;48:1543–52. 10.1136/bjsports-2013-093398 [DOI] [PubMed] [Google Scholar]
- 4. Swart NM, van Oudenaarde K, Bierma-Zeinstra SMA, et al. . Predicting no return to sports after three months in patients with traumatic knee complaints in general practice by combining patient characteristics, trauma characteristics and knee complaints. Eur J Gen Pract 2019;25:205–13. 10.1080/13814788.2019.1646241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lie MM, Risberg MA, Storheim K, et al. . What’s the rate of knee osteoarthritis 10 years after anterior cruciate ligament injury? An updated systematic review. Br J Sports Med 2019;53:1162–7. 10.1136/bjsports-2018-099751 [DOI] [PubMed] [Google Scholar]
- 6. Whittaker JL, Toomey CM, Woodhouse LJ, et al. . Association between MRI-defined osteoarthritis, pain, function and strength 3-10 years following knee joint injury in youth sport. Br J Sports Med 2018;52:934–9. 10.1136/bjsports-2017-097576 [DOI] [PubMed] [Google Scholar]
- 7. Stein T, Mehling AP, Welsch F, et al. . Long-Term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med 2010;38:1542–8. 10.1177/0363546510364052 [DOI] [PubMed] [Google Scholar]
- 8. Ardern CL, Taylor NF, Feller JA, et al. . Return-to-sport outcomes at 2 to 7 years after anterior cruciate ligament reconstruction surgery. Am J Sports Med 2012;40:41–8. 10.1177/0363546511422999 [DOI] [PubMed] [Google Scholar]
- 9. Cole BJ, Cotter EJ, Wang KC, et al. . Patient understanding, expectations, outcomes, and satisfaction regarding anterior cruciate ligament injuries and surgical management. Arthroscopy 2017;33:1092–6. 10.1016/j.arthro.2017.01.049 [DOI] [PubMed] [Google Scholar]
- 10. Filbay SR, Ackerman IN, Russell TG, et al. . Health-Related quality of life after anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 2014;42:1247–55. 10.1177/0363546513512774 [DOI] [PubMed] [Google Scholar]
- 11. Brewer B, Andersen MB, Van Raalte JL. Psychological aspects of sport injury rehabilitation: Toward a biopsychosocial approach In: Mostofsky DL, Zaichkowsky LD, eds Medical and psychological aspects of sport and exercise, 2002: 41–54. [Google Scholar]
- 12. Wiese-bjornstal DM, Smith AM, Shaffer SM, et al. . An integrated model of response to sport injury: psychological and sociological dynamics. J Appl Sport Psychol 1998;10:46–69. 10.1080/10413209808406377 [DOI] [Google Scholar]
- 13. Forsdyke D, Smith A, Jones M, et al. . Psychosocial factors associated with outcomes of sports injury rehabilitation in competitive athletes: a mixed studies systematic review. Br J Sports Med 2016;50:537–44. 10.1136/bjsports-2015-094850 [DOI] [PubMed] [Google Scholar]
- 14. Ardern CL, Taylor NF, Feller JA, et al. . A systematic review of the psychological factors associated with returning to sport following injury. Br J Sports Med 2013;47:1120–6. 10.1136/bjsports-2012-091203 [DOI] [PubMed] [Google Scholar]
- 15. te Wierike SCM, van der Sluis A, van den Akker-Scheek I, Akker-Scheek vanden, et al. . Psychosocial factors influencing the recovery of athletes with anterior cruciate ligament injury: a systematic review. Scand J Med Sci Sports 2013;23:527–40. 10.1111/sms.12010 [DOI] [PubMed] [Google Scholar]
- 16. Bandura A. Self-Efficacy: toward a unifying theory of behavioral change. Advances in Behaviour Research and Therapy 1978;1:139–61. 10.1016/0146-6402(78)90002-4 [DOI] [Google Scholar]
- 17. Everhart JS, Best TM, Flanigan DC. Psychological predictors of anterior cruciate ligament reconstruction outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc 2015;23:752–62. 10.1007/s00167-013-2699-1 [DOI] [PubMed] [Google Scholar]
- 18. Bianco T, Eklund RC. Conceptual considerations for social support research in sport and exercise settings: the case of sport injury. J Sport Exerc Psychol 2001;23:85–107. 10.1123/jsep.23.2.85 [DOI] [Google Scholar]
- 19. Marmot M, Wilkinson R. Social determinants of health. 2nd Oxford: Oxford University Press, 2005. [Google Scholar]
- 20. Bianco T. Social support and recovery from sport injury: elite skiers share their experiences. Res Q Exerc Sport 2001;72:376–88. 10.1080/02701367.2001.10608974 [DOI] [PubMed] [Google Scholar]
- 21. Babatunde F, MacDermid J, MacIntyre N. Characteristics of therapeutic alliance in musculoskeletal physiotherapy and occupational therapy practice: a scoping review of the literature. BMC Health Serv Res 2017;17:375 10.1186/s12913-017-2311-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. World Health Organization Towards a common language for functioning, disability and health: the International classification of functioning, disability, and health, 2002. [Google Scholar]
- 23. Orhan C, Van Looveren E, Cagnie B, et al. . Are pain beliefs, cognitions, and behaviors influenced by race, ethnicity, and culture in patients with chronic musculoskeletal pain: a systematic review. Pain Physician 2018;21:541-558. [PubMed] [Google Scholar]
- 24. Main CJ, Foster N, Buchbinder R. How important are back pain beliefs and expectations for satisfactory recovery from back pain? Best Pract Res Clin Rheumatol 2010;24:205–17. 10.1016/j.berh.2009.12.012 [DOI] [PubMed] [Google Scholar]
- 25. Ardern CL, Glasgow P, Schneiders A, et al. . 2016 consensus statement on return to sport from the first world Congress in sports physical therapy, Bern. Br J Sports Med 2016;50:853–64. 10.1136/bjsports-2016-096278 [DOI] [PubMed] [Google Scholar]
- 26. Munn Z, Peters MDJ, Stern C, et al. . Systematic review or scoping review? guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol 2018;18:143 10.1186/s12874-018-0611-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Arksey H, O'Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 28. Joanna Briggs Institute reviewers’ manual Methodology for JBI scoping reviews In: The Joanna Briggs Institute, 2015. [Google Scholar]
- 29. Levac D, Colquhoun H, O'Brien KK. Scoping studies: advancing the methodology. Implement Sci 2010;5:69 10.1186/1748-5908-5-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Tricco AC, Lillie E, Zarin W, et al. . Prisma extension for scoping reviews (prisma-scr): checklist and explanation. Ann Intern Med 2018;169:467 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 31. Wiese-Bjornstal DM. Psychology and socioculture affect injury risk, response, and recovery in high-intensity athletes: a consensus statement. Scand J Med Sci Sports 2010;20:103–11. 10.1111/j.1600-0838.2010.01195.x [DOI] [PubMed] [Google Scholar]
- 32. Brewer B, Redmond, Charles JR. Psychology of sport injury rehabilitation. Champaign, IL: Human Kinetics, 2017. [Google Scholar]
- 33. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006;3:77–101. 10.1191/1478088706qp063oa [DOI] [Google Scholar]
- 34. Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med 1996;334:835–40. 10.1056/NEJM199603283341306 [DOI] [PubMed] [Google Scholar]
- 35. Hong QN, Fàbregues S, Bartlett G, et al. . The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Education for Information 2018;34:285–91. 10.3233/EFI-180221 [DOI] [Google Scholar]
- 36. Souto RQ, Khanassov V, Hong QN, et al. . Systematic mixed studies reviews: updating results on the reliability and efficiency of the mixed methods appraisal tool. Int J Nurs Stud 2015;52:500–1. 10.1016/j.ijnurstu.2014.08.010 [DOI] [PubMed] [Google Scholar]
- 37. Pace R, Pluye P, Bartlett G, et al. . Testing the reliability and efficiency of the pilot mixed methods appraisal tool (MMAT) for systematic mixed studies review. Int J Nurs Stud 2012;49:47–53. 10.1016/j.ijnurstu.2011.07.002 [DOI] [PubMed] [Google Scholar]
- 38. Mainwaring LM, Hutchison M, Bisschop SM, et al. . Emotional response to sport concussion compared to ACL injury. Brain Injury 2010;24:589–97. 10.3109/02699051003610508 [DOI] [PubMed] [Google Scholar]
- 39. Ardern CL, Taylor NF, Feller JA, et al. . Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med 2013;41:1549–58. 10.1177/0363546513489284 [DOI] [PubMed] [Google Scholar]
- 40. Baranoff J, Hanrahan SJ, Connor JP. The roles of acceptance and catastrophizing in rehabilitation following anterior cruciate ligament reconstruction. J Sci Med Sport 2015;18:250–4. 10.1016/j.jsams.2014.04.002 [DOI] [PubMed] [Google Scholar]
- 41. Brewer BW, Cornelius AE, Sklar JH, et al. . Pain and negative mood during rehabilitation after anterior cruciate ligament reconstruction: a daily process analysis. Scand J Med Sci Sports 2007;17:520–9. 10.1111/j.1600-0838.2006.00601.x [DOI] [PubMed] [Google Scholar]
- 42. Brewer BW, Cornelius AE, Van Raalte JL, et al. . Attributions for recovery and adherence to rehabilitation following anterior cruciate ligament reconstruction: a prospective analysis. Psychol Health 2000;15:283–91. 10.1080/08870440008400307 [DOI] [Google Scholar]
- 43. Brewer BW, Cornelius AE, Stephan Y, et al. . Self-protective changes in athletic identity following anterior cruciate ligament reconstruction. Psychol Sport Exerc 2010;11:1–5. 10.1016/j.psychsport.2009.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Brewer BW, Cornelius AE, Van Raalte JL, et al. . Predictors of adherence to home rehabilitation exercises following anterior cruciate ligament reconstruction. Rehabil Psychol 2013;58:64–72. 10.1037/a0031297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Brewer BW, Cornelius AE, Van Raalte JL, et al. . Adversarial growth after anterior cruciate ligament reconstruction. J Sport Exerc Psychol 2017;39:134–44. 10.1123/jsep.2016-0210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Chmielewski TL, Zeppieri G, Lentz TA, et al. . Longitudinal changes in psychosocial factors and their association with knee pain and function after anterior cruciate ligament reconstruction. Phys Ther 2011;91:1355–66. 10.2522/ptj.20100277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gignac MAM, Cao X, Ramanathan S, et al. . Perceived personal importance of exercise and fears of re-injury: a longitudinal study of psychological factors related to activity after anterior cruciate ligament reconstruction. BMC Sports Sci Med Rehabil 2015;7:4 10.1186/2052-1847-7-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Langford JL, Webster KE, Feller JA. A prospective longitudinal study to assess psychological changes following anterior cruciate ligament reconstruction surgery. Br J Sports Med 2009;43:377–8. 10.1136/bjsm.2007.044818 [DOI] [PubMed] [Google Scholar]
- 49. Lepley AS, Pietrosimone B, Cormier ML. Quadriceps function, knee pain, and self-reported outcomes in patients with anterior cruciate ligament reconstruction. J Athl Train 2018;53:337–46. 10.4085/1062-6050-245-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Masten R, Stražar K, Žilavec I, et al. . Psychological response of athletes to injury. Kinesiology 2014;46:127–34. [Google Scholar]
- 51. Morrey MA, Stuart MJ, Smith AM, et al. . A longitudinal examination of athletes' emotional and cognitive responses to anterior cruciate ligament injury. Clin J Sport Med 1999;9:63–9. 10.1097/00042752-199904000-00004 [DOI] [PubMed] [Google Scholar]
- 52. Niven A, Nevill A, Sayers F, et al. . Predictors of rehabilitation intention and behavior following anterior cruciate ligament surgery: an application of the theory of planned behavior. Scand J Med Sci Sports 2012;22:316–22. 10.1111/j.1600-0838.2010.01236.x [DOI] [PubMed] [Google Scholar]
- 53. Paterno MV, Flynn K, Thomas S, et al. . Self-Reported fear predicts functional performance and second ACL injury after ACL reconstruction and return to sport: a pilot study. Sports Health 2018;10:228–33. 10.1177/1941738117745806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Roessler KK, Andersen TE, Lohmander S, et al. . Motives for sports participation as predictions of self-reported outcomes after anterior cruciate ligament injury of the knee. Scand J Med Sci Sports 2015;25:435–40. 10.1111/sms.12249 [DOI] [PubMed] [Google Scholar]
- 55. Rosenberger PH, Jokl P, Cameron A, et al. . Shared decision making, preoperative expectations, and postoperative reality: differences in physician and patient predictions and ratings of knee surgery outcomes. Arthroscopy 2005;21:562–9. 10.1016/j.arthro.2005.02.022 [DOI] [PubMed] [Google Scholar]
- 56. Scherzer CB, Brewer BW, Cornelius AE, et al. . Psychological skills and adherence to rehabilitation after reconstruction of the anterior cruciate ligament. J Sport Rehabil 2001;10:165–72. 10.1123/jsr.10.3.165 [DOI] [Google Scholar]
- 57. Shapiro JL, Brewer BW, Cornelius AE, et al. . Patterns of emotional response to ACL reconstruction surgery. J Clin Sport Psychol 2017;11:169–80. 10.1123/jcsp.2016-0033 [DOI] [Google Scholar]
- 58. Sonesson S, Kvist J, Ardern C, et al. . Psychological factors are important to return to pre-injury sport activity after anterior cruciate ligament reconstruction: expect and motivate to satisfy. Knee Surg Sports Traumatol Arthrosc 2017;25:1375–84. 10.1007/s00167-016-4294-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Thomeé P, Währborg P, Börjesson M, et al. . Self-Efficacy, symptoms and physical activity in patients with an anterior cruciate ligament injury: a prospective study. Scand J Med Sci Sports 2007;17:238–45. 10.1111/j.1600-0838.2006.00557.x [DOI] [PubMed] [Google Scholar]
- 60. Thomeé P, Währborg P, Börjesson M, et al. . Self-efficacy of knee function as a pre-operative predictor of outcome 1 year after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthr 2008;16:118–27. 10.1007/s00167-007-0433-6 [DOI] [PubMed] [Google Scholar]
- 61. Lentz TA, Zeppieri G, George SZ, et al. . Comparison of physical impairment, functional, and psychosocial measures based on fear of reinjury/lack of confidence and return-to-sport status after ACL reconstruction. Am J Sports Med 2015;43:345–53. 10.1177/0363546514559707 [DOI] [PubMed] [Google Scholar]
- 62. Nwachukwu BU, Chang B, Voleti PB, et al. . Preoperative short form health survey score is predictive of return to play and minimal clinically important difference at a minimum 2-year follow-up after anterior cruciate ligament reconstruction. Am J Sports Med 2017;45:2784–90. 10.1177/0363546517714472 [DOI] [PubMed] [Google Scholar]
- 63. McAllister DR, Tsai AM, Dragoo JL, et al. . Knee function after anterior cruciate ligament injury in elite collegiate athletes. Am J Sports Med 2003;31:560–3. 10.1177/03635465030310041401 [DOI] [PubMed] [Google Scholar]
- 64. Ardern CL, Österberg A, Tagesson S, et al. . The impact of psychological readiness to return to sport and recreational activities after anterior cruciate ligament reconstruction. Br J Sports Med 2014;48:1613–9. 10.1136/bjsports-2014-093842 [DOI] [PubMed] [Google Scholar]
- 65. Ardern CL, Taylor NF, Feller JA, et al. . Fear of re-injury in people who have returned to sport following anterior cruciate ligament reconstruction surgery. J Sci Med Sport 2012;15:488–95. 10.1016/j.jsams.2012.03.015 [DOI] [PubMed] [Google Scholar]
- 66. Bennell KL, van Ginckel A, Kean CO, et al. . Patient knowledge and beliefs about knee osteoarthritis after anterior cruciate ligament injury and reconstruction. Arthritis Care Res 2016;68:1180–5. 10.1002/acr.22794 [DOI] [PubMed] [Google Scholar]
- 67. Brewer BW, Cornelius AE, Van Raalte JL, et al. . Age-Related differences in predictors of adherence to rehabilitation after anterior cruciate ligament reconstruction. J Athl Train 2003;38:158–62. [PMC free article] [PubMed] [Google Scholar]
- 68. Brewer BW, Cornelius AE, Van Raalte JL, et al. . Presurgical anxiety, concerns, and anticipated benefits associated with anterior cruciate ligament reconstruction. Hong Kong Journal of Sports Medicine & Sports Science 2002;15:1–8. [Google Scholar]
- 69. Chan DK, Lonsdale C, Ho PY, et al. . Patient motivation and adherence to postsurgery rehabilitation exercise recommendations: the influence of physiotherapists' autonomy-supportive behaviors. Arch Phys Med Rehabil 2009;90:1977–82. 10.1016/j.apmr.2009.05.024 [DOI] [PubMed] [Google Scholar]
- 70. Chan DK-C, Hagger MS, Spray CM. Treatment motivation for rehabilitation after a sport injury: application of the trans-contextual model. Psychol Sport Exerc 2011;12:83–92. 10.1016/j.psychsport.2010.08.005 [DOI] [Google Scholar]
- 71. Chmielewski TL, Jones D, Day T, et al. . The association of pain and fear of movement/reinjury with function during anterior cruciate ligament reconstruction rehabilitation. J Orthop Sports Phys Ther 2008;38:746–53. 10.2519/jospt.2008.2887 [DOI] [PubMed] [Google Scholar]
- 72. Feucht MJ, Cotic M, Saier T, et al. . Patient expectations of primary and revision anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2016;24:201–7. 10.1007/s00167-014-3364-z [DOI] [PubMed] [Google Scholar]
- 73. Flanigan DC, Everhart JS, Pedroza A, et al. . Fear of reinjury (kinesiophobia) and persistent knee symptoms are common factors for lack of return to sport after anterior cruciate ligament reconstruction. Arthroscopy 2013;29:1322–9. 10.1016/j.arthro.2013.05.015 [DOI] [PubMed] [Google Scholar]
- 74. George SZ, Lentz TA, Zeppieri G, et al. . Analysis of shortened versions of the Tampa scale for Kinesiophobia and pain Catastrophizing scale for patients after anterior cruciate ligament reconstruction. Clin J Pain 2012;28:73–80. 10.1097/AJP.0b013e31822363f4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Hart HF, Collins NJ, Ackland DC, et al. . Is impaired knee confidence related to worse kinesiophobia, symptoms, and physical function in people with knee osteoarthritis after anterior cruciate ligament reconstruction? J Sci Med Sport 2015;18:512–7. 10.1016/j.jsams.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 76. Kvist J, Ek A, Sporrstedt K, et al. . Fear of re-injury: a hindrance for returning to sports after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 2005;13:393–7. 10.1007/s00167-004-0591-8 [DOI] [PubMed] [Google Scholar]
- 77. Lam KC, Thomas SS, Valier ARS, et al. . Previous knee injury and health-related quality of life in collegiate athletes. J Athl Train 2017;52:534–40. 10.4085/1062-6050-50.5.01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Lentz TA, Zeppieri G, Tillman SM, et al. . Return to preinjury sports participation following anterior cruciate ligament reconstruction: contributions of demographic, knee impairment, and self-report measures. J Orthop Sports Phys Ther 2012;42:893–901. 10.2519/jospt.2012.4077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Mancuso CA, Sculco TP, Wickiewicz TL, et al. . Patients' expectations of knee surgery. J Bone Joint Surg Am 2001;83:1005–12. 10.2106/00004623-200107000-00005 [DOI] [PubMed] [Google Scholar]
- 80. McGuine TA, Winterstein A, Carr K, et al. . Changes in self-reported knee function and health-related quality of life after knee injury in female athletes. Clin J Sport Med 2012;22:334–40. 10.1097/JSM.0b013e318257a40b [DOI] [PubMed] [Google Scholar]
- 81. Thomeé P, Währborg P, Börjesson M, et al. . Determinants of self-efficacy in the rehabilitation of patients with anterior cruciate ligament injury. J Rehabil Med 2007;39:486–92. 10.2340/16501977-0079 [DOI] [PubMed] [Google Scholar]
- 82. Tripp DA, Stanish W, Ebel-Lam A, et al. . Fear of reinjury, negative affect, and catastrophizing predicting return to sport in recreational athletes with anterior cruciate ligament injuries at 1 year postsurgery. Sport Exerc Perform Psychol 2011;1:38–48. 10.1037/2157-3905.1.S.38 [DOI] [Google Scholar]
- 83. Udry E, Donald Shelbourne K, Gray T. Psychological readiness for anterior cruciate ligament surgery: describing and comparing the adolescent and adult experiences. J Athl Train 2003;38:167–71. [PMC free article] [PubMed] [Google Scholar]
- 84. Webster KE, Feller JA, Lambros C. Development and preliminary validation of a scale to measure the psychological impact of returning to sport following anterior cruciate ligament reconstruction surgery. Phys Ther Sport 2008;9:9–15. 10.1016/j.ptsp.2007.09.003 [DOI] [PubMed] [Google Scholar]
- 85. Ardern CL, Taylor NF, Feller JA, et al. . Sports participation 2 years after anterior cruciate ligament reconstruction in athletes who had not returned to sport at 1 year: a prospective follow-up of physical function and psychological factors in 122 athletes. Am J Sports Med 2015;43:848–56. 10.1177/0363546514563282 [DOI] [PubMed] [Google Scholar]
- 86. Mankad A, Gordon S, Wallman K. Psycholinguistic analysis of emotional disclosure: a case study in sport injury. J Clin Sport Psychol 2009;3:182–96. 10.1123/jcsp.3.2.182 [DOI] [Google Scholar]
- 87. Samuel RD, Tenenbaum G, Mangel E, et al. . Athletes’ experiences of severe injuries as a career-change event. J Sport Psychol Action 2015;6:99–120. 10.1080/21520704.2015.1012249 [DOI] [Google Scholar]
- 88. Tagesson S, Kvist J. Greater fear of re-injury and increased tibial translation in patients who later sustain an ACL graft rupture or a contralateral ACL rupture: a pilot study. J Sports Sci 2016;34:125–32. 10.1080/02640414.2015.1035668 [DOI] [PubMed] [Google Scholar]
- 89. Cupal DD, Brewer BW. Effects of relaxation and guided imagery on knee strength, reinjury anxiety, and pain following anterior cruciate ligament reconstruction. Rehabil Psychol 2001;46:28–43. 10.1037/0090-5550.46.1.28 [DOI] [Google Scholar]
- 90. Maddison R, Prapavessis H, Clatworthy M, et al. . Guided imagery to improve functional outcomes post-anterior cruciate ligament repair: randomized-controlled pilot trial. Scand J Med Sci Sports 2012;22:816–21. 10.1111/j.1600-0838.2011.01325.x [DOI] [PubMed] [Google Scholar]
- 91. Thomeé P, Währborg P, Börjesson M, et al. . A randomized, controlled study of a rehabilitation model to improve knee-function self-efficacy with ACL injury. J Sport Rehabil 2010;19:200–13. 10.1123/jsr.19.2.200 [DOI] [PubMed] [Google Scholar]
- 92. Carson F, Polman R. Experiences of professional rugby union players returning to competition following anterior cruciate ligament reconstruction. Physical Therapy in Sport 2012;13:35–40. 10.1016/j.ptsp.2010.10.007 [DOI] [PubMed] [Google Scholar]
- 93. Evans L, Hardy L. Injury rehabilitation: a qualitative follow-up study. Res Q Exerc Sport 2002;73:320–9. 10.1080/02701367.2002.10609026 [DOI] [PubMed] [Google Scholar]
- 94. Ezzat AM, Brussoni M, Whittaker JL, et al. . A qualitative investigation of the attitudes and beliefs about physical activity and post-traumatic osteoarthritis in young adults 3-10 years after an intra-articular knee injury. Phys Ther Sport 2018;32:98–108. 10.1016/j.ptsp.2018.05.001 [DOI] [PubMed] [Google Scholar]
- 95. Filbay SR, Crossley KM, Ackerman IN. Activity preferences, lifestyle modifications and re-injury fears influence longer-term quality of life in people with knee symptoms following anterior cruciate ligament reconstruction: a qualitative study. J Physiother 2016;62:103–10. 10.1016/j.jphys.2016.02.011 [DOI] [PubMed] [Google Scholar]
- 96. Ford UW, Gordon S. Coping with sport injury: resource loss and the role of social support. J Pers Interpers Los 1999;4:243–56. 10.1080/10811449908409733 [DOI] [Google Scholar]
- 97. Heijne A, Axelsson K, Werner S, et al. . Rehabilitation and recovery after anterior cruciate ligament reconstruction: patients' experiences. Scand J Med Sci Sports 2008;18:325–35. 10.1111/j.1600-0838.2007.00700.x [DOI] [PubMed] [Google Scholar]
- 98. Ivarsson A, Stambulova N, Johnson U. Injury as a career transition: experiences of a Swedish elite handball player. Int J Sport Exerc Psychol 2016;16:1–17. 10.1080/1612197X.2016.1242149 [DOI] [Google Scholar]
- 99. Johnson U, Ivarsson A, Karlsson J, et al. . Rehabilitation after first-time anterior cruciate ligament injury and reconstruction in female football players: a study of resilience factors. BMC Sports Sci Med Rehabil 2016;8:20 10.1186/s13102-016-0046-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Johnston LH, Carroll D. The context of emotional responses to athletic injury: a qualitative analysis. J Sport Rehabil 1998;7:206–20. 10.1123/jsr.7.3.206 [DOI] [Google Scholar]
- 101. Mainwaring LM. Restoration of self: a model for the psychological response of athletes to severe knee injuries. Can J Rehabil 1999;12:145–56. [Google Scholar]
- 102. Nordahl B, Sjöström R, Westin M, et al. . Experiences of returning to elite alpine skiing after ACL injury and ACL reconstruction. Int J Adolesc Med Health 2014;26:69–77. 10.1515/ijamh-2012-0114 [DOI] [PubMed] [Google Scholar]
- 103. Olofsson L, Fjellman-Wiklund A, Söderman K. From loss towards restoration: experiences from anterior cruciate ligament injury. Adv Physiother 2010;12:50–7. 10.3109/14038190903165120 [DOI] [Google Scholar]
- 104. Pizzari T, McBurney H, Taylor NF, et al. . Adherence to anterior cruciate ligament rehabilitation: a qualitative analysis. J Sport Rehabil 2002;11:90–102. 10.1123/jsr.11.2.90 [DOI] [Google Scholar]
- 105. Podlog L, Eklund RC. A longitudinal investigation of competitive athletes' return to sport following serious injury. J Appl Sport Psychol 2006;18:44–68. 10.1080/10413200500471319 [DOI] [Google Scholar]
- 106. Podlog L, Wadey R, Stark A, et al. . An adolescent perspective on injury recovery and the return to sport. Psychol Sport Exerc 2013;14:437–46. 10.1016/j.psychsport.2012.12.005 [DOI] [Google Scholar]
- 107. Ronkainen NJ, Ryba TV. Is hockey just a game? contesting meanings of the ice hockey life projects through a career-threatening injury. J Sports Sci 2017;35:923–8. 10.1080/02640414.2016.1201211 [DOI] [PubMed] [Google Scholar]
- 108. Scott SM, Perry MA, Sole G. “Not always a straight path”: patients’ perspectives following anterior cruciate ligament rupture and reconstruction. Disabil Rehabil 2018;40:2311–7. 10.1080/09638288.2017.1335803 [DOI] [PubMed] [Google Scholar]
- 109. Thing LF. "Voices of the broken body." The resumption of non-professional female players' sports careers after anterior cruciate ligament injury. The female player's dilemma: is she willing to run the risk? Scand J Med Sci Sports 2006;16:364–75. 10.1111/j.1600-0838.2005.00452.x [DOI] [PubMed] [Google Scholar]
- 110. Carson F, Polman RCJ. Acl injury rehabilitation: a psychological case study of a professional rugby Union player. J Clin Sport Psychol 2008;2:71–90. 10.1123/jcsp.2.1.71 [DOI] [Google Scholar]
- 111. Carson F, Polman RCJ. The facilitative nature of avoidance coping within sports injury rehabilitation. Scand J Med Sci Sports 2010;20:235–40. 10.1111/j.1600-0838.2009.00890.x [DOI] [PubMed] [Google Scholar]
- 112. Rock JA, Jones MV. A preliminary investigation into the use of counseling skills in support of rehabilitation from sport injury. J Sport Rehabil 2002;11:284–304. 10.1123/jsr.11.4.284 [DOI] [Google Scholar]
- 113. Ross CA, Clifford A, Louw QA. Factors informing fear of reinjury after anterior cruciate ligament reconstruction. Physiother Theory Pract 2017;33:103–14. 10.1080/09593985.2016.1271847 [DOI] [PubMed] [Google Scholar]
- 114. Tjong VK, Murnaghan ML, Nyhof-Young JM, et al. . A qualitative investigation of the decision to return to sport after anterior cruciate ligament reconstruction: to play or not to play. Am J Sports Med 2014;42:336–42. 10.1177/0363546513508762 [DOI] [PubMed] [Google Scholar]
- 115. Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol 2000;55:68–78. 10.1037/0003-066X.55.1.68 [DOI] [PubMed] [Google Scholar]
- 116. Podlog L, Dimmock J, Miller J. A review of return to sport concerns following injury rehabilitation: practitioner strategies for enhancing recovery outcomes. Phys Ther Sport 2011;12:36–42. 10.1016/j.ptsp.2010.07.005 [DOI] [PubMed] [Google Scholar]
- 117. Quinn AM, Fallon BJ. The changes in psychological characteristics and reactions of elite athletes from injury onset until full recovery. J Appl Sport Psychol 1999;11:210–29. 10.1080/10413209908404201 [DOI] [Google Scholar]
- 118. Johnston LH, Carroll D. The provision of social support to injured athletes: a qualitative analysis. J Sport Rehabil 1998;7:267–84. 10.1123/jsr.7.4.267 [DOI] [Google Scholar]
- 119. Werbrouck A, Swinnen E, Kerckhofs E, et al. . How to empower patients? A systematic review and meta-analysis. Transl Behav Med 2018;8:660–74. 10.1093/tbm/iby064 [DOI] [PubMed] [Google Scholar]
- 120. Bright FAS, Kayes NM, Worrall L, et al. . A conceptual review of engagement in healthcare and rehabilitation. Disabil Rehabil 2015;37:643–54. 10.3109/09638288.2014.933899 [DOI] [PubMed] [Google Scholar]
- 121. Miciak M, Mayan M, Brown C, et al. . The necessary conditions of engagement for the therapeutic relationship in physiotherapy: an interpretive description study. Arch Physiother 2018;8:3 10.1186/s40945-018-0044-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Légaré F, Ratté S, Stacey D, et al. . Interventions for improving the adoption of shared decision making by healthcare professionals. Cochrane Database Syst Rev 2010;5:CD006732 10.1002/14651858.CD006732.pub2 [DOI] [PubMed] [Google Scholar]
- 123. Kinney M, Seider J, Beaty AF, et al. . The impact of therapeutic alliance in physical therapy for chronic musculoskeletal pain: a systematic review of the literature. Physiother Theory Pract 2018;6:1–13. 10.1080/09593985.2018.1516015 [DOI] [PubMed] [Google Scholar]
- 124. Wiggins AJ, Grandhi RK, Schneider DK, et al. . Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 2016;44:1861–76. 10.1177/0363546515621554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Légaré F, Thompson-Leduc P. Twelve myths about shared decision making. Patient Educ Couns 2014;96:281–6. 10.1016/j.pec.2014.06.014 [DOI] [PubMed] [Google Scholar]
- 126. Bastemeijer CM, Voogt L, van Ewijk JP, et al. . What do patient values and preferences mean? A taxonomy based on a systematic review of qualitative papers. Patient Educ Couns 2017;100:871–81. 10.1016/j.pec.2016.12.019 [DOI] [PubMed] [Google Scholar]
- 127. Carroll LJ, Lis A, Weiser S, et al. . How well do you expect to recover, and what does recovery mean, anyway? qualitative study of expectations after a musculoskeletal injury. Phys Ther 2016;96:797–807. 10.2522/ptj.20150229 [DOI] [PubMed] [Google Scholar]
- 128. Neely K, Holt N. Positive youth development through sport: a review 2011;2:299–316. [Google Scholar]
- 129. Fuller CW, Molloy MG, Bagate C, et al. . Consensus statement on injury definitions and data collection procedures for studies of injuries in rugby Union. Br J Sports Med 2007;41:328–31. 10.1136/bjsm.2006.033282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130. Swann C, Moran A, Piggott D. Defining elite athletes: issues in the study of expert performance in sport psychology. Psychol Sport Exerc 2015;16:3–14. 10.1016/j.psychsport.2014.07.004 [DOI] [Google Scholar]
- 131. Walker N, Thatcher J, Lavallee D. A preliminary development of the Re-Injury anxiety inventory (RIAI). Phys Ther Sport 2010;11:23–9. 10.1016/j.ptsp.2009.09.003 [DOI] [PubMed] [Google Scholar]
- 132. Vealey RS, Chase MA. Advances in sport psychology : Self-confidence in sport. 3rd edn Champaign, IL, US: Human Kinetics, 2008: 430–5. [Google Scholar]
- 133. Lazarus R, Folkman S. Stress, appraisal, and coping. New York: Springer Pub. Co, 1984. [Google Scholar]
- 134. Stryker S, Burke PJ. The past, present, and future of an identity theory. Soc Psychol Q 2000;63:284–97. 10.2307/2695840 [DOI] [Google Scholar]
- 135. Fletcher D, Sarkar M. Mental fortitude training: an evidence-based approach to developing psychological resilience for sustained success. J Sport Psychol Action 2016;7:135–57. 10.1080/21520704.2016.1255496 [DOI] [Google Scholar]
- 136. Smith AD. Perception and belief. Philos Phenomenol Res 2001;62:283–309. 10.1111/j.1933-1592.2001.tb00057.x [DOI] [Google Scholar]
- 137. Rees T, Hardy L, Evans L. Construct validity of the social support survey in sport. Psychol Sport Exerc 2007;8:355–68. 10.1016/j.psychsport.2006.06.005 [DOI] [Google Scholar]
- 138. Bordin ES. The generalizability of the psychoanalytic concept of the working alliance. Psychotherapy: Theory, Research & Practice 1979;16:252–60. 10.1037/h0085885 [DOI] [Google Scholar]
- 139. Richardson SOA, B; Morris M. T Overtraining athletes: personal journeys in sport. Champaign, IL: Human Kinetics, 2008. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bjsports-2019-101206supp001.pdf (349.8KB, pdf)