Abstract
The COVID-19 pandemic has disproportionately impacted the well-being of vulnerable populations in the US, including Black people. The impact on pregnant women is of special concern for the intrauterine and post-natal development of their offspring. We evaluated in an online survey a sample of 913 pregnant women, 216 Black, 571 White, 126 Other, during a 2-week stay-at-home mandate in the Philadelphia region. We applied logistic regression models and analysis of covariance to examine general and pregnancy-specific worries and negative consequences arising from the COVID-19 pandemic, symptoms of anxiety and depression, and resilience. Black pregnant women reported greater likelihood of having their employment negatively impacted, more concerns about a lasting economic burden, and more worries about their prenatal care, birth experience, and post-natal needs. In the full sample, 11.1% of women met screening criteria for anxiety and 9.9% met criteria for depression. Black women were more likely to meet criteria for depression than White women, but this difference was not significant accounting for covariates. Resilience factors including self-reliance and emotion regulation were higher in Black women. Racial disparities related to COVID-19 in pregnant women can advance the understanding of pregnancy related stressors and improve early identification of mental health needs.
Keywords: Racial disparity; Pregnancy; Stress, Anxiety; Depression; Resilience; COVID-19
1. Introduction
The COVID-19 pandemic is having colossal impact on global health and well-being. In the United States, Black communities are disproportionally affected by the pandemic, including higher mortality rates (Cyrus et al., 2020; Millett et al., 2020). The burden of COVID-19 is also impacting mental health, with increases in symptoms of anxiety and depression (Sønderskov et al., 2020; Vindegaard and Benros, 2020), particularly among women, who are overall more susceptible to these conditions (Altemus et al., 2014; Rubinow and Schmidt, 2019). There is an urgent need to examine mental health consequences of the COVID-19 pandemic in disenfranchised populations and to address them early.
Pregnant women are at heightened risk for depression and anxiety following adversity (Biaggi et al., 2016; Vesga-López et al., 2008), and are thus particularly at risk for adverse emotional health impacts from the COVID-19 pandemic. Several recent reports highlight the impact of the pandemic on pregnancy, including a study detailing clinical characteristics and pregnancy outcomes from a small sample from China (Yan et al., 2020), and a set of recommended guidelines for obstetricians (Dashraath et al., 2020; Rasmussen et al., 2020). Data from a Canadian population-based survey also suggest elevated psychological distress in pregnant women (Lebel et al., 2020). The heightened vulnerability of pregnant women to stressors, including pandemic-related stress, is of special concern due to the potential long-term adverse effects on the intrauterine environment, which directly influences fetal development (Bale et al., 2010; Van den Bergh et al., 2017).
Notably, in non-pandemic times, racial disparities were evident in pregnancy outcomes. For decades, Black women have experienced higher rates of preterm birth and maternal morbidity and mortality than White women (Grobman et al., 2018; Menon et al., 2011). Black women are also more susceptible to anxiety and depression during the prenatal period (Melville et al., 2010; Orr et al., 2006; Rich-Edwards et al., 2006). Despite these findings, there is a paucity of work examining racial disparities in the mental health and birth outcomes of Black women. This extant evidence coupled with the well-documented long term effects of prenatal stress, anxiety, and depression on women and their offspring (Dunkel Schetter and Tanner, 2012; Van den Bergh et al., 2017) underscores the urgent need for research on the current and long-term impact of the COVID-19 pandemic during pregnancy among Black women.
Our understanding of the short- and long-term effects of the pandemic on pregnant women and their offspring can also be advanced by exploring resilience, the capacity of individuals to cope with difficult and stressful situations (Feldman, 2020; Rutter, 2006; Ungar and Theron, 2020). Recent advances in the assessment of resilience include a brief, validated battery that measures multiple parameters of resilience in large-scale studies (Moore et al., 2020). For example, in an online survey of adults (n=3,042) recruited through crowdsourcing, resilience was conceptualized via factors of self-reliance, emotion-regulation, interpersonal-relationship patterns, and the neighborhood-environment. More COVID-19 worries were associated with higher rates of depression and anxiety, particularly among women. Greater resilience was associated with lower COVID-19 related worries (Barzilay et al., 2020). However, resilience has yet to be investigated among pregnant women, knowledge of which could inform targets for intervention to mitigate lasting negative sequalae arising from the pandemic.
In the present study, we evaluated a diverse sample of pregnant women at the height of the stay-at-home lockdown to prevent community transmission of COVID-19. We examined race-related differences in experience of and risk of exposure to COVID-19 (e.g., job loss, infection status, knowing people who had died), the burden arising from the COVID-19 pandemic (i.e., both general and pregnancy-specific worries), rates of anxiety and depression, and resilience factors that might mitigate burden of COVID-19. We hypothesized that: 1. Black women, compared to White women, would report: a) Greater concerns of exposure risk; b) More worries about personal impact of COVID-19; c) More pregnancy-related worries. 2. a) Across the sample, there will be increased incidence of anxiety and depression; b) Black women will have increased incidence of anxiety and depression. 3. Higher resilience will be associated with: a) Lower levels of general and pregnancy-related worries; b) Reduced incidence of anxiety and depression; c) Race differences in resilience may relate to worries, anxiety and depression.
2. Methods
2.1. Participants
Data were collected between April 17, 2020 and May 1, 2020, when Philadelphia and neighboring communities were under a statewide stay-at-home order and the community spread of COVID-19 was high in the region. A total of 3,548 women were identified through Penn Medicine medical records system as being pregnant and receiving care. Women were initially contacted through email to participate in the current online study. Across the two-week period, additional recruitment efforts (i.e., phone call, text, and/or email) were conducted for a portion of these women. Supplemental Figure 1 presents a flow-chart of sample accrual.
Of the 3,548 women who received any form of contact, a total of 913 women age ≥ 18 years completed the survey; 78 completed partial study procedures, but did not finish the survey by the end of the two week period; 326 declined participation, 151 were identified as no longer pregnant, and the remaining 2,080 women were either being actively recruited and/or could not be reached by the end of recruitment date. Table 1 (see also Table S2) presents demographics of participants obtained from electronic medical records. Compared to White (Non-Hispanic/Latina) women, Black women were significantly younger and more likely to come from lower socioeconomic status (SES) neighborhoods, be insured through Medicaid, be single, and have another child (parity>0). The two groups did not differ on gestational age at the time of survey completion. Across the whole sample, 70 (8.9%) were in the first trimester of pregnancy, 280 (35.6%) in the second trimester, and 437 (55.5%) in the third trimester. The women who completed the survey differed in race, gestational age, insurance type, marital status, and parity from those who did not complete or take part the survey (see Supplemental Material Table S1).
Table 1.
Demographics of the total sample and split by race
| Total Sample (N=787) | Black (n=216; 27.4%) | White-Non Latina/Hispanic (n=571; 72.6%) | |||
|---|---|---|---|---|---|
| Range | M (SD) | M (SD) | M (SD) | t-test | |
| Maternal Age (years) | 18.21-46.31 | 32.45(4.83) | 29.34(5.80) | 33.63(3.80) | t(785)=10.07, p<.001 |
| Gestational Age (weeks) | 7.14-40.57 | 24.86(8.35) | 25.16(8.10) | 24.74 (8.44) | t(785)=-0.63, p=.53 |
| SES | -2.53-2.39 | 0.00(1.00) | -0.91(.82) | 0.35(.82) | t(785)=19.35, p<.001 |
| Percent | Percent | Percent | Chi-Square | ||
| Private Insurance | 79.8% | 35.2% | 96.7% | χ2(1)=367.52, p<.001 | |
| Married/Living w/ Partner | 75.2% | 29.2% | 92.6% | χ2(1)=338.81, p<.001 | |
| Parity (First Pregnancy) | 54.5% | 38.0% | 60.8% | χ2(1)=32.88, p<.001 | |
SES was a z-score composite scale ranging from -2.53 to 2.39 with higher values indicating higher neighborhood SES (higher percent of residence in poverty, lower percent of residents married and residence with at least a high school education, lower median family income).
2.2. Study procedures
After providing online consent, participants completed an online REDCap-based survey to assess their COVID-19 related worries, anxiety and depression, and several resilience factors. After completing questionnaires about resilience, anxiety (Generalized Anxiety Disorder 7 questionnaire - GAD-7, Spitzer et al., 2006) and depression (Patient Health Questionnaire 2 - PHQ-2, Arroll et al., 2010), participants received personal feedback and recommendations. Feedback and recommendations were developed by a team of psychiatrists and psychologists (Barzilay et al., 2020). The study was approved by the Institutional Review Board of the University of Pennsylvania.
2.3. Measures
The measures selected were based on the literature and our previous study of risk and resilience (Moore et al., 2020), which we adapted for use in online surveys during COVID-19 (Barzilay et al., 2020). We leveraged other brief validated measures and scales associated with stress that could be applied online during the pandemic.
COVID-19 Exposure and Worries. Participants answered 5 questions about exposure to and consequences of COVID-19, including whether they had been tested, experienced symptoms, knew someone who tested positive, knew someone who died, and whether their job was impacted (see Table 2 ). Items were rated on a 5-point Likert scale (1=not at all, 5=great deal). Participants could select “I prefer not to say” or “I don't know”. For the getting tested item, “positive” and “negative” test results and “awaiting results” were collapsed in analyses (only 8 women reported testing positive, while 1 was awaiting test results). For the question about whether their job was negatively affected, responses of “lost job”, “reduced hours” and “reduced pay” were collapsed for analyses. Participants also reported their level of worry for 6 general worries about the COVID-19 pandemic (e.g., getting the virus, family getting the virus; α=.84) and 4 pregnancy-specific worries about COVID-19 (e.g., birthing experience being impacted; α=.82) (see Table 2 for list of items).
Table 2.
Descriptive statistics for COVID-19 Risk Exposure, General and Pregnancy Specific Worries in the total sample and split by race (Black/White)
| Total Sample (N=787) | Black (n=216; 27.4%) | White-Non Latina/Hispanic (n=571; 72.6%) | Race difference: Tests without covariates | Race difference: Tests with covariates | |
|---|---|---|---|---|---|
| COVID-19 Related Stress Exposures | % | % | % | Chi-Square | Binary Logistic Regression |
| Tested | 4.6% | 5.6% | 4.2% | χ2(1)=0.66, p=.418 | Wald χ2(1)=.18, p=.672 |
| Experienced symptoms they feel could be attributable to COVID-19 | 11.2% | 6.5% | 13.0% | χ2(1)=6.62, p=.010 | Wald χ2(1)=6.64, p=.010 |
| Know Someone Who Tested Positive | 44.1% | 37.0% | 46.8% | χ2(1)=6.01, p=.014 | Wald χ2(1)=.11, p=.737 |
| Know Someone Who Died | 9.5% | 13.4% | 8.1% | χ2(1)=5.24, p=.022 | Wald χ2(1)=3.60, p=.058 |
| Job Negatively Affecteda | 26.0% | 40.7% | 20.5% | χ2(1)=33.36, p<.001 | Wald χ2(1)=8.56, p=.003 |
| General COVID-19 Worries (range 1-5)b | M (SD) | M (SD) | M (SD) | t-test | |
| Family Getting COVID-19 | 3.51 (1.12) | 3.16 (1.40) | 3.65(.96) | t(785)=4.77, p<.001 | F(1,780)=8.34, p=.004 |
| Self Getting COVID-19 | 3.06 (1.09) | 2.88(1.34) | 3.12(.97) | t(785)=2.36, p=.019 | F(1,780)=2.20, p=.138 |
| Unknowingly Infecting Others | 2.91 (1.24) | 2.68(1.52) | 2.99(1.10) | t(785)=2.77, p=.006 | F(1,780)=3.98, p=.046 |
| Financial Burden of Pandemic | 2.67(1.35) | 3.09(1.54) | 2.51(1.23) | t(785)=-4.93, p<.001 | F(1,780)=4.37, p=.037 |
| Dying From COVID-19 | 2.24 (1.19) | 2.50 (1.47) | 2.14(1.06) | t(785)=-3.23, p=.001 | F(1,780)=0.88, p=.348 |
| Currently Having COVID-19 | 1.99 (1.11) | 2.16(1.44) | 1.92(.95) | t(785)=-2.28, p=.023 | F(1,780)=0.30, p=.587 |
| Pregnancy-Related COVID-19 Worries (range 1-5)b | M(SD) | M (SD) | M (SD) | t-test | |
| Having a Good Birthing Experience Because of the Pandemic | 3.84 (1.12) | 4.12(1.15) | 3.73(1.09) | t(785)=-4.40, p<.001 | F(1,780)=3.99, p=.046 |
| Receiving Good Prenatal Care Because of the Pandemic | 2.97 (1.26) | 3.46(1.41) | 2.79(1.15) | t(785)=-6.24, p<.001 | F(1,780)=5.84, p=.016 |
| Exposure During Prenatal Care Visits During the Pandemic | 2.92 (1.23) | 3.19(1.44) | 2.82(1.13) | t(785)=-3.34, p=.001 | F(1,780)=2.34, p=.127 |
| Access to Food, Meds, Baby Care Items During the Pandemic | 2.59 (1.22) | 3.03(1.44) | 2.42(1.07) | t(785)=-5.64, p<.001 | F(1,780)=7.03, p=.008 |
| Psychiatric Symptoms (% meeting Screening threshold)c | % | % | % | Chi-Square | Binary Logistic Regression |
| Anxiety | 11.8% | 13.9% | 11.0% | χ2(1)=1.23, p=.268 | Wald χ2=3.41, p=.065 |
| Depression | 10.2% | 16.2% | 7.9% | χ2(1)=11.89, p=.001 | Wald χ2=1.75, p=.185 |
Covariates in the statistics reported in the far right column are maternal age, gestational age, SES, marital status (married or living with partner vs. not), and parity (0 vs. ≧1). aJob negatively affected includes women who reported loss of job or reduction in pay or reduction in hours. b A Likert scale ranging from 1 (not at all) to 5 (a great deal) was used to assess level of worry for general COVID-19 worries and pregnancy-specific COVID-19 worries. cA screening threshold of 11 was used for GAD-7 to identify positive anxiety screens and a threshold of 3 was used on PHQ-2 to identify positive depression screens.
Anxiety and Depression. Anxiety and depression were assessed using the GAD-7 (α=.91) and PHQ-2 (α=.83). A clinical screening threshold of 11 (Mossman et al., 2017) was used for the GAD-7 and a threshold of 3 (Carey et al., 2016) was used for the PHQ-2 (see Supplemental Materials for analyses using lower thresholds).
Resilience. Participants completed a 21-item resilience questionnaire that included 5 previously-validated factors of self-reliance (3 items; α=.78), emotion regulation (5 items; α=.88), supportive close relationships (4 items; α=.70), non-hostile close relationships (5 items; α=.78), and perceived neighborhood safety (4 items; α=.91), derived from prior research (Moore et al., 2020; Barzilay et al., 2020). The emotion regulation and non-hostile relationship factors were reversed scored for the current study to indicate the presence of resilience (i.e., factors from the original study were Emotion Dysregulation and the presence of Negative Relationships).
Other measures. SES was measured using census-based geocoding for neighborhood-based variables (e.g. median household income), obtained using participant zip codes (Moore et al., 2016). Gestational and maternal age, medical insurance, marital status, and parity were all obtained through electronic health records.
2.3. Analytic Strategy
To test study hypotheses about the disproportionate negative burden of the pandemic on Black women, we focused our main analyses on comparisons between Black women and White, non-Hispanic/non-Latina women. The full original sample included 126 women from other racial/ethnic groups. While sample sizes for these other racial/ethnic groups preclude formal analytic comparisons, we report descriptive statistics for all study variables (see Supplemental Tables S.2-S.4).
We tested hypothesis 1a, using chi-square tests to establish whether risk exposure differed by race (Black vs. White). To control for possible confounds, we also conducted logistic regression models, testing for differences in risk exposure by race after controlling for age, gestational age, SES, marital status and parity. Hypotheses 1b and 1c were evaluated with separate repeated measures (RM) ANCOVA. The six general COVID-19 worries were entered as dependent variables for RM-ANCOVA (1b), and the four pregnancy specific worries were entered as dependent variables in the second RM-ANCOVA (1c). In both models race was entered as a between-group factor and covariates were those listed above. To test hypothesis 2a, we used logistic regression models with anxiety (GAD-7>10) and depression (PHQ-2>2), as dependent variables; race was entered as a between-group factor and covariates were included as described above. For hypothesis 2b, we ran similar logistic regressions with the addition of a z-scored total general COVID-19 worry score and total pregnancy-specific worry score entered at step 2 of the model to assess the association between worries and anxiety/depression. Interactions between race and each worry score were entered into step 3 of the model to test for differences in how worry predicted anxiety and depression differentially across race. To evaluate hypothesis 3 concerning the resilience parameters, we first evaluated possible race difference in resilience factors using a RM-ANCOVA with the five resilience factors (self-reliance, emotion regulation, positive relationships, absence of negative relationships, and perceived neighborhood safety) as the dependent variable and race as a between-subjects factor, with covariates as described above. Hypothesis 3a was tested using linear regression to test relationships between resilience factors and reported worries. We included covariates and tested for moderation by race by including interaction terms between race (3c) with each of the mean-centered resilience factors. For hypothesis 3b we used binomial logistic regression to test the relationship between resilience factors and anxiety and depression. As before, we included covariates and tested for moderation by race (3c) by including interaction terms between race and each of the mean-centered resilience factors.
3. Results
3.1. Exposure risk
COVID-19 risk exposures are reported in Table 2 (also see Table S3). Hypothesis 1 was generally supported. Black women were more likely to have their jobs negatively impacted by the pandemic (i.e., job loss or decreased pay), after controlling for covariates (Table 2; Table S4). Black women reported knowing more people who had died from COVID-19 compared to White women, although this difference was no longer significant after accounting for covariates (Table 2; Table S4). While White women were more likely to report having experienced symptoms that they attributed to COVID-19 and know more people who tested positive than Black women, the former was only significant after controlling for covariates.
3.2. General and pregnancy worries
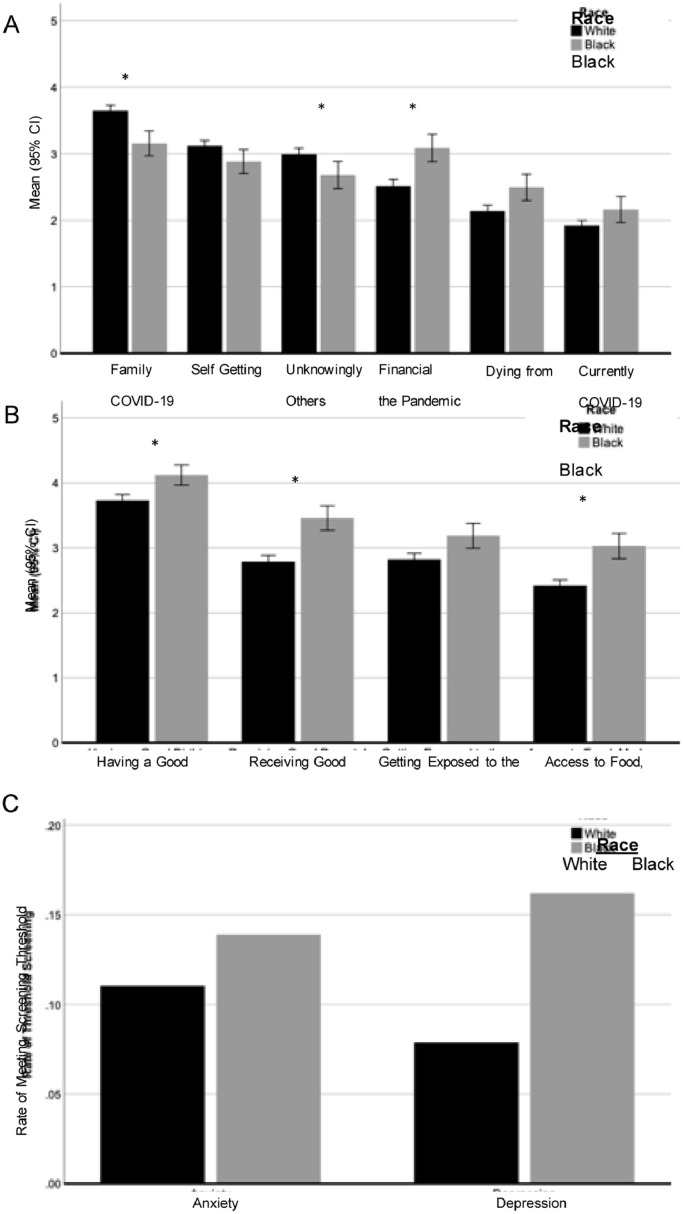
Table 2 presents descriptive statistics and race-related differences in COVID-worries (general and pregnancy-specific) and psychiatric screeners (anxiety and depression) (Figure 1 ). Supporting hypothesis 1b, regarding personal impact of COVID-19, after accounting for covariates, there were race differences in some general COVID-19 worries. Black women reported more worry about the financial burden of the pandemic while White women worried more about unknowingly infecting others and about family members getting COVID-19. Black and White women reported similar rates of worry about currently having, getting, or dying from COVID-19. For the pregnancy-specific worries (hypothesis 1c), after accounting for covariates, Black women reported higher levels of worry about their birth experience, receiving good prenatal care, and access to food, medication, and baby care items in the postnatal period. Black and White women reported similar rates of worry about getting exposed to the COVID-19 virus during prenatal visits. There were main effects of maternal age and gestational age, with younger women and women further along in pregnancy reporting more pregnancy-specific worries (Table S6).
Figure 1.
Psychological Burden of the Pandemic in Pregnant Women by Race
Level of reported worry for general pandemic items (Panel A) and pregnancy-specific pandemic related worries (panel B) are plotted by race. Panel B shows rates of anxiety (GAD-7>10) and depression (PHQ-2>2) by race. Significant Effects are indicated for effects after controlling for SES, maternal age, gestational age, marital status and parity.
3.3. Anxiety and Depression
Across the full sample, 11.1% met criteria for anxiety and 9.9% met criteria for depression. Black women were more likely to meet criteria for depression than White women, though this difference was not significant after accounting for covariates (hypothesis 2b,Table 2). Notably, applying less conservative screening thresholds, Black women had significantly higher rates of anxiety and depression after accounting for covariates (see Supplemental Tables S2-S4). Younger women were more likely to meet criteria for both anxiety and depression. Women with prior births (parity>0) were more likely to meet criteria for anxiety and single women were more likely to meet criteria for depression (Table S7). Women with more general COVID-19 and pregnancy worries were more likely to meet screening threshold for anxiety; only pregnancy specific worries predicted depression screening status. No interactions between worry and race emerged when predicting anxiety or depression status (hypothesis 2b,Table 3 ; Table S.8).
Table 3.
Regression analyses testing whether COVID worries (general and pregnancy-specific) are independently related to anxiety and depression screening status
| Positive Anxiety Screening | Positive Depression Screening | |||||||
|---|---|---|---|---|---|---|---|---|
| Wald | OR | 95% CI | Wald | OR | 95% CI | |||
| Step 1 - Covariates | ||||||||
| Race | 3.41 | 2.04 | .96 | 4.33 | 1.75 | 1.72 | .77 | 3.81 |
| SES | 1.96 | .83 | .63 | 1.08 | .38 | .91 | .68 | 1.22 |
| Maternal age | 5.72* | .93 | .88 | .99 | 6.20⁎⁎ | .93 | .88 | .98 |
| Gestational Age | 3.12 | 1.02 | 1.00 | 1.05 | 1.12 | .98 | .96 | 1.01 |
| Married/living with partner | 1.49 | 1.53 | .77 | 3.02 | 10.43⁎⁎⁎ | 3.14 | 1.57 | 6.28 |
| Parity | 5.78* | 1.81 | 1.12 | 2.93 | 3.64 | 1.67 | .99 | 2.82 |
| Step 2- Main effects (Worries) | ||||||||
| General COVID-19 Worries | 9.81⁎⁎ | 1.57 | 1.18 | 2.08 | .17 | 1.06 | .80 | 1.40 |
| Pregnancy-Specific COVID-19 Worries | 25.23⁎⁎⁎ | 2.28 | 1.65 | 3.14 | 17.36⁎⁎⁎ | 1.99 | 1.44 | 2.76 |
| Step 3 - Interactions with race | ||||||||
| General COVID-19 Worries x race | 1.67 | .69 | .40 | 1.21 | .05 | .94 | .53 | 1.66 |
| Pregnancy-Specific COVID-19 Worries x race | .46 | 1.29 | .62 | 2.67 | .27 | .84 | .44 | 1.62 |
p ≤ .05,
p ≤ .01,
p ≤ .001. A total General COVID-19 Worries score was created by summing the six general worry items; a total Pregnancy-Specific COVID-19 Worries was created by summing the four pregnancy specific worry items. Significant results are bolded. Race was coded 1=White, 2=Black
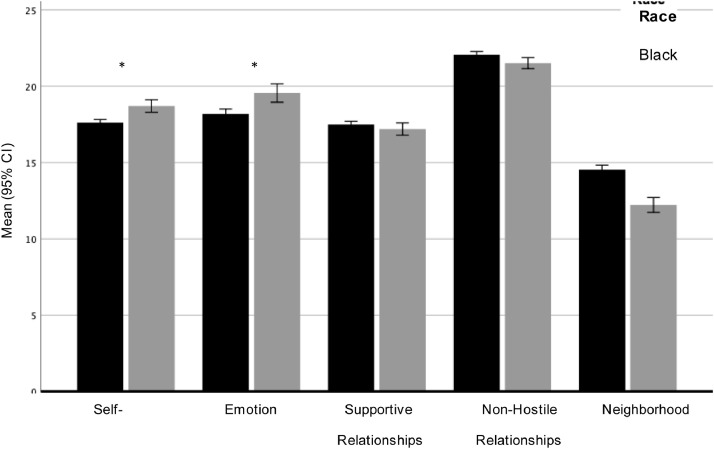
3.4. Resilience
First, we examined descriptive statistics for the five resilience factors (Table S9). Black women reported more self-reliance and better emotion regulation than White women, controlling for covariates (Table S10, Figure 2 ). White women reported having less hostility in their close relationships and greater perceived neighborhood safety than Black women, but these differences were not statistically significant after controlling for covariates.
Figure 2.
Race Differences in Resilience During the Pandemic in Pregnant Women
Footnote: Resilience scores by race. Significance is indicated for effects after controlling for SES, maternal age, gestational age, marital status and parity.
Second, using linear regression models, we tested whether resilience was related to total general and total pregnancy-specific COVID-19 worries, and whether race moderated these associations. There was evidence for some differential associations between resilience and general versus total pregnancy worries (hypothesis 3a). Higher emotion regulation and greater perceived neighborhood safety were independently related to fewer general COVID-19 worries (Table 4 ), while higher emotion regulation and less hostility in close relationships were independently related to fewer pregnancy specific worries. Having higher self-reliance was also related to more pregnancy-specific COVID-19 worries. None of these associations was moderated by race (hypothesis 3c).
Table 4.
Regression models testing whether different resilience factors are independently related worries, anxiety and depression and whether associations are moderated by race
| Total general COVID-19 worries | Total pregnancy-specific COVID-19 worries | Positive Anxiety Screening | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | B | SE | β | Wald | OR | 95% CI | Wald | OR | 95% CI | |||
| Step 1 - Covariates | ||||||||||||||
| Race | .37 | .62 | .03 | 1.62⁎⁎⁎ | .44 | .19 | .27 | .80 | .35 | 1.85 | .00 | .99 | .42 | 2.37 |
| SES | .51* | .25 | .10 | .06 | .18 | .02 | .46 | .89 | .64 | 1.25 | .20 | .92 | .64 | 1.32 |
| Maternal age | -.06 | .05 | -.05 | -.11⁎⁎ | .03 | -.14 | 6.32* | .92 | .87 | .98 | 6.75⁎⁎⁎ | .92 | .86 | .98 |
| Gestational Age | -.001 | .02 | -.001 | .04⁎⁎ | .02 | .09 | 2.23 | 1.02 | .99 | 1.05 | 3.53 | .97 | .94 | 1.00 |
| Married/living with partner | -.28 | .57 | -.02 | -.20 | .40 | -.02 | .12 | .88 | .41 | 1.88 | 6.70* | .37 | .17 | .78 |
| Parity | -.34 | .40 | -.03 | .13 | .28 | .02 | 4.43⁎⁎ | .56 | .33 | .96 | 1.60 | .69 | .39 | 1.23 |
| Step 2- Main effects (resilience factors) | ||||||||||||||
| Self-reliance | .09 | .07 | .05 | .11* | .05 | .08 | 4.92* | .91 | .83 | .99 | 3.83 | .91 | .83 | 1.00 |
| Emotion regulation | -.40⁎⁎⁎ | .05 | -.31 | -.28⁎⁎⁎ | .04 | -.29 | 54.03⁎⁎⁎ | .79 | .74 | .84 | 43.73⁎⁎⁎ | .80 | .75 | .86 |
| Supportive relationships | .00 | .07 | -.002 | -.01 | .05 | -.004 | .95 | 1.05 | .95 | 1.15 | .45 | 1.04 | .94 | 1.15 |
| Non-Hostile relationships | -.13 | .08 | -.06 | -.15⁎⁎ | .05 | -.09 | 1.26 | .95 | .86 | 1.04 | 7.37⁎⁎ | .87 | .79 | .96 |
| Perceived neighborhood safety | -.12* | .06 | -.09 | -.03 | .04 | -.03 | 1.85 | .95 | .87 | 1.03 | .10 | .99 | .90 | 1.08 |
| Step 3 - Interactions with race | ||||||||||||||
| Self-reliance x race | .02 | .15 | .01 | -.001 | .11 | .00 | 3.72 | 1.21 | 1.00 | 1.47 | 5.18* | 1.26 | 1.03 | 1.54 |
| Emotion regulation x race | -.18 | .10 | -.08 | .08 | .07 | .05 | .80 | .94 | .83 | 1.08 | 1.73 | .91 | .80 | 1.05 |
| Supportive relationships x race | -.29 | .15 | -.09 | -.06 | .11 | -.03 | .38 | .94 | .78 | 1.14 | .90 | 1.11 | .90 | 1.36 |
| Non-hostile relationships x race | -.25 | .16 | -.07 | -.06 | .12 | -.02 | .26 | 1.06 | .86 | 1.30 | .24 | 1.05 | .86 | 1.29 |
| Neighborhood safety x race | -.01 | .11 | -.004 | -.08 | .08 | -.04 | 3.01 | .87 | .74 | 1.02 | 1.37 | .91 | .77 | 1.07 |
B=Unstandardized beta coefficients; SE=Standard error; β=Standardized beta; OR=odds ratio; CI=confidence interval; Race was coded 1=White, 2=Black
p ≤ .05,
p ≤ .01,
p ≤ .001.
Third, using binary logistic regression models, we tested whether resilience was related to reduced likelihood of meeting criteria for anxiety and depression (hypothesis 3b; Table 4), and whether race moderated these associations (hypothesis 3c). More self-reliance and greater emotion-regulation were related to reduced likelihood of women screening positive for anxiety (Table 4) with no race differences in any associations (hypothesis 3c). Greater emotion-regulation and less hostility in close relationships were independently related to reduced likelihood of pregnant women screening positive for depression (hypothesis 3b). The relationship between screening self-reliance and reduced risk for meeting depression criteria was moderated by race (hypothesis 3c), such that more self-reliance was significantly related to reduced risk for depression only among White women (B=-.23, p<.01, OR=.80, 95% CI=.69, .92) but not Black women (B=.04, p=.66, OR=1.04, 95% CI=.89, 1.21).
4. Discussion
The current study, conducted during the initial height of the COVID-19 pandemic in the Philadelphia region, examined exposure risk, general and pregnancy specific COVID-19 worries, anxiety and depression, and resilience among a racially diverse sample of pregnant women. To assess the differential impact of the pandemic on Black women, we focused on comparisons between Black women and White, non-Hispanic, women. To limit the burden on participants, we utilized online evaluations that leveraged our previous efforts to establish a brief Risk and Resilience scale (Moore et al., 2020) and a web-based COVID-19 assessment of worries, anxiety and depression, as well as resilience (Barzilay et al., 2020).
We observed both similarities and important differences in the experiences of Black and White pregnant women. Regarding the exposure related impact of COVID-19, Black women were more likely to report having their jobs negatively impacted during the pandemic. They also reported knowing more people who had died from COVID-19. These findings reflect the well-recognized disproportionate toll of the pandemic on the health and economic stability of Black communities in the US (Cyrus et al., 2020; Kantamneni, 2020; Millett et al., 2020; Poteat et al., 2020), indicating structural racism (Chambers et al., 2020).
As hypothesized, race differences were evident in the levels of general COVID-19 worries reported by pregnant women. Black women reported worrying more about the financial burden of the pandemic, currently having COVID-19, and dying from COVID-19, although the latter two worries were not significant after controlling for covariates. White women reported more worries about infecting others, family members getting COVID-19, and themselves getting COVID-19, but the later worry was not significant after accounting for covariates. Increased worries about family getting COVID-19 and infecting others were also noted in a general population survey of predominantly White participants (Barzilay et al., 2020). Together, these findings suggest that greater economic burden of the pandemic on Black communities is a key stressor among Black pregnant women.
For the pregnancy-specific worries during the pandemic, Black women reported worrying more than White women about having a good birthing experience, receiving good prenatal care, and access to food, medication, and baby care items in the post-natal period. All participants in the study receive their prenatal care and will deliver within the same institution and both groups reported similar rates of worry about being exposed to the COVID-19 virus during prenatal visits. Nevertheless, the persistent race differences we observed with greater levels of worry reported by Black women, align strongly with prior reports of racial disparities in health care (Washington et al., 2008), as well as higher rates of preterm birth, preeclampsia, and maternal morbidity and mortality among Black women (Grobman et al., 2018; Menon et al., 2011). Thus, while we cannot compare these findings directly to birthing experiences of Black women pre-pandemic, these results are consistent with non-pandemic findings (McLemore et al., 2018) and the need to address underlying causes of racial disparity, such as structural racism, on maternal obstetrical and mental health (Altman et al., 2020; Chan et al., 2020; Niles et al., 2020).
The anxiety and depression screens indicated that across the whole sample, 11.1% of women met criteria for anxiety and 9.9% met criteria for depression. While depression was higher in Black women, this difference was not significant after accounting for covariates. Notably, when applying less conservative screening thresholds, Black women had higher rates of anxiety and depression after accounting for covariates. These rates of depression and anxiety are generally consistent with prior reports of anxiety and depression among pregnant women, which have been related to multiple factors (Biaggi et al., 2016; Fairbrother et al., 2016; Melville et al., 2010). Thus, our data do not offer strong support for increased anxiety and depression associated with COVID-19 in pregnant women. Although a paucity of research has examined the mental health of pregnant Black women, our findings do offer some support to mounting evidence of disproportionate rates of depression and anxiety for Black women during pregnancy as compared to White women (Melville et al., 2010; Orr et al., 2006; Rich-Edwards et al., 2006), including reports of higher rates of suicidal ideation (Zhong et al., 2016; Zhong et al., 2018). Thus, it is imperative that future studies focus on Black women's experiences of stress, anxiety, and depression during pregnancy, and examine how these experiences may impact birth outcomes and the development of offspring.
When examining resilience factors (hypothesis 3), Black women reported more personal resilience than White women, including higher levels of self-reliance and emotion regulation. In contrast, White women reported more environment related resilience factors, with less hostile close relationships and greater perceived neighborhood safety, but these differences were not statistically significant after controlling for covariates. Across the sample, there were differential associations between resilience and COVID-19 worries. Greater emotion regulation and greater perceived neighborhood safety were both independently related to fewer general COVID-19 worries, while higher emotion regulation and fewer hostile relationships were independently related to fewer pregnancy specific COVID-19 worries. Importantly, this pattern of results did not differ by race. That is, both Black and White pregnant women with more resilience in the domains of emotion regulation and fewer negative relationships reported fewer COVID-19 worries.
Consistent with hypothesis 3b, greater self-reliance and higher levels of emotion regulation were also both related to reduced likelihood that women would screen positive for anxiety, again with no race differences noted. Higher levels of emotion regulation and having fewer hostile relationships were independently related to reduced likelihood of women screening positive for depression. However, as hypothesized (3c), the relationship between self-reliance and reduced risk for meeting depression criteria was moderated by race, such that more self-reliance was related to reduced risk for depression only among White women, but not Black women. This constellation of results suggests that even though Black women exhibited higher rates of self-reliance and emotion regulation than White women, this personal resilience was not sufficient to buffer risk for depression (Sumbul et al., 2020). These findings may be due to the disproportionate effects of the pandemic on Black women relative to White women (e.g., financial burdens). Notably, Liu et al., (2020) reported in a sample of young adults assessed online during the pandemic, that individual resilience was associated with lower levels of depression and anxiety symptoms, but not PTSD. These findings obtained early in the pandemic align with the hypothesis that resilience can buffer effects of traumatic events, although we did not examine PTSD and our sample reported much lower levels of anxiety and depression and differed racially and in pregnancy status.
There are several limitations to this study. First, the survey was necessarily brief to limit participant burden. Thus, other salient concomitants of the pandemic (e.g., social isolation, family responsibilities) and their effects on mental health were not assessed. Second, the women who were not included in the study differed from those who participated. Black women were less likely to take part or be reached for the study. Several factors may have contributed to the differential participation, including job requirements, family caregiving responsibilities, internet availability, and lower levels of trust in the medical establishment (Sankaré et al., 2015; Sheppard, 2004). Notably, all of the women we attempted to contact for study participation had enrolled with our medical center's online portal, indicating that they did at one time have internet/data access but may not be interested for other reasons. Third, the small number of women from other racial/ethnic groups (e.g., Latino, Pacific Islanders) precluded further analyses representing these participants. Fourth, we lacked comparison non-pregnant groups who were sociodemographically balanced to the pregnant groups. Finally, the cross-sectional design precludes strong conclusions about cause and effect. Notably, building upon ongoing collaborations between the Penn-CHOP Lifespan Brain Institute and the Maternal and Child Health Research Center at Penn Medicine, we have permission to follow this sample and their offspring to help link COVID-19 related stressors to the mental health outcomes in mothers, and to newborn development.
In sum, this study further highlights the significant racial disparities in the impact of the COVID-19 pandemic and the experience of health care that affects the well-being of pregnant women, particularly pregnant Black women. These effects have critical implications for fetal and child development. Future studies are warranted to further characterize the scope and nature of intergenerational sequalae across and within racial groups and to specifically address how inequities in health care, structural racism, and neighborhood factors contribute to maternal and child health.
Declaration of competing interest
RB serves on the scientific board and reports stock ownership in ‘Taliaz Health’, with no conflict of interest relevant to this work. All other authors have nothing to disclose.
Acknowledgment
The study was supported by NIH grants R01-MH119219 (REG), K23-MH120437 (RB), T32-MH019112 (BHC), NR014784 (MAE), The Maternal and Child Health Research Center and the Lifespan Brain Institute of Penn Medicine and Children's Hospital of Philadelphia. We thank the study participants and the research teams.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113475.
Appendix. Supplementary materials
References
- Altemus M., Sarvaiya N., Neill Epperson C. Sex differences in anxiety and depression clinical perspectives. Front. Neuroendocrinol. 2014;35:320–330. doi: 10.1016/j.yfrne.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altman M.R., McLemore M.R., Oseguera T., Lindon A., Franck L.S. Listening to women: Recommendations from women of color to improve experiences in pregnancy and birth care. J Midwifery Womens Health. 2020;65:466–473. doi: 10.1111/jmwh.13102. [DOI] [PubMed] [Google Scholar]
- Arroll B., Goodyear-Smith F., Crengle S., Gunn J., Kerse N., Fishman T., Falloon K., Hatcher S. Validation of PHQ-2 and PHQ-9 to Screen for Major Depression in the Primary Care Population. Ann. Fam. Med. 2010;8:348–353. doi: 10.1370/afm.1139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bale T.L., Baram T.Z., Brown A.S., Goldstein J.M., Insel T.R., McCarthy M.M., Nemeroff C.B., Reyes T.M., Simerly R.B., Susser E.S., Nestler E.J. Early Life Programming and Neurodevelopmental Disorders. Biol. Psychiatry. 2010;68:314–319. doi: 10.1016/j.biopsych.2010.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barzilay R., Moore T.M., Greenberg D.M., DiDomenico, Grace E., Brown L.A, White L.K., Gur R.C., Gur R.E. Resilience, COVID-19-related stress, anxiety and depression during the pandemic in a large population enriched for healthcare providers. Transl. Psychiatry. 2020;10:291. doi: 10.1038/s41398-020-00982-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biaggi A., Conroy S., Pawlby S., Pariante C.M. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J. Affect. Disord. 2016;191:62–77. doi: 10.1016/j.jad.2015.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carey M., Boyes A., Noble N., Waller A., Inder K. Validation of the PHQ-2 against the PHQ-9 for detecting depression in a large sample of Australian general practice patients. Aust. J. Prim. Health. 2016;22:262. doi: 10.1071/PY14149. [DOI] [PubMed] [Google Scholar]
- Chambers B.D., Arabia S.E., Arega H.A., Altman M.R., Berkowitz R., Feuer S.K., Franck L.S., Gomez A.M., Kober K., Pacheco‐Werner T., Paynter R.A., Prather A.A., Spellen S.A., Stanley D., Jelliffe‐Pawlowski L.L., McLemore M.R. Exposures to structural racism and racial discrimination among pregnant and early post‐partum Black women living in Oakland. California. Stress Heal. 2020;36:213–219. doi: 10.1002/smi.2922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan A.L., Guo N., Popat R., Robakis T., Blumenfeld Y.Y., Main E., Scott K.A., Butwick A.J. Racial and ethnic disparities in hospital-based care associated with postpartum depression. J Racial Ethn Health Disparities. 2020 doi: 10.1007/s40615-020-00774-y. [DOI] [PubMed] [Google Scholar]
- Cyrus E., Clarke R., Hadley D., Bursac Z., Trepka M.J., Devieux J.G., Bagci U., Furr-Holden D., Coudray M.S., Mariano Y., Kiplagat S., Noel I., Ravelo G., Paley M., Wagner E.F. The impact of COVID-19 on African American communities in the United States. medRxiv. 2020 doi: 10.1101/2020.05.15.20096552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dashraath P., Wong J.L.J., Lim M.X.K., Lim L.M., Li S., Biswas A., Choolani M., Mattar C., Su L.L. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am. J. Obstet. Gynecol. 2020;222:521–531. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunkel Schetter C., Tanner L. Anxiety, depression and stress in pregnancy. Curr. Opin. Psychiatry. 2012;25:141–148. doi: 10.1097/YCO.0b013e3283503680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairbrother N., Janssen P., Antony M.M., Tucker E., Young A.H. Perinatal anxiety disorder prevalence and incidence. J. Affect. Disord. 2016;200:148–155. doi: 10.1016/j.jad.2015.12.082. [DOI] [PubMed] [Google Scholar]
- Feldman R. What is resilience: an affiliative neuroscience approach. World Psychiatry. 2020;19:132–150. doi: 10.1002/wps.20729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grobman W.A., Parker C.B., Willinger M., Wing D.A., Silver R.M., Wapner R.J., Simhan H.N., Parry S., Mercer B.M., Haas D.M., Peaceman A.M., Hunter S., Wadhwa P., Elovitz M.A., Foroud T., Saade G., Reddy U.M. Racial Disparities in Adverse Pregnancy Outcomes and Psychosocial Stress. Obstet. Gynecol. 2018;131:328–335. doi: 10.1097/AOG.0000000000002441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kantamneni N. The impact of the COVID-19 pandemic on marginalized populations in the United States: A research agenda. J. Vocat. Behav. 2020;119 doi: 10.1016/j.jvb.2020.103439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebel C., MacKinnon A., Bagshawe M., Tomfohr-Madsen L., Giebrecht G. Elevated depression and anxiety among pregnant individuals during the COVID-19 pandemic. PsyArXiv April. 2020:23. doi: 10.31234/osf.io/gdhkt. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.C. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Res. 2020;290 doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLemore M.R., Altman M.R., Cooper N., Williams S., Rand L., Franck L. Health care experiences of pregnant, birthing and postnatal women of color at risk for preterm birth. Soc. Sci. Med. 2018;201:127–135. doi: 10.1016/j.socscimed.2018.02.013. [DOI] [PubMed] [Google Scholar]
- Melville J.L., Gavin A., Guo Y., Fan M.-Y., Katon W.J. Depressive Disorders During Pregnancy. Obstet. Gynecol. 2010;116:1064–1070. doi: 10.1097/AOG.0b013e3181f60b0a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menon R., Dunlop A.L., Kramer M.R., Fortunato S.J., Hogue C.J. An overview of racial disparities in preterm birth rates: caused by infection or inflammatory response? Acta Obstet. Gynecol. Scand. 2011;90:1325–1331. doi: 10.1111/j.1600-0412.2011.01135.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millett G.A., Jones A.T., Benkeser D., Baral S., Mercer L., Beyrer C., Honermann B., Lankiewicz E., Mena L., Crowley J.S., Sherwood J., Sullivan P.S. Assessing differential impacts of COVID-19 on black communities. Ann. Epidemiol. 2020;47:37–44. doi: 10.1016/j.annepidem.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore T.M., Martin I.K., Gur O.M., Jackson C.T., Scott J.C., Calkins M.E., Ruparel K., Port A.M., Nivar I., Krinsky H.D., Gur R.E., Gur R.C. Characterizing social environment's association with neurocognition using census and crime data linked to the Philadelphia Neurodevelopmental Cohort. Psychol. Med. 2016;46:599–610. doi: 10.1017/S0033291715002111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore T.M., White L.K., Barzilay R., Calkins M.E., Jones J.D., Young J.F., Gur R.C., Gur R.E. Development of a scale battery for rapid assessment of risk and resilience. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mossman S.A., Luft M.J., Schroeder H.K., Varney S.T., Fleck D.E., Barzman D.H., Gilman R., DelBello M.P., Strawn J.R. The Generalized Anxiety Disorder 7-item scale in adolescents with generalized anxiety disorder: Signal detection and validation. Ann. Clin. Psychiatry. 2017;29:227–234A. [PMC free article] [PubMed] [Google Scholar]
- Niles P.M., Asiodu I.V., Crear-Perry J., Julian Z., Lyndon A., McLemore M.R., Planey A.M., Scott K.A., Vedam S. Reflecting on equity in perinatal care During a pandemic. Health equity. 2020;4:330–333. doi: 10.1089/heq.2020.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr S.T., Blazer D.G., James S.A. Racial Disparities in Elevated Prenatal Depressive Symptoms Among Black and White Women in Eastern North Carolina. Ann. Epidemiol. 2006;16:463–468. doi: 10.1016/j.annepidem.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Poteat T., Millett G.A., Nelson L.E., Beyrer C. Understanding COVID-19 risks and vulnerabilities among black communities in America: the lethal force of syndemics. Ann. Epidemiol. 2020;47:1–3. doi: 10.1016/j.annepidem.2020.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rasmussen S.A., Smulian J.C., Lednicky J.A., Wen T.S., Jamieson D.J. Coronavirus Disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am. J. Obstet. Gynecol. 2020;222:415–426. doi: 10.1016/j.ajog.2020.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards J.W., Kleinman K., Abrams A., Harlow B.L., McLaughlin T.J., Joffe H., Gillman M.W. Sociodemographic predictors of antenatal and postpartum depressive symptoms among women in a medical group practice. J. Epidemiol. Community Health. 2006;60:221–227. doi: 10.1136/jech.2005.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubinow D.R., Schmidt P.J. Sex differences and the neurobiology of affective disorders. Neuropsychopharmacology. 2019;44:111–128. doi: 10.1038/s41386-018-0148-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rutter M. Implications of resilience concepts for scientific understanding. Ann. N. Y. Acad. Sci. 2006;1094:1–12. doi: 10.1196/annals.1376.002. [DOI] [PubMed] [Google Scholar]
- Sankaré I.C., Bross R., Brown A.F., del Pino H.E., Jones L.F., Morris D.M., Porter C., Lucas-Wright A., Vargas R., Forge N., Norris K.C., Kahn K.L. Strategies to Build Trust and Recruit African American and Latino Community Residents for Health Research: A Cohort Study. Clin. Transl. Sci. 2015;8:412–420. doi: 10.1111/cts.12273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheppard V.B. Providing health care to low-income women: a matter of trust. Fam. Pract. 2004;21:484–491. doi: 10.1093/fampra/cmh503. [DOI] [PubMed] [Google Scholar]
- Sønderskov K.M., Dinesen P.T., Santini Z.I., Østergaard S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020;32:226–228. doi: 10.1017/neu.2020.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spitzer R.L., Kroenke K., Williams J.B.W., Löwe B. A Brief Measure for Assessing Generalized Anxiety Disorder. Arch. Intern. Med. 2006;166:1092. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Sumbul T., Spellen S., McLemore M.R. A Transdisciplinary Conceptual Framework of Contextualized Resilience for Reducing Adverse Birth Outcomes. Qual. Health Res. 2020;30:105–118. doi: 10.1177/1049732319885369. [DOI] [PubMed] [Google Scholar]
- Ungar M., Theron L. Resilience and mental health: how multisystemic processes contribute to positive outcomes. The Lancet Psychiatry. 2020;7:441–448. doi: 10.1016/S2215-0366(19)30434-1. [DOI] [PubMed] [Google Scholar]
- Van den Bergh B.R.H., van den Heuvel M.I., Lahti M., Braeken M., de Rooij S.R., Entringer S., Hoyer D., Roseboom T., Räikkönen K., King S., Schwab M. Prenatal developmental origins of behavior and mental health: The influence of maternal stress in pregnancy. Neurosci. Biobehav. Rev. 2017 doi: 10.1016/j.neubiorev.2017.07.003. [DOI] [PubMed] [Google Scholar]
- Vesga-López O., Blanco C., Keyes K., Olfson M., Grant B.F., Hasin D.S. Psychiatric Disorders in Pregnant and Postpartum Women in the United States. Arch. Gen. Psychiatry. 2008;65:805. doi: 10.1001/archpsyc.65.7.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vindegaard N., Benros M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain. Behav. Immun. 2020:1–12. doi: 10.1016/j.bbi.2020.05.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Washington D.L., Bowles J., Saha S., Horowitz C.R., Moody-Ayers S., Brown A.F., Stone V.E., Cooper L.A. Transforming clinical practice to eliminate racial-ethnic disparities in healthcare. J. Gen. Intern. Med. 2008;23:685–691. doi: 10.1007/s11606-007-0481-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yan J., Guo J., Fan C., Juan J., Yu X., Li J., Feng L., Li C., Chen H., Qiao Y., Lei D., Wang C., Xiong G., Xiao F., He W., Pang Q., Hu X., Wang S., Chen D., Zhang Y., Poon L.C., Yang H. Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am. J. Obstet. Gynecol. 2020;223:111.e1–111.e14. doi: 10.1016/j.ajog.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Q.Y., Gelaye B., Miller M., Fricchione G.L., Cai T., Johnson P.A., Henderson D.C., Williams M.A. Suicidal behavior-related hospitalizations among pregnant women in the USA, 2006–2012. Arch. Womens. Ment. Health. 2016;19:463–472. doi: 10.1007/s00737-015-0597-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong Q.-Y., Gelaye B., Smoller J.W., Avillach P., Cai T., Williams M.A. Adverse obstetric outcomes during delivery hospitalizations complicated by suicidal behavior among US pregnant women. PLoS One. 2018;13 doi: 10.1371/journal.pone.0192943. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.