Abstract
Background:
Through enhancement of the Wnt signaling pathway R-spondins are oncogenic drivers in colorectal cancer. Experimental data suggest that the R-spondin/Wnt axis stimulates VEGF-dependent angiogenesis. We therefore hypothesize that variations within R-spondin genes predict outcome in patients with metastatic colorectal cancer (mCRC) treated with upfront FOLFIRI and bevacizumab.
Patients and methods:
773 mCRC patients enrolled in the randomized phase III FIRE-3 and TRIBE trials and receiving either FOLFIRI/bevacizumab (training and validation cohorts) or FOLFIRI/cetuximab (control group) were involved in this study. The impact of six functional single-nucleotide polymorphisms (SNPs) within the R-spondin 1–3 genes on outcome were evaluated.
Results:
RAS and KRAS wild-type patients harboring any G allele of the RSPO2 rs555008 SNP had a longer overall survival compared to those having a TT genotype in both the training (FIRE-3) and validation (TRIBE) cohorts (29.0 vs 23.6 months, P=0.009 and 37.8 vs 19.4 months, P=0.021 for RAS wild-type patients and 28.4 vs 22.3 months, P=0.011 and 36.0 vs 23.3 months, P=0.046 for KRAS wild-type patients). Conversely, any G allele carriers with KRAS and RAS mutant tumors exhibited a shorter progression-free survival compared to TT genotype carriers, whereas the results were clinically more evident for KRAS mutant patients in both the training and validation cohorts (8.1 vs 11.2 months, P=0.023 and 8.7 vs 10.3 months, P=0.009).
Conclusion:
Genotyping of the RSPO2 rs555008 polymorphism may help to select patients who will derive the most benefit from adding bevacizumab to FOLFIRI dependent on (K)RAS mutational status.
Keywords: R-spondin, colorectal cancer, polymorphisms, bevacizumab, biomarker
INTRODUCTION
Colon cancer is the fourth most common cause of cancer-related mortality [1]. The implementation of biologicals into the 5-fluorouracil (5-FU)-based treatment regimens led to improved prognosis of mCRC [2,3]. To further optimize outcome and overcome treatment resistance in refractory mCRC new therapeutic options are mandatory [1,2]. Hyperactivation of the Wnt signaling pathway is believed to be the initiating and driving event during tumor development in colorectal cancers [4]. R-spondin proteins stimulate Wnt signaling by binding to their leucine-rich G protein coupled 4/5 receptor (LGR4/5) and transmembrane E3 ubiquitin ligase proteins zinc and ring finger 3 (ZNRF3) and ring finger 43 (RNF43) [5]. R-spondin binding promotes removal of ZNRF3 from the plasma membrane and results in increased levels of Frizzled leading to an enhanced Wnt response [6]. R-spondins play a critical role in different biological processes such as vascular formation and development of the lungs, limbs, nails, and muscles most likely through enhancement of Wnt signaling [7–9]. Moreover, the R-spondin – ZNRF3/RNF43 axis controls intestinal stem cell activity by counterbalancing the inhibitory effect of ZNRF3/RNF43 on Wnt signaling [10]. Thus, R-spondins serve as a finely tuned regulator of Wnt signaling enabling proper differentiation and self-renewal of intestinal stem cells [11].
Seshagiri et al. identified recurrent fusions involving RSPO2 and RSPO3 genes in 10% of colon tumors that resulted in upregulation of Wnt target genes [12]. Furthermore, there is increasing evidence that RSPO gene rearrangements might act as oncogenic drivers in colorectal cancer [13]. Just recently, inhibitors of RSPO gene fusions have shown promising activity in colorectal cancer mouse models [13–15].
Additionally, preclinical data suggest that the RSPO/Wnt axis stimulates angiogenesis and endothelial cell proliferation through activation of VEGFC and VEGFR3 signaling [16], which led us to explore the associations of genetic variations in RSPO genes with outcome in mCRC patients receiving first-line FOLFIRI and bevacizumab (bev).
PATIENTS AND METHODS
Study design and patient population
The study involved 773 mCRC patients enrolled in the randomized phase III FIRE-3 and TRIBE trials and receiving either first-line FOLFIRI/bev (training and validation sets) or FOLFIRI and cetuximab (cet) (FIRE-3, control group). In FIRE-3 FOLFIRI/bev arm patients were treated with bevacizumab 5mg/kg biweekly and in the FOLFIRI/cet cohort cet was administered at an initial dose of 400mg/m2, then 250mg/m2 per week. The FOLFIRI backbone regimen comprised of 180mg/m2 irinotecan, 400mg/m2 leucovorin, 400mg/m2 fluorouracil (5-FU) bolus injection and 2400mg/m2 infusion during 46 hours. Cycles were repeated biweekly until tumor progression or intolerable side-effects occured [17].
The validation cohort consisted of mCRC patients, enrolled in the randomized phase III TRIBE trial and treated identically to those in the training cohort (FOLFIRI/bev) with the exception that leucovorin was administered at a dose of 200mg/m2. After 12 cycles, patients were treated with 5-FU and bev until progression [18]. Ethics committee approval for the study was obtained for each participating site. All patients gave informed consent for molecular analyses, which were performed at the USC / Norris Comprehensive Cancer Center in Los Angeles, USA. Our study was conducted according to the reporting recommendations for tumor marker prognostic studies [REMARK] [19].
Candidate polymorphisms
We identified functional single-nucleotide polymorphisms in the RSPO 1–3 genes based on following criteria: minor allele frequency >10% in the Caucasion population, and the ability to alter the function of a gene according to public databases (https://snpinfo.niehs.nih.gov, www.ensembl.org, https://www.ncbi.nlm.nih.gov/snp/ and https://www.genecards.org/).
Genotyping
Genomic DNA was isolated from formalin-fixed paraffin-embedded tissue in the training and control sets (FIRE-3) and from blood in the validation cohort (TRIBE) using the QIAmp DNA easy kit (Qiagen, Valencia, CA, USA). Six potentially functional SNPs in three RSPO genes (RSPO1, RSPO2 and RSPO3) were examined by PCR-based direct sequencing (Supplementary Table S1). We used forward and reverse primers for PCR amplification. The resulting fragments were sequenced on an ABI 3100A Capillary Genetic Analyzer (Applied Biosystem, USA) to detect the individual SNP. The investigator (MDB) performing the DNA sequence analyses was blinded to the outcome data.
Statistical analysis
We hypothesized that SNPs within three RSPO genes are associated with clinical outcome in mCRC patients who participated in two phase III randomized trials (FIRE-3 and TRIBE). The training cohort was comprised of patients treated with first-line FOLFIRI/bev within the FIRE-3 trial, whereas patients receiving the same treatment in TRIBE served as a validation cohort. The control set consisted of patients receiving first-line FOLFIRI/cet in FIRE-3.
Primary endpoint was progression-free survival (PFS), secondary endpoints were overall survival (OS) and overall response rate (ORR). PFS was the interval from randomization until progression or death. OS was calculated from randomization until death. Patients without events were censored at last follow-up. ORR was calculated from the percentage of patients with either a complete (CR) or a partial (PR) remission using the Response Evaluation Criteria in Solid Tumors (RECIST). We evaluated the allelic distribution of polymorphisms for deviation from Hardy-Weinberg equilibrium (HWE) using the χ2 test. Differences between patient characteristics among the treatment arms were compared by using the χ2 test. The log-rank test and Kaplan Meier curves were used to assess the impact of various SNPs on PFS and OS. The correlations between each genetic variation and tumor response rate were examined using the χ2 test. SNPs were initially tested in the overall and (K)RAS wild-type population of the training cohort. Significant SNPs predicting outcome in the training cohort (FIRE-3) in univariable analysis were further tested in multivariable analysis and examined in a validation cohort (TRIBE) and a control set (FIRE-3). The adjusting parameters for multivariable analyses are outlined in Table 2 and 3. With 292 patients (249 PFS events) in the FOLFIRI/bev arm of FIRE-3 (training cohort) with genotyping results available, we would reach 80% power to detect a minimum hazard ratio (HR) of 1.40–1.52 on PFS for a SNP with a minor allele frequency from 0.1–0.5 using a two-sided 0.05 level log-rank test. The HR would be 1.49–1.65 in the validation cohort (FOLFIRI/bev arm of TRIBE, N=210, 164 PFS events) and 1.42–1.55 in the control set (FOLFIRI/cet arm of FIRE-3, N=271, 234 PFS events) using the same model and power. All P-values were from two-sided tests at a 0.05 significance level. All analyses were performed by using the SAS version 9.4.
Table 2.
Association between RSPO2 rs555008 and clinical outcomes among mCRC patients according to KRAS status
| Tumor response | Progression-free survival | Overall survival | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Genotype | N | Yes | No | Chi- square test P value | Median (95%CI), months | HR (95%CI) | Log-rank test P value | Adjusted HR (95%CI) a | Wald test P value | Median (95%CI), months | HR (95%CI) | Log-rank test P value | Adjusted HR (95%CI) a | Wald test P value | |
| KRAS wild-type | |||||||||||||||
| Training cohort | T/T | 121 | 69(63.3%) | 40(36.7%) | 0.44 | 10.1(9.0,12.0) | Reference | 0.16 | Reference | 0.44 | 22.3(17.5,26.4) | Reference | 0.011 | Reference | 0.15 |
| Any G | 91 | 57(68.7%) | 26(31.3%) | 11.5(9.6,13.0) | 0.81(0.59,1.09) | 0.88(0.64,1.22) | 28.4(22.7,35.0) | 0.64(0.45,0.90) | 0.76(0.52,1.11) | ||||||
| Validation cohort | T/T | 48 | 29(61.7%) | 18(38.3%) | 0.64 | 9.0(7.6,11.0) | Reference | 0.17 | Reference | 0.29 | 23.3(14.6,26.9) | Reference | 0.046 | Reference | 0.012 |
| Any G | 38 | 24(66.7%) | 12(33.3%) | 11.6(9.9,12.7) | 0.72(0.44,1.17) | 0.74(0.43,1.28) | 36.0(23.9,48.7) | 0.62(0.38,1.00) | 0.49(0.28,0.86) | ||||||
| Control cohort | T/T | 105 | 65(75.6%) | 21(24.4%) | 0.42 | 10.1(8.5,11.3) | Reference | 0.74 | Reference | 0.66 | 36.4(21.9,39.4) | Reference | 0.46 | Reference | 0.46 |
| Any G | 121 | 76(70.4%) | 32(29.6%) | 10.0(8.3,12.2) | 1.05(0.79,1.40) | 1.07(0.80,1.43) | 27.6(22.5,33.8) | 1.14(0.80,1.63) | 1.15(0.80,1.65) | ||||||
| KRAS mutant | |||||||||||||||
| Training cohort | T/T | 23 | 9(40.9%) | 13(59.1%) | 0.45 | 11.2(8.3,14.7) | Reference | 0.023 | Reference | 0.099 | 26.3(18.2,36.0) | Reference | 0.076 | Reference | 0.057 |
| Any G | 19 | 10(52.6%) | 9(47.4%) | 8.1(6.1,12.3) | 1.93(0.98,3.79) | 1.98(0.88,4.45) | 16.5(12.5,25.1) | 1.75(0.91,3.36) | 2.58(0.97,6.87) | ||||||
| Validation cohort | T/T | 60 | 33(55.9%) | 26(44.1%) | 0.60 | 10.3(8.8,13.0) | Reference | 0.009 | Reference | 0.027 | 27.9(20.8,38.3) | Reference | 0.10 | Reference | 0.59 |
| Any G | 28 | 14(50.0%) | 14(50.0%) | 8.7(7.8,9.5) | 1.91(1.12,3.28) | 1.99(1.08,3.65) | 19.8(15.6,26.3) | 1.52(0.91,2.56) | 1.17(0.66,2.06) | ||||||
Based on the multivariable Cox proportional hazards regression model adjusting for sex, age, ECOG performance status, primary tumor site, liver limited metastases, primary tumor resection, adjuvant chemotherapy, and BRAF status in the training and control cohorts; adjusting for sex, age, ECOG performance status, primary tumor site, number of metastatic sites, primary tumor resection, and BRAF status in the validation set.
Table 3.
Association between RSPO2 rs555008 and clinical outcomes among mCRC patients according to RAS status
| Tumor response | Progression-free survival | Overall survival | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Genotype | N | Yes | No | Chi- square test P value | Median (95%CI), months | HR (95%CI) | Log-rank test P value | Adjusted HR (95%CI) a | Wald test P value | Median (95%CI), months | HR (95%CI) | Log-rank test P value | Adjusted HR (95%CI) a | Wald test P value | |
| RAS wild-type | |||||||||||||||
| Training cohort | T/T | 94 | 51(62.2%) | 31(37.8%) | 0.34 | 9.9(8.8,12.0) | Reference | 0.073 | Reference | 0.25 | 23.6(18.6,27.5) | Reference | 0.009 | Reference | 0.16 |
| Any G | 73 | 48(69.6%) | 21(30.4%) | 11.5(9.3,12.9) | 0.74(0.53,1.04) | 0.81(0.56,1.16) | 29.0(24.2,39.5) | 0.60(0.41,0.89) | 0.74(0.48,1.13) | ||||||
| Validation cohort | T/T | 24 | 14(58.3%) | 10(41.7%) | 0.67 | 9.0(6.7,11.7) | Reference | 0.31 | Reference | 0.53 | 19.4(11.2,26.3) | Reference | 0.021 | Reference | 0.11 |
| Any G | 25 | 12(52.2%) | 11(47.8%) | 11.3(7.7,12.7) | 0.72(0.38,1.39) | 0.78(0.36,1.70) | 37.8(20.8,52.5) | 0.49(0.25,0.94) | 0.53(0.24,1.16) | ||||||
| Control cohort | T/T | 86 | 57(80.3%) | 14(19.7%) | 0.39 | 10.4(9.2,13.0) | Reference | 0.90 | Reference | 0.69 | 37.1(21.9,41.2) | Reference | 0.62 | Reference | 0.49 |
| Any G | 93 | 61(74.4%) | 21(25.6%) | 10.6(8.7,12.8) | 1.02(0.74,1.41) | 1.07(0.76,1.50) | 29.8(23.7,40.0) | 1.11(0.74,1.66) | 1.16(0.76,1.78) | ||||||
| RAS mutant | |||||||||||||||
| Training cohort | T/T | 43 | 22(52.4%) | 20(47.6%) | 0.82 | 10.9(8.5,13.0) | Reference | 0.11 | Reference | 0.020 | 21.3(15.9,31.5) | Reference | 0.52 | Reference | 0.074 |
| Any G | 32 | 16(55.2%) | 13(44.8%) | 9.2(7.2,13.4) | 1.47(0.87,2.48) | 2.01(1.12,3.62) | 19.0(16.3,26.9) | 1.19(0.70,2.01) | 1.81(0.94,3.45) | ||||||
| Validation cohort | T/T | 74 | 41(56.9%) | 31(43.1%) | 0.89 | 9.5(8.6,11.8) | Reference | 0.042 | Reference | 0.18 | 25.6(20.8,37.2) | Reference | 0.20 | Reference | 0.75 |
| Any G | 36 | 21(58.3%) | 15(41.7%) | 9.2(7.8,9.9) | 1.57(0.98,2.50) | 1.40(0.86,2.29) | 20.8(17.8,27.9) | 1.33(0.85,2.10) | 0.92(0.56,1.52) | ||||||
Based on the multivariable Cox proportional hazards regression model adjusting for sex, age, ECOG performance status, primary tumor site, liver limited metastases, primary tumor resection, adjuvant chemotherapy, and BRAF status in the training and control cohorts; adjusting for sex, age, ECOG performance status, primary tumor site, number of metastatic sites, primary tumor resection, and BRAF status in the validation set.
RESULTS
Patient baseline characteristics of the study cohorts (training, validation and control cohorts) are illustrated in Table 1. Our study comprised of 773 patients with mCRC treated with FOLFIRI/bev (training cohort FIRE-3, N=292 and validation cohort TRIBE, N=210) or FOLFIRI/cet (control set FIRE-3, N=271). The median follow-up times were 40.9, 49.9, and 41.7 months in the training, validation and control cohorts. The median PFS and OS were 10.0 and 23.7 months in the training cohort, 9.4 and 25.1 months in the validation cohort and 9.6 and 27.1 months in the control set, respectively. The RSPO3 rs10457487 SNP was not within the HWE and therefore excluded from further analyses. In the overall population of the training cohort no association with outcome could be observed (Supplementary Table S2). However, in the training cohort (FIRE-3 FOLFIRI/bev) the RSPO2 rs555008 SNP was significantly associated with OS in KRAS wild-type patients. Patients harboring any G allele showed a longer OS (28.4 vs 22.3 months) compared to those with a TT genotype in univariable analysis (HR 0.64, 95% confidence interval (CI) 0.45–0.90, P=0.011) (Table 2, Figure 1A). Similarly, any G allele carriers with KRAS wild-type tumors in the validation cohort (TRIBE FOLFIRI/bev) displayed a significant longer OS (36.0 vs 23.3 months) in both univariable (HR 0.62, 95% CI 0.38–1.00, P=0.046) and multivariable analyses (HR 0.49, 95% CI 0.28–0.86, P=0.012) (Table 2, Figure 1B). Conversely, mCRC patients with KRAS wild-type tumors harboring any G allele and treated with FOLFIRI/cet (control cohort, FIRE-3) did not have better OS (27.6 vs 36.4 months) in comparison to those with a TT genotype (univariable analysis (HR 1.14, 95% CI 0.80–1.63, P=0.46) (Table 2, Figure 1C). Interestingly, G allele carriers in the KRAS mutant subgroup of the training cohort had a significant shorter PFS compared to those carrying the TT genotype in univariable analysis (8.1 vs. 11.2 months, HR 1.93, 95% CI 0.98–3.79, P=0.023) (Table 2, Figure 2A). The same effect on PFS could also be observed in the validation cohort (8.7 vs 10.3 months) in both univariable (HR 1.91, 95% CI 1.12–3.28, P=0.009) (Table 2, Figure 2B) and multivariable analyses (HR 1.99, 95% CI 1.08–3.65, P=0.027). The same trend in outcome observed in KRAS wild-type patients could be replicated in patients with RAS wild-type mCRC. G allele carriers with a RAS wild-type primary tumor treated with FOLFIRI/bev had a longer OS than those with a TT genotype in univariable analyses in both the training (FIRE-3) and validation (TRIBE) cohorts (29.0 vs. 23.6 months, HR 0.60, 95% CI 0.41–0.89, P=0.009 and 37.8 vs 19.4 months, HR 0.49, 95% CI 0.25–0.94, P=0.021) (Table 3). Again, no difference in outcome could be seen between G allele carriers and those with a TT genotype of the RSPO2 rs555008 SNP harboring a RAS wild-type mCRC and treated with FOLFIRI/cet. Similar to KRAS mutant patients, G allele carriers with RAS mutant tumors receiving FOLFIRI/bev still exhibited a worse PFS in both the training (FIRE-3) and validation (TRIBE) cohorts (9.2 vs 10.9 months, in multivariable analysis HR 2.01, 95% CI 1.12–3.62, P=0.020 and 9.2 vs 9.5 months, in univariable analysis HR 1.57, 95% CI 0.98–2.50, P=0.042) (Table 3).
Table 1.
Baseline characteristics
| FIRE-3 | TRIBE | FIRE-3 | |||
|---|---|---|---|---|---|
| Treatment | FOLFIRI+Bev | FOLFIRI+Bev | FOLFIRI+Cet | ||
| N | N=292 | N=210 | N=271 | P-valuea | |
| Sex | 0.068 | ||||
| Male | 507 | 191(65%) | 126(60%) | 190(70%) | |
| Female | 266 | 101(35%) | 84(40%) | 81(30%) | |
| Age | <0.001 | ||||
| <65 | 421 | 144(49%) | 139(66%) | 138(51%) | |
| ≥65 | 352 | 148(51%) | 71(34%) | 133(49%) | |
| ECOG performance status | <0.001 | ||||
| 0 | 473 | 160(55%) | 173(82%) | 140(52%) | |
| 1–2 | 299 | 132(45%) | 36(17%) | 131(48%) | |
| Unspecified | 1 | - | 1(0%) | - | |
| Primary tumor site | 0.13 | ||||
| Right | 181 | 75(26%) | 53(25%) | 53(20%) | |
| Left | 563 | 210(72%) | 142(68%) | 211(78%) | |
| Unspecified | 29 | 7(2%) | 15(7%) | 7(3%) | |
| Liver limited metastases | 0.87 | ||||
| Yes | 250 | 95(33%) | 65(31%) | 90(33%) | |
| No | 523 | 197(67%) | 145(69%) | 181(67%) | |
| Number of metastatic sites | 0.39 | ||||
| 1 | 289 | 105(36%) | 89(42%) | 95(35%) | |
| 2 | 246 | 83(28%) | 85(40%) | 78(29%) | |
| ≥3 | 145 | 56(19%) | 36(17%) | 53(20%) | |
| Unspecified | 93 | 48(16%) | - | 45(17%) | |
| Primary tumor resection | <0.001 | ||||
| Yes | 615 | 252(86%) | 132(63%) | 231(85%) | |
| No | 157 | 40(14%) | 78(37%) | 39(14%) | |
| Unspecified | 1 | - | - | 1(0%) | |
| Adjuvant chemotherapy | 0.062 | ||||
| Yes | 137 | 53(18%) | 27(13%) | 57(21%) | |
| No | 635 | 239(82%) | 183(87%) | 213(79%) | |
| Unspecified | 1 | - | - | 1(0%) | |
| KRAS status | <0.001 | ||||
| Wild-type | 556 | 244(84%) | 86(41%) | 226(83%) | |
| Mutant | 181 | 48(16%) | 88(42%) | 45(17%) | |
| Unspecified | 36 | - | 36(17%) | - | |
| RAS status | <.0001 | ||||
| Wild-type | 423 | 195(67%) | 49(23%) | 179(66%) | |
| Mutant | 275 | 84(29%) | 110(52%) | 81(30%) | |
| Unspecified | 75 | 13(4%) | 51(24%) | 11(4%) | |
| BRAF status | 0.63 | ||||
| Wild-type | 664 | 258(88%) | 163(78%) | 243(90%) | |
| Mutant | 57 | 25(9%) | 11(5%) | 21(8%) | |
| Unspecified | 52 | 9(3%) | 36(17%) | 7(3%) | |
The unspecified group was not included in the analysis.
The P-value was based on the Chi-square test.
Figure 1:
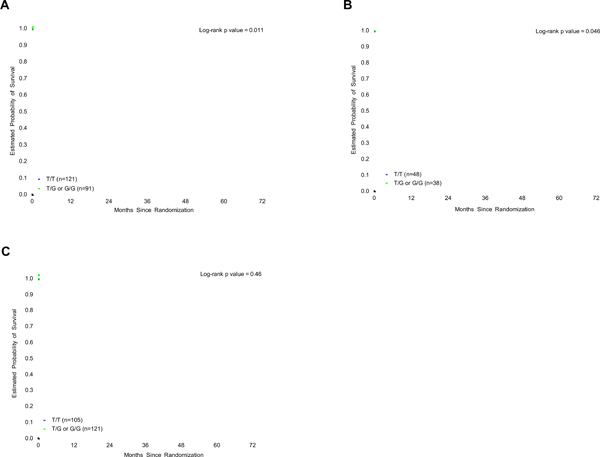
RSPO2 rs555008 and overall survival among patients with KRAS wild-type tumors. A Training cohort: RSPO2 rs555008 and OS (FIRE-3 FOLFIRI/bevacizumab arm). B Validation cohort: RSPO2 rs555008 and OS (TRIBE FOLFIRI/bevacizumab arm). C Control cohort: RSPO2 rs555008 and OS (FIRE-3 FOLFIRI/cetuximab arm).
Figure 2:
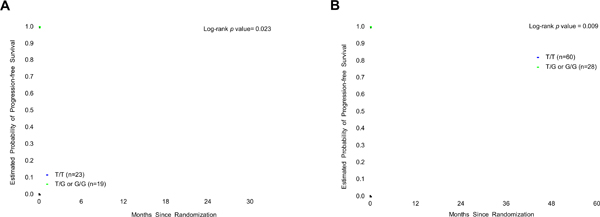
RSPO2 rs555008 and progression-free survival among patients with KRAS mutant tumors. A Training cohort: RSPO2 rs555008 and PFS (FIRE-3 FOLFIRI/bevacizumab arm). B Validation cohort: RSPO2 rs555008 and PFS (TRIBE FOLFIRI/bevacizumab arm).
DISCUSSION
Canonical Wnt signaling is not only involved in various critical biological processes such as organogenesis and tissue regeneration [20], but also plays a major role in early tumorigenesis of colorectal cancer [21]. R-spondin proteins are potent agonists of Wnt signaling and therefore can act as critical drivers of tumor development [5]. Additionally, preclinical studies demonstrated that R-spondins are involved in angiogenesis. While Caruso et al. demonstrated that R-spondin 1 enhances testicular angiogenesis in culture [22], another group could show that RSPO2 induced cell proliferation in human umbilical vein endothelial cells (HUVEC) [23]. Just recently, RSPO3 expression has been demonstrated in both mouse and human endothelial cells [24]. These results suggest that the R-spondin protein family may play a role in promoting angiogenesis. To the best of our knowledge, we provide the first evidence that a variation in the R-spondin 2 gene may predict outcome in mCRC patients treated with first-line FOLFIRI/bev. While we could demonstrate that (K)RAS wild-type mCRC patients carrying any G allele of the RSPO2 rs555008 SNP have a better OS than those with a TT genotype when treated with first-line FOLFIRI/bev in both the training and validation cohort, these associations were not observed in patients treated with FOLFIRI/cet. Interestingly, we could observe inverse associations with outcome among any G allele carriers with (K)RAS mutant tumors treated with FOLFIRI/bev. Here, any G allele carriers in both the training (FIRE-3) and validation cohorts (TRIBE) had a shorter PFS compared to those patients harboring a TT genotype. These validated inverse associations with outcome among G alleles carriers with either (K)RAS wild-type (better outcome) or (K)RAS mutant tumors (worse outcome) treated with FOLFIRI/bev suggest opposing effects of the RSPO2 rs555008 SNP on outcome depending on the (K)RAS status. The G allele of the RSPO2 rs555008 variant is located in the 3’-UTR and provides binding sites for hsa-miR-484 and hsa-miR-590–3p, which regulate post-transcriptional gene expression (https://snpinfo.niehs.nih.gov).
Preclinical studies identified a simultaneous activation of KRAS and Wnt signaling in mouse models of colorectal cancer [25]. Both enhanced and aberrant Wnt signaling as well as activating KRAS mutations are early events during colorectal tumorigenesis. Oncogenic KRAS stimulates Wnt signaling by increasing phosphorylation of Beta-catenin, which results in disruption of its binding to E-cadherin and its enhanced nuclear accumulation [26]. Given the inverse effect on outcome among TT vs. any G allele carriers of the RSPO2 rs555008 SNP depending on (K)RAS status we assume a well-balanced interplay between the RAS-RAF and the Wnt signaling pathways. While there are several lines of evidence that KRAS mutations induce upregulation of Wnt/Beta-catenin signaling [25,27] in colon cancer, literature regarding the influence of (K)RAS wild-type colon cancer on canonical Wnt signaling is scarce [27,28]. However, Horst et al could demonstrate that there is a correlation between nuclear Beta-catenin accumulation and KRAS status. Whereas immunohistochemical expression of Beta-catenin was significantly increased in KRAS mutant tumors, its staining intensity was less pronounced in KRAS wild-type tumors [28]. These findings indicate that even KRAS wild-type tumors might, albeit to a lesser degree compared to KRAS mutant tumors, directly stimulate Wnt signaling. A retrospective analysis of the AVF2197 trial demonstrated that the clinical benefit of first-line bevacizumab in mCRC patients is independent of KRAS mutation status [29]. Here we show that assessment of the RSPO2 rs555008 SNP according to the (K)RAS mutational status might help us to identify which subgroup of patients derive the most benefit from bevacizumab. Additionally, our results confirm once more that there is no “one size fits all” biomarker in mCRC and that they can differ according to the (K)RAS status (mutant versus wild-type). Just recently, we have learned from a pooled analysis of two phase III randomized trials (CRYSTAL and FIRE-3) that the location of the primary tumor has a predictive impact in RAS wild-type but not mutant patients [30]. While RAS wild-type patients with a left-sided primary tumor derive a greater benefit from cetuximab compared to bevacizumab-based chemotherapy, these associations could not be observed in RAS mutant patients [30]. Nowadays, several predictive markers such as RAS and BRAF mutational status, microsatellite status as well as sidedness guide our treatment decisions. The implementation of the RSPO2 rs555008 SNP into the treatment algorithm of mCRC may help us to identify in the future those RAS wild-type mCRC patients with left-sided primary tumors who might derive a benefit from antiangiogenic therapy with bevacizumab in the first-line setting. Additionally, assessment of the RSPO2 rs555008 SNP may help us to select those mCRC patients with a (K)RAS mutant primary tumor who will benefit most from bevacizumab-based treatment. In conclusion, the RSPO2 rs555008 SNP might serve as a predictive biomarker in mCRC patients treated with FOLFIRI and bevacizumab. While any G allele carriers of the RSPO2 rs555008 SNP with a (K)RAS wild-type tumor have a favourable outcome (OS), those harboring a (K)RAS mutant tumor have a worse outcome (PFS). Our results suggest that genotyping of the rs555008 polymorphism within the RSPO2 gene may help identify patients who will derive the most benefit from adding bevacizumab to irinotecan-based chemotherapy dependent on the (K)RAS mutational status. Targeting RSPO2 might be a promising approach to enlarge our treatment armamentarium against mCRC and to potentially overcome resistance to antiangiogenic therapies.
Supplementary Material
Highlights.
Markers predicting efficacy of bevacizumab in metastatic colon cancer are warranted
R-spondins play a role in angiogenesis and progression of colorectal cancer
R-spondins exert their oncogenic role through activation of the Wnt pathway
A polymorphism in RSPO2 predicts outcome in patients receiving FOLFIRI/bevacizumab
Potential to identify patients who will benefit most from FOLFIRI/bevacizumab
Acknowledgements
Martin D. Berger received a grant from the Werner and Hedy Berger-Janser Foundation for cancer research. This work was partly supported by the National Cancer Institute (grant number P30CA014089), the Gloria Borges Wunderglo Project, Dhont Family Foundation and Call to Cure. Yuji Miyamoto received a grant from the Japan Society for the Promotion of Science (S2606).
Funding source: Martin D. Berger received a grant from the Werner and Hedy Berger-Janser Foundation for cancer research. This work was partly supported by the National Cancer Institute (grant number P30CA014089), the Gloria Borges Wunderglo Project, Dhont Family Foundation and Call to Cure.
Role of the Funding Source
The Funding Sources had no influence on study design, data collection and analysis, decision to publish, and preparation of this manuscript.
Footnotes
Conflict of interest statement
The authors declare no conflict of interest regarding the content discussed in the manuscript.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Wyss J, Dislich B, Koelzer VH, Galvan JA, Dawson H, Hädrich M et al. Stromal PD-1/PD-L1 expression predicts outcome in colon cancer patients. Clin Colorectal Cancer. 2019;18(1):e20–38. [DOI] [PubMed] [Google Scholar]
- 2.Berger MD, Stintzing S, Heinemann V, Cao S, Yang D, Sunakawa Y et al. A Polymorphism within the Vitamin D Transporter Gene Predicts Outcome in Metastatic Colorectal Cancer Patients Treated with FOLFIRI/Bevacizumab or FOLFIRI/Cetuximab. Clin Cancer Res. 2018;24(4):784–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Berger MD, Lenz HJ. The safety of monoclonal antibodies for treatment of colorectal cancer. Expert Opin Drug Saf. 2016;15(6):799–808. [DOI] [PubMed] [Google Scholar]
- 4.Walther A, Johnstone E, Swanton C, Midgley R, Tomlinson I, Kerr D. Genetic prognostic and predictive markers in colorectal cancer. Nat Rev Cancer. 2009;9(7):489–99. [DOI] [PubMed] [Google Scholar]
- 5.De Lau W, Peng WC, Gros P, Clevers H. The R-spondin/Lgr5/Rnf43 module: regulator of Wnt signal strength. Genes Dev. 2014;28(4):305–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Krausova M, Korinek V. Wnt signaling in adult intestinal stem cells and cancer. Cell Signal. 2014;26(3):570–9. [DOI] [PubMed] [Google Scholar]
- 7.Bell SM, Schreiner CM, Wert SE, Mucenski ML, Scott WJ, Whitsett JA. R-spondin 2 is required for normal laryngeal-tracheal, lung and limb morphogenesis. Development. 2008;135(6):1049–58. [DOI] [PubMed] [Google Scholar]
- 8.Kazanskaya O, Glinka A, del Barco Barrantes I, Stannek P, Niehrs C, Wu W. R-Spondin2 is a secreted activator of Wnt/beta-catenin signaling and is required for Xenopus myogenesis. Dev Cell. 2004;7(4):525–34. [DOI] [PubMed] [Google Scholar]
- 9.Blaydon DC, Ishii Y, O’Toole EA, Unsworth HC, Teh MT, Rüschendorf F, et al. The gene encoding R-spondin 4 (RSPO4), a secreted protein implicated in Wnt signaling, is mutated in inherited anonychia. Nat Genet. 2006;38(11):1245–7. [DOI] [PubMed] [Google Scholar]
- 10.Kim KA, Wagle M, Tran K, Zhan X, Dixon MA, Liu S, et al. R-Spondin familymembers regulate the Wnt pathway by a common mechanism. Mol Biol Cell. 2008;19(6):2588–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hao HX, Jiang X, Cong F. Control of Wnt Receptor Turnover by R-spondin-ZNRF3/RNF43 Signaling Module and its Dysregulation in Cancer. Cancers. 2016;8(6). pii:E54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Seshagiri S, Stawiski EW, Durinck S, Modrusan Z, Storm EE, Conboy CB, et al. Recurrent R-spondin fusions in colon cancer. Nature. 2012;488(7413):660–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han T, Schatoff EM, Murphy C, Zafra MP, Wilkinson JE, Elemento O, et al. R-Spondin chromosome rearrangements drive Wnt-dependent tumour initiation and maintenance in the intestine. Nat Commun. 2017;8:15945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Madan B, Ke Z, Harmston N, Ho SY, Frois AO, Alam J, et al. Wnt addiction ofgenetically defined cancers reversed by PORCN inhibition. Oncogene. 2016;35(17):2197–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Storm EE, Durinck S, de Sousa e Melo F, Tremayne J, Kljavin N, Tan C, et al. Targeting PTPRK-RSPO3 colon tumours promotes differentiation and loss of stem-cell function. Nature. 2016;529(7584):97–100. [DOI] [PubMed] [Google Scholar]
- 16.Gore AV, Swift MR, Cha YR, Lo B, McKinney MC, Li W, et al. Rspo1/Wntsignaling promotes angiogenesis via Vegfc/Vegfr3. Development. 2011;138(22):4875–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stintzing S, Modest DP, Rossius L, Lerch MM, von Weikersthal LF, Decker T, et al. FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab for metastatic colorectal cancer (FIRE-3): a post-hoc analysis of tumour dynamics in the final RAS wild-type subgroup of this randomised open-label phase 3 trial. Lancet Oncol. 2016;17(10):1426–34. [DOI] [PubMed] [Google Scholar]
- 18.Loupakis F, Cremolini C, Masi G, Lonardi S, Zagonel V, Salvatore L, et al. Initialtherapy with FOLFOXIRI and bevacizumab for metastatic colorectal cancer. N Engl J Med. 2014;371(17):1609–18. [DOI] [PubMed] [Google Scholar]
- 19.Altman DG, McShane LM, Sauerbrei W, Taube SE. Reporting recommendations for tumor marker prognostic studies (REMARK): explanation and elaboration. BMC Med. 2012;10:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clevers H, Loh KM, Nusse R. Stem cell signaling. An integral program for tissuerenewal and regeneration: Wnt signaling and stem cell control. Science. 2014;346(6205):1248012. [DOI] [PubMed] [Google Scholar]
- 21.Zhan T, Rindtorff N, Boutros M. Wnt signaling in cancer. Oncogene.2017;36(11):1461–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Caruso M, Ferranti F, Corano Scheri K, Dobrowolny G, Ciccarone F, Grammatico P, et al. R-spondin 1/dickkopf-1/beta-catenin machinery is involved in testicular embryonicangiogenesis. PLoS One. 2015;10(4):e0124213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kazanskaya O, Ohkawara B, Heroult M, Wu W, Maltry N, Augustin HG, et al. TheWnt signaling regulator R-spondin 3 promotes angioblast and vascular development. Development. 2008;135(22):3655–64. [DOI] [PubMed] [Google Scholar]
- 24.Kannan L, Kis-Toth K, Yoshiya K, Thai TH, Sehrawat S, Mayadas TN, et al. R-spondin3 prevents mesenteric ischemia/reperfusion-induced tissue damage by tightening endothelium and preventing vascular leakage. Proc Natl Acad Sci USA. 2013;110(35):14348–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Janssen KP, Alberici P, Fsihi H, Gaspar C, Breukel C, Franken P, et al. APC andoncogenic KRAS are synergistic in enhancing Wnt signaling in intestinal tumor formation and progression. Gastroenterology. 2006;131(4):1096–109. [DOI] [PubMed] [Google Scholar]
- 26.Li J, Mizukami Y, Zhang X, Jo WS, Chung DC. Oncogenic K-ras stimulates Wntsignaling in colon cancer through inhibition of GSK-3beta. Gastroenterology. 2005;128(7):1907–18. [DOI] [PubMed] [Google Scholar]
- 27.Moon BS, Jeong WJ, Park J, Kim TI, Min do S, Choi KY. Role of oncogenic K-Ras in cancer stem cell activation byaberrant Wnt/β-catenin signaling. J Natl Cancer Inst. 2014;106(2):djt373 [DOI] [PubMed] [Google Scholar]
- 28.Horst D, Chen J, Morikawa T, Ogino S, Kirchner T, Shivdasani RA. DifferentialWNT activity in colorectal cancer confers limited tumorigenic potential and is regulated by MAPK signaling. Cancer Res. 2012;72(6):1547–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hurwitz HI, Yi J, Ince W, Novotny WF, Rosen O. The clinical benefitof bevacizumab in metastatic colorectal cancer is independent of K-ras mutation status: analysis of a phase III study of bevacizumab with chemotherapy in previously untreated metastatic colorectal cancer. Oncologist. 2009;14(1):22–8. [DOI] [PubMed] [Google Scholar]
- 30.Tejpar S, Stintzing S, Ciardiello F, Tabernero J, Van Cutsem E, Beier F, et al. Prognostic and Predictive Relevance of Primary Tumor Location in Patients With RAS Wild-Type Metastatic Colorectal Cancer: Retrospective Analyses of the CRYSTAL and FIRE-3 Trials. JAMA Oncol. 2017;3(2):194–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


