Abstract
Optimal breastfeeding practices can ensure healthy growth and development of infants, which in the long term can impact the country's economic development. Nevertheless, Myanmar has yet to achieve the WHO’s target of 70% for early initiation of breastfeeding, and the country’s target of 90% for exclusive breastfeeding. The purpose of this study was to assess the associations between early initiation of breastfeeding and exclusive breastfeeding and bio-demographic, socio-economic and behavioral factors in Myanmar. Using the 2015–2016 Myanmar Demographic and Health Survey, the analysis of early initiation of breastfeeding was based on a sample of 1,506 under-2 children and the analysis of exclusive breastfeeding was based on a sample of 376 children aged 0–5 months. Multiple logistic modeling, with heteroskedasticity-adjusted standard errors, was used. The prevalence rates of early initiation of breastfeeding and exclusive breastfeeding in the study were 67.9% and 52.2% respectively. Having a vaginal delivery (AOR = 2.5; 95% CI = 1.7–3.7) and having frequent (≥ 4) antenatal visits (AOR = 2.4; 95% CI = 1.5–3.8) were associated with higher odds of early initiation of breastfeeding. Having a postnatal checkup (AOR = 0.5; 95% CI = 0.3–0.9) and having an infant that was perceived to be small at birth (AOR = 2.5; 95% CI = 1.1–5.7, for infants perceived to be large at birth) were significantly associated with decreased odds of exclusive breastfeeding. In order to promote optimal breastfeeding practices, this study suggested that delivery and quality of health services during pregnancy need to be strengthened in Myanmar.
Introduction
Early initiation of breastfeeding (EIBF) is defined as breastfeeding within the first hour after giving birth. Exclusive breastfeeding (EBF) is defined as the exclusive provision of breast milk (without water, other liquids or milk substitutes, with the exception of oral rehydrated solution, drops of vitamins, minerals or medicines) to infants aged between 0–5 months. Both EIBF and EBF represent important infant and young child feeding (IYCF) indicators, according to the WHO [1–4].
Suboptimal breastfeeding practices have adverse consequences particularly in low- and middle-income countries (LMICs) [5–8]. They have been associated with increased risks of neonatal [9] and under-five mortality [6, 9], accounting for more than 0.8 million deaths among children in LMICs annually [8]. They have also been linked to lower intelligence [6] and poor health outcomes later in life [6, 8] including higher risks of infectious morbidity and mortality [6, 7], diabetes [6] and stunting [1, 8, 10], leading to economic costs of approximately 302 billion US dollars per year globally [11]. These consequences of suboptimal breastfeeding may persist and play a role in perpetuating health and socioeconomic inequalities across generations. For example, stunting among women of reproductive age has been associated with increased risks of poor perinatal outcomes in their children [8], and lower intelligence is known to impact school and labor market performance [6, 8], which affects the individual’s socioeconomic status and that of his/her offspring.
Despite clear benefits, optimal breastfeeding practices have not been widely adopted. In 2016, UNICEF reported that, globally, only two-fifths of infants under 6 months of age received EBF and less than half (45%) were brought to their mothers for breastfeeding initiation within one hour after birth [1]. In LMICs, it has been reported that 37% of infants received EBF and less than 50% were breastfed within the first hour of their lives [6].
Suboptimal breastfeeding is a problem in Myanmar. The IYCF practices have been incorporated into the National Strategy since 2011 and the Baby Friendly Hospital Initiative (BFHI) has been implemented in Myanmar since 2010 [12]. Nevertheless, the country has not achieved its goals whereby 70% of infants are expected to receive EIBF [13] and 90% are expected to receive EBF [14]. The EBF prevalence seems to have increased over time yet it remains below than the target. In 2016, half (51%) of the infant population under the age of six months received EBF [15], compared to 23.6% in 2011 [16]. The average duration of EBF was 2.3 months in 2016 [15]. The EBF prevalence was relatively high in the first month and dropped dramatically as infants became older, falling to 38% when infants reached 4–5 months of age. EIBF, on the other hand, seems to have experienced a declining trend in Myanmar. The proportion of mothers who provided EIBF was 66.8% in 2015–2016 [15], compared to 75.8% in 2011 [17]. The low breastfeeding prevalence is reflected in poor child health, with neonatal, infant and under-five mortality being comparatively high at the rates of 23.1, 36.8 and 46.2 per 1000 live births respectively in 2018, according to the World Development Indicators database.
A deeper understanding of the mechanisms behind the decisions to provide EIBF and EBF is needed so that programs to encourage optimal breastfeeding practices can be more effectively designed. Existing studies from Myanmar have identified determinants of breastfeeding practices, which include the mother’s socioeconomic characteristics (e.g. area of residence, education, occupation, and economic status) as well as the extent to which the mother utilized maternal health services during the course of her pregnancy (e.g. number of antenatal care (ANC) visits, place of delivery and receipt of breastfeeding knowledge) [12, 18, 19]. The determinants that have been found to be statistically significant in Myanmar studies are consistent with those identified in studies from other LMICs [20–23]. Nevertheless, most Myanmar studies use region-specific (as opposed to nationally representative) data and focus on only EBF [12, 18, 19]. To fill the gap, this study aims to uncover determinants of both EBF and EBIF in Myanmar using the latest nationally representative survey collected in 2015–2016.
Materials and methods
Data source
This study used a cross-sectional study design. It used data from the first DHS survey in Myanmar: the 2015–2016 Myanmar Demographic and Health Survey (MDHS). A two-stage stratified cluster sampling method was used in the MDHS, using the 2014 Census as the sampling frame [24]. The first stage involved the identification of clusters, which in the MDHS referred to enumeration areas or ward/village tracts. The second stage involved the use of equal-probability systematic sampling to select households within each cluster. Given the response rate of 98%, the MDHS covered 12,500 households, whose information was collected during December 2015—July 2016 [15].
Sample selection
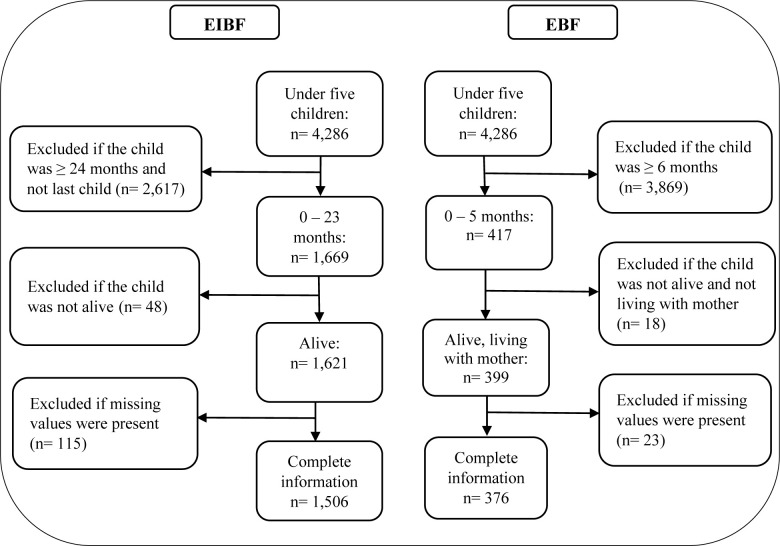
The outcomes in the study, i.e. EIBF and EBF, were investigated using different samples. The exclusion criteria were (1) children outside the age cut-offs associated with EIBF and EBF in accordance with the WHO’s guidelines [2, 3], (2) children were deceased at the time of the interview and (3) children for whom information on the variables in the empirical model (explained below) was missing. The unit of analysis was the mother-child pair (from the same household).
The EIBF sample consisted of 1,506 observations, covering last-born children aged 0–23 months. The construction of the EIBF sample involved removing 48 and 115 observations of under-two children who had been deceased and who had missing information on variables in the model respectively.
The EBF sample contained 376 observations, all of whom were children aged 0–5 months living with their mothers. Since the definition of EBF pertained to children younger than 5 months old, the construction of the EBF sample involved excluding 1,252 children who were 6–23 months old, 18 children who had been deceased or were not currently living with their mothers, and 23 children with missing information on variables included in the model. The step-by-step sample selection processes for both samples were illustrated in Fig 1.
Fig 1. Inclusion and exclusion criteria of the early initiation of breastfeeding and the exclusive breastfeeding samples.
Outcome variables
Both EIBF and EBF were operationalized as binary variables. The EIBF variable was based on the question: “How long after birth did you first put (name) to the breast?”. It took the value of 1 if breastfeeding was initiated within the first hour, and 0 otherwise.
The EBF variable was based on the following questions: “Are you still breastfeeding (name)?”, “Did (name) drink anything from a bottle with a nipple yesterday or last night (24 hours preceding the interview)?”, and “Any kind of milk (other than breast milk)?”. It took the value of 1 if the infant received breast milk exclusively, and 0 otherwise.
Explanatory variables
The explanatory variables were categorized into three groups, including bio-demographic, socio-economic and behavioral factors. The categorization was consistent with the framework used in existing studies [25, 26], and was adopted on the grounds that the referenced studies were based on Nigeria, which was an LMIC with socioeconomic settings that were comparable to Myanmar, and used data from a Demographic and Health Survey (DHS), similar to this study. The selection of the explanatory variables followed existing studies in Myanmar [12, 18, 19] and other LMICs, using DHS data [20–23]. It was also consistent with a broader conceptual framework developed by Rollins et al. [11]. This study included mother and infant attributes (individual factors), socioeconomic factors and behavioral factors (which addressed interactions between mothers and their health-related and work-related environments) as well as area-level (bio-demographic) variables, which partially captured differences in sociocultural attitudes and market factors faced by women in different geographical locations throughout the country.
All three groups of explanatory variables were hypothesized to be associated with EIBF and EBF. Bio-demographic factors referred to attributes of the mother, the child and the area of residence. Examples included age and gender of the child, the mother’s perception of the child’s birth size and the household’s region of residence. Socio-economic factors referred to household-level socioeconomic status indicators. They included the mother’s education and work status as well as the household’s economic status. Finally, behavioral factors referred to the pattern of maternal health services utilization by the mother. They encompassed ANC visits, mode and place of delivery, and postnatal checkup. The model for EBF included all of the above explanatory variables. In the EIBF model, certain variables—specifically, the child’s age and the receipt of postnatal checkup—were not accounted for because they were not related to the outcome, occurring after EIBF was determined.
Statistical analysis
First, the data were explored. Descriptive statistics were presented as counts and percentages. Simple logistic regressions were performed, with each outcome being regressed on a single explanatory variable. Sampling weights were accounted for in order to ensure national representativeness. Results for the simple logistic regressions were expressed as crude odds ratios (COR), accompanied by 95% confidence intervals (CI). The bivariate analyses provided an implication as to whether a given explanatory variable was likely to be statistically significant in multiple logistic regressions and how alternative regression specifications could be formed.
Multiple logistic regressions were undertaken, taking into account sampling weights. The results were expressed as adjusted odds ratios (AOR) along with their 95% CIs. Three multiple logistic regression specifications, denoted as Model 1, Model 2 and Model 3, were explored. In Model 1, only bio-demographic factors were controlled for. In Model 2, socio-economic factors were added, and, in Model 3, all three groups of factors (including additionally behavioral factors) were included. The three models were compared, using likelihood ratio tests, and the model with the best fit was identified and discussed. Despite the fact that the simple logistic regressions (discussed below) suggested that some of the explanatory variables were not strong predictors of EBF and/or EIBF, this study included all explanatory variables anyway. The purpose was to ensure that the specifications were theoretically (as opposed to empirically) informed and that specification bias was reduced. It should also be noted that empirically-motivated specifications (whereby different combinations of variables that were statistically significant in the bivariate analyses were included in the multiple logistic model) produced results that were largely consistent with the preferred model below and therefore were not reported to conserve space.
Also, possible violations of the regression assumptions were considered. Multicollinearity was investigated using a simple correlation matrix. It was found that the variables had pairwise correlations that were low (below 0.6) and not statistically significant. Heteroskedasticity was tested using Breusch-Pagan tests, which provided evidence of heteroskedasticity at the 1% level for both EIBF and EBF. The problem was addressed through the use of Huber-White standard errors. All statistical analyses were carried out using Stata version 14.0.
Ethical consideration
Ethics clearance was not sought since the study was based on secondary data that were publicly available on the DHS website.
Results
Descriptive statistics
Table 1 shows descriptive statistics of the outcome and the explanatory variables in the model. Among under-2 children in the EIBF sample (n = 1,506), 1,023 children or approximately 67.9% were breastfed within the first hour of birth. Children with the 2nd– 4th birth rank had the highest proportion of EIBF, with 533 out of 774 of them (71.4%) having been breastfed within the first hour of birth. The EIBF prevalence varied across regions, with the highest rate in the hilly region and the lowest rate in the coastal region (72.6% versus 44.7%). Compared to the respective comparison groups, the EIBF prevalence was noticeably higher among children with the 2nd– 4th birth rank (71.4%) and among mothers who had at least 4 antenatal care visits (70.7%) and those who had vaginal births (71.1%).
Table 1. Frequency and prevalence of EIBF and EBF by explanatory variables.
| Variables | EIBF Sample (n = 1,506) | EBF sample (n = 376) | ||
|---|---|---|---|---|
| n (%), receiving EIBF | n, variable break-down | n (%) receiving EBF | n, variable break-down | |
| Outcome variables | ||||
| EIBF | ||||
| Not within 1st hour | 483 | |||
| Within 1st hour | 1023 | |||
| EBF | ||||
| Non-EBF | 180 | |||
| EBF | 196 | |||
| Bio-demographic factors | ||||
| Child’s age (months) | ||||
| 0–1 | 64 (72.0) | 88 | ||
| 2–3 | 79 (53.4) | 149 | ||
| 4–5 | 53 (38.2) | 139 | ||
| Sex of child | ||||
| Male | 536 (66.3) | 809 | 85 (41.9) | 204 |
| Female | 487 (69.8) | 697 | 111 (64.3) | 172 |
| Mother’s age (years) | ||||
| 15–19 | 46 (74.2) | 62 | 12 (54.8) | 22 |
| 20–34 | 748 (67.5) | 1108 | 148 (52.3) | 283 |
| 35–49 | 229 (68.0) | 336 | 36 (50.8) | 71 |
| Mother's perception of birth size | ||||
| Small | 125 (61.3) | 205 | 19 (30.2) | 64 |
| Average | 633 (70.2) | 901 | 120 (57.6) | 209 |
| Large | 265 (66.1) | 401 | 57 (54.7) | 103 |
| Birth order | ||||
| 1st rank | 350 (63.3) | 553 | 78 (51.8) | 151 |
| 2nd– 4th rank | 553 (71.4) | 774 | 98 (53.4) | 184 |
| > = 5th rank | 120 (66.9) | 179 | 20 (47.8) | 41 |
| Place of residence | ||||
| Urban | 274 (71.0) | 385 | 52 (53.5) | 97 |
| Rural | 749 (66.9) | 1121 | 144 (51.7) | 279 |
| Region of residence | ||||
| Hilly | 249 (72.6) | 343 | 45 (54.2) | 84 |
| Coastal | 69 (44.7) | 153 | 17 (38.9) | 43 |
| Delta | 375 (68.6) | 548 | 68 (56.0) | 121 |
| Dry | 330 (71.5) | 462 | 66 (51.7) | 128 |
| Socio-economic factors | ||||
| Mother’s education | ||||
| No education | 160 (70.3) | 227 | 29 (44.8) | 64 |
| Primary | 447 (67.8) | 660 | 75 (49.9) | 151 |
| Secondary | 332 (68.1) | 487 | 64 (54.3) | 18 |
| > Secondary | 84 (63.8) | 132 | 28 (64.9) | 43 |
| Mother’s occupation | ||||
| Not working | 456 (69.1) | 660 | 96 (49.5) | 193 |
| Working | 567 (67.1) | 846 | 100 (54.9) | 183 |
| Economic status | ||||
| Poorest | 266 (66.1) | 402 | 51 (52.8) | 96 |
| Poorer | 205 (64.3) | 319 | 29 (40.9) | 72 |
| Middle | 180 (70.2) | 256 | 35 (54.6) | 63 |
| Richer | 189 (69.1) | 273 | 37 (50.8) | 74 |
| Richest | 183 (71.6) | 256 | 44 (61.9) | 71 |
| Behavioral factors | ||||
| ANC visits | ||||
| None | 92 (57.97) | 159 | 23 (44.1) | 52 |
| 1–3 | 285 (65.8) | 433 | 44 (45.6) | 96 |
| 4 and above | 646 (70.7) | 914 | 129 (56.8) | 228 |
| Mode of delivery | ||||
| Caesarean section | 188 (56.6) | 332 | 53 (55.9) | 96 |
| Vaginal delivery | 835 (71.1) | 1174 | 143 (50.9) | 280 |
| Place of delivery | ||||
| Home | 554 (69.3) | 780 | 103 (51.1) | 202 |
| Health facility | 469 (66.4) | 706 | 93 (53.4) | 174 |
| Postnatal checkup | ||||
| Yes | 71 (43.4) | 163 | ||
| No | 125 (58.9) | 213 | ||
(1) Sampling weights were accounted for in the estimation
(2) ANC = Antenatal care.
Among children aged 0–5 months in the EBF sample (n = 376), 196 children or approximately 52.2% were currently exclusively breastfed. Table 1 suggests that the highest EBF prevalence occurred among children aged 0–1 months and the lowest EBF prevalence was observed among children aged 4–5 months (72.0% versus 38.2%). The EBF prevalence was also highest among children who were perceived as having an average size at birth (57.6%), among female infants (64.3%), and among mothers who had not had a postnatal checkup (58.9%).
Regression analyses
The results of simple logistic regressions in terms of COR are presented in S1 Table in the appendix. EIBF was found to be significantly and positively associated with the average perceived birth size, the 2nd– 4th birth order, having had 4 or more ANC visits and having had a vaginal delivery. It was significantly and negatively associated with having residence in the coastal region. On the other hand, EBF was found to be significantly and positively associated with the fact that the infant was female and that he/she had average or large perceived birth sizes. It was also significantly and negatively associated with age of the child and the uptake of postnatal checkup. These results provided a benchmark against which robustness of the preferred multiple logistic regressions could be assessed. If the explanatory variables that were identified as statistically significant in the simple logistic regressions were indeed associated with the outcome variables, then they should remain statistically significant when more factors were controlled for in multiple logistic regressions.
As discussed in the Statistical Analysis sub-section, three different specifications, denoted as Models 1, 2 and 3, were explored. Model 1, containing only the bio-demographic factors, was nested completely within Model 2, which contained the bio-demographic and the socio-economic factors. Model 2 was nested completely within Model 3, where all three groups of factors were controlled for. Performed prior to the heteroskedasticity adjustment, likelihood ratio tests suggested that Model 3 provided a better fit than Model 2 (with the p-values of 0.000 for EIBF and 0.037 for EBF) as well as Model 1 (with the p-values of 0.000 for EIBF and 0.008 for EBF). Model 3 was therefore preferred. Results of Model 1 and 2 are shown in S2 Table in the Appendix. The results suggested that conclusions that may be drawn from this study were insensitive/ robust to specification changes.
Table 2 presents results of the preferred multiple logistic regression model (Model 3). The results were expressed in terms of AOR and 95% CIs based on heteroskedasticity-adjusted standard errors. The odds of EIBF were significantly and positively associated with the 2nd– 4th birth order (AOR = 1.4), having had 4 or more ANC visits (AOR = 2.4), and having had a vaginal delivery (AOR = 2.5). The odds of EIBF were significantly and negatively associated with the coastal region (AOR = 0.3).
Table 2. Adjusted odds ratios from preferred multiple logistic regressions of EIBF and EBF.
| Variables | EIBF [n = 1,506] | EBF [n = 376] | ||
|---|---|---|---|---|
| AOR [95%CI] | p-value | AOR [95%CI] | p-value | |
| Bio-demographic factors | ||||
| Child’s age (months) (0–1 = reference category) | ||||
| 2–3 | 0.3 [0.2–0.7] | 0.002 | ||
| 4–5 | 0.2 [0.1–0.4] | 0.000 | ||
| Sex of child (Female) | 1.2 [0.9–1.6] | 0.120 | 3.0 [1.8–5.4] | 0.000 |
| Mother’s age (years) (15–19 = reference category) | ||||
| 20–34 | 0.6 [0.3–1.3] | 0.235 | 0.6 [0.2–2.0] | 0.427 |
| 35–49 | 0.6 [0.3–1.4] | 0.242 | 0.3 [0.1–1.3] | 0.115 |
| Perception of birth size (Small = reference category) | ||||
| Average | 1.3 [0.9–2.0] | 0.129 | 2.6 [1.2–5.4] | 0.014 |
| Large | 1.1 [0.7–1.7] | 0.683 | 2.5 [1.1–5.7] | 0.034 |
| Birth order (1st rank = reference category) | ||||
| 2nd– 4th rank | 1.4 [1.0–1.9] | 0.035 | 1.5 [0.8–2.9] | 0.205 |
| > = 5th rank | 1.3[0.8–2.2] | 0.334 | 1.7 [0.6–5.0] | 0.336 |
| Place of residence (Rural) | 0.8 [0.6–1.2] | 0.291 | 1.9 [0.8–4.4] | 0.166 |
| Region of residence (Hilly = reference category) | ||||
| Coastal | 0.3 [0.2–0.5] | 0.000 | 0.4 [0.2–1.1] | 0.070 |
| Delta | 0.8 [0.5–1.1] | 0.204 | 0.7 [0.3–1.4] | 0.292 |
| Dry | 1.0 [0.7–1.5] | 0.985 | 0.6 [0.3–1.2] | 0.135 |
| Socio-economic factors | ||||
| Mother’s education (No education = reference category) | ||||
| Primary | 0.8 [0.5–1.2] | 0.290 | 1.7[0.7–3.9] | 0.230 |
| Secondary | 0.7 [0.4–1.2] | 0.174 | 1.8 [0.7–4.7] | 0.215 |
| > Secondary | 0.6 [0.3–1.2] | 0.146 | 3.0[0.9–10.6] | 0.081 |
| Mother’s occupation (Working) | 0.8 [0.6–1.1] | 0.209 | 1.3 [0.7–2.2] | 0.374 |
| Economic status (Poorest = reference category) | ||||
| Poorer | 0.8 [0.6–1.2] | 0.335 | 0.4 [0.2–1.0] | 0.041 |
| Middle | 1.1 [0.7–1.8] | 0.557 | 0.9 [0.4–2.2] | 0.844 |
| Richer | 1.1 [0.7–1.7] | 0.813 | 0.9 [0.4–2.4] | 0.876 |
| Richest | 1.3 [0.8–2.4] | 0.309 | 1.4 [0.4–4.8] | 0.545 |
| Behavioral factors | ||||
| ANC visits (None = reference category) | ||||
| 1–3 | 1.6 [1.0–2.5] | 0.053 | 1.0 [0.3–2.5] | 0.935 |
| 4 and above | 2.4 [1.5–3.8] | 0.000 | 1.9 [0.7–5.3] | 0.187 |
| Mode of delivery (Vaginal delivery) | 2.5 [1.7–3.7] | 0.000 | 0.8 [0.4–1.8] | 0.603 |
| Place of delivery (Health facility) | 1.1 [0.7–1.5] | 0.709 | 0.7 [0.3–1.5] | 0.362 |
| Postnatal checkup (Yes) | 0.5 [0.3–0.9] | 0.022 | ||
(1) AOR = adjusted odds ratios
(2) Robust standard errors were used in the calculation of the 95% CIs
(3) Sampling weights were accounted for in the estimation
(4) ANC = Antenatal care.
As for EBF, the preferred multiple logistic regression model showed that infants aged 2–3 months (AOR = 0.3) and 4–5 months (AOR = 0.2) were less likely to be breastfed exclusively compared with those aged 0–1 months. Being a female infant was associated with a 3 times higher likelihood of receiving EBF, compared to being male (AOR = 3.0). The odds of EBF were higher among mothers who perceived their babies to be of an average size (AOR = 2.6) or a large size (AOR = 2.5). Mothers that belonged to the poorer economic group had lower odds of EBF, compared to those belonged to the poorest group (AOR = 0.4). The receipt of a postnatal checkup was associated with lower EBF odds (AOR = 0.5). With the exception of economic status which was found to be statistically insignificant in the simple logistic regression for EBF, the results of simple and multiple logistic regression analyses for both EIBF and EBF were consistent.
Discussion
Using the latest nationally representative survey and multiple logistic regression modeling, this study identified determinants of EIBF and EBF in Myanmar. The study was motivated partially by the high rates of infant mortality in the country as well as the rationale of the 1989 United Nations convention (whereby breastfeeding is considered a right, to which children are entitled, and the government is encouraged to provide access to optimal breastfeeding for children) [27].
Approximately 67.9% of the sample, consisting of under-2 children, received EIBF in 2015–2016. The EIBF prevalence in the sample differed from what was reported by the MDHS at 66.8% [15]. This was because, in the sample selection process, deceased children as well as those whose information on personal and household characteristics was incomplete were excluded. By international standards, the rate of almost 70% was considered satisfactory [28]. It was comparable with other countries with the same level of economic development, e.g. Namibia and Nepal [22, 29] and was higher than what was recently observed in Bangladesh (51%) [30]. The similarity in the practices of EIBF (and EBF) among LMICs was expected; determinants of breastfeeding practices, which included structural factors (i.e., sociocultural and market factors), the environment/settings in which one lived, and individual attributes [11], were likely to be quite similar among LMICs.
While EIBF was not significantly associated with the socio-economic factors, it was associated with some of the bio-demographic factors. Higher birth order was found to be positively associated with EIBF, consistent with an existing study conducted in Nigeria [25]. It is possible that multiparous mothers produce colostrum and breast milk earlier than nulliparous ones and are able to provide EIBF more easily [31]. Also, residing in the coastal region in Myanmar was found to be negatively associated with EIBF. Compared to other regions, the coastal region is more geographically dispersed, resulting in increased transportation difficulties, lack of obstetric care providers and lack of sustainability in the provision of neonatal care.
EIBF was also associated with some of the behavioral factors. First, caesarean section was found to be inversely associated with EIBF. A similar conclusion was reached in studies conducted in Ethiopia, Namibia and Turkey [21, 22, 32]. A possible explanation is that, as a procedure, caesarean section is more time-consuming and more complicated than vaginal delivery and mothers who undergo caesarean section may experience a higher degree of fatigue and are unable to breastfeed within the first hour [1].
Also, lack of or infrequent ANC (0–3) visits was inversely associated with EIBF. The importance of ANC visits for EIBF is mixed in the literature, with positive effects found in studies based in South Asia, Nigeria and Nepal [23, 25, 29], and negative effects documented in a study based in Namibia [22]. The positive impact of ANC visits on EIBF observed here may be explained by the fact that, through ANC visits and interactions with health care professionals, mothers may learn to better appreciate the benefits of optimal breastfeeding practices and therefore adopt EIBF.
In order to promote EIBF in Myanmar, maternal health services need to be strengthened. Given that caesarean section was found to be inversely associated with EIBF, it is suggested that causes of redundant caesarean delivery be identified, specific guidelines and indications for caesarean section be strengthened, and women be encouraged to take the vaginal delivery option whenever possible. Also, it is suggested that the Baby Friendly Hospital Initiative (BFHI) program, which is already implemented in Myanmar, be scaled up. In particular, as existing studies have found a positive dose-response relationship between BFHI and breastfeeding practices [33], the number of baby-friendly hospitals should be expanded and health professionals should be provided with on-the-job training as to how to inform mothers about the benefits of EIBF and how to effectively provide breastfeeding support [27, 28].
With regard to EBF, this study found that 52.2% of infants aged 0–5 months in the sample received exclusive breastfeeding in 2015–2016. The figure was consistent with the MDHS report [15] if/when the same age group was considered. It was also in line with the minimum recommended WHO’s target of 50%, but was lower than the target of 90% set by the country itself [14, 34]. Also, the rate was found to be higher than what was discovered in a 2015 study based in one region in Myanmar (15%) [18], higher than what was found in a Nigerian study (16.4%), and lower than a Nepalese study conducted in 2011 (66.3%) [20, 35]. The comparison suggested that there was a wide variation of EBF rates even among LMICs.
EBF was found to be associated with some of the bio-demographic factors. First, age of the child was negatively associated with EBF, consistent with existing studies from other countries [35–37]. This likely reflects the general misbelief that breast milk alone cannot provide sufficient nutrients for infant growth and development [12]. It suggests that there is a need to inform mothers and caregivers, through a public platform (including, for example, ANC visits), about advantages of EBF and to assure them that breast milk is sufficient for babies up to six months of age.
EBF was found to be significantly related with sex and the perceived birth size of the child. In this study, female infants were found to have a higher chance of receiving EBF compared with male infants. A similar conclusion was reached in studies conducted in Nigeria and Vietnam [20, 36], yet a study in India suggested that male infants were more likely to receive EBF [23]. The difference may stem at least partially from cultural norms, which dictate certain gender preference, that vary across countries. Also, this study showed that infants perceived as having a large size at birth (and correspondingly a higher perceived likelihood of infant survival) were more likely to receive EBF, consistent with studies conducted in South Asia and India [23, 37].
Unlike EIBF, EBF was found to be significantly associated with one socioeconomic factor, i.e., economic status of the household. It was found that mothers that belonged to poorer households had a lower probability of providing EBF, compared to those in the poorest category as well as richer households. Evidence for the association between economic status and EBF was nevertheless mixed in the literature [12, 18, 19, 38].
Finally, it was found that the receipt of postnatal checkup, as one of the behavioral factors, reduced the probability of EBF. This finding was consistent with a study conducted in Indonesia [38]. The negative association may be explained by the fact that children who do not receive EBF are more likely to have health problems (e.g. diarrhea) and may be more likely to seek postnatal care.
In order to promote EBF in Myanmar, campaigns to encourage mothers to provide EBF, regardless of socioeconomic status or gender and size of the child, should be considered. Moreover, given that EBF was positively associated with larger perceived size of infants, programs for pregnancy diet and nutrition, e.g. nutrition counseling and prenatal meal planners, should be developed. Impacting health and growth of infants and consequently their perceived sizes, pregnancy diet and nutrition programs should be implemented at the community level so that differences in community-specific food cultures can be accounted for [8].
This study made at least two contributions. First, based on the latest MDHS and accounting for survey weights, the results were nationally representative and the conclusions should be generalizable in the context of Myanmar. Second, this study represented the first nationwide study to investigate both EIBF and EBF practices.
Limitations existed in the study. First, since the study design was cross-sectional, it was not possible to address causality between the outcome variables and the explanatory variables. Also, since the MDHS data in this study were collected retrospectively, potential recall bias might have been present due to memory decay of the respondents. There was also a possibility of social desirability bias because all answers concerning breastfeeding practices by the mothers were self-reported and some of the questions may be deemed culturally sensitive, impacting the accuracy of the responses.
Conclusions
Myanmar needs to improve the nutritional status of children and reduce infant and under-five mortality rates. The prevalence of optimal breastfeeding practices is currently below the national targets. This study identified a number of important determinants of both EIBF and EBF. As for EIBF, it was found that prior utilization of maternal and child health services was associated with an increased likelihood of EIBF. The implication is that maternal and child health services should be scaled up [28], as they play a crucial role in improving the nutrition level and wellbeing of children. In particular, the number of baby-friendly hospitals should be expanded and health professionals should be provided with on-the-job training and evaluated to ensure the quality of services regarding breastfeeding support [28]. Specific guidelines and indications for caesarean section should also be strengthened since unnecessary caesarean sections are inversely associated with EIBF. As for EBF, this study found that EBF varied with perception of mothers regarding the size of their infants. Community health education programs on pregnancy diet and nutrition, which impact health and growth of the infant [8], are likely to be crucial for the promotion of EBF.
Supporting information
(PDF)
(PDF)
Acknowledgments
The authors are thankful to the Demographic and Health Survey (DHS) program for making the data available. We would like to thank the faculty members at the M.Sc. program for Health Economics and Health Care Management, Faculty of Economics, Chulalongkorn University, for their inputs during the conceptualization of this study. Finally, we would like to thank the reviewers for their valuable and constructive comments.
Data Availability
The data set used in this study is Myanmar Demographic and Health Surveys (DHS) which are publicly available and can be downloaded from the DHS Program’s website (URL:http://www.dhsprogram.com/). The DHS Program is a project funded by USAID and implemented by ICF. So, anyone who is interested can download the data set directly from the website after request proposal.
Funding Statement
The authors received no specific funding for this work.
References
- 1.UNICEF. From the first hour of life: Making the case for improved infant and young child feeding everywhere. New York: United Nations Children's Fund; 2016. [Google Scholar]
- 2.WHO, UNICEF, USAID, AED, UCDAVIS, IFPRI. Indicators for Assessing Infant and Young Child Feeding Practices: Part 1 Definitions. WHO; 2008. [Cited 2019 June 20]. Available from: https://www.who.int/nutrition/publications/infantfeeding/9789241596664/en/ [Google Scholar]
- 3.WHO. Evidence for the ten steps to successful breastfeeding. Geneva: World Health Organization; 1998. [Google Scholar]
- 4.UNICEF. Programming guide: infant and young child feeding. New York: United Nations Children’s Fund; 2012. [Google Scholar]
- 5.Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet. 2012;380(9859):2224–2260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, et al. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017):475–490. [DOI] [PubMed] [Google Scholar]
- 7.Khan J, Vesel L, Bahl R, Martines JC. Timing of breastfeeding initiation and exclusivity of breastfeeding during the first month of life: effects on neonatal mortality and morbidity—a systematic review and meta-analysis. Maternal and Child Health Journal. 2015;19(3):468–479. 10.1007/s10995-014-1526-8 [DOI] [PubMed] [Google Scholar]
- 8.Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, de Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. The Lancet. 2013;382(9890):427–451. [DOI] [PubMed] [Google Scholar]
- 9.Smith ER, Hurt L, Chowdhury R, Sinha B, Fawzi W, Edmond KM, et al. Delayed breastfeeding initiation and infant survival: a systematic review and meta-analysis. PLOS ONE. 2017;12(7):e0180722 10.1371/journal.pone.0180722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Onis M, Branca F. Childhood stunting: a global perspective. Maternal & Child Nutrition. 2016;12(S1):12–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rollins NC, Bhandari N, Hajeebhoy N, Horton S, Lutter CK, Martines JC, et al. Why invest, and what it will take to improve breastfeeding practices? The Lancet. 2016;387(10017):491–504. [DOI] [PubMed] [Google Scholar]
- 12.Thet MM, Khaing EE, Diamond-Smith N, Sudhinaraset M, Oo S, Aung T. Barriers to exclusive breastfeeding in the Ayeyarwaddy Region in Myanmar: qualitative findings from mothers, grandmothers, and husbands. Appetite. 2016;96:62–69. 10.1016/j.appet.2015.08.044 [DOI] [PubMed] [Google Scholar]
- 13.WHO, UNICEF. Tracking Progress for Breastfeeding Policies and Programmes: Global Breastfeeding Collective; Global Breastfeeding Scorecard. WHO; 2017. [Cited 2020 May 1]. Available from: https://www.who.int/nutrition/publications/infantfeeding/global-bf-scorecard-2017/en/ [Google Scholar]
- 14.Nilsen A. Myanmar takes First Public Steps to Fight Breast Milk Substitute. Save the Children. 2018. April 4 [Cited 2019 June 20]. Available from: https://campaigns.savethechildren.net/blogs/andynilsen/myanmar-takes-first-public-steps-fight-breast-milk-substitute [Google Scholar]
- 15.Ministry of Health and Sports, DHS Program. Myanmar Demographic and Health Survey 2015–16. DHS. 2017 March. [Cited 2019 April 11]. Available from: https://dhsprogram.com/pubs/pdf/FR324/FR324.pdf
- 16.WHO, UNICEF. Multiple Indicator Cluster Surveys (MICS). Five-Year Strategic Plan for Child Health Development in Myanmar (2010–2014). WHO; 2011. [Cited 2019 April 11]. Available from: https://www.burmalibrary.org/docs21/Five%20year%20Strategic%20Plan%20for%20child%20health%20development%20Myanmar%202010-2014-red.pdf [Google Scholar]
- 17.Ministry of National Planning and Economic Development, Ministry of Health, UNICEF. Myanmar Multiple Indicator Cluster Survey 2009–2010: Monitoring the Situation of Children and Women in Myanmar. UNICEF; 2011. October [Cited 2019 April 11]. Available from: https://mics.unicef.org/files?job=W1siZiIsIjIwMTUvMDEvMjcvMTIvMzAvMDEvOTgzL015YW5tYXJfRmluYWxfbWluaV9ib29rbGV0LnBkZiJdXQ&sha=42b9a892dde6b320 [Google Scholar]
- 18.Lynn KW, Mongkolchati A, Chompikul J, Wongsawass S. Prevalence and associated factors of exclusive breastfeeding among mothers in Pan-Ta-Naw township, Myanmar. Journal of Public Health and Development. 2015;13(3):81–94 [Google Scholar]
- 19.Hmone MP, Li M, Agho K, Alam A, Dibley MJ. Factors associated with intention to exclusive breastfeed in central women’s hospital, Yangon, Myanmar. International Breastfeeding Journal. 2017;12:29 10.1186/s13006-017-0120-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Agho KE, Dibley MJ, Odiase JI, Ogbonmwan SM. Determinants of exclusive breastfeeding in Nigeria. BMC Pregnancy and Childbirth. 2011;11:2 10.1186/1471-2393-11-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lakew Y, Tabar L, Haile D. Socio-medical determinants of timely breastfeeding initiation in Ethiopia: evidence from the 2011 nationwide Demographic and Health Survey. International Breastfeeding Journal. 2015;10:24 10.1186/s13006-015-0050-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ndirangu MN, Gatimu SM, Mwinyi HM, Kibiwott DC. Trends and factors associated with early initiation of breastfeeding in Namibia: analysis of the Demographic and Health Surveys 2000–2013. BMC pregnancy and childbirth. 2018;18:171 10.1186/s12884-018-1811-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Benedict RK, Craig HC, Torlesse H, Stoltzfus RJ. Trends and predictors of optimal breastfeeding among children 0–23 months, South Asia: Analysis of national survey data. Maternal & Child Nutrition. 2018;14(S4):e12698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Department of Population, Ministry of Immigration and Population. The 2014 Myanmar Population and Housing Census: The Union Report, Census Report Volume 2. The Republic of the Union of Myanmar; 2015. [Google Scholar]
- 25.Adewuyi EO, Zhao Y, Khanal V, Auta A, Bulndi LB. Rural-urban differences on the rates and factors associated with early initiation of breastfeeding in Nigeria: further analysis of the Nigeria demographic and health survey, 2013. International Breastfeeding Journal. 2017;12:51 10.1186/s13006-017-0141-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adewuyi E, Zhao Y, Lamichhane R. Socioeconomic, bio-demographic and health/behavioral determinants of neonatal mortality in Nigeria: a multilevel analysis of 2013 demographic and health survey. International Journal of Contemporary Pediatrics. 2016;3(2):311–323. [Google Scholar]
- 27.WHO, UNICEF. Baby-friendly Hospital Initiative: Revised, Updated and Expanded for Integrated Care. WHO; 2009. [Cited 2019 June 20]. Available from: https://www.who.int/nutrition/publications/infantfeeding/bfhi_trainingcourse/en/ [PubMed] [Google Scholar]
- 28.Than MK, Nyi SN, Hlaing LM, Mar SL, Thwin T, Cashin J, et al. Scaling up breastfeeding in Myanmar through the Becoming Breastfeeding Friendly initiative. Current Developments in Nutrition. 2019;3(8): nzz078 10.1093/cdn/nzz078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Adhikari M, Khanal V, Karkee R, Gavidia T. Factors associated with early initiation of breastfeeding among Nepalese mothers: further analysis of Nepal Demographic and Health Survey, 2011. International Breastfeeding Journal. 2014;9:21 10.1186/s13006-014-0021-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Karim F, Khan ANS, Tasnim F, Chowdhury MAK, Billah SM, Karim T, et al. Prevalence and determinants of initiation of breastfeeding within one hour of birth: an analysis of the Bangladesh Demographic and Health Survey, 2014. PLOS ONE. 2019;14(7):e0220224 10.1371/journal.pone.0220224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lessen R, Crivelli-Kovach A. Prediction of initiation and duration of breast-feeding for neonates admitted to the neonatal intensive care unit. Journal of Perinatal & Neonatal Nursing. 2007;21(3):256–66. [DOI] [PubMed] [Google Scholar]
- 32.Yılmaz E, Doğa Öcal F, Vural Yılmaz Z, Ceyhan M, Kara OF, Küçüközkan T. Early initiation and exclusive breastfeeding: factors influencing the attitudes of mothers who gave birth in a baby-friendly hospital. Turkish Journal of Obstetrics and Gynecology. 2017;14(1):1–9. 10.4274/tjod.90018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pérez-Escamilla R, Martinez JL, Segura-Pérez S. Impact of the Baby-friendly Hospital Initiative on breastfeeding and child health outcomes: a systematic review. Maternal & Child Nutrition. 2016;12(3):402–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.WHO, UNICEF. The Extension of the 2025 Maternal, Infant and Young Child nutrition Targets to 2030. WHO/ UNICEF Discussion paper. WHO. 2012. [Cited 2019 April 11]. Available from: https://www.who.int/nutrition/global-target-2025/discussion-paper-extension-targets-2030.pdf. 2012.
- 35.Khanal V, Sauer K, Zhao Y. Exclusive breastfeeding practices in relation to social and health determinants: a comparison of the 2006 and 2011 Nepal Demographic and Health Surveys. BMC Public Health. 2013;13:958 10.1186/1471-2458-13-958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bui QT-T, Lee H-Y, Le AT-K, Van Dung D, Vu LT-H. Trends and determinants for early initiation of and exclusive breastfeeding under six months in Vietnam: results from the Multiple Indicator Cluster Surveys, 2000–2011. Global health action. 2016;9:29433 10.3402/gha.v9.29433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chandhiok N, Singh KJ, Sahu D, Singh L, Pandey A. Changes in exclusive breastfeeding practices and its determinants in India, 1992–2006: analysis of national survey data. International Breastfeeding Journal. 2015;10:34 10.1186/s13006-015-0059-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Agushybana F, Siramaneerat I, Raksamat W, Siriphakhamongkhon S. Population-based survey of exclusive breastfeeding in Indonesia: a secondary analysis. Pacific Rim International Journal of Nursing Research. 2018;22(1): 6–17. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Data Availability Statement
The data set used in this study is Myanmar Demographic and Health Surveys (DHS) which are publicly available and can be downloaded from the DHS Program’s website (URL:http://www.dhsprogram.com/). The DHS Program is a project funded by USAID and implemented by ICF. So, anyone who is interested can download the data set directly from the website after request proposal.