During the coronavirus disease 2019 (COVID-19) pandemic, there have been reports suggesting a decrease in hospitalizations for cardiovascular disease (CVD), including acute myocardial infarction1 and heart failure.2 This reduction relates not only to temporarily postponed elective procedures, but also acute and life-threatening conditions. The explanation for this phenomenon is not clear, but there have been concerns that fear of contracting COVID-19 may be a contributing factor.3
There is an established temporal association between influenza activity in the community and CVD hospitalizations, associating a 5% monthly increase in influenza activity with a 24% increase in heart failure.4 The pandemic has caused enforcement of hygiene and social distancing measures that influence the activity of influenza and other respiratory viruses. In this study, we describe the association between CVD hospitalizations, influenza activity, and COVID-19 burden before, during, and after restrictions from Norwegian authorities.
We used anonymized, aggregated data from publicly available databases (www.fhi.no/en) to investigate trends in hospitalizations for CVD at Akershus University Hospital, a tertiary care hospital covering a catchment area of ≈560 000 individuals, during the first wave of the COVID-19 pandemic. All hospitalizations during weeks 6 (3 weeks before the first COVID-19 case in Norway) to 21 of 2020 and 2019 with primary International Classification of Diseases–10 code I20 through I22, I25, I34 through I37, 142, I44 through I50, R07, R55, or Z034 through Z035 were included. We also recorded the number of patients hospitalized with laboratory-confirmed COVID-19 at Akershus University Hospital the corresponding week, as defined by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) detected in combined nasopharyngeal and oropharyngeal swabs determined by real-time polymerase chain reaction with cycle threshold as described by Corman (2020)5 using the ABI7500 System (Thermo Fisher Scientific). Influenza activity during the same period of 2019 and 2020 was obtained from the Norwegian Institute of Public Health as proportion of specimens positive for influenza virus A or B by real-time polymerase chain reaction among all people tested for influenza in Norway. Norwegian authorities introduced strict restrictions for travel, school closure, social distancing, hygiene, and rules for quarantine and isolation on March 12, 2020, and these restrictions were gradually eased from April 20, 2020. Incidence rates were calculated as number of hospitalizations divided by the population of the hospital catchment area during the defined period, and 95% CIs were calculated using the z values for standard normal distribution.
Weekly hospitalizations for CVD, the total number of patients hospitalized with COVID-19, and the proportion positive real-time polymerase chain reaction for influenza virus in 2019 and 2020 are presented in the Figure. The first case of COVID-19 in Norway was in week 9, and the first patient hospitalized at Akershus University Hospital with COVID-19 was admitted in week 10. There was a rapid increase in COVID-19 hospitalizations, with a peak in week 13, and a similar decrease in the following weeks. The proportion positive real-time polymerase chain reaction for influenza virus decreased from week 7 in both years. The decrease was steeper in 2020, with a positive rate under 5% in week 12 versus week 18 in 2019. The hospitalization rate for CVD ranged from 142 to 185 per week during the examined period in 2019. In 2020, there was a >50% reduction from week 9 to 13 (from 167 to 82 hospitalizations per week), with a following increase to week 17. After week 17 of 2020, the weekly number of hospitalizations for CVD remained lower than for 2019.
Figure.
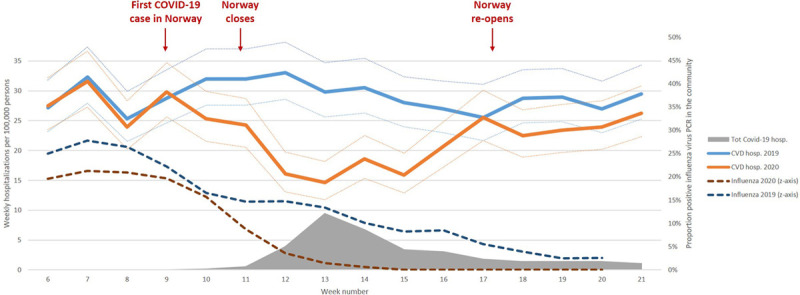
Weekly cardiovascular disease (CVD) hospitalization rates with 95% CIs in 2019 and 2020 at a tertiary care hospital in Norway and the total hospitalization rate for corona virus disease 2019 (COVID-19) the same week.
The proportion of polymerase chain reaction–positive tests for influenza virus in Norwegian laboratories in 2019 and 2020 is presented.
We observed that hospitalizations for CVD in Norway decreased during the first wave of the pandemic and remained lower than normal in the first weeks after easing the restrictions. In parallel with the rise in COVID-19 hospitalizations and the introduction of drastic restrictions, there was a rapid reduction in CVD hospitalizations and influenza activity. With a very low incidence of SARS-CoV-2 in the community and ease of restrictions by the authorities, the rate of CVD hospitalizations increased, but to a lower level than before the pandemic.
Whether the decrease in CVD hospitalizations relates to patients’ concerns over contracting COVID-19 in the hospital or reflects a true reduction in the incidence of CVD is unclear. In Norway, far-reaching restrictions were implemented early, resulting in a rapid reduction in the incidence of hospitalizations and deaths from COVID-19. Norway was one of the first countries to gradually lift restrictions, providing a unique opportunity to assess the trends in CVD hospitalizations in the next phase of the pandemic. A delay in time from symptom onset to hospitalization would have been expected if patients with CVD emergencies delayed health care contact, but the Norwegian Myocardial Infarction Registry report no such delay in 2020 compared with 2019.6 Given the known association between influenza activity and CVD, it is likely that the rapid and steep decrease in influenza associated with social distancing and hygiene measures during the pandemic’s first wave might have contributed to the decrease in CVD hospitalizations. This in turn would contribute to comparable mortality rates in Norway during the first wave of the pandemic in 2020 and previous years (Statistics Norway).
Acknowledgments
The authors thank Øyvind Antonsen and the Unit of Data Analysis at Akershus University Hospital, Lørenskog, Norway, for their contributions.
Sources of Funding
Dr Myhre is supported by a postdoctoral research grant from South-Eastern Norway Regional Health Authority and University of Oslo.
Disclosures
Dr Myhre has served on advisory boards for Novartis and Novo Nordisk and has received consulting honoraria from Novartis, AmGen, and Novo Nordisk. Dr Omland has served on advisory boards for Abbott Diagnostics, Roche Diagnostics, and Bayer; has received research support from Abbott Diagnostics, Novartis, Roche Diagnostics, Singulex, and SomaLogic via Akershus University Hospital; and has received speaker’s or consulting honoraria from Roche Diagnostics, Siemens Healthineers, and CardiNor. Dr Schirmer has received research support from Astra Zeneca and Novartis and speaker’s or consulting honoraria from MSD, Sanofi Aventis, and Pfizer. Drs Grundvold and Paulsen report no conflicts.
Footnotes
This manuscript was sent to Michael Kurz, Guest Editor, for review by expert referees, editorial decision, and final disposition.
References
- 1.Solomon MD, McNulty EJ, Rana JS, Leong TK, Lee C, Sung SH, Ambrosy AP, Sidney S, Go AS. The COVID-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630 [DOI] [PubMed] [Google Scholar]
- 2.Hall ME, Vaduganathan M, Khan MS, Papadimitriou L, Long RC, Hernandez GA, Moore CK, Lennep BW, McMullan MR, Butler J. Reductions in heart failure hospitalizations during the COVID-19 pandemic. J Card Fail. 2020;26:462–463. doi: 10.1016/j.cardfail.2020.05.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The European Society for Cardiology. ESC Guidance for the Diagnosis and Management of CV Disease During the COVID-19 Pandemic. https://www.escardio.org/Education/COVID-19-and-Cardiology/ESC-COVID-19-Guidance. Published June 10, 2020. Accessed August 3, 2020
- 4.Kytömaa S, Hegde S, Claggett B, Udell JA, Rosamond W, Temte J, Nichol K, Wright JD, Solomon SD, Vardeny O. Association of influenza-like illness activity with hospitalizations for heart failure: the Atherosclerosis Risk in Communities Study. JAMA Cardiol. 2019;4:363–369. doi: 10.1001/jamacardio.2019.0549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Corman VM, Landt O, Kaiser M, Molenkamp R, Meijer A, Chu DK, Bleicker T, Brunink S, Schneider J, Schmidt ML, et al. Detection of 2019 novel coronavirus (2019-nCoV) by real-time RT-PCR. Euro Surveill. 2020;25:2000045 doi: 10.2807/1560-7917.ES.2020.25.3.2000045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Norwegian Institute of Public Health and St. Olav’s Hospital HF. Norwegian Myocardial Infarction Registry. https://stolav.no/norsk-hjerteinfarktregister. Published July 27, 2020. Accessed August 3, 2020.


