The world continues to be entrenched in the coronavirus disease 2019 (COVID-19) pandemic, which has significantly affected our daily interpersonal interactions, including community response to public emergencies that require bystander cardiopulmonary resuscitation (bCPR). For healthcare workers on the front line of COVID-19 care, our reality is a spectrum of disease that ranges from the mildly symptomatic patient to the critically ill, hypoxic, crashing patient. The public reality is stay-at-home orders or newly implemented safer-at-home plans, job losses, and coping with the illness and death of family and friends. These events predominate daily routines in this new normal, as does a profound sense of fear: fear for the community and for healthcare providers. As a cardiac arrest outcomes researcher, I fear how this viral pandemic will threaten our altruistic societal approach to helping individuals with cardiac arrest. bCPR is an essential physical maneuver proven to impart better survival and neurological recovery for individuals with cardiac arrest. CPR requires bystanders to come into close proximity with another individual, sometimes even a stranger, at a time when the message is to socially distance and fears about severe acute respiratory syndrome coronavirus 2 transmission predominate.
Our generation has faced similar fears before in the community and among healthcare providers. In 1981, the US Centers for Disease Control and Prevention advised the public about a new infectious disease, initially causing pneumonia in homosexual men. This marked the beginning of the HIV pandemic, now a historical memory for many, but at the time the events shocked society and produced overwhelming fear. Misconceptions about disease transmission were prevalent, and discrimination against people living with HIV became pervasive. Exaggerated fears that touching someone with HIV might result in transmission of disease became ostracizing, and unsubstantiated fears of acquiring the disease by way of casual contact or touch became as endemic as the disease. We are all presently experiencing a similar fear, with pervasive underpinnings anchored on avoidance and anxiety. Similar to HIV, COVID-19 is heavily affecting disenfranchised communities (eg, those with low socioeconomic status, racial/ethnic minorities, those undomiciled, and others) that are already prone to poor access to health care, lower rates of bCPR, and delayed response from emergency medical services.1,2 Confounding preexisting disparities in rates of bCPR with the fear of an infectious virus that is aerosolized during CPR could have devastating results.
Early findings reported from 4 Italian provinces heavily affected by COVID-19 were reported in the New England Journal of Medicine.3 Compared with the previous year, Baldi et al3 reported that the incidence of out-of-hospital cardiac arrest increased by 58%. This is in stark contrast to the provision of bCPR, which decreased by 15.6% in a region that had previously reported a bCPR rate of 47%. If we translate similar findings to the United States, where rates of bCPR are variable and neighborhoods with lower socioeconomic status observe considerably less, we will undoubtedly see a devastating effect. Data from Washington showed that in the midst of the pandemic, ≈10% of individuals with cardiac arrest responded to by emergency medical services were COVID-19 positive. Assuming a transmission rate of 10% without personal protective equipment, after treating 100 patients, 1 rescuer may become infected.4 Rates of OHCA have been increasing during COVID-19, but those arrests may not be caused primarily by the virus, and limiting bystander resuscitative measures to protect the rescuer will undoubtedly result in death caused by cardiac arrest, not necessarily COVID-19.
The American Heart Association has issued an interim guideline on basic life support during COVID-19.5 Recommendations previously endorsed bCPR by the public for individuals with cardiac arrest, and in 2010 rescue breaths were removed from the basic life support algorithm in favor of a hands-only approach. That being said, even hands-only CPR can result in aerosolization of respiratory droplets and potential fomite transmission of severe acute respiratory syndrome coronavirus 2. Although evidence is sparse, current COVID-19 recommendations include taking caution while still performing bCPR. When CPR is performed on an unresponsive person, all efforts should be made to cover the face of the individual with cardiac arrest with a cloth to minimize the dispersion of respiratory droplets, and the rescuer also should have a face covering if possible for increased protection. Rescue breaths should not be provided, and the rescuer should administer guideline-concordant chest compressions and placement of an automated external defibrillator as soon as possible. Additional rescuers should remain at a distance, away from the victim’s airway and face, until they are needed to assume CPR when the initial rescuer fatigues. These suggested precautions and the early data on the risk of transmission must be relayed to the public immediately, and educational programs for bCPR should be amended to include this information as a means of keeping the rescuer safe while continuing to encourage bystander provision of basic life support to save lives.
Given the real and potential threat of viral inoculation perceived by the public, rates of bCPR will decline, undoubtedly resulting in more loss of life. There are many reasons why the public fears providing bCPR to an unresponsive person; the threat of contracting a deadly viral disease will undoubtedly enter the list of reasons not to render aid. Previous goals to improve rates of bCPR in the community are now in jeopardy as our new normal threatens to reduce current US bCPR rates. Declining rates of bCPR are a reality; addressing this issue before it results in more deaths or neurological disabilities is paramount. CPR saves lives. It saved lives before this pandemic, and it will save lives after this pandemic. Our task is to clearly understand the risk to operators, to train the public in best practices to maintain one’s personal safety, and to allay fears once we are safe to do so (Figure). Waiting for rates of bCPR to drop is too late. We must be prepared to educate and empower rescuers in our new normal.
Figure.
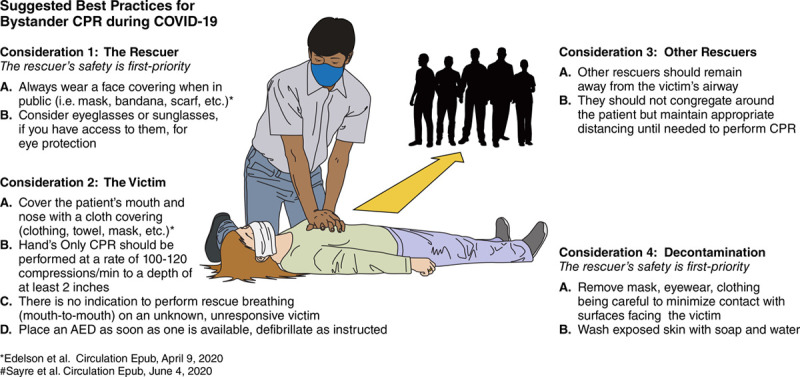
Suggested best practices for bystander cardiopulmonary resuscitation (CPR) during coronavirus disease 2019 (COVID-19).
AED indicates automated external defibrillator.
Disclosures
Dr Perman is supported by K23 HL138164 from the National Heart, Lung, and Blood Institute. The views expressed in this manuscript represent those of the author and do not necessarily represent the official views of the National Heart, Lung and Blood Institute.
Footnotes
The opinions expressed in this article are not necessarily those of the editors or of the American Heart Association.
References
- 1.Sasson C, Magid DJ, Chan P, Root ED, McNally BF, Kellermann AL, Haukoos JS; CARES Surveillance Group. Association of neighborhood characteristics with bystander-initiated CPR. N Engl J Med. 2012;367:1607–1615. doi: 10.1056/NEJMoa1110700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kleindorfer DO, Lindsell CJ, Broderick JP, Flaherty ML, Woo D, Ewing I, Schmit P, Moomaw C, Alwell K, Pancioli A, et al. Community socioeconomic status and prehospital times in acute stroke and transient ischemic attack: do poorer patients have longer delays from 911 call to the emergency department?. Stroke. 2006;37:1508–1513. doi: 10.1161/01.STR.0000222933.94460.dd [DOI] [PubMed] [Google Scholar]
- 3.Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, Klersy C, Palo A, Contri E, Ronchi V, et al. ; Lombardia CARe Researchers. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383:496–498. doi: 10.1056/NEJMc2010418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sayre MR, Barnard LM, Counts CR, Drucker CJ, Kudenchuk PJ, Rea TD, Eisenberg MS. Prevalence of COVID-19 in out-of-hospital cardiac arrest: implications for bystander CPR [published online June 4, 2020]. Circulation. doi: 10.1161/CIRCULATIONAHA.120.048951 https://www.ahajournals.org/doi/10.1161/CIRCULATIONAHA.120.048951?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%20%200pubmed [DOI] [PubMed] [Google Scholar]
- 5.Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, Berg RA, Bradley SM, Brooks SC, Cheng A, et al. ; American Heart Association ECC Interim COVID Guidance Authors. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the Emergency Cardiovascular Care Committee and Get With The Guidelines–Resuscitation Adult and Pediatric Task Forces of the American Heart Association. Circulation. 2020;141:e933–e943. doi: 10.1161/CIRCULATIONAHA.120.047463 [DOI] [PMC free article] [PubMed] [Google Scholar]


