Abstract
Mucinous lesions of appendix are a rare clinical entity and may be neoplastic or non-neoplastic. The diagnosis is usual incidental during computed tomography scan or colonoscopy performed for general abdominal symptoms or occasional finding during operation for acute appendicitis. For this reason, initial treatment should be tailored to the situation, aiming at complete resection of the appendix with disease-free margins: this can be achieved by simple appendectomy or more extensive resection. The pathological examination of the specimen is the key to offer the patient a correct and complete treatment, and, if a neoplastic pathology is found, the case should be discussed in multidisciplinary group. We describe three cases with different clinical presentation leading to different surgical treatment: one elective case, in which the diagnosis was suspected preoperatively; and two urgent cases, one mimicking an intussusception and another one presenting as an acute appendicitis.
INTRODUCTION
Appendiceal mucocele is a well-known entity that can present in a variety of clinical syndromes or can occur as an incidental surgical finding. It was first described by Rokitansky in 1842 [1] and it is a relatively rare condition, incidence of which is 0.07–0.63% of all appendectomies performed, it represents a progressive appendix dilation caused by intraluminal accumulation of mucoid substance and may be a malignant or a benign process [2]. Different classifications and terminology were used, leading to difficult comparison of the outcome and treatment between different authors. Only in 2016 the Peritoneal Surface Oncology Group International (PSOGI) proposed a unique classification and diagnostic terminology in a consensus published in American Journal of Surgical Pathology in 2016 [3, 4], in which mucinous lesions of are classified as described below:
− Non neoplastic
-
− Neoplastic:
∘ Serrated polyps with or without grade dysplasia (low or high grade)
∘ Adenoma with low- or high-grade dysplasia (PSOGI expert panel preferred to confine this term to lesions that resemble tubular, tubulovillous or villous adenomas of the colorectum limited to the mucosa without gross luminal dilatation. So many neoplasms considered previously mucinous adenomas are now classified more conservately as low-grade appendiceal mucinous neoplasms [4])
-
∘ Mucinous neoplasms
▪ Low-grade appendiceal mucinous neoplasms (LAMNs)
▪ High-grade appendiceal mucinous neoplasms (HAMNs)
∘ Mucinous adenocarcinoma (well, moderately or poorly differentiated)
Mucinous appendiceal neoplasms and mucinous adenocarcinomas are the leading cause of pseudomyxoma peritonei, a unique and unusual peritoneal malignancy characterized by slow but relentless accumulation of mucinous ascites and peritoneal implants in the peritoneal cavity [4].
The diagnosis of appendiceal mucinous lesions is usually incidental and this pathology is often discovered during radiologic or endoscopic evaluation for unrelated complaints or abdominal pain or can be a surprise during an operation for acute appendicitis. Since there are no reliable diagnostic criteria to exclude preoperatively malignant lesions, surgery should be pursued both for diagnosis and for therapy [5]. The removal of the lesion prevents also potential rupture, which can lead to pseudomyxoma peritonei, if the lesion is neoplastic [5]. The initial surgery should be tailored to the preoperative and intraoperative findings aiming at a correct specimen removal and possibly definitive treatment.
Initial surgery
A standard appendectomy with the goal to achieve a disease-free margin is recommended. The role of laparoscopy has been debated in the last years, with the surgeons’ increasing confidence. It is usually safe if care is taken not to spill the content of the mucocele, not to rupture the appendix and to put the specimen immediately in a plastic bag [11].
If it is necessary to achieve a grossly free margin, can be performed a coecal cuff resection with ileocecal valve conservation or an ileocoecal resection up to a right hemicolectomy, according to the surgeon’s discretion and the operative finding.
In case of ruptured lesions, the initial surgery should be limited to the appendectomy but, if with this resection is possible to remove the contained rupture, can be performed a right hemicolectomy. More extensive surgery, aimed at removing peritoneal mucinous disease, should be reserved to high-experience centres after the pathology report [5, 6].
Additional treatment based on pathology
Once obtained the final pathology, it should be evaluated if further surgery may be indicated, according to staging and classification [3]. Surgical options include:
− a completion right hemicolectomy with lymphadenectomy and
− cytoreductive surgery and heated intraperitoneal chemotherapy to treat peritoneal mucinous disease (pseudomyxoma peritonei).
This decision is not a standardized one, these patients should be presented at a multidisciplinary meeting and, if necessary, referred to a centre specialized in treating peritoneal surface malignancy.
We can have different scenarios:
− Simple mucocele and serrated polyps: appendectomy is curative for patients with a non-neoplastic mucinous neoplasm, these lesions are not associated with recurrence even if they rupture, therefore no additional treatment or surveillance is necessary.
− Completely resected LAMN or HAMN: if the lesion is a LAMN confined to the appendix, has not ruptured, and is completely resected by appendectomy do not require a completion right hemicolectomy [7]. In clinical cases with positive margins, there is not a unique indication, as some authors propose a completion right hemicolectomy and lymphadenectomy [7], whereas other authors confirm that it is not always necessary, since limited data suggest that a positive margin following appendectomy for unruptured LAMN does not predict disease recurrence [8]. Appendectomy alone is usually sufficient for treating HAMN limited to the appendix, but care should be taken to exclude the presence of associated invasive adenocarcinoma, including comprehensive histologic evaluation of the entire surgical specimen [8]. Patients who are found to have peritoneal mucin at the time of initial surgery should be referred to a centre specialized in the treatment of peritoneal surface malignancies [5].
− Non-metastatic adenocarcinoma of the appendix: according to a recent published guideline, patients should undergo right hemicolectomy [8] in order to achieve complete resection of nodal basin. However, Nasseri et al. [9], in a retrospective study, demonstrated that the addition of right hemicolectomy in patients with margin negative appendectomy does not offer a survival benefit in patients with non-metastatic, low-grade appendiceal mucinous adenocarcinoma.
− Peritoneal metastasis found durng appendectomy: Sugarbaker [6], in a recent study, stated that in this case a right hemicolectomy associated to a cytoreductive surgery and hyperthermic intraperitoneal chemotherapy (HIPEC) is necessary only in case of peritoneal mucinous carcinoma poorly differentiated or peritoneal metastasis of intestinal type. In case of disseminated peritoneal adenomucinosis or peritoneal mucinous carcinoma well or moderately differentiated a cytoreductive surgery and HIPEC can be associated to a simple appendectomy since the author did not find a survival advantage for right colon resection with resection of appendiceal and ileocolic lymph nodes versus appendectomy only as a part of the cytoreductive surgery.
The role of laparoscopy for the treatment of appendiceal mucocele has been debated for years, but recent reports demonstrate that laparoscopy can be a feasible technique keeping mandatory extra care in manipulating the appendix and careful extraction with plastic bag [10, 11].
CASE REPORT
Case 1
A 48 years old man, without comorbidities, visited by his physician for a persisting pain in right abdomen after a successfully treated renal colic. An abdominal ultrasound (US) was performed and was discovered a ‘thick bowel loop’ in right iliac fossa. A computed tomography (CT) scan was then ordered, conducting to the suspect of dilatation of appendix (Fig. 1).
Figure 1.
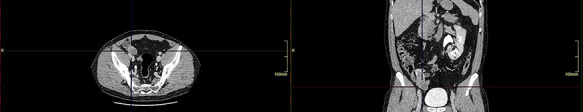
Case 1: axial and coronal CT sections.
A laparoscopic exploration was performed during which was seen a dilated appendix ~10 cm long with a thin base and an apparent intact insertion in the cecal wall, fully mobile (Fig. 2). It was decided to proceed with a formal laparoscopic appendectomy, with immediate positioning of the specimen in an endobag without peritoneal seeding (Fig. 3).
Figure 2.
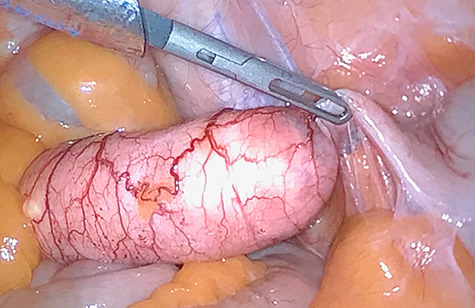
Case 1: intraoperative finding.
Figure 3.

Case 1: specimen.
The pathology report was ‘mucinous hyperplasia with appendicular mucocele, resection margin disease free’.
Case 2
An old woman, 82 years, was admitted in our emergency department for hip fracture. She had multiple comorbidities: hypertension, asthma and was described a former hysterectomy for fibromatosis. Her fractured hip was treated with a gamma nail. During the post-operative period, the patient developed pneumonia and was sent to the medical ward, where she presented incoming subocclusive crisis and abdominal pain. An abdominal US completed with CT showed a lesion in right iliac fossa mimicking an intestinal intussusception (Fig. 4). The patient underwent surgical operation and the operative finding was dilated appendix, with a thin wall full of mucinous material, with a large base implanted on a dilated cecum and the body strictly adhering to the posterior wall of the pelvis. It was decided to perform an ileocoecal resection, in order to be sure to obtain disease-free margins and the reconstruction was completed with a lateral ileocolic anastomosis.
Figure 4.
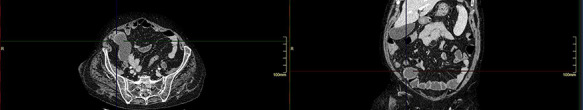
Case 2: axial and coronal CT sections.
The pathology report was ‘appendicular mucocele due to mucinous papillar cistoadenoma with epithelial high-grade dysplasia. Thirteen pericolic nodes were found negative for neoplastic cells’ A multidisciplinary meeting discussed the case and decided to keep the patient on clinical–radiological follow-up.
Case 3
A 52 years old man admitted to the emergency department with signs and symptoms of acute appendicitis. The patient presented with fever and high white blood cell count, elevated C-reactive protein and right iliac fossa pain. The patient underwent an abdominal ultrasonography that could not confirm appendicitis, and a CT scan showed a dilated appendix, and a fluid collection nearby (Fig. 5). A laparoscopic exploration was performed and a dilated appendix was found, so a laparoscopic appendectomy was performed with immediate positioning of the specimen in an endobag.
Figure 5.
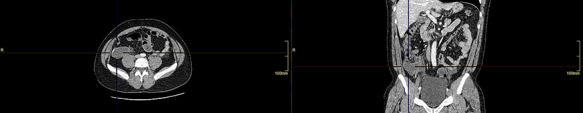
Case 3: axial and coronal CT sections.
The pathology report was ‘mucinous cistoadenoma of appendix with low grade dysplasia’. A clinical follow-up was organized.
DISCUSSION
The cases presented are different both in presentation and in treatment. The first case is an elective one, in which the diagnosis has been made preoperatively and has been successfully treated by laparoscopic appendectomy. The non-neoplastic origin was confirmed by pathology report. The second case presented with an acute diagnosis and has been diagnosed only intraoperatively, she was treated by open surgery and we decided to perform an ileocoecal resection, since we were not sure to obtain free margins with an isolated appendectomy. The pathology report demonstrated a high-grade dysplasia and negative nodes. The last case was a typical operative surprise during an urgent appendectomy for acute appendicitis and has been successfully treated with laparoscopic appendectomy. In none of the cases were visible peritoneal metastases. The treatment has been successfully achieved by laparoscopy when it was technically feasible, with a low threshold to convert to open surgery.
CONCLUSION
Appendicular mucocele may be of benign or neoplastic origin [2]. Sometimes may be detected preoperatively, during CT scan executed due to abdominal symptoms, but many times they are discovered during surgery for acute condition [5], so a correct pathway should be in surgeon’s mind to correctly treat this disease.
The decision to perform a simple appendectomy or a more extensive resection should be often taken intraoperatively. The first thing to assess is the presence of peritoneal metastases, in this case a formal appendectomy and metastases biopsy should be performed [6] to obtain a diagnosis and the patient has to be referred to a centre specialized in the treatment of peritoneal surface malignancies.
If a grossly peritoneal spread is not present, the goal is to achieve a complete resection of the disease as, until the definitive examination, an exact diagnosis cannot be expressed [4, 5, 8, 10]. This can be accomplished by appendectomy or more extensive resections up to right hemicolectomy [5].
As in our series, laparoscopy can be a useful technique to obtain a good exploration of abdominal content and to perform an appendectomy taking care to apply careful manipulation of the tissue and to prevent spillage of appendiceal content. The specimen should be promptly positioned in an endobag for further exploration and extraction in order to avoid peritoneal dissemination. The surgeon should have a low threshold to convert to open surgery in case complete resection cannot by achieved by laparoscopy or in case of suspected extra organ local involvement [10, 11].
Once obtained definitive pathology report, a multidisciplinary group should be involved in further treatment of the patient in case of malignancy.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
Contributor Information
Luca Cestino, S.C. Chirurgia Generale, Ospedale Maria Vittoria, Azienda Sanitaria Locale Città di Torino, Torino, Italy.
Federico Festa, S.C. Chirurgia Generale, Ospedale Maria Vittoria, Azienda Sanitaria Locale Città di Torino, Torino, Italy.
Giuseppe Cavuoti, S.C. Chirurgia Generale, Ospedale Maria Vittoria, Azienda Sanitaria Locale Città di Torino, Torino, Italy.
Luca Bonatti, S.C. Chirurgia Generale, Ospedale Maria Vittoria, Azienda Sanitaria Locale Città di Torino, Torino, Italy.
Stefania Soncini, S.C. Chirurgia Generale, Ospedale Maria Vittoria, Azienda Sanitaria Locale Città di Torino, Torino, Italy.
Luca Dani, S.C. Chirurgia Generale, Ospedale Maria Vittoria, Azienda Sanitaria Locale Città di Torino, Torino, Italy.
Francesco Quaglino, S.C. Chirurgia Generale, Ospedale Maria Vittoria, Azienda Sanitaria Locale Città di Torino, Torino, Italy.
References
- 1.Rokitansky C. Trattato completo di anatomia patologica. Venezia: Gattei, 1853, Tomo3: 324. [Google Scholar]
- 2. Agrusa A, Romano G, Galia M, Cucinella G, Sorce V, Di Buono G, et al. Appendiceal mucinous neoplasms: an uncertain nosological entity. Report of a case. G Chir 2016;37:86–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Carr NJ, Cecil TD, Mohamed F, Sobin LH, Sugarbaker PH, González-Moreno S, et al. Peritoneal surface oncology group international. A consensus for classification and pathologic reporting of Pseudomyxoma Peritonei and associated Appendiceal Neoplasia: the results of the peritoneal surface oncology group international (PSOGI) modified Delphi process. Am J Surg Pathol 2016;40:14–26. [DOI] [PubMed] [Google Scholar]
- 4. Carr NJ, Bibeau F, Bradley RF, Dartigues P, Feakins RM, Geisinger KR, et al. The histopathological classification, diagnosis and differential diagnosis of mucinous appendiceal neoplasms, appendiceal adenocarcinomas and pseudomyxoma peritonei. Histopathology 2017;71:847–58. [DOI] [PubMed] [Google Scholar]
- 5. Overman MJ, Compton CC, Raghav K. Appendiceal mucinous lesions In: UpToDate, Post, TW(Ed). Waltham, MA: UpToDate, 2020, [Google Scholar]
- 6. Sugarbaker PH. When and when not to perform a right colon resection with mucinous appendiceal neoplasms. Ann Surg Oncol 2017;24:729–32. [DOI] [PubMed] [Google Scholar]
- 7. Choudry HA, Pai RK. Management of mucinous appendiceal tumors. Ann Surg Oncol 2018;25:2135–44. [DOI] [PubMed] [Google Scholar]
- 8. Glasgow SC, Gaertner W, Stewart D, Davids J, Alavi K, Paquette IM, et al. The American Society of Colon and Rectal Surgeons, clinical practice guidelines for the management of appendiceal neoplasms. Dis Colon Rectum 2019;62:1425–38. [DOI] [PubMed] [Google Scholar]
- 9. Nasseri YY, Zhu R, Sutanto C, Wai C, Cohen JS, Ellenhorn J, et al. Role of right hemicolectomy in patients with low-grade appendiceal mucinous adenocarcinoma. Am J Surg 2019;218:1239–43. [DOI] [PubMed] [Google Scholar]
- 10. Sharma E, Gokani SA, Neville J, Sinha A, Agarwal T. Mucinous appendiceal adenocarcinomas: a diagnostic challenge. J Surg Case Rep 2020;2020:rjz355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Foula MS, Alardhi AM, Othman SA, Mirza Gari MK. Laparoscopic management of appendicular mucinous cystadenoma, case report. Int J Surg Case Rep 2019;54:87–9. [DOI] [PMC free article] [PubMed] [Google Scholar]


