Abstract
In this report, we describe the case of a SARS-CoV-2 infection (COVID-19) in an infant with mild fever and diarrhea in the absence of respiratory distress. A 45-day-old male infant with COVID-19 was transferred to our pediatric department. He had mild fever and diarrhea at admission. Positive-to-negative nasal swab conversion occurred on the 21st day from the onset of symptoms. However, stool swab positivity persisted during the 6-week admission period and for 7 weeks during follow-up at an outpatient clinic after discharge. Negative conversion in a stool specimen occurred on the 142nd day from the onset of symptoms. This case highlights the potential of fecal virus shedding as an important feature of viral transmission in infants and young children.
Keywords: COVID-19, infant, stool, diarrhea
INTRODUCTION
Coronaviruses are important human and animal pathogens.1 At the end of 2019, a pneumonia outbreak in Wuhan, a city in Hubei, China turned out to be the result of SARS-CoV-2 infection. SARS-CoV-2 causes a spectrum of manifestations, ranging from mild upper respiratory tract infection to severe pneumonitis, acute respiratory distress syndrome, and death.2 Although people with comorbidities and older adults are more likely to develop severe symptoms, children appear to have less severe clinical symptoms than adults.3,4 In children, symptoms include fever, runny nose, dry cough, and occasionally diarrhea. Zhang, et al.5 reported that angiotensin converting enzyme 2 is highly expressed in esophageal epithelial cells and absorptive enterocytes from the ileum and colon, suggestive of possible fecal transmission. Here, we report the case of a 45-day-old infant with COVID-19 who showed symptoms of persistent stool swab positivity for up to 20 weeks, despite negative respiratory specimens.
CASE REPORT
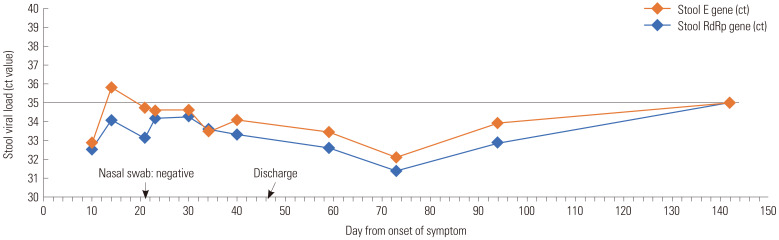
A 45-day-old male infant with COVID-19 was transferred to our pediatric department on March 2, 2020. He presented with mild fever (37.8℃) and diarrhea at admission but no cough, tachypnea, or respiratory distress. He was formula-fed, and feeding was normal. His symptoms began on February 24, 2020, and the diagnosis was confirmed on February 29. He appeared to have been infected by his father or mother. He had diarrhea three or four times a day that lasted four days. No mucus or blood was found in the feces. On physical examination, he was alert and active; other criteria were within normal limits. Samples of blood, urine, stool, and nasopharyngeal swab were obtained for analysis. RNA extraction from specimens was performed using a Libex magnetic bead extractor NP 68-S series (Xi'an TianLong Science & Technology Co., Ltd, SianXi, China). Envelope protein (E) and RNA-dependent RNA polymerase (RdRp) were used as primer probe targets, and specimens were tested using a PowerCheck™ 2019-nCoV Real-time PCR kit (KOGENE BIOTECH Co., Ltd, Seoul, Korea). Empiric therapy with parenteral cefotaxime was started on admission and continued until the fever subsided on the 4th day of admission. No antiviral medications were given. Nasal swab conversion from positive to negative occurred on the 21st day from the onset of symptoms. Urine and serum specimens for COVID-19 testing were obtained, and all results were negative. However, stool test results remained positive during the admission period. He stayed in a negatively pressured room with his parents during the 6-week admission, because there are no guidelines on stool specimens. No negative results for SARS-CoV-2 were found for at least two sequential stool specimens collected more than 24 hours apart during hospitalization. Stool testing for COVID-19 was performed regularly (every 2 to 4 weeks) at an outpatient clinic, although stool positivity persisted. Fecal viral load, as determined by PCR for E and RdRp, decreased rapidly from the 94th day and turned negative on the 142nd day from the onset of symptoms (Fig. 1).
Fig. 1. Stool viral cycle threshold trend over the first 20 weeks. Nasal swab testing performed on the 21st day from symptom onset was negative, while stool specimens were negative on the 142nd day from symptom onset. ct: cycle threshold; X-axis: day from onset of symptoms; Cut-off value of cycle threshold (ct): 35.
DISCUSSION
Pediatric SARS-CoV-2 infections are often underestimated, as they may remain asymptomatic or manifest nonspecific symptoms, such as headache, cough, nasal congestion, and/or runny nose. The majority of pediatric infants with COVID-19 exhibit only moderate to low-grade fever, or even none, though smaller infants can present primarily with gastrointestinal symptoms, such as abdominal distension, diarrhea, and food aversion.6 Early studies have indicated that individuals infected with SARS-CoV-2 might shed and spread the virus while being presymptomatic or asymptomatic.7,8,9 One study suggested that viral shedding might last for more than a month.10 In our patient, stool positivity on RT-PCR persisted for 12 weeks and finally turned negative on the 142nd day from the onset of symptoms. The cycle threshold (ct) values of stool samples showed wax and waning patterns, and these may be attributable to variations in separately performed PCR analysis or the quality of the stool samples. In a recent study, intracellular staining for viral nucleocapsid protein in gastric, duodenal, and rectal epithelia revealed SARS-CoV-2 infection of these gastrointestinal glandular epithelial cells.11 The continuous positive detection of viral RNA from feces suggests that the infectious virions are secreted from virus-infected gastrointestinal cells.11 However, data on the period of infectivity of stools with virus detection are limited. Thus, although virus was detected by RT-PCR for up to 20 weeks in this case, the true period of infectivity through viral stool excretion is not known. Moreover, not all infants with COVID-19 exhibit persistent fecal virus shedding: two children (aged 3 and 6 years) with COVID-19 treated at our hospital were initially positive on fecal RT-PCR testing, but negative on subsequent testing. Further studies of cultures of viable viruses are necessary.
Herein, we described the case of an infant with COVID-19 who showed persistent fecal viral shedding. It took about 20 weeks for the stool specimens to turn negative. Because asymptomatic patients with viral shedding may cause secondary community infections, we propose that attention is required to reduce the risk of fecal transmission and that pediatric COVID-19 patients with initial gastrointestinal symptoms should be monitored carefully.
ACKNOWLEDGEMENTS
The authors thank Mrs. Hyang Mi Lee and Mrs. Seo Jin Lee (Physician Assistants) at the pediatric department for their technical assistance.
Footnotes
The authors have no potential conflicts of interest to disclose.
- Conceptualization: Seung-Man Cho.
- Investigation: Gyoung Yim Ha.
- Writing—original draft preparation: Seung-Man Cho.
- Writing—review and editing: Gyoung Yim Ha.
- Approval of final manuscript: all authors.
References
- 1.Weiss SR, Navas-Martin S. Coronavirus pathogenesis and the emerging pathogen severe acute respiratory syndrome coronavirus. Microbiol Mol Biol Rev. 2005;69:635–664. doi: 10.1128/MMBR.69.4.635-664.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.De Rose DU, Piersigilli F, Ronchetti MP, Santisi A, Bersani I, Dotta A, et al. Novel coronavirus disease (COVID-19) in newborns and infants: what we know so far. Ital J Pediatr. 2020;46:56. doi: 10.1186/s13052-020-0820-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen ZM, Fu JF, Shu Q, Chen YH, Hua CZ, Li FB, et al. Diagnosis and treatment recommendations for pediatric respiratory infection caused by the 2019 novel coronavirus. World J Pediatr. 2020;16:240–246. doi: 10.1007/s12519-020-00345-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kam KQ, Yung CF, Cui L, Tzer Pin, Mak TM, Maiwald M, et al. A well infant with coronavirus disease 2019 with high viral load. Clin Infect Dis. 2020;71:847–849. doi: 10.1093/cid/ciaa201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang H, Kang Z, Gong H, Xu D, Wang J, Li Z, et al. The digestive system is a potential route of 2019-nCov infection: a bioinformatics analysis based on single-cell transcriptomes. bioRxiv. 2020 Jan 31; doi: 10.1101/2020.01.30.927806. [Epub]. Available at: [DOI] [Google Scholar]
- 6.Cao Q, Chen YC, Chen CL, Chiu CH. SARS-CoV-2 infection in children: transmission dynamics and clinical characteristics. J Formos Med Assoc. 2020;119:670–673. doi: 10.1016/j.jfma.2020.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zou L, Ruan F, Huang M, Liang L, Huang H, Hong Z, et al. SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med. 2020;382:1177–1179. doi: 10.1056/NEJMc2001737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bai Y, Yao L, Wei T, Tian F, Jin DY, Chen L, et al. Presumed asymptomatic carrier transmission of COVID-19. JAMA. 2020;323:1406–1407. doi: 10.1001/jama.2020.2565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tong ZD, Tang A, Li KF, Li P, Wang HL, Yi JP, et al. Potential presymptomatic transmission of SARS-CoV-2, Zhejiang Province, China,2020. Emerg Infect Dis. 2020;26:1052–1054. doi: 10.3201/eid2605.200198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158:1831–1833.e3. doi: 10.1053/j.gastro.2020.02.055. [DOI] [PMC free article] [PubMed] [Google Scholar]