Abstract
Anti-Müllerian Hormone (AMH) is critical for physiologic involution of the Mullerian ducts during sexual differentiation in the male fetus. In women, AMH is a product of the small antral follicles in the ovaries and serves to function as an autocrine and paracrine regulator of follicular maturation. As the size of the residual follicular pool depends on the quantity of small antral follicles and declines over time, the serum AMH level in women follows a characteristic trajectory: a gradual decline throughout the reproductive years and a precipitous drop at menopause, becoming undetectable soon after. Thus, AMH is clinically useful as a screening tool for diminished ovarian reserve (Cui et al. in Fertil Steril 105(02):481–485, 2016). Perturbations in serum AMH are linked with a variety of pathological conditions, for instance, polycystic ovaries syndrome (PCOS), the pathophysiology likely being the excess follicles in this syndrome which produce increased amounts of AMH (Dumont et al. in Reprod Biol Endocrinol 13:137, 2015). AMH is also elevated in some ovarian tumors such as adult granulosa cell tumors, and it can be used as a tumor marker to gauge response to therapy and monitor for recurrence. Within the domain of assisted reproductive technology, serum AMH assays are widely used to derive prognostic information such as the chance of successful ovarian stimulation, subsequent embryo quality and even pregnancy rates. Finally, in the rapidly evolving field of oncofertility, serum AMH holds great promise as a predictor of ovarian reserve after completion of cancer therapy. Our aim is to put forth an in-depth review of the clinical applications of AMH in contemporary practice.
Keywords: Anti-Müllerian hormone, Assisted reproduction techniques, Oncofertility, PCOS, Targeted therapy
Introduction
The AMH is a member of the transforming growth factor (TGFβ) superfamily. It is an homodimer disulfide-linked glycoprotein with a molecular weight of 140 kDa. The gene is located on the short arm of chromosome 19 in humans, band 19p 13.3 (Fig. 1).
Fig. 1.
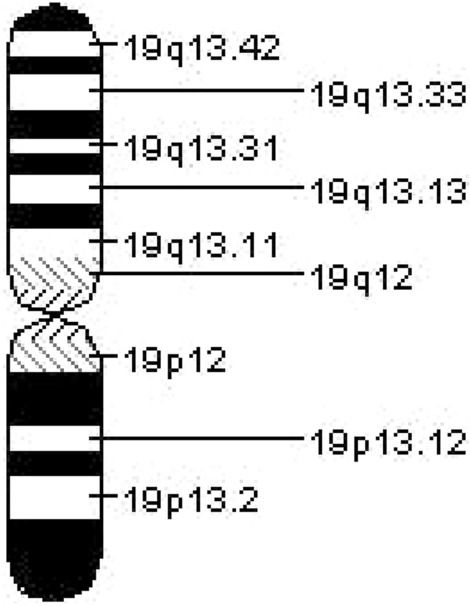
Chromosome 19
Anti-Müllerian Hormone (AMH) is critical for physiologic involution of the Mullerian ducts during sexual differentiation in the male fetus. In women, AMH is a product of the small antral follicles in the ovaries and serves to function as an autocrine and paracrine regulator of follicular maturation. As the size of the residual follicular pool depends on the quantity of small antral follicles and declines over time, the serum AMH level in women follows a characteristic trajectory: a gradual decline throughout the reproductive years and a precipitous drop at menopause, becoming undetectable soon after. Thus, AMH is clinically useful as a screening tool for diminished ovarian reserve [1].
Perturbations in serum AMH are linked with a variety of pathological conditions, for instance, polycystic ovaries syndrome (PCOS), the pathophysiologic link being the excess follicles in this syndrome which produce increased amounts of AMH [2]. AMH is also elevated in some ovarian tumors such as adult granulosa cell tumors, and it can be used as a tumor marker to gauge response to therapy and monitor for recurrence. Within the domain of assisted reproductive technology (ART), serum AMH assays are widely used to derive prognostic information such as the chance of successful ovarian stimulation, subsequent embryo quality and even pregnancy rates. Finally, in the rapidly evolving field of oncofertility, serum AMH holds great promise as a predictor of ovarian reserve after completion of cancer therapy.
Clinical Applications of AMH
Assisted reproductive technology
Fertility preservation
Ovarian neoplasms
Polycystic ovarian syndrome (PCOS)
Pediatric reproductive endocrinology
Prediction of early menopause
AMH in Assisted Reproductive Technology (ART)
AMH in the Evaluation of Ovarian Reserve
The total number of oocytes in women is predetermined by genetic factors and invariably declines with time from 1 to 2 million at birth to about 25,000 at age 40 and less than 1000 post-menopause. As the follicular pool depletes, serum inhibin B levels (produced by small antral follicles) decrease, leading to attenuation of the negative feedback on the pituitary. This in turn causes a serial rise in serum follicle stimulating hormone (FSH), consequently leading to earlier follicle recruitment and prompt increase in serum estradiol. Thus, ovarian reserve (OR), a term which denotes the quantity of the residual follicular pool, was classically determined by serum FSH and estradiol (E2) levels in the early follicular phase [3].
As our understanding of reproductive physiology progressed, other alternatives emerged: antral follicular count (AFC) and serum AMH. The antral follicle count (AFC) is measured with the help of ultrasound and correlates well with the amount of primordial follicles remaining, thus providing an indirect measure of ovarian reserve [3]. With ultrasound being operator-dependent, other markers of ovarian reserve have been sought so as to provide an objective assessment.
Serum AMH offers a significant potential advantage in this regard; being produced by small antral follicles that are gonadotropin-independent, it demonstrates little intra-cycle as well as inter-cycle variability in measurements. Indeed, serum AMH was found to have equivalent performance in predicting OR as AFC performed by sonography (the gold standard) in a large systematic review in 2014 [4]. In general, serum AMH level of < 1 ng/ml is accepted as a low ovarian reserve. Thus, serum AMH has established itself as an integral component in the determination of OR and it is now the most sensitive marker of ovarian reserve in the general in vitro fertilization (IVF) population [5].
AMH Measurement for Personalized Ovarian Stimulation
The individualization of controlled ovarian stimulation is an important aim of contemporary infertility practice. AMH evaluation assists in choosing the optimum stimulation protocol, hence reducing the likelihood of ovarian hyperstimulation syndrome (OHSS) or cycle cancelation from nonresponsiveness, leading us closer to the realization of personalized infertility therapy [6]. It also helps in predicting poor responders. Thus, serum AMH assays are being increasingly utilized in clinical practice for this purpose.
However, it is also important to recognize the limitations of AMH as its utilization for predicting pregnancy in patients undergoing ART is fraught with diagnostic uncertainties, being neither sensitive nor specific. The possible explanation is that serum AMH is a quantitative marker of small antral follicles and cannot be substituted as a marker of oocyte quality.
Hence, women can be infertile even with high AMH levels, whereas there are pregnancies described in women with near-undetectable AMH [7]. Intra-follicular AMH level may provide more accurate information regarding successful pregnancy with IVF but needs further research to be validated as a clinical tool [8].
AMH for Fertility Preservation (FP) Prior to Cancer Therapy
Cancer treatment with chemotherapy and/or radiation is a known cause of premature ovarian insufficiency (POI) in reproductive age women and effectively renders them infertile. As rapid strides in cancer therapy allow more survival than ever before, a discussion regarding fertility preservation assumes great importance in these women. Several studies report a correlation between serum AMH levels prior to therapy with the ovarian reserve after completion of treatment [9]. Thus, measurement of AMH can give practical insights into the potential reproductive lifespan after completion of treatment [10].
Furthermore, pre-treatment AMH measurement can also assist in predicting cancer therapy-related amenorrhea significantly, especially in breast cancer patients [11]. These results can help physicians generate individualized risks of POI, have comprehensive discussions with their patients regarding residual ovarian function post-therapy and allow patients to make a well-informed decision as to undergo fertility preservation treatments or not.
An important caveat is that although AMH levels assist in determining ovarian reserve post-therapy, an individual susceptibility to gonadotoxicity should also be accounted for. Decanter et al. [12] showed different patterns of ovarian recovery (based on ultrasensitive AMH assays) in 32 patients treated for breast cancer with the same treatment protocol. Patients must also be informed that neither pre-treatment nor post-treatment AMH levels predict subsequent successful pregnancy and pregnancies can occur even with a markedly low serum AMH level.
The current gold standard technique for fertility preservation after controlled ovarian stimulation (COS) is oocyte/embryo vitrification. In healthy patients, recent data have suggested that 8–20 mature oocytes after COS are needed to achieve a reasonable success of live birth, but this number should be individualized according to age [13]. As serum AMH represents a good predictor of response to COS even in cancer patients, it is correlated with the number of oocytes that can be vitrified, and it can also aid in the calculation of recombinant FSH dose in the stimulation protocol [14].
A recent study reported the use of serum AMH to identify women with a greater likelihood of suffering from cancer therapy-related infertility, the rationale being that AMH is a very sensitive predictor of the number of primordial follicles in young women with healthy ovaries [15]. Early identification of these women will likewise assist physicians in making a timely referral to reproductive endocrinologists so that patients can have an open discussion regarding available options for preserving their fertility and set realistic expectations regarding future fertility, which in turn will enhance their quality of life after treatment by orders of magnitude.
Future Directions: Therapeutic Potential of AMH
Recombinant AMH is emerging as an exciting therapeutic modality in fertility preservation. As discussed, cancer therapy is known to be gonadotoxic through several possible mechanisms, including substantial toxicity on primordial follicles and/or on small antral follicles secreting AMH [16]. According to a newer model of gonadotoxicity termed the ‘burn-out effect,’ cancer therapy, especially cyclophosphamide, induces enormous recruitment of the residual inactive follicles which then undergo atresia [17]. Since AMH is a key regulator of the recruitment of primordial follicles, pre-treatment with recombinant AMH might restrict the gonadotoxicity and follicular depletion that accompany cancer therapy [18].
AMH in Ovarian Neoplasms
AMH has been identified as a tumor marker in adult granulosa cell tumors since a long time and levels are elevated in up to 93% cases [19]. More recent reviews have focused on the anti-proliferative effects of AMH on epithelial ovarian neoplasms. Although the precise mechanism is unknown, several hypotheses have been advanced, including inhibition of stem cell factor, activation of apoptotic pathways, as well as arrest of the cell cycle at the G1/S checkpoint in epithelial ovarian cancer cells [20]. Since stem cell factor is also an important mediator of tumor invasion, metastases and development of drug resistance, its suppression by AMH can theoretically reduce the likelihood of these outcomes and augment the relatively dismal 5-year survival rates of this malignancy. Thus, recombinant AMH holds great promise as an investigational targeted therapy in epithelial ovarian cancers.
AMH in Polycystic Ovaries Syndrome (PCOS)
PCOS is a widely prevalent disorder, affecting more than 100 million women worldwide. Most clinicians diagnose PCOS on the basis of the Rotterdam criteria [21]. However, these features, especially ultrasound appearance of the ovaries, can be menstrual cycle-dependent and/or be affected by oral contraceptive use. Hence, serum AMH which remains stable with cycles and is independent of oral contraceptive use has been explored as a diagnostic marker for PCOS, either alone or in combination with other markers to improve detection.
AMH levels are elevated in PCOS, reflecting the increased load of small antral follicles [22]. Ovarian surgery like ovarian drilling may reduce these AMH levels, and overzealous surgeries may lead to premature ovarian failure or insufficiency. Hyperandrogenism due to either insulin resistance and hyperinsulinism or LH excess is considered a key driver of intra-ovarian PCOS pathology and derives from increased synthesis of androgens by the theca cells of small antral follicles. However, testosterone assays in reproductive-age females frequently suffer from inaccuracy. As AMH is produced by granulosa cells of the same small antral follicles, it may be utilized as an indirect marker of the degree of intra-ovarian hyperandrogenism in these women. In light of these discoveries, it is plausible that once diagnostic thresholds have been established, AMH may well be considered indispensable for the diagnosis and assessment of severity of PCOS.
AMH in Pediatric Reproductive Endocrinology
AMH has numerous applications in clinical pediatrics. As discussed earlier, it is required for the physiologic involution of Mullerian ducts in male fetuses. Since AMH is the product of the Sertoli cells in the testes of males, a positive assay is evidence of testes being present in cryptorchidism and disorders of sex development [23]. In females, AMH can help localize the source of virilization: raised levels are found in testicular tissue-induced virilization, while levels are normal in congenital adrenal hyperplasia [23]. In children treated for ovotestis, AMH can identify the presence of testicular tissue before and after surgical intervention [24]. It is also useful in Klinefelter syndrome as its levels reflect the degree of testicular dysfunction in this condition [25]. Turner syndrome patients are especially likely to undergo accelerated depletion of ovarian follicles, and monitoring of AMH is an excellent indicator of premature ovarian insufficiency in these patients [26]. It is also being investigated as a test for differentiating hypogonadotropic hypogonadism from constitutional pubertal delay. Thus, AMH has established itself as a truly versatile marker in pediatric reproductive endocrinology.
AMH in Prediction of Age at Menopause
Declining AMH levels indicate gradual decrease in reproductive capacity with age; hence, they may be considered as a potential marker for menopause.
A recent study showed that every fall of AMH level by 0.10 ng/mL was related to a 14% increased risk of early menopause (p < 0.001) [27]. Another study reported that the combination of AMH and age was a more reliable predictor of early menopause than age alone [28]. Women above age of 40 with low AMH levels have shown improvements in ovarian reserve markers with DHEA supplementation. DHEA therapy has reported improvement in ovarian function, pregnancy rates and decreased embryo aneuploidy and miscarriage rate in infertile women predicted to have early menopause with low AMH [29, 30].
Conclusion
AMH is a signaling molecule of central importance for follicular recruitment and growth. In recent years, serum AMH has proven effective in evaluation of ovarian disorders in women, right from childhood to menopause. A significant advantage of serum AMH is its low intra-cycle and inter-cycle variability as it is produced from small antral follicles, which are gonadotropin independent. Its strong correlation with follicle numbers and high negative predictive value for premature ovarian insufficiency make it an attractive tool in the infertility specialist’s armamentarium. It also aids in individualization of ART protocols, thus minimizing iatrogenic effects as well as cost.
With cancer survival improving and quality of life in survivors gaining importance in reproductive-age women, serum AMH has been found to be useful in predicting ovarian reserve after completion of cancer therapy and can help physicians inform their patients regarding their risk of premature ovarian insufficiency. AMH lends itself to utilization as a diagnostic marker in PCOS due to the fact that its levels remain stable across cycles and are independent of oral contraceptive use. It also has significant scope in assisting the diagnosis of disorders of sexual development in clinical pediatrics.
Recombinant AMH therapy represents an exciting new direction in gynecologic oncology and fertility preservation. Significant improvements in understanding the functions of AMH and its potential to act as a targeted therapy with limited adverse effects make it a particularly attractive avenue to pursue. However, extensive clinical research is required to assess its safety and efficacy prior to its widespread use for this purpose. Thus, AMH has proven to be a pluripotent marker of clinical significance for all practicing gynecologists.
Dr. Laxmi Shrikhande
She is Medical Director and Senior Consultant at Shrikhande Hospital and Research Centre Pvt Ltd, Nagpur. She is Chairperson Designate ICOG 2020 and Senior Vice President FOGSI 2012. She has delivered 11 orations and 450 guest lectures. To her credit, she has 20 national and 11 international publications.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Laxmi Shrikhande is a Medical Director and Senior Consultant at Shrikhande Hospital and Research Centre Pvt Ltd, Nagpur, India. Bhushan Shrikhande is a Clinical Associate at Shrikhande Hospital and Research Centre Pvt Ltd, Nagpur, India. Aditya Shrikhande is a Research Associate at Shrikhande Hospital and Research Centre Pvt Ltd, Nagpur, India.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Cui L, Qin Y, Gao X, et al. Antimüllerian hormone: correlation with age and androgenic and metabolic factors in women from birth to postmenopause. Fertil Steril. 2016;105(02):481–485. doi: 10.1016/j.fertnstert.2015.10.017. [DOI] [PubMed] [Google Scholar]
- 2.Dumont A, Robin G, Catteau-Jonard S, et al. Role of anti-Müllerian hormone in pathophysiology, diagnosis and treatment of polycystic ovary syndrome: a review. Reprod Biol Endocrinol. 2015;13:137. doi: 10.1186/s12958-015-0134-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.La Marca A, Sighinolfi G, Radi D, et al. Anti-Mullerian hormone (AMH) as a predictive marker in assisted reproductive technology (ART) Hum Reprod Update. 2010;16(02):113–130. doi: 10.1093/humupd/dmp036. [DOI] [PubMed] [Google Scholar]
- 4.Iliodromiti S, Anderson RA, Nelson SM. Technical and performance characteristics of anti-Müllerian hormone and antral follicle count as biomarkers of ovarian response. Hum Reprod Update. 2015;21(06):698–710. doi: 10.1093/humupd/dmu062. [DOI] [PubMed] [Google Scholar]
- 5.Tal R, Seifer DB. Ovarian reserve testing: a user’s guide. Am J Obstet Gynecol. 2017;217(02):129–140. doi: 10.1016/j.ajog.2017.02.027. [DOI] [PubMed] [Google Scholar]
- 6.Yates AP, Rustamov O, Roberts SA, et al. Anti-Mullerian hormone-tailored stimulation protocols improve outcomes whilst reducing adverse effects and costs of IVF. Hum Reprod. 2011;26(9):2353–2362. doi: 10.1093/humrep/der182. [DOI] [PubMed] [Google Scholar]
- 7.Tokura Y, Yoshino O, Ogura-Nose S, et al. The significance of serum anti-Müllerian hormone (AMH) levels in patients over age 40 in first IVF treatment. J Assist Reprod Genet. 2013;30(6):821–825. doi: 10.1007/s10815-013-9991-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Karkanaki A, Vosnakis C, Panidis D. The clinical significance of anti-Müllerian hormone evaluation in gynecological endocrinology. Hormones. 2011;10(2):95–103. doi: 10.14310/horm.2002.1299. [DOI] [PubMed] [Google Scholar]
- 9.Peigne M, Decanter C. Serum AMH level as a marker of acute and long-term effects of chemotherapy on the ovarian follicular content: a systematic review. Reprod Biol Endocrinol. 2014;12:26. doi: 10.1186/1477-7827-12-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dillon KE, Sammel MD, Prewitt M, et al. Pretreatment anti-Müllerian hormone levels determine rate of posttherapy ovarian reserve recovery: acute changes in ovarian reserve during and after chemotherapy. Fertil Steril. 2013;99:477–483. doi: 10.1016/j.fertnstert.2012.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dunlop CE, Anderson RA. Uses of anti-Müllerian hormone (AMH) measurement before and after cancer treatment in women. Maturitas. 2015;80:245–250. doi: 10.1016/j.maturitas.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Decanter C, Cloquet M, Dassonneville A, et al. Different patterns of ovarian recovery after cancer treatment suggest various individual ovarian susceptibilities to chemotherapy. Reprod Biomed Online. 2018;36:711–718. doi: 10.1016/j.rbmo.2018.02.004. [DOI] [PubMed] [Google Scholar]
- 13.Cobo A, Garcia-Velasco JA, Coello A, et al. Oocyte vitrification as an efficient option for elective fertility preservation. Fertil Steril. 2016;105:755–764. doi: 10.1016/j.fertnstert.2015.11.027. [DOI] [PubMed] [Google Scholar]
- 14.Sermondade N, Sonigo C, Sifer C, et al. Serum anti-Müllerian hormone is associated with the number of oocytes matured in vitro and with primordial follicle density in candidates for fertility preservation. Fertil Steril. 2019;111:357–362. doi: 10.1016/j.fertnstert.2018.10.018. [DOI] [PubMed] [Google Scholar]
- 15.Fabbri R, Macciocca M, Melotti C, et al. Anti-Müllerian hormone as an ovarian reserve marker in young cancer women who undergo ovarian tissue cryopreservation. Future Oncol. 2014;10:1343–1351. doi: 10.2217/fon.14.76. [DOI] [PubMed] [Google Scholar]
- 16.Bedoschi G, Navarro PA, Oktay K. Chemotherapy-induced damage to ovary: mechanisms and clinical impact. Future Oncol. 2016;12(20):2333–2344. doi: 10.2217/fon-2016-0176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.L. Kalich-Philosoph, H. Roness, A. Carmely et al., “Cyclophosphamide triggers follicle activation and “burnout”; AS101 prevents follicle loss and preserves fertility,” Science Translational Medicine, vol. 5, no. 185, Article ID 185ra62, 2013. [DOI] [PubMed]
- 18.Roness H, Spector I, Leichtmann-Bardoogo Y, et al. Pharmacological administration of recombinant human AMH rescues ovarian reserve and preserves fertility in a mouse model of chemotherapy, without interfering with anti-tumoural effects. J Assist Reprod Genet. 2019;36:1793–1803. doi: 10.1007/s10815-019-01507-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Färkkilä A, Koskela S, Bryk S, et al. The clinical utility of serum anti-Müllerian hormone in the follow-up of ovarian adult-type granulosa cell tumors—a comparative study with inhibin B. Int J Cancer. 2015;137:1661–1671. doi: 10.1002/ijc.29532. [DOI] [PubMed] [Google Scholar]
- 20.Zhang T, Deng L, Xiong Q, et al. Anti-Müllerian hormone inhibits proliferation and induces apoptosis in epithelial ovarian cancer cells by regulating the cell cycle and decreasing the secretion of stem cell factor. Oncol Lett. 2018;16(3):3260–3266. doi: 10.3892/ol.2018.8985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lauritsen MP, Bentzen JG, Pinborg A, et al. The prevalence of polycystic ovary syndrome in a normal population according to the Rotterdam criteria versus revised criteria including anti-Müllerian hormone. Hum Reprod. 2014;29(4):791–801. doi: 10.1093/humrep/det469. [DOI] [PubMed] [Google Scholar]
- 22.Bungum L, Franssohn F, Bungum M, et al. The circadian variation in Anti-Müllerian hormone in patients with polycystic ovary syndrome differs significantly from normally ovulating women. PLoS ONE. 2013;8(9), Article ID e68223 [DOI] [PMC free article] [PubMed]
- 23.Lindhardt Johansen M, Hagen CP, Johannsen TH, et al. Anti-mullerian hormone and its clinical use in pediatrics with special emphasis on disorders of sex development. Int J Endocrinol. 2013;2013, Article ID 198698 [DOI] [PMC free article] [PubMed]
- 24.Josso N, Rey RA, Picard JY. Anti-müllerian hormone: a valuable addition to the toolbox of the pediatric endocrinologist. Int J Endocrinol. 2013;2013:674105. doi: 10.1155/2013/674105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Aksglaede L, Christiansen P, Sørensen K, et al. Serum concentrations of anti-Müllerian hormone (AMH) in 95 patients with Klinefelter syndrome with or without cryptorchidism. Acta Paediatr Int J Paediatr. 2011;100(6):839–845. doi: 10.1111/j.1651-2227.2011.02148.x. [DOI] [PubMed] [Google Scholar]
- 26.Visser JA, Hokken-Koelega ACS, Zandwijken GRJ, et al. Anti-Mullerian hormone levels in girls and adolescents with Turner syndrome are related to karyotype, pubertal development and growth hormone treatment. Hum Reprod. 2013;28(7):1899–1907. doi: 10.1093/humrep/det089. [DOI] [PubMed] [Google Scholar]
- 27.Bertone-Johnson ER, Manson JE, Purdue-Smithe AC, et al. Anti-Mullerian hormone levels and incidence of early natural menopause in a prospective study. Hum Reprod. 2018;33:1175–1182. doi: 10.1093/humrep/dey077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Depmann M, Eijkemans MJ, Broer SL, et al. Does AMH relate to timing of menopause? Results of an individual patient data meta-analysis. J Clin Endocrinol Metab. 2018;103:3593–3600. doi: 10.1210/jc.2018-00724. [DOI] [PubMed] [Google Scholar]
- 29.Gleicher N, Barad DH. Dehydroepisterone (DHEA) supplementation in diminished ovarian reserve (DOR) Reprod Biol Endocrinol. 2011;9:67. doi: 10.1186/1477-7827-9-67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sing V, Thakur P, Agrawal S, et al. Role of DHEA in diminished ovarian reserve, systematic review. World J Pharmaceut Res. 2015;4:2488–2507. [Google Scholar]


