Abstract
Objective
To correlate serial monitoring of lactic acid in pregnancy-associated sepsis (PAS) subjects with maternal prognosis.
Methods
All pregnant, post-abortal (2 weeks) and postpartum women with suspected sepsis fulfilling any 2 of the Quick Sequential Organ Failure Assessment criteria were considered as cases. Lactic acid was measured at 0, 24 and 48 h of admission, and lactate clearance was calculated.
Results
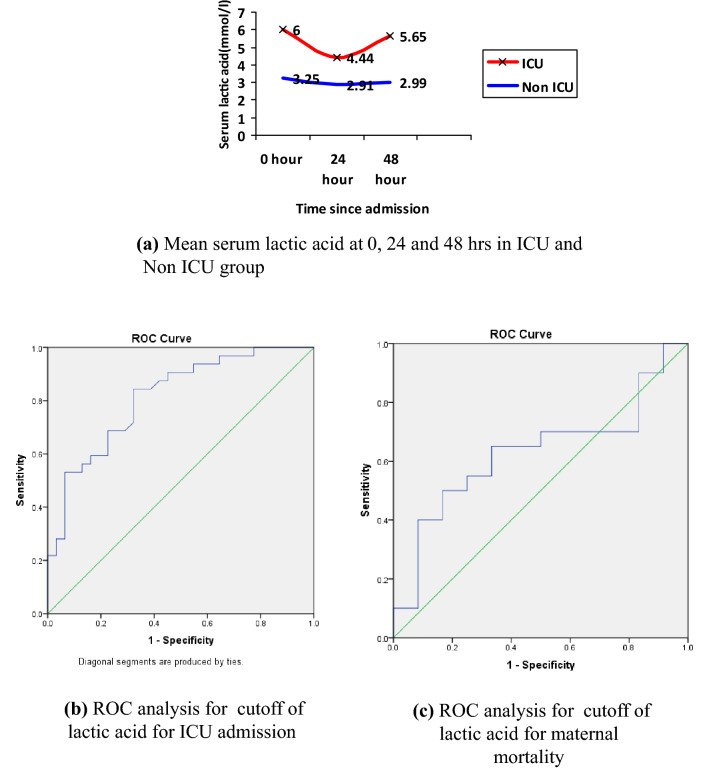
The mean value of lactic acid was significantly higher in the Intensive Care Unit (ICU) group than the Non-ICU group at 0, 24, and 48 h with values being (6.00 ± 2.46 mmol/l vs 3.25 ± 1.92 mmol/l), (4.44 ± 2.24 mmol/l vs 2.91 ± 1.77 mmol/l) and (5.65 ± 2.91 mmol/l vs 2.99 ± 1.93 mmol/l), respectively. Lactic acid in the survivor group was significantly lower as compared to the mortality group (3.79 ± 0.32 mmol/l vs 7.3 ± 0.56 mmol/l). A cut-off of 3.8 mmol/l with area under the curve of 0.814 has a sensitivity of 84% and specificity of 68% for predicting ICU admission. The mean lactate clearance was 46% in cases who survived and 22.5% in cases who had mortality. When lactate clearance was 60%, no mortality was seen, whereas when there was 100% rise in lactic acid, they all had mortality.
Conclusion
The mean lactic acid at 0, 24 and 48 hours was significantly higher in the ICU group as compared to the Non-ICU group. Serum lactic acid at zero hours of the presentation was significantly higher in ICU cases. Lactate clearance (fall) helps to prognosticate as fall of ≥ 60% lactic acid level is associated with 100% survival, whereas a rise of 100% in serum lactic acid is associated with 100% mortality.
Keywords: Serial lactic acid, ICU, Pregnancy-associated sepsis, Mortality, SOFA score
Introduction
Sepsis is a life-threatening organ dysfunction due to dysregulated host response to infection. End organ damage is identified as an acute change in total Sequential Organ Failure Assessment Score (SOFA) [1]. Infection in pregnancy is not reliably detected by commonly used laboratory tests like WBC and C-reactive protein (CRP) as they are frequently raised in healthy pregnant females too. According to WHO, sepsis is one of the four main causes of maternal mortality together with haemorrhage, hypertensive disease and abortion [2].
Serum lactate is a surrogate marker of tissue perfusion; increased lactic acid signifies tissue hypoxia. Serum lactate is produced by accelerated aerobic glycolysis driven by excess beta-adrenergic stimulation [3]. Randomized controlled trials have demonstrated a significant reduction in mortality with lactate-guided resuscitation. If initial lactate is elevated (> 2 mmol/l), it should be remeasured within 2–4 h to guide resuscitation to normalize lactate levels [4].
Lactic acid in sepsis has been advocated in SSC 2016 guidelines as a prognostic marker, and serial lactic acid monitoring and lactic acid clearance can also predict mortality [1]. Reliable clinical and microbiological parameters that may be used to diagnose obstetrics’ sepsis are lacking. Microbiological cultures lead to diagnostic delay, suboptimal sensitivity and specificity. We assessed the role of serial monitoring of lactic acid in pregnancy-associated sepsis (PAS) and its association with ICU admission and mortality. Since it is a rapid assay, a speedy intervention can be made and sepsis-related morbidity and mortality can be reduced which will help us to improve maternal health quality.
Materials and Methods
After obtaining ethical clearance from institutional ethics committee, the study was carried out from November 2017 to October 2018 in a tertiary care hospital. During this period of 12 months, there were 19,459 deliveries (live + still births + abortion) and 19,216 live births. A total of 70 cases were screened, and those satisfying two or more qSOFA criteria were enrolled, i.e. 63 PAS cases were enrolled. Demographic detail and risk factors (such as income status, education, history of dai handling, anaemia and chronic disease) for development of sepsis in our cases were assessed and recorded. Detailed routine investigations like complete blood count, liver function test, kidney function test and coagulation profile were performed. Culture and sensitivity reports were obtained for blood, urine, pus and high vaginal swab. Two ml of blood sample was collected in plain vial for lactic acid analysis at 0, 24 and 48 h of admission, serum was separated immediately and stored in aliquots at -80 degrees centigrade, and analysis is done by colorimetric assay. The maternal outcome was noted in the form of requirement of ICU admission and maternal mortality. ICU admission was decided on the basis of study conducted by Nates et al. [5] which was used to prioritize the cases who needed ICU care. Critically ill cases, i.e. those who required life support like invasive ventilation, continuous renal replacement therapies and haemodynamic monitoring, were first priority for ICU admission. Cases were followed up till discharge or mortality. Organ failure assessment was done, and SOFA score was calculated for all cases. We evaluated levels of serum lactic acid in cases of PAS at 0, 24 and 48 h of admission, and comparison was done between ICU and Non-ICU groups. Treatments such as inotropes, antibiotics and blood transfusions were administered as per hospital protocol and were recorded.
Results
In our hospital rate of sepsis are approximately 3.23 per 1000 deliveries and 3.27 per 1000 live births. We enrolled a total of 63 cases of PAS. Out of these cases, 32 (50.7%) were admitted to ICU and 31 were not admitted to ICU. The rate of septicaemia, i.e. blood culture positivity in PAS cases, in our study was 26.9%. Twenty out of 63 cases expired, giving a mortality rate of 30.1%. All the mortalities were reported from the ICU group. Both the ICU and Non-ICU groups were comparable in age, religion, socio-economic status and education as depicted in Table 1.
Table 1.
Socio-demographic characteristics of 63 cases
| Parameters | No. of cases n = 63 (%) | Group A (ICU PAS) N = 32 |
Group B (Non-ICU) n = 31 |
p value** |
|---|---|---|---|---|
| Age (years) | ||||
| 20–24 | 20 (31.7%) | 11 | 9 | 0.52 |
| 25–30 | 43 (62.6%) | 21 | 22 | |
| Religion | ||||
| Hindu | 36 (57.1%) | 15 | 21 | 0.051 |
| Muslim | 27 (42.8) | 17 | 10 | |
| Others | 00 | |||
| Socio-economic* | ||||
| Lower | 45 (71.4%) | 22 | 23 | 0.197 |
| Middle | 18 (28.5%) | 10 | 8 | |
| Upper | 00 | |||
| Education | ||||
| Illiterate | 47 (74.6%) | 26 | 21 | 0.114 |
| Up to 10th class | 14 (22.2%) | 5 | 9 | |
| Graduate | 02 (3%) | 1 | 1 |
Majority of PAS cases were postpartum, i.e. 55.5%, 33.3% were antenatal and 11.2% were post-abortal. The most common risk factor in PAS cases was anaemia seen in 85.7% cases followed by unbooked status in 64% and poor nutrition in 57.1%. Septicaemia was seen in 26.9% cases, UTI in 25.3% cases, genital infection in 12.6% and wound infection in 0.06% cases. Total SOFA score was calculated for all the cases and compared for various maternal outcomes. ICU admission was required in all cases with a score of more than 12, but only 41% of cases with a SOFA score less than or equal to 12 required an ICU admission. All the cases in the Non-ICU group had a SOFA score less than or equal to 12. The mean SOFA score for ICU cases was significantly higher than that of the Non-ICU group (10.7 vs 5.2, p value = 0.00). Mean SOFA score of the cases who expired was significantly higher than the cases who survived (12.0 vs 6.1, p value = 0.00). On detailed organ failure assessment, the most common organ system involved was respiratory followed by kidney.
Lactic acid levels were monitored serially at 0 h, 24 h and 48 h of admission in both ICU and Non-ICU groups. The mean value of lactic acid at 0, 24 and 48 h was 6.00 ± 2.46 mmol/l, 4.44 ± 2.24 mmol/l and 5.65 ± 2.91 mmol/l, respectively, in the ICU group and 3.25 ± 1.92 mmol/l, 2.91 ± 1.77 mmol/l and 2.99 ± 1.93 mmol/l in the Non-ICU group as shown in Fig. 1, and the difference was statistically significant (p value < 0.05). On ROC analysis, we found that lactic acid cut-off value of 3.8 mmol/l had best sensitivity and specificity, i.e. 84%,68% (AUC = 0.814, p value = 0.035) and 82.5%, 17% (AUC = 0.629, p value = 0.228) for ICU admission and prognosticating regarding survival, respectively (Figure 1b, c). Majority of ICU PAS subjects (78%) had lactic acid more than equal to 4 mmol/l. Lactic acid value of 4 mmol/l had a sensitivity of 78% and specificity of 68.1% for ICU admission. We also compared the cut-off of 4 mmol/with the maternal outcomes like ICU admission, number of organ failure, duration of hospital stay and maternal mortality, and it was found to be statistically significant for all of them as described in Table 2.
Fig. 1.
Mean serum lactic acid of ICU group and ROC analysis for cutoff of lactic acid with ICU admission and maternal mortality
Table 2.
Maternal outcome with lactic acid
| ≥4 mmol/l | <4 mmol/l | *p value | |
|---|---|---|---|
| ICU admission | 25 | 7 | 0.00 |
| Culture positive | 21 | 24 | 0.176 |
| No. of organ failure | 0.05 | ||
| 0 | 03 | 4 | |
| 1 | 16 | 20 | |
| 2 | 10 | 04 | |
| 3 | 05 | 0 | |
| Duration of hospital stay | 0.03 | ||
| <1 day | 5** | 0 | |
| 2–4 days | 9 | 4 | |
| 5–9 days | 1 | 5 | |
| > 10 days | 20 | 19 | |
| Maternal mortality | 15 | 5 | 0.034 |
*Chi-square test, p value < 0.05
**All 5 cases had mortality for < 24 h
Out of 20 mortality cases, 5 cases expired even before 24 h of admission. All mortalities were seen in the ICU group. The mean lactic acid for these 5 cases was 8.3 ± 1.0 mmol/l, and range of lactic acid was 6–12 mmol/l. The mean lactic acid at 0 h in cases who expired after 24 h was significantly higher as compared to who survived (7.3 ± 0.56 mmol/l vs 3.79 ± 0.32 mmol/l p value = 0.03). We compared serial lactic acid in the ICU group between survivors and mortality group. The mean lactic acid at 24 h and 48 h in the mortality group was found to be significantly higher as compared to cases who survived. The lactic acid levels in all mortality cases were compared with total cases (ICU + Non-ICU) who survived, and 48-h mean lactic acid was also found to be significantly higher in cases who expired (7.38 ± 1.92 mmol/l vs 3.13 ± 2.08, p value = 0.025). This is depicted in Table 3.
Table 3.
Comparison of lactic acid in ICU cases in between mortality and survival groups
| Lactic acid | Mortality(n = 20)(ICU) | Survival (ICU) (n = 12) | p value |
|---|---|---|---|
| 0 h | 6.4 ± 2.5(n = 20) | 5.1 ± 2.0 | 0.150 |
| 24 h | 5.26 ± 2.2 (n = 15) | 3.43 ± 1.8 | 0.032 |
| 48 h | 7.39 ± 1.9(n = 15) | 3.48 ± 2.4 | 0.000 |
| Mortality cases (n = 20) | Survival cases (n = 43)(ICU + Non-ICU) |
||
|---|---|---|---|
| 0 Hour | 6.4 ± 2.59 | 3.79 ± 2.12 | 0.265 |
| 24 Hour | 5.25 ± 2.2 | 3.06 ± 1.80 | 0.294 |
| 48 Hour | 7.38 ± 1.92 | 3.13 ± 2.08 | 0.025 |
Various ratios of lactic acid in 15 cases of mortality beyond 24 h were analysed and compared to maternal mortality. Rise in lactic acid at 48 h (Ratio > 1) was seen in 11 out of 15 cases in the mortality group (p value = 0.045) as depicted in Table 4. The percentage fall, i.e. lactic acid clearance [(lactic acid 48 h–lactic acid 0 h)/lactic acid 0 h], was analysed and correlated with mortality in both the groups. Lactate clearance was seen in 39% PAS cases (31 out of 63) out of which 83.3% survived. In our study, the mortality rate in the lactate clearance group was 17% and in the nonclearance group was 37%. The range of lactate clearance varied from 0 to 100%. The mean lactate clearance was 46% in cases who survived and 22.5% in cases who had mortality. We observe that with a fall of ≥ 60% in lactic acid no mortality was seen in PAS cases. We also calculated the percentage rise in lactic acid and observed that out of 27 cases 8 cases, i.e. 40.7%, had mortality. All cases with more than 100% rise (4/4) had mortality as depicted in Table 5.
Table 4.
Ratio of lactic acid at 0, 24 and 48 h with mortality
| Lactic acid ratio | Maternal mortality N = 15 |
No maternal mortality N = 12 |
p value* |
|---|---|---|---|
| 48HR/0HR | 0.045 | ||
| ≤1 (fall) | 4 | 8 | |
| >1 (rise) | 11 | 4 | |
| 24HR/0HR | 0.262 | ||
| ≤1 | 6 | 8 | |
| >1 | 9 | 3 | |
| 48HR/24HR | 0.095 | ||
| ≤1 | 2 | 5 | |
| >1 | 13 | 6 | |
*Chi-square test, p value < 0.05
Table 5.
Comparison of percentage lactic acid fall and rise with mortality
| % fall in lactic acid | ICU (n = 13) |
Mortality in ICU cases | Non ICU (n = 18) |
Mortality in Non ICU cases |
|---|---|---|---|---|
| 0–20% | 4 | 2 | 4 | 0 |
| 20–40% | 1 | 1 | 4 | 0 |
| 40–60% | 5 | 1 | 4 | 0 |
| 60–80% | 1 | 0 | 4 | 0 |
| % rise in lactic acid | ICU (n = 14) |
Mortality in ICU cases | Non ICU (n = 13) |
Mortality in Non ICU cases |
|---|---|---|---|---|
| < 50% | 8 | 6 | 5 | 0 |
| 50–100% | 1 | 1 | 2 | 0 |
| 100–200% | 2 | 2* | 2 | 0 |
| > 200% | 2 | 2* | 4 | 0 |
*2/2 cases expired
To summarize a cut-off ≥ 4 mmol/l at admission, lactic acid 48 h-to-lactic acid 0 h ratio ≥ 1 and 100% rise in lactic acid, i.e. doubling of lactic acid, is indicative of poor survival, whereas a lactate clearance of ≥ 60% has 100% survival. Therefore, we suggest serial monitoring of lactic acid as a useful tool to prognosticate patient for maternal outcome. A rise of lactic acid at 24 or 48 h is a caution for intensifying management to prevent mortality in PAS.
Discussion
Serum lactate is a useful prognostic tool for sepsis. Serum lactate is produced by accelerated aerobic glycolysis driven by excess beta-adrenergic stimulation [3]. As septic shock develops, there is organ dysfunction and a decrease in clearance of lactic acid and a further increase in serum lactic acid levels are noted. Therefore, serial monitoring of lactic acid has importance in the prognosis of the cases of sepsis. Lactate-guided resuscitation has shown a significant reduction in mortality.
We compared serum lactic acid levels in PAS cases at admission, at 24 h and 48 h between ICU and Non-ICU group. On plotting ROC curves, a cut-off of 3.8 mmol/l was considered best for prognosticating ICU admission. Alveera et al. [6] observed that 64.2% of cases had lactic acid ≥ 2.2 mmol/l in pregnancy-associated sepsis and their data were in cohesion with our data. Albright et al. [7] found similar result of serum lactic acid concentration of 4 mmol/l as an indicator of severe sepsis. According to his study, the area under the curve for the prediction of ICU admission was 0.72 and a cut-off of 2.5 mmol/l had a sensitivity of 63% and specificity of 85%. In our study, 96.8% PAS cases admitted to ICU had lactic acid levels more than equal to 2 mmol/l and 78% had lactic acid more than equal to 4 mmol/l. Similarly, Agarwal et al. [8] had found that a cut-off of 4 mmol/l had a sensitivity of 37.9%, specificity of 88.1% and positive predictive value of 81.4% for the severity of PAS. Hence, from our study, it was postulated that lactic acid value of 2 mmol/l and 4 mmol/l had a sensitivity of 96.9%,78% and specificity of 23%, 68.1% for ICU admission, respectively. The cut-off of 4 mmol/l was statistically significant for predicting ICU admission, number of organ failure and duration of hospital stay (p value = 0.00,0.05,0.03, respectively). Multiorgan failure was seen in 19 out of 63 cases out of which 16 were admitted in ICU. Though there are supporting data for corroboration of lactic acid with a number of organ failure, our study results were not statistically significant. A study by Agarwal et al. [9] found that the mean values of lactic acid for 2 and 3 organ failures were 3.25 ± 0.92 mmol/l and 3.89 ± 0.80 mmol/l, respectively, and mean lactic acid levels for multiorgan failure (3.70 ± 0.81) mmol/l) cases were significantly high as compared to single-organ failure (3.02 ± 0.92 mmol/l) (p value = 0.006). Analysis of lactic acid levels in relation to mortality showed that the mean lactic acid in 5 cases who expired before 24 h was very high, i.e. 8.3 ± 1.0 mmol/l. The mean lactic acid at 0 h in cases who expired after 24 h was significantly higher as compared to cases who survived (7.3 ± 0.56 vs 3.79 ± 0.32 p value = 0.03). The mean lactic acid even at 48 h was found to be significantly high in cases who had mortality compared to cases who survived. Rise in lactic acid at 48 h (Ratio > 1) was found to be statistically significant to predict mortality (p value = 0.045). In our study, the mortality rate in the lactate clearance group was 17% and in the nonclearance group was 37% which was consistent with the findings of a study by Bhatt et al. [8] according to which mortality rate in the lactate clearance group was 15.2% as compared to 36.1% in the lactate nonclearance group. When lactic acid clearance was PAS subjects with lactate clearance ≥ 60% at 48 h, whereas all cases with a 100% rise in lactic acid had mortality.
Thus, from our study, we suggest that serial monitoring of lactic acid is a useful tool for prognostication and lactate clearance is associated with better survival in pregnancy-associated sepsis. Increase in lactate levels represents tissue hypoxia which leads to more targeted resuscitation by aggressive fluid administration, thereby reversing tissue hypoxia and hence organ failure at pulmonary level. Also, lactate clearance was associated with a decrease in inflammatory biomarkers and improved organ function. SSC guidelines 2018 update also postulated that if initial lactate levels were more than > 2 mmol/l, lactate should be remeasured within 2–4 h and resuscitation should be done to normalize lactate. Early lactate-guided resuscitation has shown significant reduction in morbidity and mortality.
The strength of our study was that we did a prospective study over a period of 12 months on serial lactic acid levels monitoring in a tertiary care hospital which caters to a large number of patients from Delhi and UP including all the referral cases.
In a country like India with poor socio-economic conditions, sepsis has a crucial impact on maternal mortality, and it is important to do a narrative study so that sepsis is dealt with a wiser approach and early lactate-guided resuscitation as recommended by SSC 2018 [1, 2] is started. Serial lactate monitoring can help in triaging patients who require intensive monitoring and care, i.e. ICU admission, and is helpful in developing countries where there is scarcity of beds. Hence, we suggest that lactic acid is an independent marker of sepsis that is unaltered by physiological changes of pregnancy and its serial monitoring can be used to prognosticate obstetric sepsis.
The limitations for the study were that we could not assess the change of antibiotics or other management according to change in lactic acid and we could not compare it with healthy pregnant cases. We did not correlate maternal lactic acid levels with neonatal sepsis, and thus, our study could not say whether measurement of serum lactic acid could indicate neonatal sepsis.
Conclusion
Our tertiary care institution with a PAS rate of 3.23 per 1000 deliveries had 63 cases of PAS with 50.1% ICU admission and a mortality rate of 30%. It was seen that mean lactic acid at 0 h, 24 h and 48 h was significantly higher in Group A (ICU PAS) as compared to Group B (Non-ICU PAS)(p value < 0.05). A cut-off of 3.8 mmol/l with AUC of 0.814 has a sensitivity of 84% and specificity of 68% for predicting ICU admission in Indian obstetric population. Lactate clearance (fall) helps to prognosticate as a fall of ≥ 60% lactic acid level is associated with 100% survival, whereas a rise of > 100% in serum lactic acid is associated with 100% mortality.
Recommendations
We recommend serial lactate monitoring from admission to 48 h for prognosis and analysis of lactate clearance to guide resuscitation measures and improve survival.
Dr Penzy Goyal
is a postgraduate student in the Department of Obstetrics and Gynecology at University College of Medical Sciences (UCMS), Delhi. She was born in Delhi in 1993 and did her schooling in Delhi and MBBS in UCMS, Delhi. Her fields of interests include high-risk pregnancy and gynaecological oncology. She is a member of Association Of Obstetric and Gynaecology of Delhi (AOGD). She has completed her research work under the guidance of Professor Rachna Agarwal (Department of Obstetric and Gynaecological UCMS) after obtaining the institutional ethical clearance. Through her research work “Serial monitoring of lactic acid in PAS subjects”, she has tried to emphasize the need for serial lactic acid monitoring in order to guide resuscitation.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Statements
All investigations and procedures in the study were in accordance with the ethical standards of the institution.
Informed Consent
Informed consent was obtained from all individual participants included in the study. In case of critically ill and unconscious patient, consent with available close relative was taken.
Footnotes
Penzy Goyal, Postgraduate student, Department of Obstetric and Gynaecology UCMS, Delhi; Rachna Agarwal, Professor, Department of Obstetric and Gynaecology UCMS, Delhi; Himsweta Srivastava, Assistant Professor, Department of Obstetric and Gynaecology UCMS, Delhi; Rajarshi Kar, Assistant Professor, Department of Biochemistry, UCMS; Medha Mohta, Director Professor, Department of Anaesthesia, UCMS Delhi; Meera Sikka, Director Professor and Head Department of Pathology, UCMS, Delhi.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi: 10.1007/s00134-017-4683-6. [DOI] [PubMed] [Google Scholar]
- 2.Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315(8):801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Casserly B, Phillips GS, Schorr C, et al. Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med. 2015;43:567–573. doi: 10.1097/CCM.0000000000000742. [DOI] [PubMed] [Google Scholar]
- 4.Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Crit Care Med. 2018;46(6):997–1000. doi: 10.1097/CCM.0000000000003119. [DOI] [PubMed] [Google Scholar]
- 5.Nates JL, Nunnally M, Kleinpell R, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016;44(8):1553–1602. doi: 10.1097/CCM.0000000000001856. [DOI] [PubMed] [Google Scholar]
- 6.Alveera, Cunha PD. Serum lactic acid: an independent predictor of severe sepsis in obstetric patients. Int J Rec Trends Sci Technol. 2014;13(1):5–10. doi: 10.14445/22315381/IJETT-V13P202. [DOI] [Google Scholar]
- 7.Albright CM, Ali TN, Lopes V, et al. Lactic acid measurement to identify risk of morbidity from sepsis in pregnancy. Am J Perinatol. 2015;32(5):481–486. doi: 10.1055/s-0034-1395477. [DOI] [PubMed] [Google Scholar]
- 8.Agarwal R, Yadav RK, Garg S et al. Lactic acid as an adjuvant marker in pregnancy-associated sepsis. S Afr J Obstet Gynaecol [S.l.], v. 24, n. 1, p. 8-10, may. 2018. ISSN 2305-8862. Available at: http://www.sajog.org.za/index.php/SAJOG/article/view/1219. Date Accessed 29 Mar 2019.
- 9.Bhat SR, Swenson KE, Francis MW, et al. Lactate clearance predicts survival among patients in the emergency department with severe sepsis. West J Emerg Med. 2015;16(7):1118–1126. doi: 10.5811/westjem.2015.10.27577. [DOI] [PMC free article] [PubMed] [Google Scholar]