Abstract
Background
Compared to White and high socioeconomic status (SES) patients, Black and low SES patients receive less adequate pain care. Providers may contribute to these disparities by making biased decisions that are driven, in part, by their attitudes about race and SES.
Purpose
We examined the effects of patient race and SES on providers’ chronic pain decisions and the extent to which providers’ implicit and explicit attitudes about race and SES were related to these decisions.
Methods
Physician residents/fellows (n = 436) made pain care decisions for 12 computer-simulated patients with chronic back pain that varied by race (Black/White) and SES (low/high). Physicians also completed measures assessing implicit and explicit attitudes about race and SES.
Results
There were three significant race-by-SES interactions: (a) For high SES patients, Black (vs. White) patients were rated as having more pain interference; the opposite race difference emerged for low SES patients. (b) For high SES patients, Black (vs. White) patients were rated as being in greater distress; no race difference emerged for low SES patients. (c) For low SES patients, White (vs. Black) patients were more likely to be recommended workplace accommodations; no race difference emerged for high SES patients. Additionally, providers were more likely to recommend opioids to Black (vs. White) and low (vs. high) SES patients, and were more likely to use opioid contracts with low (vs. high) SES patients. Providers’ implicit and explicit attitudes predicted some, but not all, of their pain-related ratings.
Conclusion
These results highlight the need to further examine the effects of patient race and SES simultaneously in the context of pain care.
Keywords: Chronic pain, Race, Socioeconomic status, Disparities, Decision making, Attitudes
Providers were influenced by patient race and socioeconomic status, as well as their own attitudes about race and socioeconomic status, when making pain care decisions
Introduction
Black and low socioeconomic status (SES) patients are at heightened risk for suboptimal pain care. Compared to White and high SES counterparts, Black and low SES patients are less likely to have their pain assessed and diagnosed [1–3]. Providers may be more concerned about Black and low SES patients not adhering to treatment recommendations and/or misusing medications [4, 5], which likely contributes to these patients receiving fewer pain treatments, including opioids and other modalities [2, 6, 7]. Black and low SES individuals are also less likely to be rated as requiring disability benefits, and they have poorer biopsychosocial outcomes (e.g., worse mental health, more financial strain) after pain-related disability settlements [3, 8].
Patient race and SES are intertwined and likely interact to have direct and indirect effects on providers’ pain-related decisions [9]. Prior work in health disparities often controls for SES in an attempt to illuminate the unique effects of patient race [10]. However, this approach may produce results showing a significant SES effect but not a significant race effect, leading to the erroneous conclusion that race does not matter [9]. Yet, the socioeconomic distribution is not equal for Black and White populations. Black individuals are twice as likely to live in poverty or be unemployed than White individuals [11]. Thus, it is misguided—phenomenologically and statistically—to attempt to control for the effects of SES in order to understand racial disparities in pain care. Empirical research is needed to examine the effects of both race and SES as primary variables of interest on providers’ pain-related judgments.
Providers’ implicit and explicit attitudes have potentially important effects on their pain-related judgments. Implicit attitudes are automatic evaluations that occur without awareness, whereas explicit attitudes are deliberate and conscious [12]. Some studies have shown that providers with pro-White implicit attitudes are more likely to deliver care to White than Black patients [13, 14]. However, the overall evidence for the association between implicit racial attitudes and provision of care is mixed [15]. Less is known about providers’ implicit attitudes about SES, which is an important knowledge gap given the overlap between race and SES. Of the few conducted studies, none found a significant relationship between providers’ implicit attitudes about SES and their clinical decisions [16–19]. In terms of providers’ explicit attitudes, strong links have not been found with clinical care [20, 21]. A key limitation is that this previous work has not examined implicit and explicit attitudes in the context of chronic pain, which may be particularly susceptible to the influence of patient demographics and provider biases given its subjective nature and clinical uncertainty [22]. In this context, providers’ demographic-based attitudes may “fill in the gaps” of insufficient or ambiguous information, resulting in systematic differences in chronic pain care across race and SES groups [22].
The current study used virtual human (VH) technology and lens model design to investigate the extent to which patient race and SES influence providers’ pain-related decisions, and the extent to which providers’ implicit and explicit attitudes are related to these decisions. As with prior decision-making studies, VH technology is particularly well-suited to this study due to its combination of realism and control [23–25]. We had three main hypotheses. First, we hypothesized that providers would rate Black (vs. White) and low (vs. high) SES patients as experiencing less pain-related interference and distress and would be less likely to recommend them opioid analgesics but more likely to use an opioid contract with them. We also expected providers to be less likely to recommend workplace accommodations to Black and low SES patients. Our second hypothesis was that patient race and SES would interact so that providers would provide the most conservative care (i.e., lower opioid, higher opioid contract, and lower workplace accommodation ratings) to patients who were both Black and low SES. Our third hypothesis was that providers’ implicit and explicit attitudes about race and SES would moderate the relationship between patient group (race or SES) and providers’ pain-related decisions, such that providers with pro-White and pro-high SES attitudes would rate Black and low SES patients as experiencing less pain-related interference and distress and would recommend them the most conservative care. Lastly, we explored the relationship between provider characteristics (e.g., race, sex) and their pain-related decisions and attitudes.
Methods
Participants
Participants (“providers”) were recruited from physician residency and fellowship programs across the USA through e-mail, word of mouth, and posted fliers (local sites). Eligible participants were at least 18 years old, English speaking, enrolled in an accredited physician residency or fellowship, and had access to a computer. Residents and fellows were recruited because they deliver patient care and, thus, provide meaningful data about factors that influence pain care decision making early in providers’ careers.
We recruited 502 providers for the study. Of those, 7 did not meet eligibility requirements and 59 did not complete the pain decision-making task, yielding a final sample of 436 providers (Table 1). The sample was predominately male (59%) with a mean age of 29.7 years (SD = 3.1). Approximately 68% identified as White, 25% as Asian, 2% as Black, and 5% as other or not reported. Approximately 5% identified as Hispanic. The majority worked in a hospital setting (81%). On average, providers rated their clinical experience with chronic pain as 41.4 (SD = 23.7) on a 0 (not at all experienced) to 100 (very experienced) scale.
Table 1.
Provider Characteristics
| N = 436 | n (%)/mean (SD) |
|---|---|
| Sex | |
| Male | 255 (59%) |
| Female | 181 (41%) |
| Age (years) | 29.72 (3.08) |
| Race | |
| White | 297 (68%) |
| Asian | 110 (25%) |
| Black | 9 (2%) |
| Other/Not reported | 20 (5%) |
| Ethnicity | |
| Not Hispanic | 416 (95%) |
| Hispanic | 20 (5%) |
| Practice setting | |
| Hospital | 354 (81%) |
| Outpatient clinic | 49 (11%) |
| Other/Not reported | 33 (8%) |
| Health care experience | |
| <1 year | 330 (76%) |
| 1–4 years | 94 (21%) |
| 5–9 years | 12 (3%) |
| Clinical experience with pain (0–100) | 41.40 (23.74) |
Study Design and Procedures
This study is a planned secondary analysis of baseline data from a larger randomized controlled trial testing a virtual-perspective taking intervention to reduce racial and SES disparities in pain care [26]. We employed a lens model design in which participants weigh environmental “cues” to make decisions [27]. Lens model studies often present a series of profiles with cues that participants may “use” (i.e., are influenced by) to make decisions. This methodology has previously been employed in studies of medical decision making, including pain care [24, 28, 29]. In the current study, we were interested in the two patient cues of race (Black/White) and SES (low/high). Four unique profiles were needed to represent each possible cue combination (two levels of race × two levels of SES). Patients also varied by sex equally across race and SES categories, but patient sex was not investigated in the current study. All other patient variables were matched across profiles. To enhance the reliability of the decision-making data and maximize statistical power, we created 12 unique patient profiles so that each cue combination was presented thrice to each provider [30].
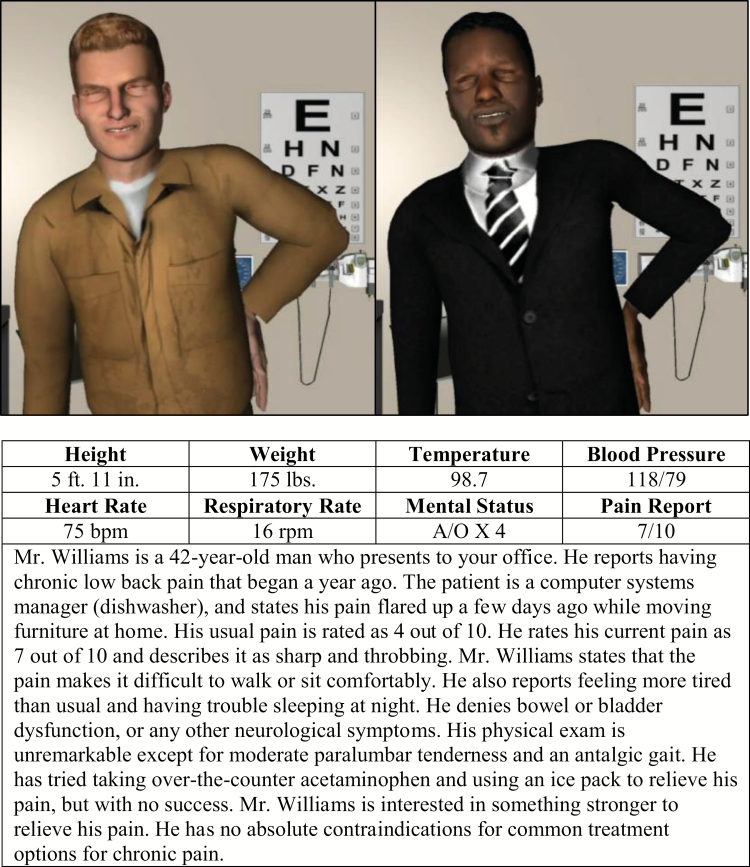
Each patient profile consisted of a virtual patient video and text vignette (Fig. 1). Videos were created with AutoDesk Character Generator, which allows for the development of realistic VHs. This program can apply standardized facial expressions and other parameters to patients of different sociodemographic groups of interest (i.e., race and SES), which maximizes experimental control and ecological validity. The VH videos were 30 s long, continuously looped, and depicted patients from the waist up seated in a standard outpatient exam room. The patients conveyed pain through facial expressions and body posture (i.e., bracing their lower back). Patient race was distinguished by altering skin color and facial phenotypes. Patient SES was indicated by occupation and depicted by clothing (and associated text-based descriptions [see below]; [9]). Low SES patients wore clothing associated with low-income/prestige jobs (e.g., fast food worker, hotel housekeeping), and high SES patients wore clothing associated with high-income/prestige jobs (e.g., lawyer, computer programmer; [31]). These videos have been used in previous studies, and prior work has demonstrated that laypersons, medical trainees, and physicians can reliably differentiate VH patients’ characteristics (e.g., race, sex, age; [25, 32]).
Fig. 1.
Still images taken from full-motion video of virtual patients with pain (White/low socioeconomic status [SES] patient [left pane] and Black/high SES patient [right pane]) and an example text vignette for a high SES patient with parenthetical content representing a low SES patient.
Each VH video was accompanied by a text vignette. Patients were described as having chronic low back pain. Vignettes also contained additional patient information, including vital signs, self-reported pain intensity (average 7–9/10), daily impact of pain, treatment history, and occupation. Information presented in the vignettes slightly varied across patients to enhance clinical realism but was otherwise equivalent apart from patient occupation. Stated occupation systematically varied to match patients’ clothing, such that low SES patients were described as having low income/prestige jobs, while high SES patients were described as having high income/prestige jobs. The order of patient videos was randomized.
The study was delivered online. Data were collected between May 2016 and July 2017. Providers were given a unique username to access the study website. Upon entering the website, the initial page stated that the purpose of the study was to gain a better understanding of how health care providers make decisions about pain assessment and treatment. Providers were not informed about the intervention component of the parent study. After consenting to participate, providers completed a demographic questionnaire, completed a measure of social desirability, viewed videos of and made pain assessment and treatment decisions for 12 VH patients with chronic pain, and completed measures of their implicit and explicit attitudes about race and SES. Tasks were randomized for each provider. Providers were compensated with a gift card for participating. This study was approved by the local Institutional Review Board.
Measures
Demographic questionnaires
Providers reported their age, sex, race, ethnicity, practice setting, health care experience (years), and experience with pain on a visual analog scale (VAS; 0 “not at all experienced” – 100 “very experienced”).
Pain assessment and treatment recommendation ratings
For each patient, providers made five ratings on separate VASs (0–100). Providers rated the “level of pain-related interference in daily activities” and the “level of distress” they thought the patient had been experiencing over the past few days from “no interference (distress)” to “extreme interference (distress).” For pain treatments, providers rated their likelihood of recommending an opioid analgesic to relieve the patient’s pain. Providers also rated their likelihood of using an opioid contract, a bilateral agreement outlining the expectations of opioid use and the consequences for breaching it [33]. The item asked “In the event that you prescribed an opioid analgesic for this patient, how likely are to you to use an opioid contract?” and was rated from “not at all likely” to “very likely.” Additionally, providers rated the degree they would recommend the patient take time off from work and/or seek workplace accommodations from “not at all” to “extremely.” Similar scales have been used successfully in prior studies to assess providers’ pain assessment and treatment recommendations [7, 29].
Implicit attitudes
Implicit attitudes about race and SES were measured with separate Implicit Association Tests (IATs; [34]). For the race IAT, providers categorized facial images as Black or White individuals and evaluative words as good or bad (e.g., “pleasure” = good, “awful” = bad). For the SES IAT, providers categorized higher or lower class words (e.g., “prosperous” = high, “needy” = low) and evaluative words. Providers were asked to press one computer key if the stimulus was a Black face (low SES word) or a good word and press a different key if the stimulus was a White face (high SES word) or a bad word. In reverse trials, providers were instructed to press one key for Black faces (low SES) and bad words and another key for White faces (high SES) and good words. Faster responses to the White (high SES)/good and Black (low SES)/bad pairings than to the Black (low SES)/good and White (high SES)/bad pairings are assumed to indicate a preference or implicit attitude favoring White (high SES) individuals. The IAT produces a D score for each provider’s implicit attitudes about race and SES. D scores range from −2 to +2 with positive values indicating a preference for White and high SES individuals, whereas negative values indicate a preference for Black and low SES individuals [34]. The IAT has demonstrated good reliability and validity and has been shown to be a stronger predictor of prejudice and stereotypes than self-report [35].
Explicit attitudes
Explicit attitudes about race and SES were measured with Feeling Thermometer (FT) Scales. Providers were asked to rate their feelings toward Black and White individuals, and low and high SES individuals on four separate VASs from “extremely cold and unfavorable” (0) to “extremely warm and favorable” (100). Difference scores—White (high SES) minus Black (low SES)—were calculated as an indicator of explicit attitudes. Positive scores indicated an explicit preference for White and high SES individuals. These instruments have been shown to be a reliable and valid method to assess feelings toward different social groups [36].
Social desirability
The 13-item version of the Marlowe-Crowne Social Desirability Scale (MCSDS) was used to assess participants’ general propensity to engage in socially desirable responding. The MCSDS is a self-report measure assessing respondents’ tendency to present themselves in a favorable light. Participants respond true/false to a series of “statements concerning personal attitudes and traits.” Example items include “I am always courteous, even to people who are disagreeable” and “There have been occasions when I took advantage of someone” (reverse scored). Higher scores indicate a greater tendency to engage in socially desirable responding. The MCSDS is a reliable and valid measure of social desirability [37].
Statistical Analyses
We used descriptive statistics to summarize provider demographics and characterize providers’ responses to the IATs and FTs. Average IAT scores were compared to previously defined cut points (direction: positive scores indicate pro-White bias and negative scores indicate pro-Black bias; magnitude: ±.15= slight bias, ±.35 = moderate bias, ±.65 = strong bias; [35]). One-sample t-tests were used to examine differences in providers’ FT scores for Black vs. White individuals and low SES vs. high SES individuals. For each pain assessment and treatment outcome variable, providers’ ratings for each cue combination (White/low SES, White/high SES, Black/low SES, Black/high SES) were averaged, so that each provider had four ratings, representing the four patient combinations. We used repeated-measures ANOVAs to examine main (hypothesis 1) and interactive (hypothesis 2) effects of patient race and SES for each pain-related rating. When significant interactions were present, main effects were not interpreted. Significant interactions were examined with Bonferroni-corrected pairwise comparisons. To examine if providers’ implicit and explicit attitudes moderated the relationships between patient group (race or SES) and providers’ pain-related ratings (hypothesis 3), we conducted repeated-measures moderation analyses with 5,000 bootstrap resamples using the MEMORE SPSS macro [38]. This approach tests for a significant interaction in a repeated-measures design by creating a difference score for the within-subjects variable (e.g., interference rating for White patients minus interference rating for Black patients) and regressing it on the between-subjects moderator variable (e.g., race IAT score). Moderation is indicated when the between-subjects moderator significantly predicts the within-subjects difference score. For significant moderation effects, the Johnson–Neyman (J–N) technique was used to determine the range of IAT or FT scores for which patient race or SES significantly influenced providers’ pain-related ratings. Finally, bivariate correlations and independent samples t-tests explored the relationship of provider characteristics (social desirability, sex, and racial minority status), attitudes, and pain-related decisions.
Results
Bivariate correlations across the two pain assessment and three pain treatment decisions are presented in Table 2.
Table 2.
Bivariate Correlations Between Pain-Related Decisions
| Distress | Opioids | Opioid contract | Workplace accommodations | |
|---|---|---|---|---|
| Interference | .91** | .34** | .10* | .52* |
| Distress | .32** | .11* | .48** | |
| Opioids | -.05 | .29** | ||
| Opioid Contract | .02 |
*p < .05, **p < .01.
Providers’ Pain-Related Ratings
Interference
There was a significant interaction between patient race and SES (F[1, 436] = 17.52, p < .01, η p2 = .04; Table 3). For high SES patients, providers ascribed higher pain interference to Black (M = 54.49 [SD = 18.51]) than White patients (M = 52.73 [SD = 18.82]; η p2 = .03), whereas for low SES patients, providers ascribed higher interference to White (M = 59.82 [SD = 17.94]) than Black patients (M = 58.86 [SD = 17.81]; η p2 = .01).
Table 3.
Results for the Effects of Patient Race and SES on Pain Assessment and Treatment Ratings
| Decision | Patient variable | EMM (SE) | F | η p2 | |
|---|---|---|---|---|---|
| Interference | |||||
| Race | Black | 56.68 (0.83) | 1.45 | .00 | |
| White | 56.28 (0.83) | ||||
| SES | Low | 59.34 (0.83) | 169.04** | .28 | |
| High | 53.61 (0.86) | ||||
| Race × SES | 17.52** | .04 | |||
| Distress | |||||
| Race | Black | 55.87 (0.83) | 22.04** | .05 | |
| White | 54.39 (0.83) | ||||
| SES | Low | 56.68 (0.83) | 81.29** | .16 | |
| High | 53.59 (0.83) | ||||
| Race × SES | 15.58** | .04 | |||
| Opioids | |||||
| Race | Black | 25.00 (1.09) | 13.06** | .03 | |
| White | 23.79 (1.08) | ||||
| SES | Low | 25.46 (1.10) | 30.88** | .07 | |
| High | 23.32 (1.10) | ||||
| Race × SES | 3.07 | .01 | |||
| Opioid Contract | |||||
| Race | Black | 42.47 (1.74) | 0.19 | .00 | |
| White | 42.63 (1.73) | ||||
| SES | Low | 43.43 (1.73) | 19.29** | .04 | |
| High | 41.67 (1.74) | ||||
| Race × SES | 0.06 | .00 | |||
| Workplace Accommodations | |||||
| Race | Black | 38.06 (1.16) | 11.58** | .03 | |
| White | 39.47 (1.12) | ||||
| SES | Low | 43.26 (1.16) | 223.12** | .34 | |
| High | 34.27 (1.16) | ||||
| Race × SES | 25.94** | .06 |
EMM Estimated marginal means; SE Standard error; SES Socioeconomic status.
**p < .01.
Distress
There was a significant interaction between patient race and SES (F[1, 436] = 15.58, p < .01, η p2 = .04; Table 3). For high SES patients, providers ascribed more distress to Black (M = 54.89 [SD = 17.71]) than White patients (M = 52.28 [SD = 18.11]; η p2 = .07), whereas race differences did not emerge for low SES patients.
Opioid treatment and opioid contracts
The main effect of patient race on opioid treatment ratings was significant (F[1, 436] = 13.06, p < .01, η p2 = .03; Table 3). Providers were more likely to recommend opioids for Black than White patients. The main effect of patient SES on opioid treatment ratings was also significant (F[1, 436] = 30.88, p < .01, η p2 = .07). Providers were more likely to recommend opioids for low than high SES patients. There was not a significant interaction between patient race and SES on opioid treatment ratings. The main effect of patient race on opioid contract ratings was not significant. The main effect of patient SES on opioid contract ratings was significant (F[1, 436] = 19.29, p < .01, η p2 = .04). Providers were more likely to use opioid contracts with low than high SES patients. There was not a significant interaction between patient race and SES on opioid contract ratings.
Workplace accommodations
There was a significant interaction between patient race and SES (F[1, 436] = 25.94, p < .01, η p2 = .06; Table 3). For high SES patients, race difference did not emerge, whereas for low SES patients, providers were more likely to recommend workplace accommodations for White (M = 44.89 [SD = 24.96]) than Black patients (M = 41.63 [SD = 25.17]); η p2 = .06).
Provider Attitudes
Providers exhibited a slight implicit preference for White over Black individuals (M = 0.31 [SD = 0.39]) and a strong implicit preference for high SES over low SES individuals (M = 0.90 [SD = 0.35]). On explicit measures, providers indicated more warm/favorable feelings towards White (t[415] = −3.43, p < .01, drm = −.14) and low SES (t[426] = 3.03, p < .01, drm = 0.15) individuals than Black and high SES individuals, respectively. Provider’s implicit and explicit attitudes about race were not significantly correlated (r = .07, p = .16), nor were their implicit and explicit attitudes about SES (r = .10, p = .06). Implicit and explicit attitudes did not significantly differ by provider race or sex (all p values > .05).
Implicit attitudes and pain-related decisions
Providers’ race IAT scores moderated the relationship between patient race and providers’ ratings of distress (b = 2.45; 95% confidence interval [CI]: [0.89, 4.00]; Table 4). J–N results indicated that patient race significantly affected distress ratings for providers with race IAT scores < 0.65 (0.65 is the cut point for strong bias; positive values indicate pro-White bias and negative values indicate pro-Black bias); these providers ascribed more distress to Black than White patients. Providers’ race IAT scores also moderated the relationship between patient race and workplace accommodation ratings (b = 2.85; 95% CI: [0.79, 4.91]). J–N results indicated that providers with race IAT scores > 0.16 (0.15 is the cut-point for slight bias) were more likely to recommend workplace accommodations to White than Black patients. Providers’ race IAT scores did not significantly moderate their other pain-related ratings, and providers’ SES IAT scores did not moderate any of their pain-related ratings.
Table 4.
Moderation Results of Implicit and Explicit Attitudes
| Pain rating | b | SE | 95% CI [low, high] | Sample within the J–N significance region (%) |
|---|---|---|---|---|
| Moderator: Race IAT | ||||
| Interference | 1.26 | 0.85 | [−0.40, 2.92] | — |
| Distress | 2.45 | 0.79 | [0.89, 4.00] | 80.0% |
| Opioids | 1.17 | 0.87 | [−0.53, 2.88] | — |
| Opioid Contracts | −1.09 | 0.95 | [−2.95, 0.78] | — |
| Workplace Accommodations | 2.85 | 1.05 | [0.79, 4.91] | 68.8% |
| Moderator: SES IAT | ||||
| Interference | −1.14 | 1.24 | [−3.58, 1.29] | — |
| Distress | −1.56 | 0.95 | [−3.43, 0.32] | — |
| Opioids | −1.54 | 1.09 | [−3.68, 0.60] | — |
| Opioid Contracts | −0.42 | 1.21 | [−2.79, 1.95] | — |
| Workplace Accommodations | −1.02 | 1.69 | [−4.35, 2.30] | — |
| Moderator: Race FT | ||||
| Interference | 0.01 | 0.02 | [−0.03, 0.06] | — |
| Distress | 0.03 | 0.02 | [−0.01, 0.07] | — |
| Opioids | 0.05 | 0.02 | [0.01, 0.10] | 80.0% |
| Opioid Contracts | −0.04 | 0.02 | [−0.09, 0.01] | — |
| Workplace Accommodations | 0.03 | 0.03 | [−0.02, 0.08] | — |
| Moderator: SES FT | ||||
| Interference | −0.02 | 0.02 | [−0.07, 0.02] | — |
| Distress | 0.00 | 0.02 | [−0.04, 0.03] | — |
| Opioids | 0.00 | 0.02 | [−0.04, 0.04] | — |
| Opioid Contracts | −0.05 | 0.02 | [−0.10, −0.01] | 78.9% |
| Workplace Accommodations | 0.06 | 0.03 | [0.00, 0.12] | 98.8% |
CI Confidence interval; J–N, Johnson–Neyman; IAT Implicit association test; SE Standard error; SES Socioeconomic status.
Explicit attitudes and pain-related decisions
Providers’ race FT scores significantly moderated the relationship between patient race and providers’ opioid ratings (b = 0.05; 95% CI: [0.01, 0.10]; Table 4). J–N results indicated that patient race significantly affected opioid ratings for providers with race FT scores < 11.68 (positive scores indicate a general preference for White people); these providers were more likely to recommend opioids to Black than White patients. Providers’ SES FT scores significantly moderated their opioid contract ratings (b = −0.05; 95% CI: [−0.10, −0.01]). J–N results indicated that providers with SES FT scores > −15.56 (negative scores indicate a general preference for low SES people) were more likely to use opioid contracts with low than high SES patients. Also, of note is the moderation result for workplace accommodation ratings (b = 0.06; 95% CI: [0.00, 0.12]). J–N results indicated that providers with SES FT scores < 70.43 (positive scores indicate a general preference for high SES people) were more likely to recommend workplace accommodations for low than high SES patients, although this result should be interpreted with caution given the 95% CI contained 0.
Provider Characteristics
Scores on the social desirability measure (MCSDS) were not consistently correlated with providers’ pain-related ratings for Black versus White or low versus high SES patients (i.e., the difference scores for the within-subject variables). Among the significant correlations, the magnitude of these effects were weak; higher MCSDS scores (i.e., higher social desirability) were associated with higher ratings of interference (r = −.11, p = .03), distress (r = −.10, p = .04), and opioid contracts (r = −.10, p = .04) for Black than White patients. MCSDS scores were not significantly correlated with race differences in opioid ratings or workplace accommodations or with SES differences in any of the pain assessment and treatment domains (all p values > .05). Male and female providers did not significantly differ in their pain-related decisions (all p values > .05). When compared with racial minority providers, White providers ascribed greater pain interference (t[433] = −2.91, p < .01, d = 0.30) to Black than White patients and were more likely to recommend opioids for Black (t[433] = −2.01, p = .05, d = 0.21) and high SES patients (t[433] = 2.20, p = .03, d = 0.23) than to White and low SES patients, respectively.
Discussion
This study examined the effects of patient race and SES on providers’ pain-related decisions. Results indicated significant main effects of patient race and SES on provider opioid ratings and a main effect of SES on opioid contract ratings. There were significant race × SES interaction effects on provider ratings of pain interference, distress, and workplace accommodations. Additionally, providers’ implicit attitudes about race and explicit attitudes about race and SES moderated some of their pain-related decisions.
Providers were more likely to recommend opioids for Black and low SES patients. These results diverged from study hypotheses and previous work showing Black and low SES patients are less likely to receive opioids compared to their demographic counterparts [6]. One potential explanation is methodological. Previous studies have conducted retrospective analyses of clinical data [6]. Race and SES differences in real clinical settings may be due, in part, to third variables (e.g., differences in nonverbal communication styles) that were controlled for in the current study. The current study also presented “ideal” conditions for decision making. Providers had unlimited time and a low-stress context compared to real clinical settings that impose high cognitive demands via time pressures and interruptions [39]. This contrast is important because, according to the dual process model (DPM), people are more likely to be influenced by stereotypes when making decisions under high cognitive load [40]. Interpreted through this lens, the ideal conditions allowed providers to engage in deliberate cognitive processes, which are more likely to be driven by their (presumably) egalitarian beliefs about race and SES. Another potential, albeit speculative, explanation is that current and recently trained physicians are more knowledgeable about pain and disparities than past cohorts. The Institute of Medicine and popular media have reported on these topics recently [1, 41, 42], and health disparities curricula is increasingly being incorporated into medical education [43, 44]. Relatedly, providers may also be aware that Black and low SES individuals have less access to care [45]. Thus, if a Black or low SES patient presents in clinic, despite these barriers, providers may assume a high level of suffering that necessitates pain care. Moreover, the recent opioid crisis—the rapid increase in opioid prescriptions and misuse—has been portrayed by the media and perceived by many to be a “suburban White problem” [46]. Thus, providers may have been particularly hesitant to recommend opioids to White and high SES patients. Future research is needed to determine which, if any, of the aforementioned tentative interpretations holds true.
As hypothesized, providers were more likely to use opioid contracts with low SES than high SES patients. We previously found that providers believe low SES patients are more likely to misuse opioids [4]. Such beliefs likely contributed to the opioid contract disparity observed herein given other work demonstrating that providers employ opioid contracts with patients they have a subjective “hunch” will misuse medication [47]. One might assume that study providers were more likely to use contracts with low SES patients because they were more likely to recommend them opioids in the first place. However, the opioid contract item was specifically phrased to decouple it from the opioid treatment item, and, indeed, provider responses to the two items were not significantly correlated.
A novel aspect of the current study is that we examined the interactive effects of patient race and SES on providers’ pain-related decisions. For high SES patients, providers ascribed more pain-related interference to Black (vs. White) patients, but the opposite race difference emerged for low SES patients. Providers also rated high SES Black patients as experiencing greater distress than high SES White patients but did not demonstrate a race difference in their distress ratings for low SES patients. Providers may have been less favorable in their views of low SES Black (vs. low SES White) patients—i.e., rating them as being less impaired by their pain—as a result of stereotypical beliefs, widely held by the general public, associating Black people with laziness and welfare and White people with hard work [48]. This stereotype might be particularly salient when assessing and treating low SES patients. That is, if providers hold (or are otherwise influenced by) this stereotypical view, they may have attributed low SES Black patients’ impairments to characterological defects as opposed to consequences of their pain. By contrast, the high SES condition provides counter evidence to the race–work stereotype, which may explain why providers perceived high SES Black patients as experiencing greater pain-related interference and distress, despite their SES advantage. A race × SES interaction also emerged for workplace accommodations; providers were more likely to recommend accommodations for White than Black patients, but this occurred only for low SES patients. For low SES patients, providers may have been influenced again by racial stereotypes about work and recommended fewer accommodations to Black patients as a result. On the flip side, race differences in accommodation ratings for high SES patients may not have emerged because providers assumed these patients were hardworking—regardless of race—because of their high prestige jobs.
The race × SES interactive effects can also be interpreted with patient SES as the “main effect” and race as the moderator. From this perspective, providers ascribed more interference and distress to low than high SES patients and were more likely to recommend them workplace accommodations in general, but these SES effects were stronger for White than Black patients. These results suggest that providers are influenced more by patient SES when making pain-related decisions for White than Black patients. One explanation for this is that 68% of the sample was White (vs. 2% Black), which is similar to the race distribution of providers in real clinical settings (75% White vs. 6% Black; [49]). The out-group homogeneity effect states that people view individuals from an outgroup (i.e., Black patients for White providers) as being more alike and individuals from their own group (i.e., White patients for White providers) as having unique characteristics [50]. Applied to the current study, White providers may have been less attuned to—and less influenced by—socioeconomic differences among Black patients.
This is one of the first studies to examine the extent to which providers’ implicit and explicit attitudes about race and SES are related to chronic pain care decisions. Results indicated that providers’ implicit attitudes about race moderated their distress ratings such that all providers—except those with strong pro-White attitudes—ascribed more distress to Black than White patients. Based on a few prior studies, one might expect that providers with a strong pro-White implicit bias would be most, not least, influenced by race [13, 14]. Nevertheless, the current results are consistent with the direction of prior findings; providers with the most pro-White bias showed the least pro-Black responding by rating Black and White patients equivalently on pain-related distress. The other providers (i.e., those with pro-Black implicit bias, no implicit bias, or slight to moderate pro-White implicit bias) may have ascribed more distress to Black patients due to their awareness of the many disadvantages that Black individuals face with regard to pain and medical care, as well as in society at large (e.g., discrimination). By this interpretation, it required a strong implicit bias against Black individuals (i.e., a strong pro-White implicit bias) to not demonstrate these race effects for distress ratings. Results also indicated that providers with a pro-White implicit bias were more likely to recommend workplace accommodations to White than Black patients. This aligns with previous work showing that providers with a pro-White implicit bias are more likely to recommend care for White than Black patients [13, 14]. Implicit attitudes about SES did not moderate the relationship between patient SES and provider decisions. The small literature on providers’ implicit SES attitudes and provision of care, which includes acute and postoperative pain care, also has not found a significant relationship [16–19]. Collectively, this suggests that patient SES may influence provider decisions via means other than implicit attitudes. Further research is needed to elucidate the primary drivers of SES disparities in pain care.
Providers’ explicit attitudes about race and SES moderated their opioid treatment and opioid contract decisions, respectively. Providers with a pro-Black bias (negative FT score) or with minimal pro-White bias (FT score <11.68) were more likely to recommend opioids to Black than White patients. Providers with a pro-high SES bias (positive FT score) or with minimal pro-low SES bias (FT scores > −15.56) were more likely to use opioid contracts with low (vs. high) SES patients. Additionally, all providers—except those with strong pro-high SES bias (FT score > 70.43)—were more likely to recommend workplace accommodations for low (vs. high) SES patients. These findings are noteworthy given that prior work has not consistently found a relationship between explicit attitudes and clinical care. Decisions about opioids (prescriptions and contracts) and workplace accommodations are high stakes and require careful deliberation. Opioids frequently have an unfavorable risk–benefit ratio and are increasingly scrutinized for chronic pain. Likewise, workplace accommodations impose extra burdens on providers (e.g., paperwork, interacting with employers). Consequently, provider decision making about these modalities may be governed more by explicit attitudes, which, by definition, are deliberative. Furthermore, according to the DPM, settings that impose minimal cognitive load—like the conditions of the current methodology—allow providers greater access to and use of explicit attitudes when making decisions. Future work is needed to elucidate which pain-related decisions are most influenced by patient race and SES and provider attitudes, as well as the environmental conditions that amplify or diminish these effects. Additionally, the current study measured general attitudes about race and SES groups. Prior work has demonstrated that laypersons and health professionals have beliefs about race and SES that are specific to pain and medical care, such as that Black patients have higher pain tolerance than White patients [51, 52]. These specific beliefs may better predict pain care decisions and, thus, merit further study.
The current study has several limitations. First, methodological advantages notwithstanding, VH patients do not fully capture real-world clinical environments. Relatedly, although the large sample is a strength, it may increase the likelihood of finding statistically significant differences that lack substantive clinical implications. This is particularly relevant for interaction effects; thus, these findings should be considered tentative pending future studies. The interaction effects for interference and distress warrant particular attention in future studies given the high correlation among these two variables. Nevertheless, the results were not identical, suggesting that despite their high correlation, interference and distress are distinct. Second, providers were asked about sensitive topics, which may have elicited socially desirable responses. Although social desirability scores largely did not correlate with race and SES differences in pain-related ratings, there is still the concern that our within-subjects design, fixed order of clinical decision items, and general description of the study purpose evoked demand characteristics and resulted in counter-stereotypical responding—we cannot rule out this possibility. Third, the results may not generalize to pain conditions other than chronic back pain. Relatedly, we examined two categories of race (Black/White) and SES (low/high). Other race/ethnic groups and SES categories (e.g., blue collar, middle class) should be considered in future studies. Further, SES was manipulated via occupational income/prestige. Other indicators of SES (e.g., education) may affect provider decisions in real clinical settings. Fourth, the SES IAT is not as well established as other versions of the IAT, especially regarding construct validity. As such, these results should be considered with caution. Of particular concern is the fact that the SES IAT used words for the SES stimuli instead of images like in the race IAT. Because the words representing the SES and evaluative categories are more similar to each other than the stimuli used in other versions of the IAT, this may introduce a methodological bias, resulting in artificially inflated scores. For this reason, we are currently developing an SES IAT with images. Finally, the sample consisted of physician residents and fellows who were largely White and working in hospital settings, with limited health care experience; thus, the results may not apply to other health care professionals or settings. Limitations notwithstanding, this is one of the first studies to find that patient race and SES uniquely and interactively impact provider decisions for chronic pain care. The results highlight the need to incorporate both race and SES in research on provider decision making for diverse patients.
Acknowledgments
The authors thank Shankar Manamalkav for his excellent technical assistance in the development and implementation of this project. Research reported in this publication was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R01MD008931. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. There are no conflicts of interest that might be seen as influencing or prejudicing the research.
Compliance with Ethical Standards
Conflict of Interest The authors declare that they have no conflict of interest.
Ethnical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent was obtained from all individual participants included in the study. These procedures were approved by Indiana University IRB.
References
- 1. Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: The National Academies Press; 2003. [PubMed] [Google Scholar]
- 2. Joynt M, Train MK, Robbins BW, Halterman JS, Caiola E, Fortuna RJ. The impact of neighborhood socioeconomic status and race on the prescribing of opioids in emergency departments throughout the United States. J Gen Intern Med. 2013;28:1604–1610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chibnall JT, Tait RC, Andresen EM, Hadler NM. Race and socioeconomic differences in post-settlement outcomes for African American and Caucasian Workers’ Compensation claimants with low back injuries. Pain. 2005;114:462–472. [DOI] [PubMed] [Google Scholar]
- 4. Hollingshead NA, Matthias MS, Bair M, Hirsh AT. Healthcare providers’ perceptions of socioeconomically disadvantaged patients with chronic pain: a qualitative investigation. J Health Dispar Res Pract. 2016;9:3. [Google Scholar]
- 5. Becker WC, Starrels JL, Heo M, Li X, Weiner MG, Turner BJ. Racial differences in primary care opioid risk reduction strategies. Ann Fam Med. 2011;9:219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Meghani SH, Byun E, Gallagher RM. Time to take stock: a meta-analysis and systematic review of analgesic treatment disparities for pain in the United States. Pain Med. 2012;13:150–174. [DOI] [PubMed] [Google Scholar]
- 7. Nampiaparampil DE, Nampiaparampil JX, Harden RN. Pain and prejudice. Pain Med. 2009;10:716–721. [DOI] [PubMed] [Google Scholar]
- 8. Chibnall JT, Tait RC. Long-term adjustment to work-related low back pain: associations with socio-demographics, claim processes, and post-settlement adjustment. Pain Med. 2009;10:1378–1388. [DOI] [PubMed] [Google Scholar]
- 9. Meghani SH, Chittams J. Controlling for socioeconomic status in pain disparities research: All-Else-Equal analysis when “All Else” is not equal. Pain Med. 2015;16:2222–2225. [DOI] [PubMed] [Google Scholar]
- 10. Hayward MD, Miles TP, Crimmins EM, Yang Y. The significance of socioeconomic status in explaining the racial gap in chronic health conditions. Am Sociol Rev. 2000;65:910–930. [Google Scholar]
- 11. Pew Research Center. On views of race and inequality, Blacks and Whites are worlds apart. Available at https://www.pewsocialtrends.org/2016/06/27/on-views-of-race-and-inequality-blacks-and-whites-are-worlds-apart/. Accessibility verified March 29, 2019.
- 12. Dovidio JF, Kawakami K, Gaertner SL. Implicit and explicit prejudice and interracial interaction. J Pers Soc Psychol. 2002;82:62–68. [DOI] [PubMed] [Google Scholar]
- 13. Green AR, Carney DR, Pallin DJ, et al. . Implicit bias among physicians and its prediction of thrombolysis decisions for black and white patients. J Gen Intern Med. 2007;22:1231–1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sabin JA, Greenwald AG. The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. Am J Public Health. 2012;102:988–995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hall WJ, Chapman MV, Lee KM, et al. . Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: a systematic review. Am J Public Health. 2015;105:e60–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Haider AH, Sexton J, Sriram N, et al. . Association of unconscious race and social class bias with vignette-based clinical assessments by medical students. Jama. 2011;306:942–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Haider AH, Schneider EB, Sriram N, et al. . Unconscious race and class bias: its association with decision making by trauma and acute care surgeons. J Trauma Acute Care Surg. 2014;77:409–416. [DOI] [PubMed] [Google Scholar]
- 18. Haider AH, Schneider EB, Sriram N, et al. . Unconscious race and class biases among registered nurses: vignette-based study using implicit association testing. J Am Coll Surg. 2015;220:1077–1086.e3. [DOI] [PubMed] [Google Scholar]
- 19. Haider AH, Schneider EB, Sriram N, et al. . Unconscious race and social class bias among acute care surgical clinicians and clinical treatment decisions. JAMA Surg. 2015;150:457–464. [DOI] [PubMed] [Google Scholar]
- 20. Blair IV, Steiner JF, Fairclough DL, et al. . Clinicians’ implicit ethnic/racial bias and perceptions of care among Black and Latino patients. Ann Fam Med. 2013;11:43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hagiwara N, Penner LA, Gonzalez R, et al. . Racial attitudes, physician-patient talk time ratio, and adherence in racially discordant medical interactions. Soc Sci Med. 2013;87:123–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Burgess DJ, van Ryn M, Crowley-Matoka M, Malat J. Understanding the provider contribution to race/ethnicity disparities in pain treatment: insights from dual process models of stereotyping. Pain Med. 2006;7:119–134. [DOI] [PubMed] [Google Scholar]
- 23. Hirsh AT, Alqudah AF, Stutts LA, Robinson ME. Virtual human technology: capturing sex, race, and age influences in individual pain decision policies. Pain. 2008;140:231–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hirsh AT, George SZ, Robinson ME. Pain assessment and treatment disparities: a virtual human technology investigation. Pain. 2009;143:106–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Hirsh AT, Hollingshead NA, Bair MJ, Matthias MS, Wu J, Kroenke K. The influence of patient’s sex, race and depression on clinician pain treatment decisions. Eur J Pain. 2013;17:1569–1579. [DOI] [PubMed] [Google Scholar]
- 26. Hirsh AT, Miller MM, Hollingshead NA, et al. . A randomized controlled trial testing a virtual perspective-taking intervention to reduce race and socioeconomic status disparities in pain care. Pain. 2019;160:2229–2240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Wigton RS. Social judgement theory and medical judgement. Think Reas. 1996;2:175–190. [Google Scholar]
- 28. Wigton RS. Applications of judgment analysis and cognitive feedback to medicine. In: Amsterdam N, ed. Human Judgment: The SJT View (Vol. 54). Amsterdam, Netherlands: Elsevier; 1988:227–245. [Google Scholar]
- 29. Hirsh AT, Hollingshead NA, Ashburn-Nardo L, Kroenke K. The interaction of patient race, provider bias, and clinical ambiguity on pain management decisions. J Pain. 2015;16:558–568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cooksey R. Judgment Analysis: Theory, Methods, and Applications. San Francisco, CA: Academic Press; 1996. [Google Scholar]
- 31. Nam CB, Boyd M. Occupational status in 2000; over a century of census-based measurement. Popul Res Policy Rev. 2004;23:327–358. [Google Scholar]
- 32. Alqudah AF, Hirsh AT, Stutts LA, Scipio CD, Robinson ME. Sex and race differences in rating others’ pain, pain-related negative mood, pain coping, and recommending medical help. J Cyber Ther Rehabil. 2010;3:63–70. [PMC free article] [PubMed] [Google Scholar]
- 33. Fishman SM, Bandman TB, Edwards A, Borsook D. The opioid contract in the management of chronic pain. J Pain Symptom Manage. 1999;18:27–37. [DOI] [PubMed] [Google Scholar]
- 34. Greenwald AG, Nosek BA, Banaji MR. Understanding and using the implicit association test: I. An improved scoring algorithm. J Pers Soc Psychol. 2003;85:197–216. [DOI] [PubMed] [Google Scholar]
- 35. Greenwald AG, Poehlman TA, Uhlmann EL, Banaji MR. Understanding and using the implicit association test: III. Meta-analysis of predictive validity. J Pers Soc Psychol. 2009;97:17–41. [DOI] [PubMed] [Google Scholar]
- 36. Alwin DF. Feeling thermometers versus 7-point scales which are better? Sociol Methods Res. 1997;25:318–340. [Google Scholar]
- 37. Reynolds WM. Development of reliable and valid short forms of the Marlowe‐Crowne social desirability scale. J Clin Psychol. 1982;38:119–125. [Google Scholar]
- 38. Montoya AK. Moderation analysis in two-instance repeated measures designs: Probing methods and multiple moderator models. Behav Res Methods. 2019;51:61–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. van Ryn M, Burgess DJ, Dovidio JF, et al. . The impact of racism on clinician cognition, behavior, and clinical decision making. Du Bois Rev. 2011;8:199–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Burgess DJ, Phelan S, Workman M, et al. . The effect of cognitive load and patient race on physicians’ decisions to prescribe opioids for chronic low back pain: A randomized trial. Pain Med. 2014;15:965–974. [DOI] [PubMed] [Google Scholar]
- 41. Institute of Medicine and the Committee on Advancing Pain Research. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 42. Galvin G. How racial bias has shaped the opioid epidemic. Available at https://www.usnews.com/news/healthiest-communities/articles/2019-02-11/racism-helped-shape-the-opioid-epidemic-study-suggests. Accessibility verified November 1, 2019.
- 43. American Medical Association. Med school curriculum changes aim to eliminate health care disparities. Available at https://www.ama-assn.org/education/accelerating-change-medical-education/med-school-curriculum-changes-aim-eliminate-health. Accessibility verified November 1, 2019.
- 44. Awosogba T, Betancourt JR, Conyers FG, et al. . Prioritizing health disparities in medical education to improve care. Ann N Y Acad Sci. 2013;1287:17–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Agency for Healthcare Research and Quality. Access and disparities in access to health care. Available at http://www.ahrq.gov/research/findings/nhqrdr/nhqdr16/access.html. Accessibility verified September 8, 2018.
- 46. Hansen H, Netherland J. Is the prescription opioid epidemic a white problem? Am J Public Health. 2016;106:2127–2129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Starrels JL, Wu B, Peyser D, et al. . It made my life a little easier: Primary care providers’ beliefs and attitudes about using opioid treatment agreements. J Opioid Manag. 2014;10:95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Brown-Iannuzzi JL, Dotsch R, Cooley E, Payne BK. The relationship between mental representations of welfare recipients and attitudes toward welfare. Psychol Sci. 2017;28:92–103. [DOI] [PubMed] [Google Scholar]
- 49. Castillo-Page L. Diversity in the Physician Workforce: Facts and Figures 2010. Washington, DC: Association of American Medical Colleges; 2010. [Google Scholar]
- 50. Park B, Rothbart M. Perception of out-group homogeneity and levels of social categorization: Memory for the subordinate attributes of in-group and out-group members. J Pers Soc Psychol. 1982;42:1051. [Google Scholar]
- 51. Hoffman KM, Trawalter S, Axt JR, Oliver MN. Racial bias in pain assessment and treatment recommendations, and false beliefs about biological differences between blacks and whites. Proc Natl Acad Sci USA 2016;113:4296–4301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hollingshead NA, Meints SM, Miller MM, Robinson ME, Hirsh AT. A comparison of race-related pain stereotypes held by White and Black individuals. J Appl Soc Psychol. 2016;46:718–723. [DOI] [PMC free article] [PubMed] [Google Scholar]